Tuft cells represent a fourth type of intestinal secretory cell that constitutes the primary source of endogenous intestinal opioids and are the only epithelial cell that constitutively express cyclooxygenases.
Abstract
The unique morphology of tuft cells was first revealed by electron microscopy analyses in several endoderm-derived epithelia. Here, we explore the relationship of these cells with the other cell types of the intestinal epithelium and describe the first marker signature allowing their unambiguous identification. We demonstrate that although mature tuft cells express DCLK1, a putative marker of quiescent stem cells, they are post-mitotic, short lived, derive from Lgr5-expressing epithelial stem cells, and are found in mouse and human tumors. We show that whereas the ATOH1/MATH1 transcription factor is essential for their differentiation, Neurog3, SOX9, GFI1, and SPDEF are dispensable, which distinguishes these cells from enteroendocrine, Paneth, and goblet cells, and raises from three to four the number of secretory cell types in the intestinal epithelium. Moreover, we show that tuft cells are the main source of endogenous intestinal opioids and are the only epithelial cells that express cyclooxygenase enzymes, suggesting important roles for these cells in the intestinal epithelium physiopathology.
Introduction
The intestinal epithelium is a highly dynamic tissue with continuous proliferation, migration, differentiation, and apoptosis, resulting in complete renewal every 2–7 d, in a spatially and temporally organized manner. This process is coordinated by a small number of highly conserved signaling pathways (Sancho et al., 2004). While migrating toward the villi, progenitor cells differentiate into distinct cell types that can be identified using morphological criteria and through expression of specific genes. Differentiated epithelial cells belong to two classes: absorptive enterocytes and secretory cells. Secretory cells can be further subdivided into three cell types: mucus-producing goblet cells, hormone-secreting enteroendocrine cells, and bactericidal Paneth cells.
The composition of the villus epithelium mainly results from the interaction of signaling pathways that are active in crypt stem and progenitor cells. The most studied examples are the Wingless-related MMTV integration site (Wnt) and Notch pathways. Inhibition of the Wnt signaling pathway induces a complete loss of crypt epithelial progenitors (Korinek et al., 1998; Pinto et al., 2003). Genetic and pharmacologic inhibition of the Notch pathway drives the cells toward a secretory fate, even though the Wnt cascade remains active (Fre et al., 2005; van Es et al., 2005b) and, accordingly, deletion of the Notch effector hairy/enhancer of split 1 (Hes1) results in the generation of excessive numbers of goblet, enteroendocrine, and Paneth cells (Jensen et al., 2000; Suzuki et al., 2005). Conversely, the basic-helix-loop-helix transcription factor encoded by the Atonal homologue 1 gene (Atoh1, also called Math1), which is repressed by the HES1 transcription factor, is required for a progenitor cell to adopt a secretory fate (Yang et al., 2001; Shroyer et al., 2007; van Es et al., 2010). It is often thought that a single Atoh1-dependent secretory progenitor exists for all three secretory cell types. However, some data instead point toward the existence of several bi-potential progenitors that can each produce either an enterocyte or a secretory cell belonging to the goblet, enteroendocrine, or Paneth cell type, a fate choice that likely relies on Notch signaling (Bjerknes and Cheng, 1999). In addition to ATOH1, a set of transcription factors determines the cell fate choice and differentiation toward goblet, Paneth, or enteroendocrine cell types. Neurogenin 3 (Neurog3, also called Ngn3) is essential for all intestinal enteroendocrine cells (Jenny et al., 2002; Mellitzer et al., 2010) and has been reported to be repressed by the growth factor-independent 1 (GFI1) transcription factor, which is normally expressed in both Paneth and goblet cells (Bjerknes and Cheng, 2010). Deletion of the Gfi1 gene, in turn, results in an increased enteroendocrine cell population at the expense of Paneth and goblet cells (Shroyer et al., 2005), likely due to cellular reprogramming of Paneth and goblet cells toward a Neurog3+ enteroendocrine cell phenotype (Bjerknes and Cheng, 2010). The Kruppel-like factor 4 (Klf4) and SAM pointed domain containing Ets transcription factor (Spdef) genes are required for terminal differentiation of goblet cells (Katz et al., 2002). Spdef is necessary for Paneth cell maturation (Gregorieff et al., 2009), and differentiation is shifted toward the goblet cell type, at the expense of the absorptive as well as Paneth and enteroendocrine cell types in the intestinal epithelium of transgenic animals overexpressing Spdef (Noah et al., 2010). Finally, the SRY-box containing gene 9 (Sox9) is essential for differentiation of Paneth cells (Bastide et al., 2007; Mori-Akiyama et al., 2007), and Wnt signaling through the Frizzled-5 receptor is required for their terminal maturation (van Es et al., 2005a).
The permanent turnover of the intestinal epithelium relies on the self-renewing capacity of stem cells. The Wnt target gene Leucine-rich repeat containing G protein–coupled receptor 5 (Lgr5) has been identified as a marker of crypt base columnar (CBC) cells (Barker et al., 2007). Genetic lineage-tracing experiments revealed that CBC cells are multipotent and self-renewing, thus representing genuine intestinal stem cells (Bjerknes and Cheng, 1999; Barker et al., 2007). In addition, cells located above the Paneth cell compartment (also known as the +4 position) and expressing the Bmi1 polycomb ring finger oncogene (Bmi1) have been reported to have features of stem cells (Sangiorgi and Capecchi, 2008). However, the presence of these cells is limited to the duodenum, and recent studies showed that Bmi1 expression is, at least partially, overlapping with Lgr5 expression (van der Flier et al., 2009). Both Lgr5+ and Bmi1+ cells are actively cycling, and the presence of a long-lived quiescent stem cell population in the intestinal epithelium is still a matter of debate. For instance, we have recently demonstrated that the solitary cells expressing the doublecortin-like kinase 1 protein (DCLK1, also called DCAMKL1), which have been considered as putative quiescent stem cells (Giannakis et al., 2006; May et al., 2008, 2009; Dekaney et al., 2009; Jin et al., 2009; Sureban et al., 2009), are bona fide tuft cells (Gerbe et al., 2009). Since their first identification in the rat trachea (Rhodin and Dalhamn, 1956) and mouse gastrointestinal tract (Jarvi and Keyrilainen, 1956), tuft cells (also known as brush cells) have been found in several endoderm-derived epithelia. These cells are characterized by long and blunt microvilli with prominent rootlets, and by a well-developed tubulovesicular system in the supranuclear cytoplasm (Sato, 2007). Several markers have been proposed for tuft cells, including villin, fimbrin (Höfer and Drenckhahn, 1992), neuronal nitric oxyde synthase (Kugler et al., 1994), α-gustducin (Höfer et al., 1996), Ulex europaeus lectin 1 (Gebhard and Gebert, 1999; Gebert et al., 2000), Cytokeratin 18 (Höfer and Drenckhahn, 1996), and the transient receptor potential cation channel, subfamily M, member 5 (TRPM5; Bezençon et al., 2007). However, due to their ubiquitous expression in the intestinal epithelium, villin and fimbrin are not very suitable markers of intestinal tuft cells (Höfer and Drenckhahn, 1996). Similarly, α-gustducin, Trpm5, and Ulex europaeus lectin 1 expression have also been reported in subtypes of enteroendocrine cells (Jang et al., 2007; Sutherland et al., 2007; Bezençon et al., 2008; Kokrashvili et al., 2009). Finally, the high neuronal nitric oxyde synthase expression reported for stomachal and pancreatic tuft cells (Kugler et al., 1994) is not a property of intestinal tuft cells (Sutherland et al., 2007), and the validity of Cytokeratin 18 as a marker for mouse intestinal tuft cells is controversial (Gebert et al., 2000). Thus, none of the above markers is strictly tuft cell specific and, more than 50 years after their initial discovery, functional studies of tuft cells are still nonexistent. Here, we report a marker signature that allows unambiguous identification of mouse and human tuft cells, both in the small and large intestines. We extend our previous study to demonstrate that DCLK1-expressing tuft cells are short lived, post-mitotic cells that are permanently generated from Lgr5-expressing stem cells. Furthermore, unlike what is commonly thought, we show that tuft cells do not belong to the enteroendocrine lineage, but rather constitute a distinct entity with transcription factor requirements for differentiation that differ from those of enterocytes, enteroendocrine, Paneth, and goblet cells.
