Abstract
This study presents results of a subgroup analysis from a randomized trial to examine whether Structural Ecosystems Therapy (SET), a family intervention intended to improve medication adherence and reduce drug relapse of HIV-seropositive (HIV+) women recovering from drug abuse, provided benefits for families with children. Data from 42 children and 25 mothers were analyzed at baseline, and 4, 8, and 12 months post-baseline. Results of longitudinal Generalized Estimating Equations analyses suggested that SET was more efficacious than the Health Group (HG) control condition in decreasing children's internalizing and externalizing problems and reducing mothers' psychological distress and drug relapse. Children in SET reported improvements in positive parenting as compared to the children in HG, but there were no differences in mother-reported positive parenting, or parental involvement as reported by either the children or mothers. These findings suggest that family interventions such as SET may be beneficial for mothers and children. An adaptation of SET specifically for families with children could further enhance benefits and improve acceptability and cost-effectiveness.
Keywords: children's externalizing and internalizing problems, maternal HIV, maternal drug abuse, Structural Ecosystems Therapy
Women, particularly African American and of childrearing age, are increasingly at risk for HIV/AIDS. The most recent report from the Centers for Disease Control and Prevention (CDC, 2009) estimates that 26% of all new HIV/AIDS diagnoses are among women. A sizable proportion of HIV seropositive (HIV+) women are mothers. The HIV Cost and Services Utilization Study surveyed a nationally representative sample of HIV+ adults receiving health care in 1996 and 1997. Of 840 women in the sample, 60% had minor children living with them (Schuster et al., 2000).
Children of HIV+ mothers have been found to be at risk for internalizing and externalizing problems (e.g., Forehand et al., 2002; Tompkins & Wyatt, 2008), although some studies have not found significantly increased risk for children of HIV+ mothers when compared with demographically similar controls (e.g. Lester et al., 2010). Studies have also demonstrated that children of HIV+ mothers are detrimentally affected by maternal substance abuse (Lester et al., 2009; Rotheram-Borus & Stein, 1999). Children with dually-diagnosed parents appear to derive greater adverse effects from the parent's substance abuse than from HIV (Cowgill et al., 2007; Leonard, Gwadz, Cleland, Vekaria, & Ferns, 2008).
Research has demonstrated the linkages between parenting processes and child outcomes in families affected by parental HIV and/or substance abuse. Studies with demographically comparable groups of children with HIV+ and HIV-mothers have found less close parent-child relationships (Forehand et al., 2002; Kotchick et al., 1997) and less monitoring (Forehand et al., 2002) in families with HIV+ mothers, which in turn were connected to less favorable child outcomes. Lester et al. (2010), however, while finding that family processes were associated with children's internalizing and externalizing problems, also found that children with HIV+ mothers reported more positive maternal bonds than children not in HIV-affected families. There is also research linking impaired parenting processes (e.g. supervision, closeness, and positive parenting) with internalizing and externalizing problems among children whose mothers have substance abuse disorders (Kandel, 1990; Stanger et al., 2002).
Family Interventions
Family interventions for children at risk due to a parent's substance abuse or HIV have shown encouraging results. Partners in Parenting (Knight, Bartholomew, & Simpson, 2007), a parenting skills program for mothers in substance abuse treatment, resulted in improved parenting and reduced family conflict. Focus on Families (Catalano, Gainey, Fleming, Haggerty, & Johnson, 1999), which supplements methadone treatment with family training and case management, resulted in improved parenting and reduced drug use in parents. Rotheram-Borus and colleagues' coping skills intervention for HIV+ parents and their adolescent children has resulted in decreased unprotected sex, alcohol use, and contact with the criminal justice system in parents at two years post intervention (Rotheram-Borus, Lee, Gwadz, & Draimin, 2001), reduced negative family events, decreased externalizing and internalizing problems in adolescents, and improved problem solving in parents at 4 years (Rotheram-Borus et al., 2003) and improved problem solving in adolescents at 6 years (Rotheram-Borus, Lee, Lin, & Lester, 2004).
Persons living with HIV/AIDS (PLWHA) are also in need of psychosocial interventions to address their health and due to increased risk for psychological distress (Remien et al., 2006; Simoni & Ng, 2000) and drug abuse (Klinkenberg & Sacks, 2004). Despite the recognition that families affect the emotional and physical wellbeing of PLWHA (Pequegnat & Szapocznik, 2002; Rotheram-Borus, Flannery, Rice, & Lester, 2005), interventions have for the most part been individually oriented. The exceptions are the work of Rotheram-Borus cited above, a couples intervention for HIV medication adherence (Remien et al., 2005) and Structural Ecosystems Therapy (SET, Mitrani, Robinson, & Szapocznik, 2009) which is the focus of the present study.
SET (Mitrani et al., 2009) aims to improve the psychosocial functioning of HIV+ women by improving interactions within the family, and between the woman, family, social environment and service providers. These interactional changes are meant to increase the woman's access to support from her family, social network and community resources, and to help her establish boundaries with problematic elements such as drug abusing family and peers. SET is based on Brief Strategic Family Therapy (Szapocznik & Kurtines, 1989), which in turn is based upon structural (Minuchin & Fishman, 1981) and strategic (Haley, 1987) family therapy approaches. As a structural/strategic family therapy, the theoretical underpinnings of SET propose that interactional changes will set into motion a series of effects on individuals, which in the case of SET are specifically targeted at the HIV+ woman's emotional health, self-care, and drug use.
A randomized trial of SET with HIV+ African American women found that SET reduced psychological distress as compared to an individual person-centered intervention and a community control condition (Szapocznik et al., 2004), and lowered drug use relapse (Feaster et al., 2010b) and increased medication adherence (Feaster et al., 2010c) as compared to the person-centered intervention. Szapocznik and colleagues (2004) found that reduced family hassles partially mediated the effects of SET on psychological distress, providing some support for the theoretical mechanism of change. A recently completed randomized trial of SET, which serves as the parent trial for the current study, was aimed at improving HIV medication adherence and preventing relapse among HIV+ women in drug recovery. The trial had mixed results. Women in SET did not experience better drug use or medication adherence outcomes as compared to those in a Health Group (HG) control condition, but did show improvement in CD4T-cell count and in theoretical mechanisms of action on drug relapse including accessing substance abuse services in response to relapse and separating from drug-using household members (Feaster et al., 2010a).
