Abstract
Journal of Clinical Oncology recently published ASCO's update to its guideline on the use of bone-modifying agents for patients with bone metastases, the scope of which was narrowed to the use of bone-modifying agents for patients with evidence of bone metastases.
Journal of Clinical Oncology (JCO) recently published ASCO's update to its guideline on the use of bone-modifying agents for patients with breast cancer with bone metastases.1 A commentary on this guideline appears in this issue of Journal of Oncology Practice. ASCO first published evidence-based clinical practice guidelines for use of bisphosphonates in breast cancer in 2000 and updated these guidelines in 2003. In its current update, the scope was narrowed to the use of bone-modifying agents for patients with evidence of bone metastases. The updated guideline uses the term “bone-modifying agents” to encompass both bisphosphonates and newer osteoclast inhibitors. The topic of the use of bone-modifying agents for the adjuvant treatment of breast cancer and in managing treatment-associated bone loss will be covered in a separate guideline update.
The guideline is based on a systematic search and review of the literature. The recommendations on efficacy are based only on phase III randomized controlled trials. The primary outcome of interest in these trials was skeletal-related events (SREs), the definition of which typically includes fracture, radiation to the bone, surgery to the bone, and spinal cord compression and may or may not include hypercalcemia of malignancy.
Six of the eight recommendations are substantively unchanged from the 2003 guideline update. A new recommendation was added regarding osteonecrosis of the jaw, a condition recognized after the preparation of the 2003 guidelines. This guideline on metastatic breast cancer also added a new bone-modifying agent, denosumab (Table 1). For each of the recommendations, clinical judgment should also take into consideration the patient's general performance status, overall prognosis, and goals of care.
Table 1.
New Bone-Modifying Agent
| Recommendation Category | 2003 Recommendations | 2011 Recommendations | Change |
|---|---|---|---|
| Indications and time of initiation | For breast cancer patients who have evidence of bone destruction on plain radiographs, IV pamidronate 90 mg delivered over 2 h or zoledronic acid 4 mg over 15 min every 3 to 4 wk are recommended. Starting bisphosphonates in women with an abnormal bone scan and an abnormal CT or MRI scan showing bone destruction, but normal plain radiographs, is considered reasonable by Panel consensus based on the findings in women with lytic or mixed lytic/blastic changes on plain radiographs. There is insufficient evidence relating to efficacy to support one bisphosphonate over the other. For each of the guidelines, clinical judgment should also take into consideration the patient's general performance status and overall prognosis. | For patients with breast cancer who have evidence of bone metastases, denosumab 120 mg subcutaneously every 4 wk, or IV pamidronate 90 mg delivered over no less than 2 h, or zoledronic acid 4 mg over no less than 15 min every 3 to 4 wk is recommended. Starting bone-modifying agents in women with an abnormal bone scan and an abnormal CT scan or MRI showing bone destruction, but normal plain radiographs, is considered reasonable by Panel consensus based on the findings in women with lytic or mixed lytic/blastic changes on plain radiographs. Starting bone-modifying agents in women with only an abnormal bone scan but without evidence of bone destruction on radiographs, CT scans, or MRI is not recommended outside of a clinical trial. There is insufficient evidence relating to efficacy to support one bone-modifying agent over another. | Addition of new bone-modifying agent. Term changed from bisphosphonates to bone-modifying agents. |
Note: Bolded text indicates substantive changes. Italicized text indicates minor changes.
Abbreviations: IV, intravenous; CT, computed tomography; MRI, magnetic resonance imaging; h, hours; min, minutes; wk, weeks.
No additional data identified using the methods of this systematic review are available with regard to the dose, dose interval, duration of therapy of bone-modifying agents, or pain management. These recommendations appear in Table 2. The adverse event recommendations, including the new recommendation for osteonecrosis of the jaw, rely on evidence from randomized controlled trials, case-control, and cohort studies (Table 3).
Table 2.
