Abstract
Background:
Intense pulsed light (IPL) has been used for the treatment of facial acne. Modifications of various parameters allow flexibility in treatment, which include energy fluence, pulse duration, and pulse delay. We compared the efficacy of burst-pulse (multiple pulse) mode with single-pulse mode in treatment of acne.
Objective:
This study was designed to evaluate the efficacy of the IPL in treatment of facial acne and to compare burst-pulse and single-pulse mode in treatment of acne.
Materials and Methods:
Ten patients with facial acne were subjected to monotherapy with IPL. Baseline grading of acne was done with Michelsons acne severity index; however, right and left side of face were scored separately and a total score was also taken. IPL was administered once weekly for four sessions. Right side was subjected to IPL with burst-pulse mode, and left side was subjected to single-pulse mode. Severity score assessed after the end of treatment. Clinical photographs were also obtained for evaluation.
Results:
All patients revealed a reduction in number of acne for both single- and burst-pulse mode treated sides. The mean total score was 49.4 at baseline and showed 49.19% reduction after four sessions of IPL. Burst-pulse mode treated side showed a better control than that of single-pulse mode.
Conclusion:
IPL as a monotherapy showed beneficial effect in treatment of facial acne. Burst-pulse mode was better than the single-pulse mode in clearing acne.
Keywords: Acne, intense pulse light, pulse mode
Introduction
We are at an exciting time in the evolution of acne therapy, as many new advances are providing positive results for our patients. Lasers and light sources have become a useful addition to our therapeutic armamentarium for acne vulgaris. The use of intense pulsed light (IPL) may further enhance the benefits of these devices. IPL works in two modes (single- and burst-pulse modes). We conducted this study to compare the burst-pulse and single-pulse modes in IPL for treating acne vulgaris and to study the efficacy of IPL in treating acne vulgaris.
Materials and Methods
Ten patients with grade 1–4 acne vulgaris were included in the study. They were subjected to monotherapy with IPL (V care Medical Systems Private limited, Bangalore, Karnataka). Patients who were taking oral or topical antiacne medications before reporting to us were excluded from the study. Baseline grading of acne was done with Michelsons acne severity index (Number of comedones, papules, pustules, infiltrated and cystic lesions are counted. Severity index is 0.5 for comedones, 1 for papules, 2 for pustules, 3 for infiltrated lesion, and 4 for cystic lesions. Multiplying each type of lesion with its severity index and adding score together give the final score) however, right side and left side of face were scored separately and a total score was also noted. Grading was done by a blinded observer. Informed consent was obtained from all the patients. Test dose with IPL was done on the forearm, and the most tolerable dose was selected. Starting dose was 1 J less than the most tolerable dose, which varied among the patients. The lowest fluence used for treatment on the face was 15 J, and the maximum fluence used was 21 J and 420 nm cutoff filter was used for the study. IPL was administered once a week for 4 weeks, and the fluence was increased by 1 J every session. Right side of the face was subjected to burst-pulse mode, and the left side was subjected to single-pulse mode. The IPL parameters were: auto mode, skin type 4, pulse width 12 ms, single-pulse mode for left side of face and burst-pulse mode (five pulses and pulse delay 6 ms) for right side of face. Severity index was calculated after four sessions, and digital photographs were taken at the baseline and after four sessions for comparison. Results were statistically analyzed using paired t-test.
Results
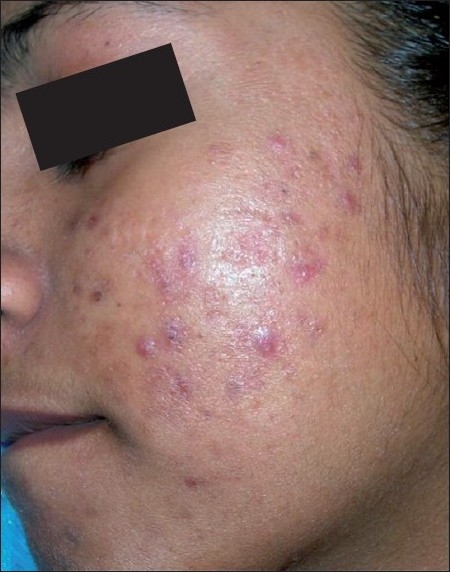
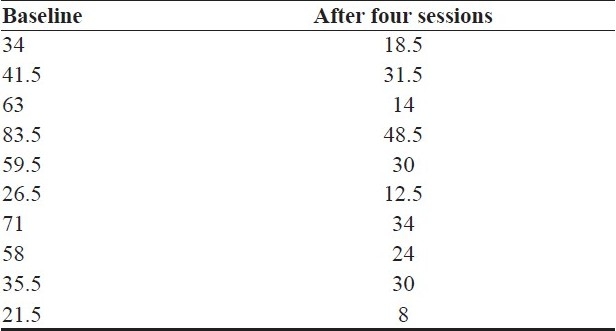
Ten patients (six males and four females) were included in the study. Age group varied from 18 to 25. Clinical significant acne clearance was observed. No adverse side effects were observed during treatment and post-treatment. The mean baseline score was 22.4 for single-pulse mode, which showed 40.17% reduction after four sessions [Figures 1 and 2]. The mean acne severity score at baseline was 27 for burst-pulse mode and showed 56.66% reduction after four sessions [Figures 3 and 4]. Burst-pulse treated side showed a better control than the single-pulse treated site. [Figures 5 and 6] The mean total score was 49.4 at baseline and showed 49.19% reduction after four sessions of IPL [Table 1]. Table 2 shows the total score at the baseline and after four sessions of IPL. Paired t-test was performed for statistical analysis. Total score showed statistically significant improvement after four sessions of IPL (SD = 4.5351, critical t-value = 2.2622, t value = 5.3693). The improvement in severity score on burst-pulse mode treated side was statistically significant (SD = 3.0433, t-value = 5.0439). Severity score of single-pulse mode treated side also showed significant improvement (SD = 1.9621, t-value = 4.5868).
Figure 1.