One of the findings in the parent trial for the current study was that living with children was associated with treatment engagement (attending two or more sessions) across both interventions (Mitrani, Feaster, Weiss-Laxer, & McCabe, 2010). Among women who were randomized to SET, the engagement rate was 71% for women living with children as compared to 54% for women not living with children. This finding that SET might be better-accepted by women with children, coupled with the known risks to children with respect to parental HIV and drug use as well as the potential of family interventions for improving parenting functions and the wellbeing of parents and children, highlights the significance of examining the impact of SET in families with children. Evidence of SET's effects for mothers and children could be used to lay the groundwork for a future adaptation of SET for families with children.
Aims of the Study
The current sub-group analysis tests the hypothesis that SET will result in improved outcomes relative to the HG control group, and specifically that: 1) children will have significantly lower internalizing and externalizing problems; 2) mothers will have significantly improved outcomes in constructs parallel to those being examined in the children, psychological distress and drug use; and 3) children and mothers will experience improved positive parenting (positive reinforcement, e.g., praise or a hug, which a parent uses in response to a child's desired behavior) and parental involvement (e.g., how often a parent spends time with a child or talks about events in the child's life). Measures from mothers and children on child outcomes and parenting are tested separately because of research demonstrating parent-child discordance in ratings (De Los Reyes & Kazdin, 2005; Lester et al., 2010). Because of gender differences that have been noted on internalizing and externalizing problems in children (Achenbach & Rescorla, 2001; Quay & Peterson, 1987) we examined whether any significant intervention effects for children were moderated by gender.
Methods
Participants
Participants were 25 mothers recruited as part of a randomized trial comparing SET and HG (Feaster et al., 2010a) for HIV+ women in drug recovery, and 42 of their children (biological and step). All women in the trial were either taking HIV medications or at a stage of HIV infection at which HIV medications would be advised, and met DSM–IV criteria for a substance use diagnosis within the last year (cocaine either primary or secondary). Methods of the larger trial are more fully described in Feaster et al. (2010a). A companion study examining the family mechanisms of SET enrolled family members of the women. The subgroup for this study was created by including only those target women in the trial with children who enrolled in the family mechanisms study, lived with the woman, and were between ages 6 and 18 years. Table 1 shows characteristics of the women in each condition. There were 19 girls and 23 boys in this sample, with no gender difference by condition, SET (n of girls = 7, 47%), and HG (n of girls = 12, 44%), χ2(1, N = 42) = 0.02, p = .89. Children in SET were younger (M = 11.20, SD = 3.67) than children in HG (M = 13.85, SD = 3.07), F(1, 41) = 6.25, p < .05.
Table 1. Baseline Characteristics of Target Women Assigned to Each Condition.
| Characteristic | SET (n = 9) | HG (n = 16) | ||
|---|---|---|---|---|
| Age in years (M, SD) | 38.88 | 5.19 | 40.24 | 7.7 |
| Employed (n, %) | 2 | 22% | 3 | 19% |
| Hispanic (n, %) | 1 | 11% | 1 | 6% |
| African American (n, %) | 7 | 78% | 15 | 94% |
| Never married, not cohabitating (n, %) | 4 | 44% | 10 | 63% |
| Household income in U.S. dollars (M, SD) | 13,556 | 7086 | 9,770 | 6163 |
| CD4 Cell Count (M, SD) | 625.13 | 283.89 | 555.07 | 360.97 |
| Log HIV viral load (M, SD) | 3.69 | 1.14 | 2.86 | 1.33 |
| Years since HIV diagnosis (M, SD) | 9.79 | 5.18 | 9.22 | 5.21 |
| Years of substance abuse (M, SD) | 21.13 | 7.26 | 18.12 | 9.08 |
| Cocaine dependence (n, %) | 7 | 78% | 16 | 100% |
| Dependent on multiple substances (n, %) | 5 | 56% | 14 | 88% |
Note. SET = Structural ecosystems therapy; HG = Health group.
p < .05.
Treatment Conditions
SET (Mitrani et al., 2009) applies structural/strategic techniques to increase adaptive interactions and reduce problematic interactions within the family and between the HIV+ woman, her family, and the larger community and provider network (e.g., health care, substance abuse treatment, religious institutions, neighbors). The aim of these interactional changes is to improve the HIV+ woman's emotional and physical wellbeing, and specifically to improve medication adherence and reduce drug relapse.
As a process-based intervention SET is not limited to a particular content area. SET therapists were instructed to address relapse prevention and HIV medication adherence and the intended dosage was twelve 1-hr sessions over a period of 4 months. Sessions are intended as conjoint and women were guided in including family members and others. On average 2.41 (SD = 0.58, range 1 to 5) persons in addition to the target women (mothers, siblings, grandmothers, current and past partners, cousins, friends, and health-care workers) attended sessions. Sessions were conducted at the woman's home or other locations preferred by the women. There is a SET manual and sessions were videotaped for supervision and fidelity ratings.
The three categories of SET techniques are joining, diagnosing, and restructuring (cf. Minuchin & Fishman, 1981; Szapocznik & Kurtines, 1989). Joining refers to the process of establishing a therapeutic system that includes the therapist, woman, her family, and representatives from other relevant systems. Diagnosing refers to the identification of interactional patterns that contribute to the problems experienced by the woman, and thus need to be changed, as well as those that are sources of support and thus should be reinforced. SET's diagnostic framework includes five dimensions: (a) structure (leadership, subsystems and alliances, and communication flow); (b) developmental stage (the age-appropriateness of family members' roles and behaviors); (c) resonance (the level of permeability of boundaries among family members and between the family and other systems); (d) identified patienthood (the extent to which the HIV+ woman is viewed as the cause of the family's problems); and (e) conflict resolution (the management of problems and disagreements). Restructuring involves orchestrating interactional changes and includes three categories of techniques: (a) working in the present (also known as enactment) involves shaping interactions between persons in a session; (b) reframing (Minuchin & Fishman, 1981) is a strategy of cognitive restructuring through re-labeling that permits more positive interactions to emerge; and (c) shifting boundaries, used when a treatment goal is to move people closer together (such as bringing a woman closer to a potential source of support) or further apart (such as creating distance between a woman and a substance abusing household member), involves regulating the distance or proximity between individuals such as by including or excluding persons from a session, or by directing disengaged individuals to do an activity together.