Results
A set of molecular markers allows unambiguous identification of tuft cells in the mouse intestinal epithelium
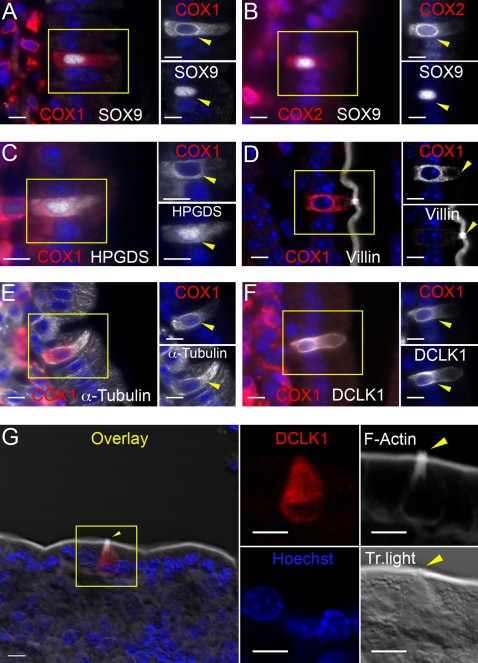
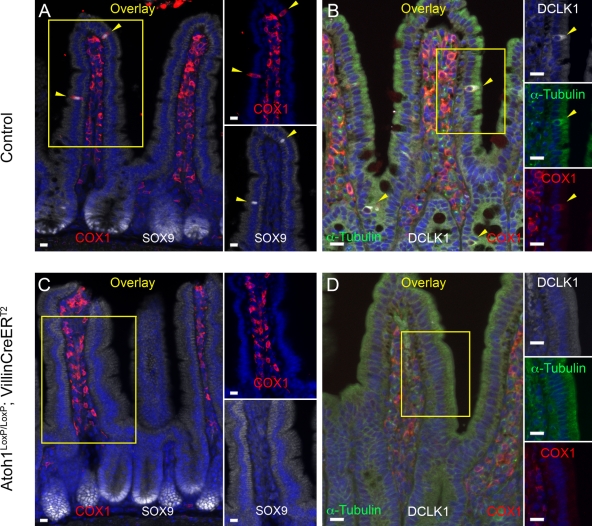
Trpm5-expressing cells, hypothesized to be tuft cells, were previously shown to express the cyclooxygenase 1 and 2 (COX1 and COX2) enzymes (Bezençon et al., 2008), and we recently found that expression of the DCLK1 protein is a specific marker of tuft cells (Gerbe et al., 2009). We have now extended these observations with multiple costaining experiments of the mouse small intestinal epithelium, based on previously published micro-array data (Bezençon et al., 2008). This allows us to identify a unique marker signature of tuft cells, which includes coexpression of SOX9, COX1, COX2, hematopoietic prostaglandin-D synthase (HPGDS), and DCLK1 (Fig. 1, A–C and F). Compared with other epithelial cells, cells displaying this signature show a stronger immunoreactivity toward villin, α-tubulin and F-actin, which is a typical feature of tuft cells (Höfer and Drenckhahn, 1996; Fig. 1, D, E, and G). The SOX9–COX1 or the HPGDS–COX1 limited signature allowed unambiguous identification of tuft cells in the mouse and human colon, as well as in other epithelia such as in the mouse gall bladder (Fig. S1, A–C).
Figure 1.
Molecular characterization of mouse intestinal tuft cells. Immunofluorescent stainings for (A) SOX9 and COX1, (B) SOX9 and COX2, (C) HPGDS and COX1, (D) villin and COX1, (E) α-tubulin and COX1, and (F) DCLK1 and COX1. Each panel contains a merged image on the left, and gray level pictures of the indicated individual markers corresponding to the yellow inset area on the right. (G) Whole-mount immunofluorescent staining for DCLK1 and F-actin on a dissociated fragment of intestinal epithelium. Panels on the right show higher magnification of the cropped area of the overlay image. Yellow arrowheads point at tuft cells. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
All DCLK1+ cells are post mitotic tuft cells
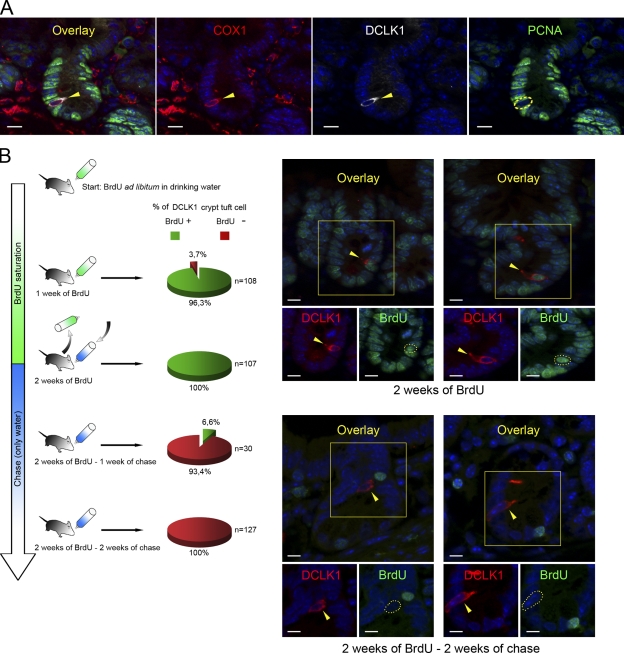
Because DCLK1-expressing cells lack differentiation markers typical of the other intestinal epithelial cells, and do not proliferate, DCLK1 has been considered as a marker of putative quiescent intestinal epithelial stem cells (Giannakis et al., 2006; May et al., 2008, 2009; Dekaney et al., 2009; Jin et al., 2009; Sureban et al., 2009). We previously reported, like others (Giannakis et al., 2006; May et al., 2009), that DCLK1+ cells are never observed in a proliferative state. We further confirm this using the proliferating cell nuclear antigen (PCNA; Fig. 2 A), and Ki67 or phospho-histone H3 (Fig. S1 D) as proliferation markers (n > 200 cells). Furthermore, DCLK1-expressing cells express typical tuft cell markers (Gerbe et al., 2009). Yet, the possibility existed that we had overlooked a second, nontuft fraction of DCLK1+ cells, which might represent quiescent stem cells. To clarify this important point we first compared the level of DCLK1 expression with that of other tuft cell markers and found that 98.1% of DCLK1+ cells were COX1+ (n = 253), the rare DCLK1+ COX1− cells being mainly found in the lower half of the crypts. To further characterize these DCLK1+ COX1− cells present in crypt bottoms, we exploited one of the unique morphological features of tuft cells that is not found in other epithelial cells: the axial bundles of actin filaments supporting the microvilli (Höfer and Drenckhahn, 1998), which can be visualized with phalloidin. An intense, apical staining of F-actin with phalloidin was found in 100% of DCLK1+ tuft cells present in crypt bottoms (n = 74). In addition, we found that SOX9 expression is higher in tuft cells present in crypt bottoms than in Paneth or CBC stem cells. This demonstrates that although COX1 is barely detectable in differentiating tuft cells, strong SOX9 expression or the pattern of actin filaments unambiguously identify all DCLK1-expressing cells as tuft cells.
Figure 2.
DCLK1-expressing tuft cells are post-mitotic and continuously renewed. (A) Immunofluorescent staining for COX1, DCLK1, PCNA, and Hoechst. The PCNA− nucleus of a tuft cell is highlighted by a yellow dotted circle. (B) Experimental scheme of the BrdU birth dating experiment. Relative proportion and number of crypt DCLK1-expressing cells positive for BrdU are indicated. Two representative immunofluorescent stainings for DCLK1 and BrdU are shown for the indicated time point. Nuclei are stained with Hoechst (blue). Yellow dotted circles highlight tuft cell nuclei.
DCLK1+ tuft cells are postmitotic and undergo permanent turnover fueled by Lgr5-expressing CBC stem cells
If all DCLK1-expressing cells are indeed differentiated cells, we would expect them to have a turnover rate similar to that of the other cell types of the intestinal epithelium, and, like other intestinal epithelial cell types, they should originate from Lgr5+ CBC stem cells. To measure their turnover rate, we birth-dated the DCLK1+ tuft cell population with BrdU. Wild-type C57BL/6 mice were treated with BrdU in drinking water for 1 or 2 wk. After 1 wk of BrdU treatment, we found that 96% DCLK1+ crypt tuft cells were BrdU+. This proportion reached 100% after 2 wk of BrdU treatment (Fig. 2 B). After 2 wk of BrdU treatment, 93% and 100% of tuft cells were BrdU− after 1 and 2 wk of chase with normal drinking water, respectively (Fig. 2 B). Therefore, DCLK1+ tuft cells are not quiescent stem cells but instead are postmitotic, short-lived differentiated cells, and their turnover time is close to 7 d.
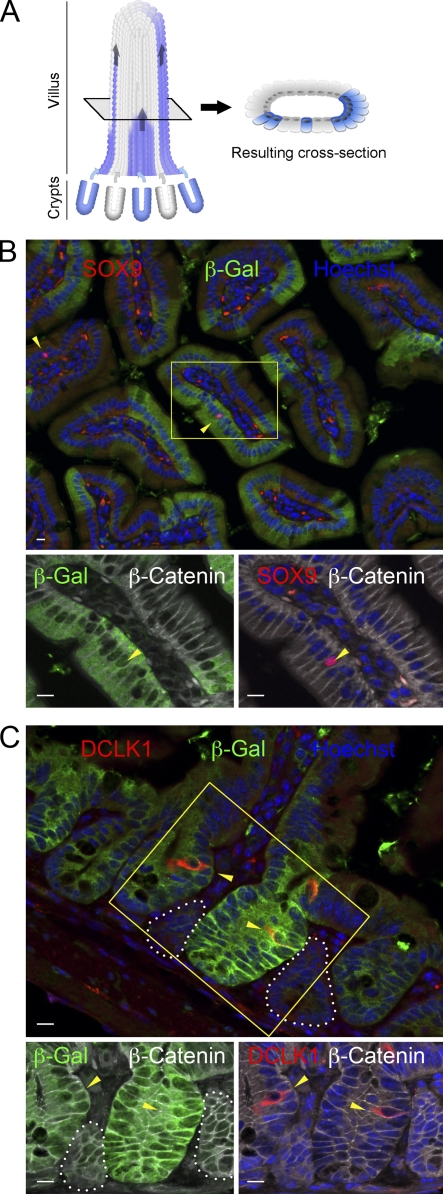
We then performed a lineage tracing experiment using the Lgr5-EGFP-IRES-CreERT2;Rosa26-LacZ compound knock-in mouse line, in which the expression of the LacZ reporter gene is prevented by a stop cassette flanked by LoxP sequences (Barker et al., 2007). Upon tamoxifen injection, CRE activity is induced in Lgr5+ stem cells and the stop cassette is excised, leading to permanent LacZ expression in the progeny of recombined Lgr5-expressing CBC stem cells. Of note, the intrinsically mosaic Cre expression in intestinal crypts of Lgr5-EGFP-IRES-CreERT2;Rosa26-LacZ mice results in a mosaic pattern of β-galactosidase in the corresponding villi (Fig. 3 A). If tuft cells originate from Lgr5-expressing stem cells, we would expect that the proportion of total β-galacosidase+ epithelial cells is identical to that of β-galactosidase+ tuft cells. When we quantified this, we found 53 β-galacosidase+ tuft cells out of 10,650 β-galactosidase+ epithelial cells (0.49%), and 51 β-galacosidase− tuft cells out of 14,340 β-galacosidase− epithelial cells (0.35%). The difference between the two values was not significant (P = 0.23), and both values were close to the representation of tuft cells in wild-type intestinal tissue sections (0.4%; see Fig. S2 A). In addition, tuft cells located within a stretch of β-galacosidase+ epithelial cells were invariably β-galacosidase+, as shown with SOX9 (Fig. 3 B) and DCLK1 (Fig. 3 C) stainings. This demonstrates that, like the four established differentiated cytotypes of the intestinal epithelium, tuft cells derive from Lgr5-expressing intestinal crypt base columnar stem cells.
