Abstract
Purpose
The current wars in Iraq and Afghanistan have led to an increasing number of female veterans seeking medical and mental healthcare in the Department of Veterans Affairs (VA) healthcare system. To better understand gender differences in healthcare needs among recently returned veterans, we examined the prevalence of positive screenings for depression, posttraumatic stress disorder (PTSD), military sexual trauma (MST), obesity, and chronic pain among female and male veterans of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) receiving care at the VA Connecticut Healthcare System.
Methods
We performed a retrospective, cross-sectional data analysis of OEF/OIF veterans at VA Connecticut who received services in either Primary Care or the Women's Health Clinic between 2001 and 2006.
Results
In this study, 1129 electronic medical records (1032 men, 197 women) were examined. Female veterans were more likely to screen positive for MST (14% vs. 1%, p < 0.001) and depression (48% vs. 39%, p = 0.01) and less likely to screen positive for PTSD (21% vs. 33%, p = 0.002). There was no significant gender difference in clinically significant pain scores. Men were more likely than women to have body mass index (BMI) >30 kg/m2 (21% vs. 13%, p = 0.008).
Conclusions
These results suggest that important gender differences exist in the prevalence of positive screenings for MST, depression, obesity, and PTSD. As the VA continues to review and improve its services for women veterans, clinicians, researchers, and senior leaders should consider innovative ways to ensure that female veterans receive the health services they need within the VA system.
Introduction
The current wars in Iraq and Afghanistan have engendered a growing population of female veterans seeking healthcare through the Veterans Administration (VA). At present, 15% of active military, 17% of National Guard/Reserves, and 20% of new recruits are women.1 Recent studies suggest that women are among the fastest growing segments of new users of VA healthcare and that as many as 40% of women returning from Iraq and Afghanistan may elect to use the VA.2
Accommodating women who have served in Operation Enduring Freedom (OEF) (in Afghanistan) or Operation Iraqi Freedom (OIF) poses a unique challenge for the VA. Women are serving extended and repeated deployments in Iraq and Afghanistan, potentially putting them more at risk of physical or mental health problems than female veterans from previous eras.3 Because the VA previously has provided care for a largely male population, the influx of female veterans who have served in Iraq or Afghanistan, with potentially different healthcare needs, raises concerns about providing high-quality care for female veterans.
Certain medical and mental health conditions, including depression,4 posttraumatic stress disorder (PTSD),5 chronic pain,6–10 and sexual trauma,11 are more prevalent in women than men in civilian populations. Obesity is less prevalent in women in civilian populations.12 For VA strategic planning, it is important to determine the prevalence of these conditions in women veterans so that appropriate services are allocated to meet their needs.
Preliminary studies of the prevalence of these conditions in women veterans show results that differ from those found in the civilian population. In contrast to studies in civilian populations, some preliminary evidence suggests that men and women deployed in Iraq may have similar rates of PTSD and depression.13,14 Because of the large body of civilian evidence that these conditions are more common in women, further research is clearly needed to clarify the relative prevalence of mental health disorders in female and male veterans of OEF/OIF and to monitor the trajectory of these disorders over time after deployment.
Unlike studies of PTSD and depression, in studies of pain, preliminary evidence shows that women veterans may have a higher prevalence of pain than male veterans (similar to civilian reports). In one survey of women veterans seen in a primary care clinic, a higher prevalence of persistent pain was found in female veterans (78%)15 than had been noted in male veterans (50%) in a previous study.16
Gender differences in the identification and treatment of military sexual trauma (MST) are also an important consideration for the VA. MST is defined as severe or threatening forms of sexual harassment and sexual assault sustained in military service. The annual incidence of sexual assault is 3% among active duty women and 1% among active duty men. Sexual coercion and unwanted sexual attention within the military occur at an annual rate of 8% and 27%, respectively, among women and 1% and 5%, respectively, among men.17 Evidence suggests that women who have experienced MST report higher levels of depression, substance abuse, and medical conditions18,19 than those without MST. A more recent study suggests that there is a strong association between MST and mental health conditions, including PTSD, eating disorders, and personality disorders.11
Obesity is also a growing problem in the VA, as it is associated with an increased risk of adverse outcomes in the general population.20 A study of veterans receiving care at VA medical facilities found the prevalence of obesity to be higher among women (37%) than men (33%).21
In the VA, universal screening for medical and mental health conditions, including depression, PTSD, MST, body mass index (BMI), and a pain score, is required. (MST is a one-time screen. Depression screening, PTSD screening, and the BMI measurement are performed annually, and pain scores are recorded as part of vital signs at every visit.) Because further studies are needed to clarify whether there are gender differences in the burden of stress-related conditions in female and male veterans of OEF/OIF, we chose to use the VA clinical reminder screening data to further evaluate this patient population. We hypothesized that female veterans would be more likely to have positive screens for depression, PTSD, MST, and obesity than male veterans and to have higher pain scores.