The HG control condition was selected to control for common factors in therapy such as level of attention, therapist qualities and enthusiasm, or client expectancies. The intervention was adapted from the Wellness Manual developed by Hartfield (cf. Baker et al., 2003) and designed to replicate a popular program available in the local community. Sessions included information about HIV adherence and HIV transmission risk reduction in the following sequence: introduction to anatomy, sexually transmitted infections, HIV basics for women, communicating with partner, alcohol and drugs, safer sex and pregnancy, your baby/child and violence against women, HIV medication adherence. The HG met bi-weekly over a 4-month period for an average of 1.5 hrs per session. Sessions were conducted in the evening at the study offices located at an urban medical campus. There is an HG manual and sessions were videotaped for fidelity rating. On average, 4.90 (SD = 2.25) women attended each group session.
Dosage was comparable across treatment conditions, for number of sessions (SET: M = 6.38, SD = 4.75; HG: M = 4.24, SD = 2.97), F(1, 24) = 1.92, p = .18; and engagement (defined as attending at least two sessions; SET: n = 6, 67%; HG: n = 13, 81%), χ2(1, N = 25) = 0.01, p = .94. Videotaped sessions from SET and HG were rated (1 = not at all/poor to 5 = extensively/excellent) for fidelity to therapy protocol. Two raters were initially trained to an inter-rater reliability coefficient of .80 with the rating supervisor, and retrained every 6 months to prevent drift. Overall inter-rater reliability was .98 for SET and .96 for HG. SET sessions were rated on joining, tracking and eliciting diagnostic enactments, creating a context for change, restructuring the family system, and content focus of therapy session. Ratings of SET sessions showed fair to average (∼3) fidelity (joining, M = 3.89, SD = 0.81; eliciting diagnostic enactments, M = 3.72, SD = 0.78; creating context for change, M = 2.58, SD = 1.01; restructuring, M = 2.41, SD = 0.82). HG sessions were rated for joining, promoting group cohesiveness, acting as a “switchboard,” wrapping up and the extent that assigned topics were covered. Ratings of HG sessions showed above average fidelity (joining; M = 4.13, SD = 0.68; promoting cohesiveness, M = 3.31, SD = 1.01; acting as a switchboard, M = 4.86, SD = 0.39; wrapping-up, M = 3.17, SD = 1.38; topic coverage, M = 4.20, SD = 0.61; Feaster et al., 2010a).
Interventionists
In HG, facilitators were one African American female certified addiction counselor and one Hispanic female master's level social worker with 9.6 (SD = 7.2) years experience. In SET, therapists were two African American women and one Hispanic woman; all were master's level social workers with 12.0 (SD = 14.0) years experience. Interventionists were aware of the study aims for the parent trial (relapse prevention and improving medication adherence for the HIV+ woman) but were not aware of any aims related to the current sub-group analyses.
Procedure
Participants were assessed at baseline and 4-months, 8-months, and 12-months post-baseline. Aside from the demographics measure, all measures were administered at baseline and all follow-ups. Both the randomized trial and the family mechanisms studies were approved by the university Institutional Review Board; all mothers gave informed consent and permission for their children to participate and children gave assent. Participants received $40 at baseline, $55 at 4 months, $75 at 8 months, and $100 at 12 months. Women could receive up to $120 for full participation in either condition. Figure 1 shows participant flow through the study.
Figure 1.
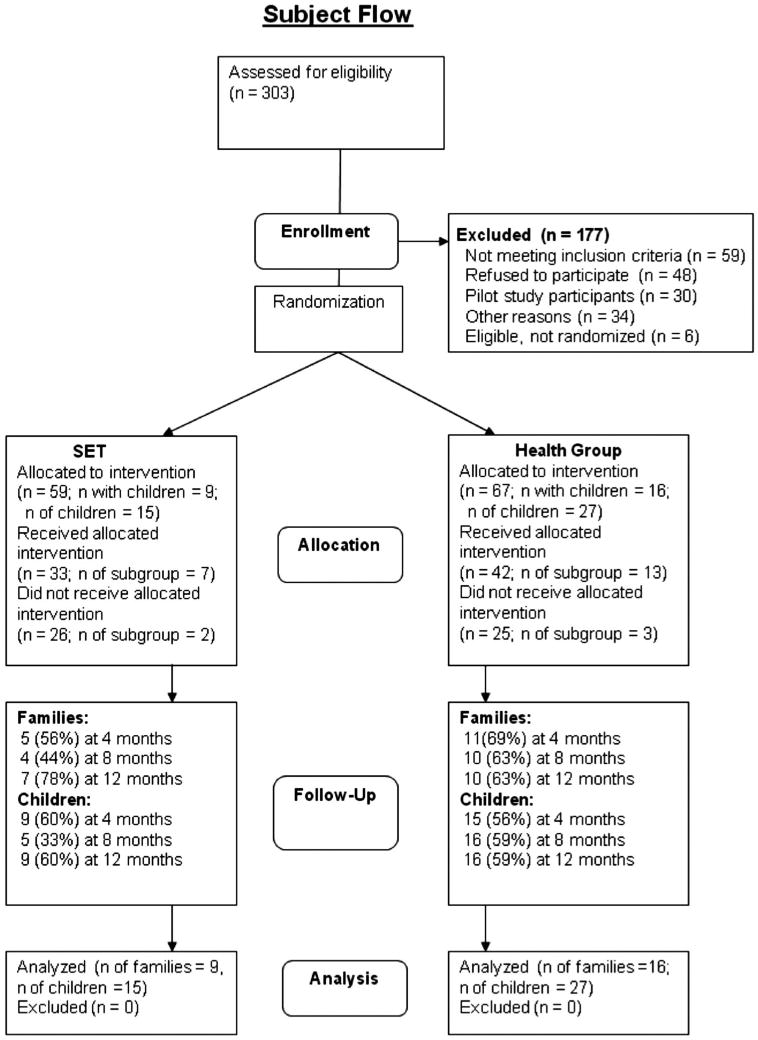
CONSORT Subject Flow Diagram.