Figure 3.
Tuft cells derive from Lgr5+ CBC stem cells. (A) Scheme explaining how chimeric Cre expression in crypts results in heterogeneous β-galactosidase staining in the adjacent villi (several crypts contribute to the generation of the cells constituting each villus). Wild-type (gray) and β-galactosidase (blue) cells coming from un-recombined (gray) and recombined (blue) crypts can migrate and colonize the same villus. The resulting cross section is shown. (B) Immunofluorescent staining for SOX9, β-galactosidase, β-catenin, and Hoechst in the Lgr5-EGFP-IRES-creERT2; Rosa26-LacZ mouse. Arrowheads point at SOX9+ tuft cells. The inset shows higher magnification of a SOX9+ tuft cells nucleus within a stretch of β-galactosidase+ cells. (C) Immunofluorescent staining for DCLK1, β-galactosidase, β-catenin, and Hoechst in intestinal sections from the Lgr5-EGFP-IRES-creERT2; Rosa26-LacZ mouse line. Arrowheads point at DCLK1+ tuft cells. The inset shows higher magnification of two DCLK1+ tuft cells within β-galactosidase+ crypts. β-galactosidase- crypts are shown by white dotted lines. Bars, 10 µm.
Differentiated tuft cells appear postnatally
The first tuft cells appear around d 7 after birth and become readily detectable a week later (Fig. 4). In adult mice, tuft cells are scattered throughout the crypt and villus epithelium, and represent ∼0.4% of all epithelial cells (Fig. S2 A). In adult animals, representation of the tuft cell population is similar throughout the entire length of the small and large intestines (Fig. S2 B). Except for SOX9, also expressed in Paneth cells, tuft cells do not share expression of other markers with enterocytes, goblet, or enteroendocrine cells (Fig. S3), suggesting that they constitute a distinct differentiated cell type.
Figure 4.
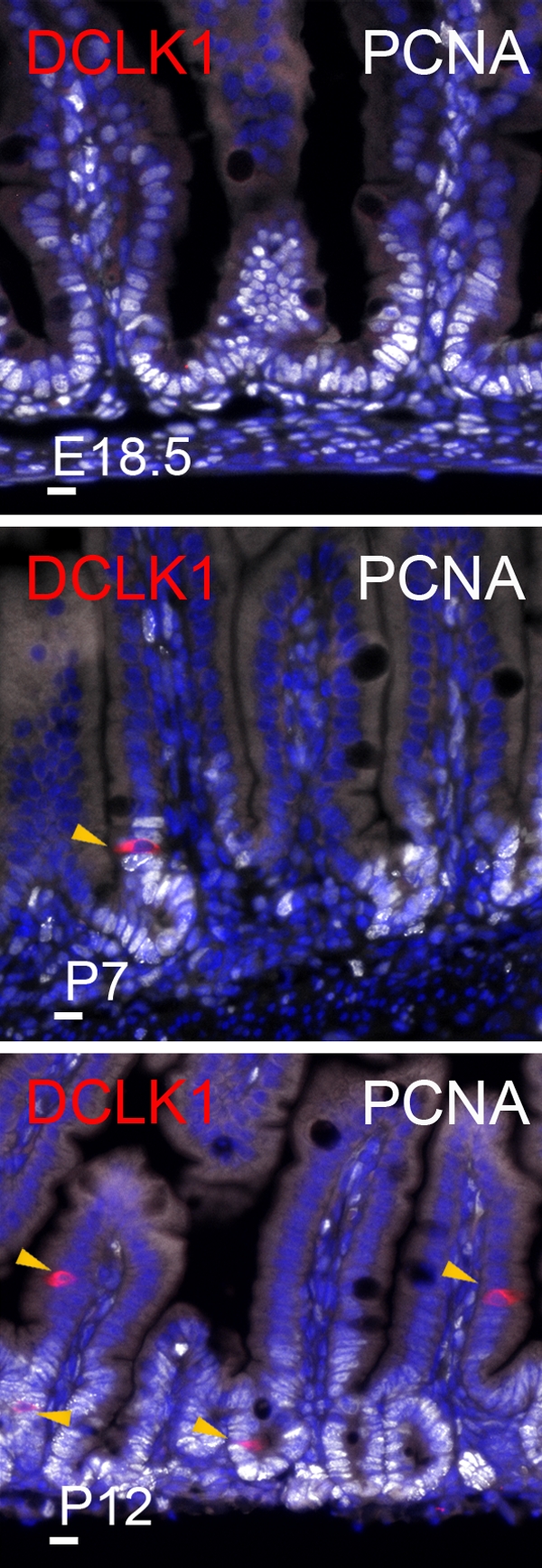
Tuft cells appear after birth. Immunofluorescent staining for DCLK1 and PCNA in the developing small intestine of E18.5, P7, and P12 mice. Arrowheads point at DCLK1-expressing tuft cells. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
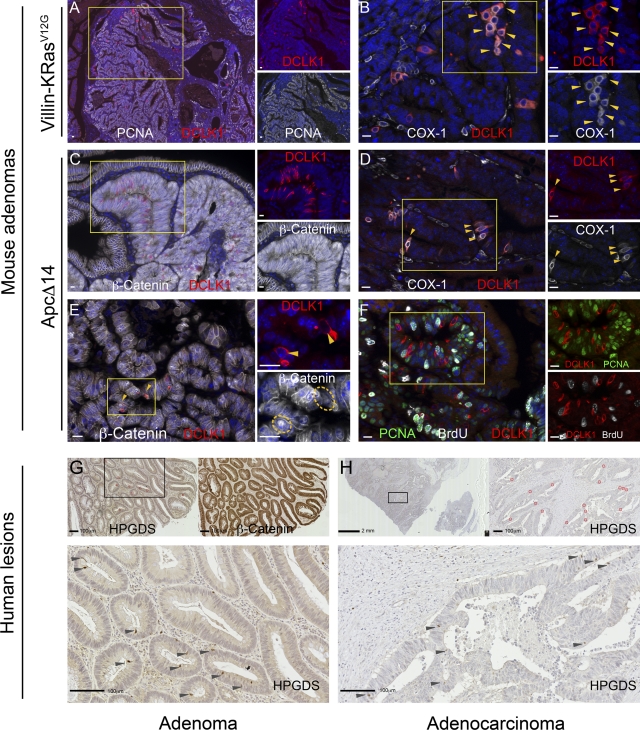
Presence of cells expressing tuft cell differentiation markers in intestinal tumors
Because tuft cells are the only epithelial cells expressing the COX1 and COX2 enzymes in the healthy intestinal epithelium, and these enzymes are strongly linked to intestinal tumorigenesis (Wang and Dubois, 2010), we analyzed the status of tuft cells in mouse small intestinal and colon tumors originating from two different oncogenic initiating events. Surprisingly, tuft cells could still be identified in the transformed lesions of mice carrying a k-RasV12G activating mutation (Janssen et al., 2002; Fig. 5, A and B) or a mutation in the Adenomatosis polyposis coli (Apc) tumor suppressor gene (Colnot et al., 2004; Fig. 5, C–F). In both cases, tuft cells invariably stained negative for expression of proliferation markers such as PCNA and did not incorporate BrdU (Fig. 5 F). In human lesions, tuft cells were also found in adenomas (Fig. 5 G), but rarely in adenocarcinoma (Fig. 5 H). This indicates that the tuft cell differentiation pathway is remarkably conserved in early tumor tissue, but not in their more malignant counterpart, raising the question of the potential role played by tuft cells during tumorigenesis.
Figure 5.
Tuft cells are found in mouse and human intestinal tumors. Immunofluorescent staining for tuft cells in K-RasV12G mouse adenoma (A and B); ApcΔ14 mouse adenoma (C–F), human adenoma (G), and human adenocarcinoma (H). Large fields (A and C) show clusters of tuft cells within the lesions. The lesion is delimited by PCNA (A) or β-catenin staining (C). DCLK1+ tuft cells coexpress the COX1 enzyme (B and D), show nuclear translocation of β-catenin (E), and are not in a proliferative state (F). Using HPGDS staining, tuft cells can also be detected in human adenomas (G) and, in rare cases, in restricted areas of human adenocarcinomas (H). For fluorescent staining, overlay (left) and individual signals of the indicated markers (right) are shown. Yellow dotted circles in E highlight tuft cell nuclei. Arrowheads point at tuft cells identified by DCLK1, COX1, and HPGDS expression. Nuclei are stained with Hoechst (blue) or hematoxylin (G and H). Bars: (A–F) 10 µm; (G and H) 100 µm.
The ATOH1 transcription factor is required for tuft cell differentiation, which identifies them as secretory cells
Having shown that tuft cells are differentiated and constantly renewed, we then asked to what extent they share the differentiation pathways previously reported for enterocytes, goblet, Paneth, and enteroendocrine cells and, therefore, to what extent tuft cells are related to these four cell types. It is generally assumed that commitment toward a specific differentiated cytotype involves the choice between one of the secretory fates (goblet, Paneth, or enteroendocrine cells) and the absorptive fate (enterocyte). This early cell fate decision is controlled by ATOH1 because differentiation of all secretory cell types is impaired in Atoh1 knock-out mice, whereas differentiation of the absorptive enterocytes is unaffected (Shroyer et al., 2007). Compared with Atoh1LoxP/LoxP or Villin-CreERT2 control mice (n = 5), in which tuft cell representation is unchanged, the intestinal epithelium of tamoxifen-injected Atoh1LoxP/LoxP; Villin-CreERT2 mice (n = 5) is completely devoid of tuft cells (Fig. 6). This conclusion was based on the analysis of several markers of tuft cells, including the SOX9 transcription factor and the COX1 enzyme (Fig. 6, A and C) and the α-tubulin and DCLK1 proteins (Fig. 6, B and D), which are related to the unique morphology of tuft cells. Thus, together with goblet, Paneth, and enteroendocrine cells, tuft cells depend on Atoh1 function for their differentiation and belong to a secretory lineage of the intestinal epithelium.