Additional Efficacy and Pain Recommendations
| Recommendation Category | 2003 Recommendations | 2011 Recommendations | Change |
|---|---|---|---|
| Role of bone-modifying agents in the presence of extraskeletal metastases | Starting bisphosphonates in women without evidence of bone metastases even in the presence of other extraskeletal metastases is not recommended. This clinical situation has not been studied using IV bisphosphonates and should be the focus of new clinical trials. Starting bisphosphonates in women with only an abnormal bone scan but without evidence of bone destruction on radiographs, CT scans, or MRI is not recommended. | Starting bone-modifying agents in women without evidence of bone metastases even in the presence of other extraskeletal metastases is not recommended. This clinical situation has been inadequately studied using IV bisphosphonates or other bone-modifying agents and should be the focus of new clinical trials. |
(Unchanged in substance from 2003) Term changed from bisphosphonates to bone-modifying agents. |
| Optimal duration | The Panel suggests that once initiated, intravenous bisphosphonates be continued until evidence of substantial decline in a patient's general performance status. The Panel stresses that clinical judgment must guide what is a substantial decline. There is no evidence addressing the consequences of stopping bisphosphonates after one or more adverse skeletal events. | The Panel suggests that once initiated, bone-modifying agents be continued until evidence of substantial decline in a patient's general performance status. The Panel stresses that clinical judgment must guide what constitutes a substantial decline. There is no evidence addressing the consequences of stopping bone-modifying agents after one or more adverse skeletal-related events. |
(Unchanged in substance from 2003) Term changed from bisphosphonates to bone-modifying agents. |
| Optimal intervals between dosing | For breast cancer patients who have evidence of bone destruction on plain radiographs, intravenous pamidronate 90 mg delivered over 2 h or zoledronic acid 4 mg over 15 min every 3 to 4 wk are recommended. There is insufficient evidence relating to efficacy to support one bisphosphonate over the other. For each of the guidelines, clinical judgment should also take into consideration the patient's general performance status and overall prognosis. | For patients with breast cancer who have evidence of bone destruction on plain radiographs, denosumab 120 mg subcutaneously every 4 wk, IV pamidronate 90 mg delivered over 2 h, or zoledronic acid 4 mg over 15 min every 3 to 4 wk are recommended. | Addition of new bone-modifying agent. The second-to-last sentence of 2003 recommendation is in Recommendation 1 of 2011 recommendations. The last sentence from 2003 recommendation applies to all recommendations. |
| Role of bone-modifying agents in pain control | The Panel recommends that the current standards of care for cancer pain management must be applied throughout bisphosphonate therapy and is required by good clinical practice. These standards of care for pain management include analgesics, corticosteroids, interventional procedures, nonsteroidal anti-inflammatory agents, systemic radiopharmaceuticals, and local radiation therapy. Among other therapeutic options, IV pamidronate or zoledronic acid may be of benefit among women with pain caused by bone metastases to relieve pain when used concurrently with systemic chemotherapy and/or hormonal therapy, because it was associated with a modest pain control benefit in controlled trials. | The Panel recommends that the current standards of care for cancer bone pain management be applied at the onset of pain, in concert with the initiation of bone-modifying agent therapy. This is required by good clinical practice. The standard of care for pain management includes the use of nonsteroidal anti-inflammatory agents, opioid and nonopioid analgesics, corticosteroids, adjuvant agents, interventional procedures, systemic radiopharmaceuticals, local radiation therapy, and surgery. Bone-modifying agents are an adjunctive therapy for cancer-related bone pain control and are not recommended as first-line treatment for cancer-related pain. IV pamidronate or zoledronic acid may be of benefit for patients with pain caused by bone metastases and contribute to pain relief when used concurrently with analgesic therapy, systemic chemotherapy, radiation therapy, and/or hormonal therapy. Bone-modifying agents have been associated with a modest pain control benefit in controlled trials. | Change in timing of pain management. Term changed from bisphosphonates to bone-modifying agents. |
Note: Bolded text indicates substantive changes. Italicized text indicates minor changes.
Abbreviation: IV, intravenous; CT, computed tomography; MRI, magnetic resonance imaging; h, hours; min, minutes; wk, weeks.
Table 3.