Measures
Children's internalizing and externalizing behaviors
On the Youth Self-Report (YSR; Achenbach & Rescorla, 2001) children between 11 and 18 years rated their behavior (0 = not true, 1 = somewhat/sometimes true, 2 = very/often true). The rule-breaking and aggressive behavior subscales were combined into an externalizing scale. The anxious/depressed, withdrawn/depressed, and somatic complaints subscales were combined into an internalizing scale. Children in 19 families completed the YSR; two cases were missing data and the remaining children were under 11 years. Reliability was good (internalizing, α = .86; externalizing, α = .84). On the Revised Behavior Problems Checklist (Quay & Peterson, 1987) mothers rated problem behaviors (0 = No problem; 1 = mild; 2 = severe) for children between 6 and 18 years. The conduct disorder, socialized aggression, and attention problems subscales were combined into an externalizing scale. The anxiety-withdrawal subscale alone served as a measure of internalizing. In the current sample mothers in 23 families rated children's behaviors; two cases were missing data. Reliability was good for externalizing (α = .95) and internalizing (α = .81). All scales were converted into T-scores for analysis.
Mothers' psychological distress and drug use
The Structured Interview Guide for the Hamilton Anxiety and Depression Subscales (SIGH-AD; Williams, 1988) is a semi-structured interview that measures symptoms of anxiety and depression in the past 7 days. All 25 mothers completed this measure; reliability was good (α = .80, depression; α = .88, anxiety). Due to high correlation, r = .91, p < .001, these were combined into a single psychological distress composite. A qualitative urine drug toxicology screen (UDS) for cocaine, opioids, amphetamines, sedatives/barbiturates, phencyclidine, and tetrahydrocannabinol utilizing a homogenous enzyme immunoassay technique for each substance was used to measure drug use (0 = no use, 1 = any use). The assay tests THC at a 20-ng cut-off and cocaine and metabolites are tested at a 50-ng cut-off. The probability of a false positive is below .00002. UDS data was available for all 25 mothers.
Parenting
The Parenting Practices Questionnaire (Gorman-Smith, Tolan, Zelli, & Huesmann, 1996) asked mothers to rate each child's behavior, and vice-versa, on two dimensions: positive parenting and parental involvement. Mothers and children in 21 families completed the parenting measures; none for children under 11 years. Reliability was acceptable for positive parenting (α = .68, mother-report; α = .84, child-report) and parental involvement (α = .80, mother-report; α = .76, child-report).
Analysis Plan
Each outcome was tested in a separate Generalized Estimating Equations (GEE) analysis in SPSS 17, which allowed the inclusion of all data over time and different distributions for the outcome variables, as well as robust estimation for correlations from repeated measures over time and within the same family, i.e., multiple children of the same mother, using an AR-1 covariance structure (Diggle, Liang, & Zeger, 1994). Because children were in the same age group during the year, using T-scores was not a problem. Analyses were conducted for each of four child outcomes: children's internalizing problems, children's externalizing problems, parental involvement, and positive parenting practices, separately for mother-report and child-report; as well two mother outcomes: psychological distress and drug use. Independent variables in these models were time, treatment condition, and time × treatment. Child's age was controlled in analyses of child outcomes and parenting. Rather than employ a Bonferroni correction, we maintained alpha = .05 per test due to the small sample. In order to explore whether gender affected the results, a moderation test was done with outcomes that showed a statistically significant time × treatment effect. Effect sizes followed Cohen's (1992) guidelines: small, d = .2; medium, d = .5; large, d = .8.
Results
Children's Internalizing and Externalizing Behaviors
Summary statistics are shown for all outcomes in Table 2 and estimated trajectories for outcomes in which there were significant effects are shown in Figure 2. Hypothesis 1 stated that SET would result in improved internalizing and externalizing outcomes for children as compared to the HG control group. Results of the GEE analysis with mother-reported internalizing problems revealed a significant time × treatment interaction, B = −1.18, SE = 0.57, p < .05, 95% CI [−2.30, −0.07]. On average, there was a medium-sized decrease (d = 0.42) in mother-reported internalizing problems for children in SET, but little change in HG (d = 0.13). Similarly, for child-reported internalizing problems there was a significant time × treatment interaction, B = −1.94, SE = 0.73, p < .01, 95% CI [−3.37, −0.51]. On average, child-reported internalizing problems showed a small-to-medium-sized decrease (d = 0.36) in SET but remained generally constant in HG (d = 0.08).
Table 2. Mother and Child Outcomes at Each Assessment Point for Families Assigned to SET and HG.