Figure 6.
Atoh1 is required for tuft cell differentiation. Immunofluorescent staining for the SOX9 transcription factor (A and C), the COX1 enzyme (A–D), and for the structural- and morphological-related tuft cells markers DCLK1 and α-tubulin (B and D) in intestines from control (A and B) and Atoh1-deficient mice (C and D), 3 wk after tamoxifen injection. Each panel contains the merged image on the left, and separate pictures of the indicated markers corresponding to the yellow inset on the right. Yellow arrowheads point at tuft cells revealed by SOX9 and COX1 or DCLK1, α-tubulin, and COX1 expression. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
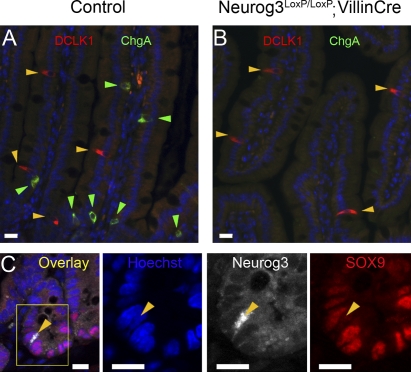
Distinct genetic requirements for differentiation between tuft and enteroendocrine cells
Tuft cells have recently been proposed to represent a subset of enteroendocrine cells (Formeister et al., 2009; Kokrashvili et al., 2009). To test this possibility, we checked whether Neurog3, a transcription factor essential for all enteroendocrine subtypes (Jenny et al., 2002; Mellitzer et al., 2010), is also required for tuft cells. We analyzed the tuft cell population in the intestinal epithelium of Neurog3LoxP/LoxP; Villin-Cre mice (n = 4), in which the Neurog3 gene is constitutively deleted at mid-gestation in all intestinal epithelial cells, and in control Neurog3LoxP/LoxP mice (n = 4). DCLK1 and chromogranin A (ChgA) immunohistochemical staining of sections from Neurog3-deficient mice and littermate controls showed that tuft cells are still present in the absence of Neurog3, whereas no enteroendocrine cells are found (Fig. 7, A and B). This indicates that tuft and enteroendocrine cells do not share the same transcription factor requirements for differentiation.
Figure 7.
Neurog3 is dispensable for tuft cell differentiation. (A and B) Immunofluorescent staining for DCLK1 and ChgA expression in intestines from 6-mo-old control or Neurog3-deficient mice. Yellow and green arrowheads point at tuft and enteroendocrine cells, respectively. (C) Immunofluorescent staining for SOX9 and Neurog3 in wild-type mouse intestine. The arrowhead points at a Neurog3+, SOX9− cell. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
Furthermore, within the crypt progenitor cell compartment, Neurog3 expression was restricted to enteroendocrine progenitor cells, in which SOX9 is barely detectable, in contrast to tuft cells where SOX9 is highly expressed (Fig. 7 C). These data, and the lack of evidence for an endocrine function of tuft cells, lead to the conclusion that tuft cells do not represent a subset of enteroendocrine cells.
Distinct genetic requirements for differentiation between tuft and Paneth or goblet cells
Goblet and Paneth cells share some transcription factor requirements for differentiation, for instance GFI1 (Shroyer et al., 2005; Bjerknes and Cheng, 2010) and SPDEF (Gregorieff et al., 2009; Noah et al., 2010). To investigate the relationship between these two cell types and tuft cells, we first analyzed tuft cell differentiation in Gfi1-deficient mice (Shroyer et al., 2005). In such mice (n = 5), we observed the expected increased representation of Neurog3+ and/or ChgA+ cells (Fig. S4 A), at the expense of goblet and Paneth cells (Shroyer et al., 2005). As previously reported (Bjerknes and Cheng, 2010), we also observed de novo Neurog3 expression and the presence of ChgA+ granules in some Gfi1-deficient lysozyme+ Paneth cells (Fig. S4 B). In contrast, the tuft cell population was not affected and Neurog3 expression was never detected in tuft cells (n = 126) from Gfi1-deficient mice (Fig. S4, A and B). This indicates that, unlike Paneth and goblet cells, tuft cells do not require GFI1 to repress Neurog3 expression.
Second, we examined whether tuft cell differentiation requires SPDEF function. Similar numbers of tuft cells were identified after staining sections of intestine from Spdef-deficient and control mice (Fig. S4 C). This indicates that tuft cells can still differentiate in the absence of Spdef, which again distinguishes them from goblet and Paneth cells.
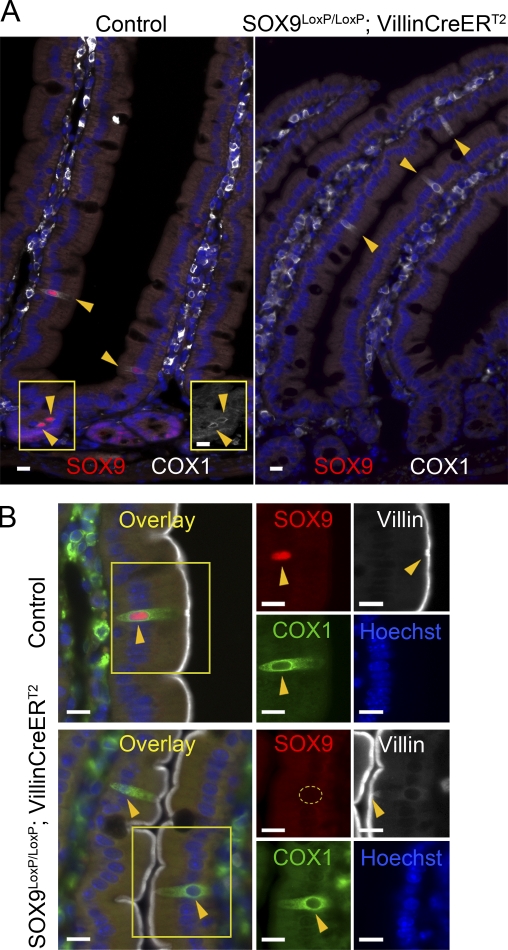
Finally, it was shown previously that the SOX9 transcription factor is expressed in terminally differentiated Paneth cells (Blache et al., 2004) and is required for their differentiation (Bastide et al., 2007; Mori-Akiyama et al., 2007). The finding that post-mitotic tuft cells also express SOX9 prompted us to test whether it is required for their differentiation. Tamoxifen was injected to induce deletion of Sox9 and the mice were analyzed after various times, ranging from 1 wk to 4 wk after induction, the latest time corresponding to at least four complete renewal cycles of the intestinal epithelium. Independently of the time left between the tamoxifen injection and the analysis, tuft cells were still present in Sox9LoxP/LoxP; Villin-CreERT2 mice (n = 2), as evidenced by COX1 staining (Fig. 8 A), and still displayed their typical villin-immunoreactive apical tuft (Fig. 8 B) and DCLK1 expression (not depicted). Thus, SOX9 is not necessary for tuft cell survival and differentiation, nor for the expression of the COX1 and DCLK1 proteins.
Figure 8.
Normal tuft cell differentiation in Sox9-deficient intestine. (A) Immunofluorescent staining for SOX9 and COX1 in intestines from control or Sox9-deficient mice, 1 mo after the first tamoxifen injection. Yellow arrowheads point at tuft cells identified by SOX9 and/or COX1 expression. The right inset shows the gray level picture of the COX1 staining, which is hardly visible in the merged image. (B) Immunofluorescent staining for SOX9, villin, and COX1 in the intestines of wild-type and Sox9-deficient mice. Each panel contains the merged image on the left, and individual fluorescent signals of the indicated markers corresponding to the yellow inset on the right. Arrowheads point at tuft cells identified by SOX9 and/or COX1 and villin expression. The tuft cell nucleus shown in the Sox9-deficient tissue is highlighted by the yellow circle. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
Taken together, these data show that most of the well-known genetic factors that control differentiation of goblet and Paneth cells are not essential for differentiation of tuft cells, which suggests that tuft cells are not closely related to either of these two cell types.
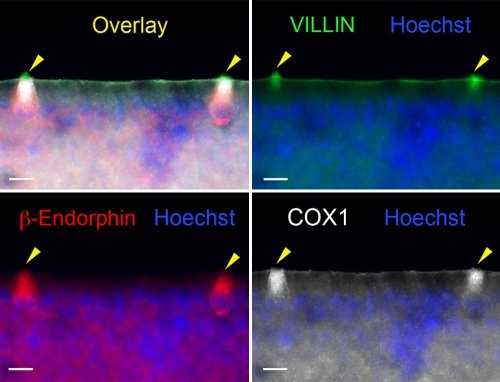
Tuft cells are responsible for opioid production by the intestinal epithelium
Endogenous opioids mediate multiple functions in the regulation of the gastrointestinal mucosa physiology, including regulation of gastric emptying, gut motility, intestinal secretion, and pain (Holzer, 2009), and their production was recently reported to rely on a subpopulation of enteroendocrine cells (Kokrashvili et al., 2009) expressing the TRPM5 ion channel, but not ChgA, a marker of most enteroendocrine cells. As tuft cells are sometimes considered as enteroendocrine cells, and Trpm5 expression has been reported in tuft cells (Bezençon et al., 2008), Kokrashvili et al. (2009) hypothesized that opioid-producing cells could be tuft cells. We tested this hypothesis using our tuft cell markers. Indeed, costaining of intestinal villi for β-endorphin, COX1, and villin expression confirmed that β-endorphin production is restricted to tuft cells (Fig. 9). Importantly, all tuft cells express β-endorphin (n = 70) in the intestinal epithelium, thus validating the first tuft cell–specific functional property identified so far.