Adverse Event Recommendations
| Recommendation Category | 2003 Recommendations | 2011 Recommendations | Change |
|---|---|---|---|
| Renal safety concerns | In patients with pre-existing renal disease and a serum creatinine less than 3.0 mg/dL (265 μmol/L), no change in dosage, infusion time, or interval of pamidronate or zoledronic acid is required. Use of these bisphosphonates among patients with worse function has been minimally assessed. Infusion times less than 2 h with pamidronate or less than 15 min with zoledronic acid should be avoided. The Panel recommends that serum creatinine should be monitored prior to each dose of pamidronate or zoledronic acid, in accordance with FDA-approved labeling. Serum calcium, electrolytes, phosphate, magnesium, and hematocrit/hemoglobin should also be monitored regularly but there is no evidence upon which to base a recommendation for time intervals. In contrast to multiple myeloma patients, there currently is no data to support routine assessments for albuminuria in breast cancer patients. |
In patients with a calculated serum creatinine clearance > 60 mL/min, no change in dosage, infusion time, or interval of pamidronate or zoledronic acid administration is required. Use of bone-modifying agents among patients with reduced renal function has been incompletely assessed. The packet insert of zoledronic acid provides guidance for dosing when baseline serum creatinine clearance is ≥ 30 and < 60 mL/min. Infusion times less than 2 h with pamidronate or less than 15 min with zoledronic acid should be avoided. The Panel recommends that serum creatinine should be monitored prior to each dose of pamidronate or zoledronic acid, in accordance with FDA-approved labeling. Serum calcium, electrolytes, phosphate, magnesium, and hematocrit/hemoglobin should also be monitored regularly. The risk of hypocalcemia with denosumab dosed at 120 mg every 4 wk has not been evaluated in patients with a creatinine clearance less than 30 mL/min or receiving dialysis. Monitor for hypocalcemia in patients with impaired creatinine clearance.There is no evidence to guide the interval for monitoring serum calcium, electrolytes, phosphate, magnesium, and hematocrit/hemoglobin with denosumab, pamidronate, or zoledronic acid. |
Addition regarding denosumab. A change in serum creatinine clearance threshold. Last sentence of 2003 recommendation taken out. Term changed from bisphosphonates to bone-modifying agents. |
| Osteonecrosis of the jaw | N/A | Osteonecrosis of the jaw (ONJ) is an uncommon but potentially serious condition associated with the use of bone-modifying agents. The Update Committee concurs with the revised FDA label for zoledronic acid and pamidronate and the FDA label for denosumab and recommends that all patients with cancer receive a dental examination and necessary preventive dentistry prior to initiating therapy with inhibitors of osteoclast function unless there are mitigating factors that preclude the dental assessment. These recommendations should be observed whenever possible. While receiving inhibitors of osteoclast function, patients should maintain optimal oral hygiene and, if possible, avoid invasive dental procedures that involve manipulation of the jaw bone or periosteum. Although most cases of ONJ have occurred in patients treated with IV bisphosphonates and bone-modifying agents who underwent an invasive dental procedure, cases have occurred spontaneously and have been reported in patients treated with other bone-modifying agents, including oral bisphosphonates and direct osteoclast inhibitors. | New recommendation |
| The role of biochemical markers | The use of the biochemical markers to monitor bisphosphonate use is not suggested for routine care. | The use of the biochemical markers to monitor bone-modifying agent use is not recommended for routine care. |
(Unchanged in substance from 2003) Term changed from bisphosphonates to bone-modifying agents. |
Note: Bolded text indicates substantive changes. Italicized text indicates minor changes.
Abbreviations: IV, intravenous; h, hours; min, minutes; wk, weeks.
The guideline reviews data from studies on biomarkers, however, it continues to recommend against their routine use for the purposes of diagnosing SREs; predicting SREs and/or the risk of SREs; predicting whether a patient will benefit from receiving a particular bone-modifying agent; aiding selection of a particular agent; and/or monitoring response during treatment, unless the patient is enrolled onto a clinical trial (Table 3). The markers found by this systematic review were investigated for the primary purposes of monitoring, predictive value (including pain reduction), and use as a diagnostic tool.
The guideline includes a special commentary on the role of vitamin D deficiency and bone-modifying agents. Currently, there are insufficient data on which to base a recommendation on the level of vitamin D and calcium supplementation for patients taking bone-modifying agents. It also includes a section on research the Update Committee recommends be conducted to address outstanding questions, including questions on dose interval and duration of therapy of bone-modifying agent therapy.
The tables in this article are reprinted from the recent Guideline Update and provide the updated recommendations. JCO published an Executive Summary of the guideline1, which presents a brief summary overview of the complete ASCO Clinical Practice Guideline Update and a brief discussion of the relevant literature for each updated recommendation. The complete guideline, including comprehensive discussions of the literature, a description of methodology, all cited references, and a data supplement,
Guideline Update Slides (in PDF format)
which contains the evidence tables used to formulate these recommendations, is available at www.asco.org/guidelines/bisphosbreast, along with a patient guide. As in other ASCO Guidelines, the full Guideline Update includes a discussion of Patient Communication and Health Disparities relevant to this topic. A slide set is provided as an online Data Supplement of this article.