| Condition and variable | Baseline | 4 Months | 8 Months | 12 Months | ||||
|---|---|---|---|---|---|---|---|---|
| M or N | SD or % | M or N | SD or % | M or N | SD or % | M or N | SD or % | |
| SET mother-report child internalizing | 53.68 | 11.20 | 49.70 | 5.15 | 52.18 | 8.95 | 44.75 | 4.11 |
| HG mother-report child internalizing | 50.49 | 8.83 | 48.38 | 8.79 | 52.53 | 10.62 | 49.23 | 12.88 |
| SET child-report child internalizing | 58.33 | 16.50 | 51.43 | 11.76 | 46.89 | 5.39 | 46.71 | 6.17 |
| HG child-report child internalizing | 47.17 | 8.86 | 46.45 | 7.64 | 45.11 | 8.27 | 46.83 | 8.68 |
| SET mother-report child externalizing | 50.86 | 7.44 | 55.58 | 10.07 | 57.76 | 17.83 | 49.20 | 7.70 |
| HG mother-report child externalizing | 53.88 | 11.56 | 50.25 | 9.36 | 57.24 | 13.80 | 52.22 | 15.19 |
| SET child-report child externalizing | 57.74 | 11.68 | 55.48 | 14.44 | 49.14 | 6.37 | 46.89 | 7.46 |
| HG child-report child externalizing | 49.50 | 8.81 | 46.59 | 7.53 | 47.38 | 7.47 | 48.21 | 10.53 |
| SET mother psy. distress | 9.33 | 9.81 | 13.67 | 12.66 | 6 | 7.38 | 1.40 | 1.67 |
| HG mother psy. distress | 12.40 | 12.67 | 8.86 | 11.11 | 6.75 | 7.34 | 10.78 | 10.57 |
| SET mother drug use | 1 | 11% | 1 | 11% | 0 | 0% | 1 | 11% |
| HG mother drug use | 3 | 19% | 4 | 25% | 3 | 19% | 5 | 31% |
| SET mother-report pos. parenting | 4.27 | 0.72 | 4.14 | 0.72 | 4.67 | 0.33 | 4.27 | 0.80 |
| HG mother-report pos. parenting | 4.33 | 0.62 | 4.64 | 0.44 | 4.39 | 0.57 | 4.36 | 0.66 |
| SET child-report pos. parenting | 4.07 | 0.92 | 4.13 | 1.07 | 4.56 | 0.51 | 4.67 | 0.37 |
| HG child-report pos. parenting | 3.78 | 1.13 | 3.95 | 1.09 | 3.83 | 1.11 | 3.50 | 0.86 |
| SET mother-report parental inv. | 4.15 | 0.74 | 4.18 | 0.61 | 4.45 | 0.48 | 4.45 | 0.41 |
| HG mother-report parental inv. | 4.46 | 0.59 | 4.39 | 0.54 | 4.48 | 0.42 | 4.22 | 0.79 |
| SET child-report parental inv. | 4.13 | 0.83 | 4.27 | 0.20 | 4.28 | 0.63 | 4.39 | 0.52 |
| HG child-report parental inv. | 3.93 | 0.86 | 4.20 | 0.65 | 4.14 | 0.40 | 4.02 | 0.60 |
Note. SET = Structural ecosystems therapy; HG = Health group; Internalizing and Externalizing are T-scores; Parental Inv. = Parental involvement; Pos. Parenting = Positive parenting; Psy. Distress = Psychological distress of the target woman. Drug use = positive urine drug screen for the target women.
Figure 2.
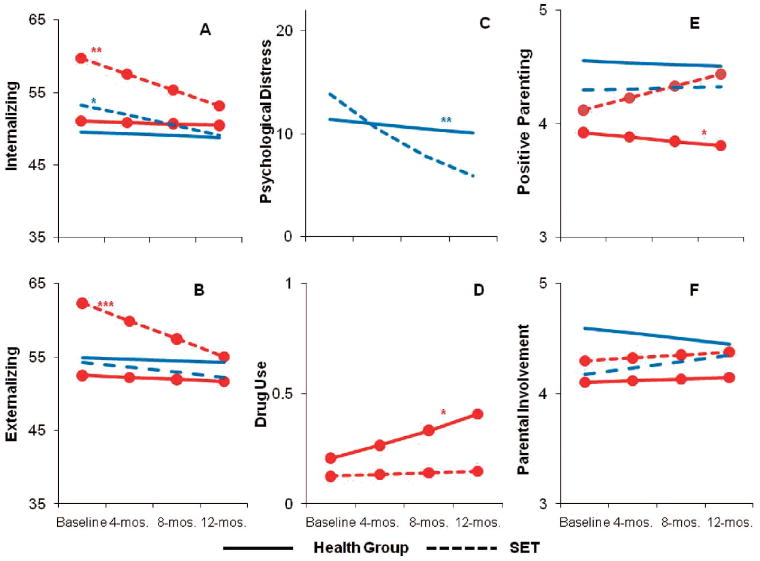
Estimated outcome trajectories for participants in SET and the Health Group across the 12-month follow-up. Child reports in red with filled circles and mother reports in plain blue lines for (A) child internalizing problems and (B) child externalizing problem; (C) mother psychological distress in plain blue lines and (D) mother drug use in red with filled circles; and child reports in red with filled circles and mother reports in plain blue lines for (E) positive parenting and (F) parental involvement. * denotes SET trajectories that are significantly different from the Health Group: * p < .05. ** p < .01. *** p < .001.
There was no significant time × treatment interaction in mother-reported externalizing problems, B = −0.45, SE = 0.66, p = .50, 95% CI [−1.74, 0.85]. However, analysis of child-reported externalizing behaviors revealed a significant time × treatment interaction, B = −2.17, SE = 0.58, p < .001, 95% CI [−3.31, −1.03]. On average, children in SET reported a large-sized decrease (d = .73) in externalizing behaviors across time, whereas children in HG reported generally stable externalizing behaviors (d = 0.08).
Child's Gender
There was no evidence for moderation of treatment effects on child-reported internalizing problems, B = 1.28, SE = 1.68, p = .45, or externalizing problems, B = −0.71, SE = 1.50, p = .64. Child's gender significantly moderated the treatment effect on mother-reported internalizing problems, B = −2.18, SE = 1.11, p < .05. Specifically, in SET the treatment effect on mother-reported internalizing problems occurred primarily for girls, not boys.
Mother's Psychological Distress and Drug Use
Hypothesis 2 stated that SET would result in improved psychological distress and drug use outcomes for mothers as compared to HG. Psychological distress was positively skewed with overdispersion, so a negative binomial distribution was used in the GEE analysis (Atkins & Gallop, 2007). Results showed a significant time × treatment interaction, B = −0.25, SE = 0.09, p < .01, 95% CI [−0.41, −0.08] on mother's psychological distress. On average, mothers assigned to SET reported a large-sized decrease (d = .78) in psychological distress over time, compared to no change for mothers in HG (d = 0.13).
Drug use had a binary distribution (use or no use), so a logistic distribution was used in the GEE analysis. Results showed a significant time × treatment interaction, B = −0.29, SE = 0.15, p < .05, 95% CI [−0.58, −0.01] on mother's drug use. This result translates to a medium-sized increase in the odds of a positive UDS over follow-up for mothers in HG (OR = 2.69, d = 0.55); mothers in SET had almost no increased risk (OR = 1.13, d = .07).
Parenting
Hypothesis 3 stated that SET would result in improved positive parenting and parental involvement for children and mothers as compared to HG. There was no significant time × treatment interaction for parent-reported positive parenting, B = 0.03, SE = 0.08, p = .75, 95% CI [−0.13, 0.18]; parent-reported parental involvement, B = 0.11, SE = 0.07, p = .14, 95% CI [−0.03, 0.25]; or child-reported parental involvement, B = 0.01, SE = 0.08, p = .86, 95% CI [−0.14, 0.17]. There was a significant time × treatment interaction, B = 0.15, SE = 0.07, p < .05, 95% CI [0.01, 0.29] on child-reported positive parenting. On average, children in SET reported small-to-medium sized increases (d = .31) in positive parenting, but children in HG showed a small decrease (d = .11).