Figure 9.
Tuft cells are responsible for opioid production by the intestinal epithelium. Whole-mount immunofluorescent staining for β-endorphin, COX1, and villin in dissociated fragments of villus epithelium. Arrowheads point at tuft cells. Nuclei are stained with Hoechst (blue). Bars, 10 µm.
Discussion
Intestinal tuft cells have long been refractory to functional analyses, and until now could only be formally identified by electron microscopic analysis. In this paper we report several molecular markers that allow unambiguous identification of tuft cells of the intestinal epithelium, as well as in other organs (see Fig. S1), thus paving the way to their characterization.
Development of tuft cells
Tuft cells can be identified by DCLK1 expression from 1 wk postnatal in the mouse intestine. This is consistent with a study in the rat stomach, in which tuft cells are detected from the weaning stage (4 wk postnatal; Iseki et al., 1991). However, it cannot be excluded that immature tuft cells that do not express differentiation markers such as DCLK1 exist at earlier stages. For instance, tuft cells have been identified in the 20-wk-old fetal human small intestine, but their DCLK1 expression status has not been analyzed (Moxey and Trier, 1978).
Early differentiation of tuft cells in crypt bottoms
In the mouse small intestine, most tuft cells are found on villi or near the crypt–villus junction, but some are present in intestinal crypts where they can be detected at virtually any position above the Paneth cell compartment. Even when localized in crypts, identifiable tuft cells are postmitotic, always express differentiation markers such as DCLK1, HPGDS, and strong SOX9 expression, have elevated F-actin immunoreactivity, and display a gradient expression of COX1 and COX2 (exemplified for COX1 in Fig. 8 A). The presence of DCLK1+, COX1low in crypt bottoms suggests that, like for the enteroendocrine cell lineage (Fig. S5 and Bjerknes and Cheng, 2006), tuft cell fate commitment may occur at an early stage, in the close vicinity of or even within the stem cell compartment.
DCLK1, quiescent stem cells, and tuft cells
The fact that crypt base–located post-mitotic tuft cells express none of the common markers of the other, best known, lineages probably explains why DCLK1-expressing cells have previously been proposed as quiescent stem cells (Giannakis et al., 2006; May et al., 2008, 2009; Dekaney et al., 2009; Jin et al., 2009; Sureban et al., 2009). However, the majority of DCLK1+ cells are found in the villi, not in the stem cell compartment. In this study we confirmed DCLK1 as a specific marker of tuft cells. This permanently renewed cell population with a high turnover rate can hardly be considered as a likely source of quiescent stem cells, at least in healthy conditions. However, self-renewing stem cells and early differentiated precursor cell populations may not be sharply and definitely distinguished during the dynamics of epithelial turnover. For instance, tracing the progeny of Neurog3-expressing cells with a LacZ reporter gene could, in some rare events, identify complete β-galactosidase+ crypt–villus axes, indicating that Neurog3-controlled Cre expression occurred in pluripotent cells of the crypt, or that Neurog3-expressing enteroendocrine precursor cells reverted to a pluripotent state (Schonhoff et al., 2004). In our case, DCLK1 expression was only detected in post-mitotic cells, but it is not possible to definitively exclude that some early tuft cells that are still in the vicinity of the stem cell niche might have the capacity to de-differentiate and revert to a stem cell phenotype under stress conditions, which could potentially explain the results found by others using in vitro culture assays (May et al., 2009).
Tuft cells represent a fourth secretory cell type of the intestinal epithelium
Although tuft cells were identified 50 years ago, they have remained poorly characterized. As a result, the relationship between tuft cells and the four other cell types of the intestinal epithelium has remained elusive, and it is currently assumed that only four main differentiated cell types constitute this epithelium. Studies on the lineage of intestinal epithelial cells are still scarce, but pioneering experiments established that multipotent Lgr5-expressing CBC stem cells (Barker et al., 2007) produce several types of intermediate bipotent or monopotent precursors from which enterocyte or goblet cells (Bjerknes and Cheng, 1999) and enteroendocrine cells (Bjerknes and Cheng, 2006) arise. In addition, multiple gene deletion studies in mouse models facilitated the decoding of transcription factor requirements for differentiation of these four cell types, but tuft cells have never been considered in such studies.
Here, we evaluated the status of tuft cells in several of these genetically engineered mouse lines. We found that tuft cells are absent in Atoh1-deficient mice, which according to the prevalent model of intestinal epithelial differentiation (van der Flier and Clevers, 2009), characterizes them as a secretory cell type. This is consistent with their capacity to produce (Fig. 9) and release opioids through an exocrine–paracrine mechanism (Kokrashvili et al., 2009). However, the fact that previous reports included tuft cells in the enteroendocrine lineage (Formeister et al., 2009; Kokrashvili et al., 2009) prompted us to investigate whether one or several differentiation pathways are shared between enteroendocrine and tuft cells. We found that in contrast to the enteroendocrine cell lineage, which strictly depends on Neurog3 function (Jenny et al., 2002; Mellitzer et al., 2010), tuft cells are still produced in the absence of Neurog3. In addition, COX1low tuft cells that are still in the process of terminal maturation express high levels of SOX9 and never express Neurog3, whereas SOX9 is barely detectable in Neurog3-expressing enteroendocrine precursor cells (Bjerknes and Cheng, 2006). Tuft cells and Ngn3-dependent enteroendocrine cells thus constitute distinct cell types. In the future, however, it is conceivable that an endocrine type of secretion is demonstrated for tuft cells. In this case, they could be considered as type 2 enteroendocrine cells, which do not require Ngn3 function for their differentiation.
Moreover, whereas differentiation of both goblet and Paneth cells is regulated by GFI1 (Shroyer et al., 2005; Bjerknes and Cheng, 2010) and SPDEF (Gregorieff et al., 2009; Noah et al., 2010), these transcription factors are not essential for tuft cells. In addition, Paneth cells require SOX9 function to differentiate (Bastide et al., 2007; Mori-Akiyama et al., 2007) but tuft cells, which express high levels of SOX9 in their terminally differentiated state, are still present in Sox9-deficient intestinal epithelium.
In summary, although tuft cells are produced from the same Lgr5+ stem cell as enterocytes, goblet, Paneth, and enteroendocrine cells, we show here that they represent an independent cell type: (i) they express a specific marker signature, and (ii) except for ATOH1, none of the transcription factors known to be required for differentiation of the other intestinal epithelial cell types and that we tested here is essential for tuft cell differentiation (Fig. 10).
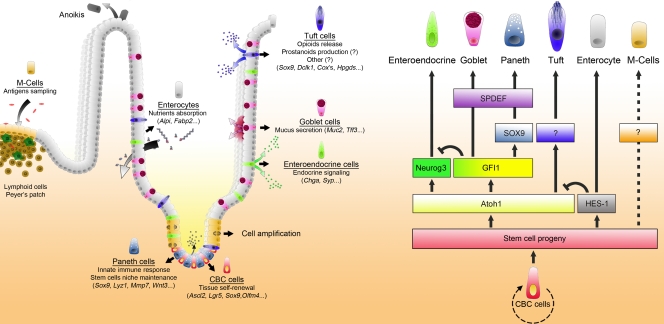
Figure 10.
Updated model for the differentiation of the intestinal epithelial cell types. The scheme on the left represents a crypt–villus unit in the adult mouse small intestinal epithelium. The main functions, including the recently discovered function of Paneth cells in maintaining the CBC stem cell population (Sato et al., 2011), and representative molecular markers identifying each of the cell types and the intestinal stem cell are indicated. Opioid secretion is known to occur in the gut lumen (blue arrows; see Kokrashvili et al., 2009). Strong evidence suggests that tuft cells can also act as an epithelial source of prostanoids (Bezençon et al., 2008 and this paper), but the underlying secretion mechanism still has to be demonstrated. The diagram on the right summarizes the genetic hierarchy of epithelial cell lineage commitment in the intestine. Intestinal CBC stem cells proliferate and produce progenitors. Choice between absorptive or secretory cell fates is under the control of the hairy/enhancer of split 1 (Hes1) or atonal homologue 1 (Atoh1) gene. Within the cells committed to secretory types, Neurog3 is required for enteroendocrine cell differentiation. Gfi1 is required for Paneth and goblet cell differentiation, preventing the expression of Neurog3. Sox9 is essential for differentiation of Paneth cells. Spdef is required for both Paneth and goblet cell terminal maturation. M-cells are known to derive from Lgr5+ CBC stem cells (Barker and Clevers, 2010), but knowledge of the molecular pathways leading to their differentiation is still missing.
Future studies will deepen the knowledge of the lineage intermediates that are shared by precursors of several differentiated cell types and refine the current understanding of the relationship between tuft cells and the other constituents of the intestinal epithelium.
Understanding the role played by tuft cells in the physiopathology of the intestinal epithelium is currently hampered by the absence of animal models specifically devoid of tuft cells. As previously suggested by gene profiling experiments in intestinal Trpm5-expressing cells (Bezençon et al., 2008), we confirm here that tuft cells are the only epithelial cells in the healthy mucosa to express the COX1 and COX2 enzymes, whose expression is rate limiting for the biosynthesis of prostanoids. Tuft cells also express Hpgds and thus represent a likely epithelial source of prostaglandin-D2. This is important given the central role played by prostanoids in mediating inflammation and tumorigenesis in the intestinal epithelium (Stenson, 2008; Wang and Dubois, 2010). Indeed, the presence of tuft cell clusters in tumors from Apc- or K-Ras–mutated mice suggests a possible contribution of tuft cells during tumorigenesis. The previous observation that siRNA-mediated inhibition of Dclk1 expression in tumor xenografts resulted in reduced tumor growth (Sureban et al., 2009) further supports this notion. Finally, we show here that tuft cells are the only intestinal epithelial cells to produce β-endorphin in healthy conditions, and thus likely contribute to the regulation of vasoconstriction, peristaltic movements, and pain in the intestine.