In this article, we report the use of text processing techniques to retrieve screening data from the electronic medical record to determine the frequency of positive screens for stress-related conditions in female veterans of OEF/OIF.
Materials and Methods
Sample and sources of data
We performed a retrospective, cross-sectional data analysis using electronic medical records of OEF/OIF veterans at VA Connecticut who received services in either Primary Care or the Women's Health Clinic from October 1, 2001, through May 7, 2007. To identify OEF/OIF veterans in Connecticut, we obtained the local OEF/OIF roster file through the OEF/OIF Coordinator at VA Connecticut. The local roster contained Connecticut OEF/OIF military discharges from October 1, 2001, through May 7, 2007, who had enrolled for services or used VA care.
All demographic variables, including sex, age, race/ethnicity, marital status, and service-connected disability (i.e., a disability caused by an injury or illness incurred in or aggravated by military service), were extracted from electronic medical records. Pain scores, height, and weight were extracted from the vital signs package in the electronic medical record, and screening data were extracted from progress notes using text processing technology. Pain scores are recorded in the electronic medical record by a health technologist who takes the patient's vital signs and asks the patient to rate pain on a scale of 0–10. Pain scores were dichotomized in two ways: any pain (pain score of ≥1) and pain score >4 (clinically relevant pain). Height is measured yearly at medical visits, and weight is recorded at every visit. BMI was calculated from patient height and weight according to the standard BMI calculation: weight (kg)/height (m)2. Anyone with BMI >30.0 kg/m2 is considered obese.22
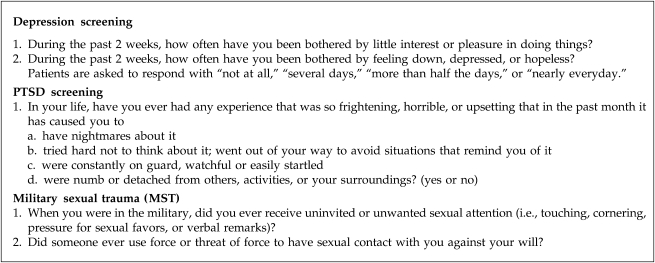
The primary outcome for this study was a positive screen for PTSD, depression, pain, obesity, or MST. Figure 1 shows the questions used for screening at the VA for depression, PTSD, and MST. A positive screen for depression is a score ≥3 points of a possible 6, and a positive screen for PTSD is a positive answer to three of four questions. A positive answer to either question about sexual trauma confers a positive screen. In the VA, an electronic clinical reminder package prompts a provider to do recommended annual screenings for medical and mental health conditions. The clinical reminder and the screening results are automatically stored as text in the medical record progress note. We were, thus, able to capture the clinical reminder data by searching the progress notes using the text indexing and searching tools in the database management system SQL server 2005.23
FIG. 1.
Depression, PTSD, and MST screening questions.
A sample of 25 male and 25 female veterans was randomly selected to perform a check of the reliability of the text processing techniques. The electronic record data were manually reviewed and compared with the text processing results, and a simple kappa was performed to test for the level of agreement beyond chance between the measures. In our validation test comparing electronic text processing techniques with manual chart review, there was very good agreement between the two techniques (mean κ = 0.91). Agreement was strongest for MST (κ = 0.94). The agreement statistics suggest that the electronic text processing methods were a good substitute for chart review in determining the presence of screening for these conditions.