Discussion
Women with HIV are at risk for mental health problems and drug abuse, which negatively impact their physical wellbeing and compromise their ability to fulfill key life functions. SET was developed in recognition of the central role that families play in the lives of HIV+ women, and the potential to improve the women's wellbeing by correcting problematic and stress-inducing interactions as well as facilitating supportive interactions. The majority of women with HIV are mothers who are raising children, and these children are vulnerable to mental health and behavioral problems. The purpose of this sub-sample analysis was to examine whether both mothers and children could benefit from SET.
We found that SET resulted in reduced internalizing and externalizing symptoms in the children, reduced psychological distress and drug relapse in the mothers, and increased child-reported positive parenting. Externalizing and internalizing problems are associated with serious sequellae including substance abuse (Fombonne, Wostear, Cooper, Harrington, & Rutter, 2001; McGee, Williams, Poulton, & Moffit, 2000) and suicidality (Hallfors et al., 2004; O'Donnell, O'Donnell, Wardlaw, & Stueve, 2004), underscoring the significance of the child outcomes in this study. Past research demonstrating that children of HIV+ mothers are negatively affected by maternal substance abuse (Cowgill et al., 2007; Leonard et al., 2008; Rotheram-Borus et al., 2001), positively affected by reduction in parental substance abuse (Lester et al., 2009) and negatively affected by maternal psychological distress or depression (Lester et al., 2010; Pilowsky et al., 2001) highlight the significance of the mother's outcomes in this study.
The differences in treatment effects on child vs. mother reports of internalizing, externalizing and positive parenting are consistent with prior research showing low parent-child concurrence on children's internalizing and externalizing (De Los Reyes & Kazdin, 2005) and the finding by Lester et al. (2010) that adolescents with HIV + parents reported more positive family functioning than their mothers. A post-hoc examination of the patterns of correlations of mother and child reports on the same construct (with observations collapsed across treatment conditions and time points) revealed higher correlations for externalizing (r = .20) than internalizing (r = .04), a pattern similar to that found in previous studies (De Los Reyes & Kazdin, 2005) and with comparable magnitude as found in research with non-referred children (Thompson, Merritt, Keith, Murphy, & Johndrow, 1993). The gender moderation effect on mother-reported internalizing suggests that the mothers might be more aware of their daughter's internalizing problems, and in fact there was stronger concurrence on internalizing between mothers and daughters (r = .27) than mothers and sons (r = −.27). Lester et al. (2010) posit that children of HIV+ mothers might be less self-disclosing of their problems in an attempt to protect their mothers. Our finding suggests that this might be especially true for boys.
Although we are encouraged by the study outcomes, the level of treatment utilization was suboptimal for maximizing benefits and cost-effectiveness. The rates of attendance at one or more sessions in the current sample (78%) is similar to that reported in the Rotheram-Borus et al. (2001) parent-child intervention trial (75%) but lower than those reported by Remien et al. (2005) couple's intervention trial (91%). As a single-family home-based therapy, SET is more expensive than Rotheram-Borus et al.'s (2001) group intervention and Remien's (2005), which is delivered in a clinic setting. Future work on SET should address service utilization and cost.
There are other significant limitations in the current study which warrant caution in interpreting the results. First, although this examination was described and planned prior to study inception, the small resulting sample size, which was further reduced by study attrition and the fact that some of the measures were relevant only to a subsample of the children, limited power and the ability to test mechanisms of action. Another limitation is that the children in the current study ranged widely in age. The small sample size precludes examination of age effects, although age was controlled in the analyses of child outcomes and parenting. In addition, this is a convenience sample which limits the generalizability of the findings.
Future Research
The putative mechanism of change in SET is the transformation of relationships within the family. The results of the current study partially support this theory, but we were unable to adequately test reciprocal processes and change mechanisms due to small sample size. Some important unanswered questions include whether the effects for children preceded or were subsequent to the mother's effects, whether positive parenting as perceived by the children preceded or was subsequent to reductions in mothers' effects or children's effects, and whether positive parenting or other family functioning processes mediated improvement in the children and/or mothers. The results of this study suggest that children and mothers were getting better together in response to a family intervention, which merits further research with larger samples.
Further work to adapt SET for mothers and children is warranted. The SET manual instructs therapists to address family functioning across any subsystem that the therapist deems relevant to the woman's target outcomes, including parenting if applicable, but parenting is not a required content area, nor was it a focus of training or supervision in this trial. However, when we examined the clinical contact logs we found that “children/parenting” was addressed in all of the cases with children and in 90% of the sessions. Anecdotal therapist reports indicate that women with children were more interested in addressing parenting issues than in focusing on their own health, particularly in early sessions. Because the first objective in SET is building the therapeutic alliance, therapists follow the client's lead in establishing therapeutic goals. It appears that by first engaging the women on parenting issues the therapists gained the women's trust and could then address the women's own health, including drug use, without damaging the alliance (Mitrani et al., 2009). SET therapists report that a prominent theme in some cases was strained relationships between mothers and children related to the mother's drug use. Our results indicate that the children experienced some improvement in their relationships with their mothers but the mothers did not, suggesting an area where the model might be improved. A mother-child adaptation of SET might add a required focus on parenting and parent-child relationship to be addressed in vivo and supplemented by empirically supported parenting skills modules.
Acknowledgments
This research was funded by National Institute on Drug Abuse grants R01DA16543, (Victoria B. Mitrani, Principal Investigator) and R01DA15004 (Daniel Feaster, Principal Investigator). Support for this research was also received from the Center of Excellence for Health Disparities Research: El Centro, National Center on Minority Health and Health Disparities grant P60MD002266; and The National Institutes of Health Office of Research on Women's Health and the University of Miami, General Clinical Center Research Grant M01RR16587.
Contributor Information
Victoria B. Mitrani, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami
Brian E. McCabe, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami
Carleen Robinson, Department of Psychiatry and Behavioral Sciences, Leonard M. Miller School of Medicine, University of Miami.