In conclusion, we present here molecular and genetic evidences that tuft cells constitute a genuine fifth cell type in the intestinal epithelium, as well as the first insights into functions of these cells with their production of prostanoids and opioids. Further studies will determine whether tuft cells from other endoderm-derived epithelia share similar functions.
Materials and methods
Animals: mouse strains
The Sox9LoxP/LoxP; Villin-CreERT2 strain was obtained by mating Sox9LoxP/LoxP mice (Kist et al., 2002) with Villin-CreERT2 animals (el Marjou et al., 2004). Sox9 deletion in the intestinal epithelium was induced by a single daily i.p. injection of 1 mg tamoxifen (Sigma-Aldrich) for 5 d. Mice were sacrificed 1 wk and 1 mo after the first tamoxifen injection. The ApcΔ14 (Colnot et al., 2004), Villin-K-RasV12G (Janssen et al., 2002), Neurog3LoxP/LoxP; Villin-Cre (Mellitzer et al., 2010), Gfi1−/− (Shroyer et al., 2005), and Spdef−/− (Gregorieff et al., 2009) strains have been described previously. The Lgr5-EGFP-IRES-creERT2; Rosa26-LacZ strain has been described previously (Barker et al., 2007); mice were induced at 4 wk of age by a single i.p. injection of tamoxifen, and were analyzed 14 or 22 mo later. Atoh1LoxP/LoxP; Villin-CreERT2 mice were obtained by crossing Atoh1LoxP/LoxP (Shroyer et al., 2007) and Villin-CreERT2 animals (el Marjou et al., 2004). Atoh1 deletion was induced by a single daily i.p. injection of 1 mg tamoxifen (Sigma-Aldrich) for 4 d. Mice were sacrificed on d 5 or 22 after the first tamoxifen injection. Wild-type animals used in this study had a C57BL/6 genetic background. For proliferation analyses, mice were injected with 0.1 mg BrdU (Roche)/PBS per gram of mouse body weight. Mice were sacrificed 2 h after injection. For long-term BrdU incorporation studies, BrdU was given ad libitum (0.5 mg/ml) during the indicated time.
Human samples
Slides of human intestinal biopsies were kindly provided by Drs. J.-F. Bourgaux and C. Pignodel (Centre Hospitalier Régional Universitaire, Nîmes, France).
Fluorescent and bright-field immunohistochemistry on paraffin-embedded tissue
Tissue dissection, fixation, and immunohistochemistry on thin sections of paraffin-embedded tissue were performed essentially as described previously (Bastide et al., 2007). In brief, 5-µm-thick sections were dewaxed in xylene and rehydrated in graded alcohol baths. Antigen retrieval was performed by boiling slides for 20 min in 10 mM sodium citrate buffer, pH 6.0. Nonspecific binding sites were blocked in blocking buffer (TBS, pH 7.4, 5% dried milk, and 0.5% Triton X-100) for 60 min at RT. Sections were then incubated with primary antibodies diluted in blocking buffer overnight at 4°C. Primary antibodies used in this study were as follows: anti-SOX9 (AB5535; 1:1,000) and anti-villin (MAB1671; 1:500) were purchased from Millipore. Anti-COX1 (sc-1754; 1:200), anti-COX2 (sc-1747; 1:200), anti-PCNA (sc-56; 1:200), and anti-MUC2 (sc-15334; 1:200) were from Santa Cruz Biotechnology, Inc. Anti-HPGDS (160013; 1:200) was from Cayman Chemical. Anti–α-tubulin (32–2500; 1:200) was from Invitrogen. Anti-Neurog3 (F25A1B3; 1:100) was from the Developmental Studies Hybridoma Bank (Iowa City, IA). Anti–β-catenin (610154; 1:200) was from BD. Anti–β-endorphin (20063; 1:100) was from Immunostar. Anti-BrdU was from Abcam (Ab1893; 1:300) or from the Developmental Studies Hybridoma Bank (G3G4; 1:300). Anti–β-galactosidase (ab9361; 1:400) was from Abcam. Anti-lysozyme (RB-372; 1:500) was from NeoMarkers. Anti-DCLK1 was from Abcam (ab37994; 1:200) or Abgent (AP7219b; 1:200). Anti-ChgA was from Immunostar (20085; 1:1,000) or Santa Cruz Biotechnology, Inc. (sc-1488; 1:400). Anti-Ki67 (ab15580; 1:500) and anti–phospho-histone H3 (ab14955; 1:800) were from Abcam. Slides were then washed two times with 0.1% PBS-Tween (Sigma-Aldrich) before incubation with fluorescent secondary antibodies conjugated with either Alexa 488, Cyanin-3, or Cyanin-5 (Jackson ImmunoResearch Laboratories, Inc.) and Hoechst at 2 µg/ml (Sigma-Aldrich) in PBS–Triton X-100 0.1% (Sigma-Aldrich). Stained slides were then washed two extra times in PBS before mounting with aqueous glycerol–mowiol medium. Methods used for bright-field immunohistochemistry were identical, except that slides were incubated with 1.5% H2O2 in methanol for 20 min and washed in PBS to quench endogenous peroxydase activity before antigen retrieval. Envision+ (Dako) was used as a secondary reagent. Signals were developed with DAB (Sigma-Aldrich) and a hematoxylin counterstain (DiaPath) was used. After dehydration, sections were mounted in Pertex (Histolab).
Whole-mount fluorescent immunohistochemistry
For some experiments, immunolabeling was performed directly on whole crypts or whole pieces of villus epithelium. In brief, the small intestine was removed, flushed with PBS, and turned inside-out on a wooden stick before being incubated in 10 mM DTT for 15 min at room temperature to remove mucus. Tissue was then incubated in cold Ca2+/Mg2+-free PBS containing 10 mM EDTA for 20 min and nearly intact pieces of villus epithelium were recovered by gentle shaking. Cycles of incubation/shaking were repeated until whole crypts were obtained. Whole fragments of epithelium were fixed in 4% PFA for 2 h at RT and then washed twice in PBS before being processed for immunohistochemistry. Pieces of epithelium were first incubated and permeabilized in blocking buffer (TBS, pH 7.4; 5% dried milk, and 0.5% Triton X-100) for 1 h at RT before incubation with primary antibodies overnight. Material was then washed four times in PBS Triton X-100 (0.1%) at RT before incubation with fluorescent-conjugated secondary antibodies (Jackson ImmunoResearch Laboratories, Inc.) and Hoechst at 2 µg/ml (Sigma-Aldrich) for 60 min at RT in PBS Triton X-100 (0.1%). Stained tissues were washed two extra times in PBS, smeared in poly-lysine–coated slides, and mounted in glycerol–mowiol medium. F-actin staining was performed with Alexa Fluor 647–conjugated phalloidin (Invitrogen).
Microscopy and imaging
Fluorescent pictures were acquired at room temperature under a microscope (AxioImager Z1; Carl Zeiss, Inc.), equipped with a camera (AxioCam MRm; Carl Zeiss, Inc.), EC Plan Neofluar (5x, NA 0.16; 10x, NA 0.3; 20x, 0.5 NA; 100x, NA 1.3) and Plan Apochromat (40x, NA 0.95; 63x, NA 1.4) objectives, the Apotome Slider system equipped with an H1 transmission grid (Carl Zeiss, Inc.), and AxioVision software (Carl Zeiss, Inc.). Aqueous mounting medium (0.1 M Tris, pH 8.5, 24% glycerol wt/vol, 10% mowiol wt/vol [Sigma-Aldrich], and 2.5 mg.ml−1 final DABCO [Sigma-Aldrich]) was used for fluorescent acquisition. Bright-field immunohistochemistry pictures were taken at room temperature with a microscope (Eclipse 80i; Nikon) with Plan Fluor (10x, NA 0.3; 20x, NA 0.5; 40x, NA 0.75; and 60x, NA 0.5–1.25) lenses (Nikon) and a digital camera (Q-Imaging Retiga 2000R with a Q-Imaging RGB Slider). Pictures were captured with Q-Capture Pro software (Nikon). For wide-field acquisition of bright-field images, slides were scanned at 20x with the Nanozoomer Slide Scanner (Hamamatsu Photonics). Resulting images were visualized and annotated with NDPview software (Hamamatsu Photonics). Post-treatment of pictures, annotations, and panel composition were performed with Photoshop software (Adobe).
Statistical analyses
Histograms and determination of standard deviations were calculated with Excel software (Microsoft). Statistical analysis of proportions of β-galactosidase+ tuft cells versus β-galactosidase+ epithelial cells was performed by a Mann-Whitney test with Prism software (GraphPad Software, Inc.).
Online supplemental material
Fig. S1 shows identification of tuft cells in mouse and human tissues, using the tuft cell signature. Fig. S2 shows that tuft cells are found all along the intestinal tract. Fig. S3 shows that intestinal tuft cells do not share terminal differentiation markers with the other secretory cell lineages. Fig. S4 shows that the tuft cell population is not affected in Gfi-1– or Spdef-deficient mice. Fig. S5 shows early enteroendocrine cell differentiation in intestinal crypts. Online supplemental material is available at http://www.jcb.org/cgi/content/full/jcb.201010127/DC1.
Acknowledgments
The authors wish to thank Drs. Nick Barker and Alex Gregorieff for reagents, Maaike van den Born for technical help, Daniel Fisher and Catherine Legraverend for critical reading and editing of the manuscript, and the staff of the animal facility for excellent service. The Neurogenin3 antibody (F25A1B3) developed by Dr. O.D. Madsen and the BrdU antibody (G3G4) developed by Dr. S.J. Kaufman were obtained from the Developmental Studies Hybridoma Bank developed under the auspices of the NICHD and maintained by The University of Iowa, Department of Biology (Iowa City, IA).