Authors
ASCO Clinical Practice Guideline Update Recommendations on the Role of Bone-Modifying Agents in Metastatic Breast Cancer was developed and written by Catherine H. Van Poznak, MD; Sarah Temin, MSPH; Gary C. Yee, PharmD, Nora A. Janjan, MD, MPSA, MBA, FACP, FAC; William E. Barlow, PhD; J. Sybil Biermann, MD; Linda D. Bosserman, MD, FACP; Cindy Geoghegan, Bruce E. Hillner, MD; Richard L. Theriault, DO; Dan S. Zuckerman, MD; and Jamie H. Von Roenn, MD.
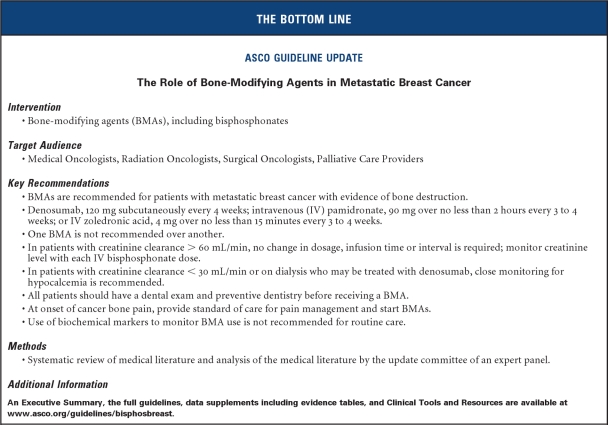
THE BOTTOM LINE: ASCO Guideline Update.
The Role of Bone-Modifying Agents in Metastatic Breast Cancer
Intervention
Bone-modifying agents (BMAs), including bisphosphonates
Target Audience
Medical Oncologists, Radiation Oncologists, Surgical Oncologists, Palliative Care Providers
Key Recommendations
BMAs are recommended for patients with metastatic breast cancer with evidence of bone destruction.
Denosumab, 120 mg subcutaneously every 4 weeks; intravenous (IV) pamidronate, 90 mg over no less than 2 hours every 3 to 4 weeks; or IV zoledronic acid, 4 mg over no less than 15 minutes every 3 to 4 weeks.
One BMA is not recommended over another.
In patients with creatinine clearance > 60 mL/min, no change in dosage, infusion time or interval is required; monitor creatinine level with each IV bisphosphonate dose.
In patients with creatinine clearance < 30 mL/min or on dialysis who may be treated with denosumab, close monitoring for hypocalcemia is recommended.
All patients should have a dental exam and preventive dentistry before receiving a BMA.
At onset of cancer bone pain, provide standard of care for pain management and start BMAs.
Use of biochemical markers to monitor BMA use is not recommended for routine care.
Methods
Systematic review of medical literature and analysis of the medical literature by the update committee of an expert panel.
Additional Information
An Executive Summary, the full guidelines, data supplements including evidence tables, and Clinical Tools and Resources are available at www.asco.org/guidelines/bisphosbreast.
Supplementary Material
Authors' Disclosures of Potential Conflicts of Interest
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory Role: Catherine H. Van Poznak, Amgen (C) Stock Ownership: None Honoraria: None Research Funding: Catherine H. Van Poznak, Amgen, Novartis Expert Testimony: None Other Remuneration: None
Author Contributions
Conception and design: Catherine H. Van Poznak, Jamie H. Von Roenn, Sarah Temin
Administrative support: Sarah Temin
Collection and assembly of data: Catherine H. Van Poznak, Sarah Temin
Data analysis and interpretation: Catherine H. Van Poznak, Jamie H. Von Roenn, Sarah Temin
Manuscript writing: Catherine H. Van Poznak, Jamie H. Von Roenn, Sarah Temin
Final approval of manuscript: Catherine H. Van Poznak, Jamie H. Von Roenn, Sarah Temin
Reference
- 1.Van Poznak CH, Temin S, Yee GC, et al. American Society of Clinical Oncology executive summary of the clinical practice guideline update recommendations on the role of bone-modifying agents in metastatic breast cancer. J Clin Oncol. doi: 10.1200/JOP.2011.000212. doi: 10.1200/JCO.2010.32.5209. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Guideline Update Slides (in PDF format)