Nomi S. Weiss-Laxer, Center of Excellence for Health Disparities Research: El Centro, School of Nursing and Health Studies, University of Miami
Daniel J. Feaster, Department of Epidemiology and Public Health, Leonard M. Miller School of Medicine, University of Miami
References
- Achenbach TM, Rescorla LA. Manual for ASEBA school-age forms & profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Atkins DC, Gallop RJ. Rethinking how family researchers model infrequent outcomes: A tutorial on count regression and zero-inflated models. Journal of Family Psychology. 2007;21:726–735. doi: 10.1037/0893-3200.21.4.726. [DOI] [PubMed] [Google Scholar]
- Baker SA, Beadnell B, Stoner S, Morrison DM, Gordon J, Collier C, Steilstra S. Skills training versus health education to prevent STDs/HIV in heterosexual women: A randomized controlled trial utilizing biological outcomes. AIDS Education and Prevention. 2003;15:1–14. doi: 10.1521/aeap.15.1.1.23845. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=tfh&AN=9177823&site=ehost-live. [DOI] [PubMed]
- Catalano RF, Gainey RR, Fleming CB, Haggerty KP, Johnson NO. An experimental intervention with families of substance abusers: One-year follow-up of the focus on families project. Addiction. 1999;94:241–254. doi: 10.1046/j.1360-0443.1999.9422418.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10396792. [DOI] [PubMed]
- Centers for Disease Control and Prevention HIV/AIDS surveillance report, 2007:19. 2009 Retrieved from http://cdc.gov/hiv/topics/surveillance/resources/reports/2007report/pdf/2007SurveillanceReport.pdf.
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cowgill BO, Beckett MK, Corona R, Elliott MN, Zhou AJ, Schuster MA. Children of HIV-infected parents: Custody status in a nationally representative sample. Pediatrics. 2007;120:494–503. doi: 10.1542/peds.2006-3319. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Diggle P, Liang KY, Zeger SL. Analysis of longitudinal data. New York: Oxford University Press; 1994. [Google Scholar]
- Feaster DJ, Brincks AM, Mitrani VB, Prado G, Schwartz SJ, Szapocznik J. The efficacy of structural ecosystems therapy for HIV medication adherence with African American women. Journal of Family Psychology. 2010c;24:51–59. doi: 10.1037/a0017954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feaster DJ, Burns MJ, Brincks AM, Prado G, Mitrani VB, Mauer MH, Szapocznik J. Structural ecosystems therapy for HIV+ African American women and drug abuse relapse. Family Process. 2010b;49:204–219. doi: 10.1111/j.1545-5300.2010.01318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feaster DJ, Mitrani VB, Burns MJ, McCabe BE, Brincks AM, Rodriguez AE, Robbins MS. A randomized controlled trial of structural ecosystems therapy for HIV medication adherence and substance abuse relapse. Drug and Alcohol Dependence. 2010a doi: 10.1016/j.drugalcdep.2010.04.017. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M. The Maudsley long-term follow-up of child and adolescent depression. British Journal of Psychiatry. 2001;179:218–223. doi: 10.1192/bjp.179.3.218. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11532797. [DOI] [PubMed]
- Forehand R, Jones DJ, Kotchick BA, Armistead L, Morse E, Morse PS, Stock M. Noninfected children of HIV-infected mothers: A 4-year longitudinal study of child psychosocial adjustment and parenting. Behavior Therapy. 2002;33:579–600. doi: 10.1016/S0005-7894(02)80018-1. [DOI] [Google Scholar]
- Gorman-Smith D, Tolan PH, Zelli A, Huesmann LR. The relation of family functioning to violence among inner-city minority youths. Journal of Family Psychology. 1996;10:115–129. doi: 10.1037/0893-3200.10.2.115. [DOI] [Google Scholar]
- Haley J. Problem-solving therapy. 2nd. San Francisco, CA: Jossey-Bass; 1987. [Google Scholar]
- Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: Association with sex and drug behavior. American Journal of Preventative Medicine. 2004;27:224–230. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Kandel DB. Parenting styles, drug use, and children's adjustment in families of young adults. Journal of Marriage and Family Therapy. 1990;52:183–196. [Google Scholar]
- Klinkenberg WD, Sacks S, for the HIV/AIDS Treatment, Adherence, and Health Outcomes and Cost Study Group Mental disorders and drug abuse in persons living with HIV/AIDS. AIDS Care. 2004;16:S22–42. doi: 10.1080/09540120412331315303. [DOI] [PubMed] [Google Scholar]
- Knight DK, Bartholomew NG, Simpson DD. An exploratory study of “Partners in Parenting” within two substance abuse treatment programs for women. Psychological Services. 2007;4:262–276. doi: 10.1037/1541-1559.4.4.262. [DOI] [Google Scholar]
- Kotchick BA, Forehand R, Brody G, Armistead L, Morse E, Simon P, Clark L. The impact of maternal HIV infection on parenting in inner-city African American families. Journal of Family Psychology. 1997;11:447–461. [Google Scholar]
- Leonard NR, Gwadz MV, Cleland CM, Vekaria PC, Ferns B. Maternal substance use and HIV status: Adolescent risk and resilience. Journal of Adolescence. 2008;31:389–405. doi: 10.1016/j.adolescence.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester P, Stein JA, Bursch B, Rice E, Green S, Penniman T, Rotherarm-Borus MJ. Family-based processes associated with adolescent distress, substance use and risky sexual behavior in families affected by maternal HIV. Journal of Clinical Child & Adolescent Psychology. 2010;39:32–340. doi: 10.1080/15374411003691677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester PE, Weiss RE, Rice E, Comulada WS, Lord L, Alber S, Rotheram-Borus MJ. The longitudinal impact of HIV+ Parents' drug use on their adolescent children. American Journal of Orthopsychiatry. 2009;79:51–59. doi: 10.1037/a0015427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee R, Williams S, Poulton R, Moffitt T. A longitudinal study of cannabis use and mental health from adolescence to early adulthood. Addiction. 2000;95:491–503. doi: 10.1046/j.1360-0443.2000.9544912.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10829326. [DOI] [PubMed]