This work was supported by the Agence Nationale pour la Recherche (ANR-09-BLAN-0368-01), Institut National du Cancer (INCa 2007-1-COL-6-IC-1 to S. Robine and PLBIO09-070 to P. Jay), and Association pour la Recherche contre le Cancer (ARC 5050). F. Gerbe was supported by the Ligue Nationale contre le Cancer (LNCC).
The authors disclose no conflict of interest.
Footnotes
Abbreviations used in this paper:
- Atoh1
- atonal homologue 1
- CBC
- crypt base columnar
- ChgA
- chromogranin A
- COX
- cyclooxygenase
- DCLK1
- doublecortin-like kinase 1
- Gfi1
- growth factor-independent 1
- Hes1
- hairy/enhancer of split 1
- HPGDS
- hematopoietic prostaglandin-D synthase
- Lgr5
- leucine-rich repeat containing G protein–coupled receptor 5
- Neurog3
- Neurogenin3
- PCNA
- proliferating cell nuclear antigen
- Sox9
- SRY-box containing gene 9
- Spdef
- SAM pointed domain containing ets transcription factor
- Trpm5
- transient receptor potential cation channel, subfamily M, member 5
- Wnt
- Wingless-related MMTV integration site
References
- Barker N., Clevers H. 2010. Leucine-rich repeat-containing G-protein-coupled receptors as markers of adult stem cells. Gastroenterology. 138:1681–1696 10.1053/j.gastro.2010.03.002 [DOI] [PubMed] [Google Scholar]
- Barker N., van Es J.H., Kuipers J., Kujala P., van den Born M., Cozijnsen M., Haegebarth A., Korving J., Begthel H., Peters P.J., Clevers H. 2007. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 449:1003–1007 10.1038/nature06196 [DOI] [PubMed] [Google Scholar]
- Bastide P., Darido C., Pannequin J., Kist R., Robine S., Marty-Double C., Bibeau F., Scherer G., Joubert D., Hollande F., et al. 2007. Sox9 regulates cell proliferation and is required for Paneth cell differentiation in the intestinal epithelium. J. Cell Biol. 178:635–648 10.1083/jcb.200704152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezençon C., le Coutre J., Damak S. 2007. Taste-signaling proteins are coexpressed in solitary intestinal epithelial cells. Chem. Senses. 32:41–49 10.1093/chemse/bjl034 [DOI] [PubMed] [Google Scholar]
- Bezençon C., Fürholz A., Raymond F., Mansourian R., Métairon S., Le Coutre J., Damak S. 2008. Murine intestinal cells expressing Trpm5 are mostly brush cells and express markers of neuronal and inflammatory cells. J. Comp. Neurol. 509:514–525 10.1002/cne.21768 [DOI] [PubMed] [Google Scholar]
- Bjerknes M., Cheng H. 1999. Clonal analysis of mouse intestinal epithelial progenitors. Gastroenterology. 116:7–14 10.1016/S0016-5085(99)70222-2 [DOI] [PubMed] [Google Scholar]
- Bjerknes M., Cheng H. 2006. Neurogenin 3 and the enteroendocrine cell lineage in the adult mouse small intestinal epithelium. Dev. Biol. 300:722–735 10.1016/j.ydbio.2006.07.040 [DOI] [PubMed] [Google Scholar]
- Bjerknes M., Cheng H. 2010. Cell Lineage metastability in Gfi1-deficient mouse intestinal epithelium. Dev. Biol. 345:49–63 10.1016/j.ydbio.2010.06.021 [DOI] [PubMed] [Google Scholar]
- Blache P., van de Wetering M., Duluc I., Domon C., Berta P., Freund J.N., Clevers H., Jay P. 2004. SOX9 is an intestine crypt transcription factor, is regulated by the Wnt pathway, and represses the CDX2 and MUC2 genes. J. Cell Biol. 166:37–47 10.1083/jcb.200311021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colnot S., Niwa-Kawakita M., Hamard G., Godard C., Le Plenier S., Houbron C., Romagnolo B., Berrebi D., Giovannini M., Perret C. 2004. Colorectal cancers in a new mouse model of familial adenomatous polyposis: influence of genetic and environmental modifiers. Lab. Invest. 84:1619–1630 10.1038/labinvest.3700180 [DOI] [PubMed] [Google Scholar]
- Dekaney C.M., Gulati A.S., Garrison A.P., Helmrath M.A., Henning S.J. 2009. Regeneration of intestinal stem/progenitor cells following doxorubicin treatment of mice. Am. J. Physiol. Gastrointest. Liver Physiol. 297:G461–G470 10.1152/ajpgi.90446.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- el Marjou F., Janssen K.P., Chang B.H., Li M., Hindie V., Chan L., Louvard D., Chambon P., Metzger D., Robine S. 2004. Tissue-specific and inducible Cre-mediated recombination in the gut epithelium. Genesis. 39:186–193 10.1002/gene.20042 [DOI] [PubMed] [Google Scholar]
- Formeister E.J., Sionas A.L., Lorance D.K., Barkley C.L., Lee G.H., Magness S.T. 2009. Distinct SOX9 levels differentially mark stem/progenitor populations and enteroendocrine cells of the small intestine epithelium. Am. J. Physiol. Gastrointest. Liver Physiol. 296:G1108–G1118 10.1152/ajpgi.00004.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fre S., Huyghe M., Mourikis P., Robine S., Louvard D., Artavanis-Tsakonas S. 2005. Notch signals control the fate of immature progenitor cells in the intestine. Nature. 435:964–968 10.1038/nature03589 [DOI] [PubMed] [Google Scholar]
- Gebert A., al-Samir K., Werner K., Fassbender S., Gebhard A. 2000. The apical membrane of intestinal brush cells possesses a specialised, but species-specific, composition of glycoconjugates—on-section and in vivo lectin labelling in rats, guinea-pigs and mice. Histochem. Cell Biol. 113:389–399 10.1007/s004180000148 [DOI] [PubMed] [Google Scholar]
- Gebhard A., Gebert A. 1999. Brush cells of the mouse intestine possess a specialized glycocalyx as revealed by quantitative lectin histochemistry. Further evidence for a sensory function. J. Histochem. Cytochem. 47:799–808 10.1177/002215549904700609 [DOI] [PubMed] [Google Scholar]
- Gerbe F., Brulin B., Makrini L., Legraverend C., Jay P. 2009. DCAMKL-1 expression identifies Tuft cells rather than stem cells in the adult mouse intestinal epithelium. Gastroenterology. 137:2179–2180, author reply :2180–2181 10.1053/j.gastro.2009.06.072 [DOI] [PubMed] [Google Scholar]
- Giannakis M., Stappenbeck T.S., Mills J.C., Leip D.G., Lovett M., Clifton S.W., Ippolito J.E., Glasscock J.I., Arumugam M., Brent M.R., Gordon J.I. 2006. Molecular properties of adult mouse gastric and intestinal epithelial progenitors in their niches. J. Biol. Chem. 281:11292–11300 10.1074/jbc.M512118200 [DOI] [PubMed] [Google Scholar]
- Gregorieff A., Stange D.E., Kujala P., Begthel H., van den Born M., Korving J., Peters P.J., Clevers H. 2009. The ets-domain transcription factor Spdef promotes maturation of goblet and paneth cells in the intestinal epithelium. Gastroenterology. 137:1333–1345: e1–e3 10.1053/j.gastro.2009.06.044 [DOI] [PubMed] [Google Scholar]
- Höfer D., Drenckhahn D. 1992. Identification of brush cells in the alimentary and respiratory system by antibodies to villin and fimbrin. Histochemistry. 98:237–242 10.1007/BF00271037 [DOI] [PubMed] [Google Scholar]
- Höfer D., Drenckhahn D. 1996. Cytoskeletal markers allowing discrimination between brush cells and other epithelial cells of the gut including enteroendocrine cells. Histochem. Cell Biol. 105:405–412 10.1007/BF01463662 [DOI] [PubMed] [Google Scholar]
- Höfer D., Drenckhahn D. 1998. Identification of the taste cell G-protein, alpha-gustducin, in brush cells of the rat pancreatic duct system. Histochem. Cell Biol. 110:303–309 10.1007/s004180050292 [DOI] [PubMed] [Google Scholar]
- Höfer D., Püschel B., Drenckhahn D. 1996. Taste receptor-like cells in the rat gut identified by expression of alpha-gustducin. Proc. Natl. Acad. Sci. USA. 93:6631–6634 10.1073/pnas.93.13.6631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzer P. 2009. Opioid receptors in the gastrointestinal tract. Regul. Pept. 155:11–17 10.1016/j.regpep.2009.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iseki S., Kanda T., Hitomi M., Ono T. 1991. Ontogenic appearance of three fatty acid binding proteins in the rat stomach. Anat. Rec. 229:51–60 10.1002/ar.1092290107 [DOI] [PubMed] [Google Scholar]
- Jang H.J., Kokrashvili Z., Theodorakis M.J., Carlson O.D., Kim B.J., Zhou J., Kim H.H., Xu X., Chan S.L., Juhaszova M., et al. 2007. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc. Natl. Acad. Sci. USA. 104:15069–15074 10.1073/pnas.0706890104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen K.P., el-Marjou F., Pinto D., Sastre X., Rouillard D., Fouquet C., Soussi T., Louvard D., Robine S. 2002. Targeted expression of oncogenic K-ras in intestinal epithelium causes spontaneous tumorigenesis in mice. Gastroenterology. 123:492–504 10.1053/gast.2002.34786 [DOI] [PubMed] [Google Scholar]
- Jarvi O., Keyrilainen O. 1956. On the cellular structures of the epithelial invasions in the glandular stomach of mice caused by intramural application of 20-methylcholantren. Acta Pathol Microbiol Scand Suppl. 39(Suppl 111):72–73 [PubMed] [Google Scholar]