Analyses
Chi-square tests were used to test the significance of differences for all categorical variables. Logistic regression analyses were used with positive screens for pain, PTSD, depression, MST, and obesity as outcomes, with gender as an independent variable. These analyses were adjusted for the potentially confounding effects of age, race, marital status, and service-connected disability. We present odds ratios (OR) and 95% confidence intervals (CI) that were drawn from these logistic regression analyses. All statistical analyses were performed using SAS version 9 (SAS Institute, Inc., Cary, NC).
Results
A total of 197 female and 1032 male veterans of OEF/OIF were seen at least once in a primary care or women's health clinic at VA Connecticut between 2001 and 2006. Female veterans were younger (p < 0.0001), more likely to be black or unknown race than white (p < 0.001), and less likely to be married (p < 0.01) than male veterans (Table 1). More than 90% of all veterans were screened for depression and MST, and just under 90% of male and female veterans were screened for PTSD. Because pain is measured as a vital sign along with height and weight, 100% of veterans were screened for pain. There were no statistically significant differences in screening rates by gender for pain, depression, PTSD, or MST.
Table 1.
Characteristics of VA Connecticut OEF/OIF Veterans, by Gender, 2001–2006
| Overall | Female | Male | p value | |
|---|---|---|---|---|
| Total number | 1229 | 197 | 1032 | |
| Age (mean), years | 32 | 30 | 32 | 0.0004 |
| Race, n (%) | ||||
| Black | 133 (11) | 38 (19) | 95 (9) | |
| White | 788 (64) | 105 (53) | 683 (66) | <0.001 |
| Other | 308 (25) | 54 (27) | 254 (25) | |
| Marital status, n (%) | ||||
| Currently married | 431 (35) | 50 (26) | 381 (37) | |
| Separated/divorced/widowed | 149 (13) | 31 (5.5) | 118 (11.1) | |
| Never married | 637 (52) | 114 (58) | 523 (50) | |
| Unknown | 5 (0.4) | 0 | 5 (0.5) | 0.004 |
| Service-connected disabilitya | 440 (36) | 75 (38) | 365 (35) | 0.468 |
Service-connected disability, disability caused by an injury or illness incurred in or aggravated by military service.
Among the veterans who were screened for depression, PTSD, pain, and MST, female veterans were more likely to screen positive for depression (48% vs. 39%, p = 0.012) but less likely to screen positive for PTSD (21% vs. 33%, p = 0.002). Female veterans were less likely to screen positive for any pain (38% vs. 45%, p < 0.0001), but there was no significant difference by gender in pain scores >4 (clinically significant pain). Positive screening for MST was significantly more common in female than male veterans (14% vs. 1%, p < 0.001). Men were more likely to be obese than women (21% vs. 13%, p = 0.008) (Table 2).
Table 2.
Differences in Rates of Positive Screenings by Gender in VA CT OEF/OIF Veterans
| Female positive screen n (%) | Male positive screen n (%) | p value | |
|---|---|---|---|
| MSTa | 26 (14) | 6 (1) | <0.001 |
| PTSD | 37 (21) | 292 (33) | 0.002 |
| Depression | 92 (48) | 380 (39) | 0.012 |
| BMI >30 | 25 (13) | 215 (21) | 0.008 |
| Any painb | 71 (38%) | 464 (45%) | <0.0001 |
| Pain score >4c | 49 (65) | 286 (62) | 0.608 |
MST, military sexual trauma; PTSD, posttraumatic stress disorder; BMI, body mass index.
Any pain, pain score >0 (scale 0–10).
Pain >4, clinically significant pain.
The age, race, service-connected disability, and marital status adjusted ORs for the association of a positive screen with gender are shown in Table 3. Female gender was associated with a significantly greater odds for a positive screen for depression (OR 1.58, 95% CI 1.15-2.17) and MST (OR 25.6, 95% CI 10.23-63.94) compared with male gender. However, female gender was negatively associated with a positive screen for PTSD (OR 0.55, 95% CI 0.37-0.82) or obesity (OR 0.58, 95% CI 0.37-0.92) compared with male gender.
Table 3.