- Minuchin S, Fishman HC. Family therapy techniques. Cambridge, MA: Harvard University Press; 1981. [Google Scholar]
- Mitrani VB, Feaster DJ, Weiss-Laxer NS, McCabe BE. Malaise, motivation, and motherhood: Predictors of engagement in a behavioral treatment for HIV+ women in drug abuse recovery. AIDS and Behavior. 2010 doi: 10.1007/s10461-010-9714-z. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani VB, Robinson C, Szapocznik J. Structural Ecosystems Therapy (SET) for women with HIV/AIDS. In: Stanton M, Bray J, editors. Handbook of Family Psychology. West Sussex, UK: Blackwell Publishing; 2009. [Google Scholar]
- O'Donnell L, O'Donnell C, Wardlaw DM, Stueve A. Risk and resiliency factors influencing suicidality among urban African American and Latino youth. American Journal of Community Psychology. 2004;33:37–49. doi: 10.1023/B:AJCP.0000014317.20704.0b. [DOI] [PubMed] [Google Scholar]
- Pequegnat W, Szapocznik J. The role of families in preventing and adapting to HIV/AIDS: Issues and answers. In: Pequegnat W, Szapocznik J, editors. Working with families in the era of HIV/AIDS. Thousand Oaks, California: Sage Publications; 2002. pp. 3–26. [Google Scholar]
- Pilowsky DJ, Lyles CM, Cross SI, Celentano D, Nelson KE, Vlahov D. Characteristics of injection drug using parents who retain their children. Drug and Alcohol Dependence. 2001;61:113–122. doi: 10.1016/s0376-8716(00)00130-7. Retrieved from www.elsevier.com:locate:drugalcdep. [DOI] [PubMed]
- Quay HC, Peterson DR. Manual for the Revised Behavioral Problem Checklist. University of Miami, Department of Psychology; 1987. Unpublished manuscript. [Google Scholar]
- Remien RH, Exner T, Kertzner RM, Ehrhardt AA, Rotheram-Borus MJ, Johnson MO, Kelly JA, of the NIMH Healthy Living Project Trial Group Depressive symptomatology among HIV-positive women in the era of HAART: A stress and coping model. American Journal of Community Psychology. 2006;38:275–285. doi: 10.1007/s10464-006-9083. [DOI] [PubMed] [Google Scholar]
- Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, Jung TM. Couple-focused support to improve HIV medication adherence: A randomized controlled trial. AIDS. 2005;19:807–814. doi: 10.1097/01.aids.0000168975.44219.45. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15867495. [DOI] [PubMed]
- Rotheram-Borus MJ, Flannery D, Rice E, Lester P. Families living with HIV. AIDS Care. 2005;17:978–987. doi: 10.1080/09540120500101690. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16176894. [DOI] [PubMed]
- Rotheram-Borus MJ, Lee M, Leonard N, Lin Y, Franzke L, Turner E, Gwadz M. Four-year behavioral outcomes of an intervention for parents living with HIV and their adolescent children. AIDS. 2003;17:1217–1225. doi: 10.1097/01.aids.0000060337.12269.1d. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Lee M, Lin Y, Lester P. Six-year intervention outcomes for adolescent children of parents with the human immunodeficiency virus. Archives of Pediatric Adolescent Medicine. 2004;158:742–748. doi: 10.1001/archpedi.158.8.742. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15289245. [DOI] [PubMed]
- Rotheram-Borus MJ, Lee MB, Gwadz M, Draimin B. An intervention for parents with AIDS and their adolescent children. American Journal of Public Health. 2001;91:1294–1302. doi: 10.2105/ajph.91.8.1294. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446764/ [DOI] [PMC free article] [PubMed]
- Rotheram-Borus MJ, Stein JA. Problem behavior of adolescents whose parents are living with AIDS. American Journal of Orthopsychiatry. 1999;69:228–239. doi: 10.1037/h0080424. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10234388. [DOI] [PubMed]
- Schuster MA, Kanouse D, Morton S, Bozzette SA, Miu A, Scott GB, Shapiro MF. HIV-infected parents and their children in the United States. American Journal of Public Health. 2000;90:1074–1081. doi: 10.2105/ajph.90.7.1074. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10897185. [DOI] [PMC free article] [PubMed]
- Simoni JM, Ng MT. Trauma, coping, and depression among women with HIV/AIDS in New York City. AIDS Care. 2000;12:567–580. doi: 10.1080/095401200750003752. Retrieved from http://www.ncbi.nlm.nih.gov/sites/pubmed. [DOI] [PubMed]
- Stanger C, Kamon J, Dumenci L, Higgins ST, Bickel WK, Grabowski J, LeslieAmass L. Predictors of internalizing and externalizing problems among children ofcocaine and opiate dependent parents. Drug and Alcohol Dependence. 2002;66:199–212. doi: 10.1016/s0376-8716(01)00201-0. Retrieved from www.elsevier.com/locate/drugalcdep. [DOI] [PubMed]
- Szapocznik J, Feaster DJ, Mitrani VB, Prado G, Smith L, Robinson-Batista C, Robbins MS. Structural ecosystems therapy for HIV-seropositive African American women: Effects on psychological distress, family hassles, and family support. Journal of Consulting and Clinical Psychology. 2004;72:288–303. doi: 10.1037/0022-006X.72.2.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szapocznik J, Kurtines WM. Breakthroughs in family therapy with drug-abusing and problem youth. New York, NY: Springer; 1989. [Google Scholar]
- Thompson RJ, Merritt KA, Keith BR, Murphy LB, Johndrow DA. Mother-child agreement on the child assessment schedule with nonreferred children: A research note. Journal of Child Psychology and Psychiatry. 1993;34:813–820. doi: 10.1111/j.1469-7610.1993.tb01073.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8340447. [DOI] [PubMed]
- Tompkins TL, Wyatt GE. Child psychosocial adjustment and parenting in families affected by maternal HIV/AIDS. Journal of Child and Family Studies. 2008;17:823–838. doi: 10.1007/s10826-008-9192-3. [DOI] [Google Scholar]
- Williams J. Structured Interview Guide for the Hamilton Depression and Anxiety Scales (SIGH-AD) New York, NY: New York State Psychiatric Institute; 1998. [Google Scholar]