- Jenny M., Uhl C., Roche C., Duluc I., Guillermin V., Guillemot F., Jensen J., Kedinger M., Gradwohl G. 2002. Neurogenin3 is differentially required for endocrine cell fate specification in the intestinal and gastric epithelium. EMBO J. 21:6338–6347 10.1093/emboj/cdf649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen J., Pedersen E.E., Galante P., Hald J., Heller R.S., Ishibashi M., Kageyama R., Guillemot F., Serup P., Madsen O.D. 2000. Control of endodermal endocrine development by Hes-1. Nat. Genet. 24:36–44 10.1038/71657 [DOI] [PubMed] [Google Scholar]
- Jin G., Ramanathan V., Quante M., Baik G.H., Yang X., Wang S.S., Tu S., Gordon S.A., Pritchard D.M., Varro A., et al. 2009. Inactivating cholecystokinin-2 receptor inhibits progastrin-dependent colonic crypt fission, proliferation, and colorectal cancer in mice. J. Clin. Invest. 119:2691–2701 10.1172/JCI38918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J.P., Perreault N., Goldstein B.G., Lee C.S., Labosky P.A., Yang V.W., Kaestner K.H. 2002. The zinc-finger transcription factor Klf4 is required for terminal differentiation of goblet cells in the colon. Development. 129:2619–2628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kist R., Schrewe H., Balling R., Scherer G. 2002. Conditional inactivation of Sox9: a mouse model for campomelic dysplasia. Genesis. 32:121–123 10.1002/gene.10050 [DOI] [PubMed] [Google Scholar]
- Kokrashvili Z., Rodriguez D., Yevshayeva V., Zhou H., Margolskee R.F., Mosinger B. 2009. Release of endogenous opioids from duodenal enteroendocrine cells requires Trpm5. Gastroenterology. 137:598–606: 606: e1–e2 10.1053/j.gastro.2009.02.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek V., Barker N., Moerer P., van Donselaar E., Huls G., Peters P.J., Clevers H. 1998. Depletion of epithelial stem-cell compartments in the small intestine of mice lacking Tcf-4. Nat. Genet. 19:379–383 10.1038/1270 [DOI] [PubMed] [Google Scholar]
- Kugler P., Höfer D., Mayer B., Drenckhahn D. 1994. Nitric oxide synthase and NADP-linked glucose-6-phosphate dehydrogenase are co-localized in brush cells of rat stomach and pancreas. J. Histochem. Cytochem. 42:1317–1321 10.1177/42.10.7523487 [DOI] [PubMed] [Google Scholar]
- May R., Riehl T.E., Hunt C., Sureban S.M., Anant S., Houchen C.W. 2008. Identification of a novel putative gastrointestinal stem cell and adenoma stem cell marker, doublecortin and CaM kinase-like-1, following radiation injury and in adenomatous polyposis coli/multiple intestinal neoplasia mice. Stem Cells. 26:630–637 10.1634/stemcells.2007-0621 [DOI] [PubMed] [Google Scholar]
- May R., Sureban S.M., Hoang N., Riehl T.E., Lightfoot S.A., Ramanujam R., Wyche J.H., Anant S., Houchen C.W. 2009. Doublecortin and CaM kinase-like-1 and leucine-rich-repeat-containing G-protein-coupled receptor mark quiescent and cycling intestinal stem cells, respectively. Stem Cells. 27:2571–2579 10.1002/stem.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellitzer G., Beucher A., Lobstein V., Michel P., Robine S., Kedinger M., Gradwohl G. 2010. Loss of enteroendocrine cells in mice alters lipid absorption and glucose homeostasis and impairs postnatal survival. J. Clin. Invest. 120:1708–1721 10.1172/JCI40794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori-Akiyama Y., van den Born M., van Es J.H., Hamilton S.R., Adams H.P., Zhang J., Clevers H., de Crombrugghe B. 2007. SOX9 is required for the differentiation of paneth cells in the intestinal epithelium. Gastroenterology. 133:539–546 10.1053/j.gastro.2007.05.020 [DOI] [PubMed] [Google Scholar]
- Moxey P.C., Trier J.S. 1978. Specialized cell types in the human fetal small intestine. Anat. Rec. 191:269–285 10.1002/ar.1091910302 [DOI] [PubMed] [Google Scholar]
- Noah T.K., Kazanjian A., Whitsett J., Shroyer N.F. 2010. SAM pointed domain ETS factor (SPDEF) regulates terminal differentiation and maturation of intestinal goblet cells. Exp. Cell Res. 316:452–465 10.1016/j.yexcr.2009.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto D., Gregorieff A., Begthel H., Clevers H. 2003. Canonical Wnt signals are essential for homeostasis of the intestinal epithelium. Genes Dev. 17:1709–1713 10.1101/gad.267103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodin J., Dalhamn T. 1956. Electron microscopy of the tracheal ciliated mucosa in rat. Z. Zellforsch. Mikrosk. Anat. 44:345–412 10.1007/BF00345847 [DOI] [PubMed] [Google Scholar]
- Sancho E., Batlle E., Clevers H. 2004. Signaling pathways in intestinal development and cancer. Annu. Rev. Cell Dev. Biol. 20:695–723 10.1146/annurev.cellbio.20.010403.092805 [DOI] [PubMed] [Google Scholar]
- Sangiorgi E., Capecchi M.R. 2008. Bmi1 is expressed in vivo in intestinal stem cells. Nat. Genet. 40:915–920 10.1038/ng.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato A. 2007. Tuft cells. Anat. Sci. Int. 82:187–199 10.1111/j.1447-073X.2007.00188.x [DOI] [PubMed] [Google Scholar]
- Sato T., van Es J.H., Snippert H.J., Stange D.E., Vries R.G., van den Born M., Barker N., Shroyer N.F., van de Wetering M., Clevers H. 2011. Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature. 469:415–418 10.1038/nature09637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonhoff S.E., Giel-Moloney M., Leiter A.B. 2004. Neurogenin 3-expressing progenitor cells in the gastrointestinal tract differentiate into both endocrine and non-endocrine cell types. Dev. Biol. 270:443–454 10.1016/j.ydbio.2004.03.013 [DOI] [PubMed] [Google Scholar]
- Shroyer N.F., Wallis D., Venken K.J., Bellen H.J., Zoghbi H.Y. 2005. Gfi1 functions downstream of Math1 to control intestinal secretory cell subtype allocation and differentiation. Genes Dev. 19:2412–2417 10.1101/gad.1353905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shroyer N.F., Helmrath M.A., Wang V.Y., Antalffy B., Henning S.J., Zoghbi H.Y. 2007. Intestine-specific ablation of mouse atonal homolog 1 (Math1) reveals a role in cellular homeostasis. Gastroenterology. 132:2478–2488 10.1053/j.gastro.2007.03.047 [DOI] [PubMed] [Google Scholar]
- Stenson W.F. 2008. What is the function of cyclooxygenases in the normal and inflamed intestine? Inflamm. Bowel Dis. 14:S104–S105 10.1002/ibd.20700 [DOI] [PubMed] [Google Scholar]
- Sureban S.M., May R., Ramalingam S., Subramaniam D., Natarajan G., Anant S., Houchen C.W. 2009. Selective blockade of DCAMKL-1 results in tumor growth arrest by a Let-7a MicroRNA-dependent mechanism. Gastroenterology. 137:649–659: 659: e1–e2 10.1053/j.gastro.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland K., Young R.L., Cooper N.J., Horowitz M., Blackshaw L.A. 2007. Phenotypic characterization of taste cells of the mouse small intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 292:G1420–G1428 10.1152/ajpgi.00504.2006 [DOI] [PubMed] [Google Scholar]
- Suzuki K., Fukui H., Kayahara T., Sawada M., Seno H., Hiai H., Kageyama R., Okano H., Chiba T. 2005. Hes1-deficient mice show precocious differentiation of Paneth cells in the small intestine. Biochem. Biophys. Res. Commun. 328:348–352 10.1016/j.bbrc.2004.12.174 [DOI] [PubMed] [Google Scholar]
- van der Flier L.G., Clevers H. 2009. Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annu. Rev. Physiol. 71:241–260 10.1146/annurev.physiol.010908.163145 [DOI] [PubMed] [Google Scholar]
- van der Flier L.G., van Gijn M.E., Hatzis P., Kujala P., Haegebarth A., Stange D.E., Begthel H., van den Born M., Guryev V., Oving I., et al. 2009. Transcription factor achaete scute-like 2 controls intestinal stem cell fate. Cell. 136:903–912 10.1016/j.cell.2009.01.031 [DOI] [PubMed] [Google Scholar]
- van Es J.H., Jay P., Gregorieff A., van Gijn M.E., Jonkheer S., Hatzis P., Thiele A., van den Born M., Begthel H., Brabletz T., et al. 2005a. Wnt signalling induces maturation of Paneth cells in intestinal crypts. Nat. Cell Biol. 7:381–386 10.1038/ncb1240 [DOI] [PubMed] [Google Scholar]
- van Es J.H., van Gijn M.E., Riccio O., van den Born M., Vooijs M., Begthel H., Cozijnsen M., Robine S., Winton D.J., Radtke F., Clevers H. 2005b. Notch/gamma-secretase inhibition turns proliferative cells in intestinal crypts and adenomas into goblet cells. Nature. 435:959–963 10.1038/nature03659 [DOI] [PubMed] [Google Scholar]
- van Es J.H., de Geest N., van de Born M., Clevers H., Hassan B.A. 2010. Intestinal stem cells lacking the Math1 tumour suppressor are refractory to Notch inhibitors. Nat. Commun.. 1:1–5 10.1038/ncomms1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Dubois R.N. 2010. Eicosanoids and cancer. Nat. Rev. Cancer. 10:181–193 10.1038/nrc2809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q., Bermingham N.A., Finegold M.J., Zoghbi H.Y. 2001. Requirement of Math1 for secretory cell lineage commitment in the mouse intestine. Science. 294:2155–2158 10.1126/science.1065718 [DOI] [PubMed] [Google Scholar]