Before treatment (single-pulse mode)
Figure 2.
After treatment (single-pulse mode)
Figure 3.

Before treatment (burst-pulse mode)
Figure 4.

After treatment (burst-pulse mode)
Figure 5.

Burst-pulse treated site after four sessions
Figure 6.

Single-pulse treated site after four sessions
Table 1.
Acne severity score for single- and burst-pulse modes
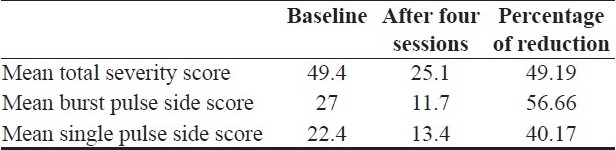
Table 2.
Acne severity score - total score for full face
Discussion
IPL technology involves application of a noncoherent, nonlaser broadband, filtered flash lamp source directed to the skin. Modifications of various parameters allow flexibility in treatment, which include wavelength, energy fluence, pulse duration, and pulse delay.
IPL acts by photodynamic therapy (PDT) in the treatment of acne vulgaris.[1] Propionibacterium acnes (P. acnes) produces the porphyrins during their growth and proliferation in the follicular units. The porphyrins produced during this proliferative phase are protoporphyrin IX and coproporphyrin III. These porphyrins have an absorption spectrum that is in the near ultraviolet (UV) and visible spectrum of light. The major absorption peak for these porphyrins is at 415 nm, known commonly as the Soret band. This absorption peak is in the blue range of the visible light spectrum.[2] A second major peak, seen at 630 nm, is also visible in the absorption spectrum, which corresponds to red light. Therefore, phototherapy devices have been developed that utilize either blue light or red light PDT for the treatment of inflammatory acne vulgaris lesions. The PDT process seen in this reaction involves the photoexcitation of the P. acnes porphyrins after exposure to the appropriate light source. This will then form singlet oxygen within the microorganism itself, resulting in the selective destruction of the bacteria. The reaction occurs rapidly and has been observed in vivo.[1–3]
A variety of IPL sources have been used to treat acne vulgaris. Elman et al.[4] treated 19 patients with IPL and showed that 85% of the individuals had a >50% improvement in their acne vulgaris lesions following twice weekly therapy for 4 weeks. Dierickx[5] reported on the Lux V™ handpiece from the Palomar Medical Technologies IPL systems (EsteLux® , MediLux™, and StarLux™ Systems). Fourteen patients with mild-to-moderate inflammatory acne vulgaris lesions received five treatments that were administered every 2–4 weeks. At 6 months post-therapy, clearance rates of 72% for noninflammatory acne vulgaris lesions and 73% for inflammatory acne vulgaris lesions were observed. Paithankar et al.[6] reported 50% reduction in inflammatory acne vulgaris with IPL-ClearTouch/SkinStation (Radiancy, Orangeburg, NY, USA).
IPL technology works in single- and burst-pulse modes. In the single-pulse mode, the fluence will be delivered in single shot, whereas in burst-pulse mode fluence is divided into series of pulses with a delay between the pulses. There are no studies comparing the single- and burst-pulse modes.
We found 49% reduction in the acne severity score with weekly IPL monotherapy after four treatments. Both the modes showed a reduction in acne score, but burst-pulse mode (56%) showed a better clearance than the single-pulse mode (40%). IPL as a monotherapy leads to significant acne clearance, and burst-pulse mode (five pulses, 6 ms pulse delay) was better than single-pulse mode in our study. Combining IPL with topical and systemic medications may further enhance the efficacy of IPL. Since our sample size was small, further studies with a large sample size are required to establish these findings.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Gold MH. Acne and PDT: New techniques with lasers and light sources. Lasers Med Sci. 2007;22:67–72. doi: 10.1007/s10103-006-0420-z. [DOI] [PubMed] [Google Scholar]
- 2.Sigurdsson V, Knulst AC, van Weelden H. Phototherapy of acne vulgaris with visible light. Dermatology. 1997;194:256–60. doi: 10.1159/000246114. [DOI] [PubMed] [Google Scholar]
- 3.Taub AF. Photodynamic therapy in dermatology: History and horizons. J Drugs Dermatol. 2004;3:S8–25. [PubMed] [Google Scholar]
- 4.Elman M, Lask G. The role of pulsed light and heat energy (LHE™) in acne clearance. J Cosmet Laser Ther. 2004;6:91–5. doi: 10.1080/14764170410035584. [DOI] [PubMed] [Google Scholar]
- 5.Dierickx CC. Treatment of acne vulgaris with a variable-filtration IPL system. Lasers Surg Med. 2004;34:66. [Google Scholar]
- 6.Paithankar DY, Ross EV, Saleh BA, Blair MA, Graham BS. Acne treatment with a 1450nm wavelength laser and cryogen spray cooling. Lasers Surg Med. 2002;31:106–14. doi: 10.1002/lsm.10086. [DOI] [PubMed] [Google Scholar]