Age, Race, Service-connected Disability, and Marital Status Adjusted Odds of Positive Screen as Function of Gender among OEF/OIF Veterans at VA Connecticut, October 1, 2001–October 1, 2006
| |
Female vs. male |
|
||
|---|---|---|---|---|
| OR | Lower confidence limit (95%) | Upper confidence limit (95%) | p value | |
| Any paina | 0.72 | 0.52 | 1.00 | 0.05 |
| Pain score >4b | 1.14 | 0.68 | 1.91 | 0.63 |
| PTSD | 0.53 | 0.35 | 0.79 | 0.002 |
| MST | 25.49 | 10.10 | 64.35 | <0.001 |
| Depression | 1.57 | 1.14 | 2.17 | 0.01 |
| BMI>30 | 0.58 | 0.37 | 0.92 | 0.02 |
Any pain, pain score >0 (scale 0–10)
Pain >4, clinically significant pain.
PTSD, posttraumatic stress disorder; MST, military sexual trauma; BMI, body mass index.
Discussion
Our study provides preliminary data about gender differences in positive screening for depression, PTSD, pain, MST, and obesity in returning veterans from Iraq and Afghanistan. These data items were chosen for study because previous research supported a hypothesis that women veterans might be more or less vulnerable to these conditions than male veterans.4–11,14 Knowledge of the prevalence of physical and mental health problems in female veterans will be essential for the VHA as it plans for the predicted increase in the female veteran population in the next few years.2
Screening data indicate that MST and depression were more prevalent among female veterans than male veterans, with 14% of women in the sample screening positive for MST, and nearly half (48%) of all women in the sample screening positive for depression. This is in concordance with national and non-VA (civilian) data sources4 that report that women are at twice the risk of depression regardless of racial or ethnic background or economic status.
In our study, women were less likely to screen positive for PTSD (21% screened women vs. 33% screened men). This was in contrast to our hypothesis (based on primarily civilian data) that has shown twice the rate of PTSD in females as in males after trauma exposure. Two other recently published studies13,14 have shown minimal differences in the prevalence of PTSD among male and female veterans of the Afghanistan and Iraq conflicts. Whether there are gender differences in the risk of PTSD and other mental health problems among women and men exposed to similar levels of combat remains an important unanswered question, but our results suggest that military duty in Iraq confers a lower risk of PTSD in women compared with men. One hypothesis suggests that risk has more to do with the intensity and frequency of combat experience than with gender.3 In addition, it is possible that the “healthy warrior effect” (the disproportionate loss of psychologically unfit personnel early in training)24 might even the playing field for men and women deployed. Our data did not include combat exposure, and disentangling the relationship among PTSD, MST, and combat exposure remains an important research question to be answered.
In our study, there were no statistically significant differences in pain scores between male and female veterans. Although previous studies have reported higher rates of many different pain conditions6–10 in women compared with men, we did not find a significant difference in rates of clinically significant pain among female vs. male veterans screened for pain.
Overall, fewer people met the criteria for obesity in this study in comparison to previous studies of veterans. This may reflect the young age of our population and their recent military discharge, as obesity is more prevalent in older ager groups.25 However, there was a statistically significant difference between male and female veterans who met obesity criteria according to BMI standards. To address the growing problem of obesity, in 2004 the VA introduced the Managing Overweight and/or Obesity for Veterans Everywhere (MOVE) program. Though the MOVE program has been successful in the VA, the VA must continue to adapt this program to meet the needs of younger veterans. Given that previous studies have found an association between PTSD and obesity,26 the VA must continue to adapt its programs for PTSD and other risk factors for obesity among OEF/OIF veterans.
A number of limitations in this work are worth reporting. The results presented in this study are based on veterans of OEF/OIF who have sought care in VA Connecticut over the last 6 years and, thus, are not necessarily representative of veterans in general. Additionally, our data are taken from VA Clinical Reminders and should be interpreted only as screening data. We are not able to determine from electronic screening data whether PTSD, depression, or sexual trauma preexisted, occurred postdeployment, or resulted from a traumatic exposure in OEF/OIF. It is also unknown what proportion of those who screen positive for these conditions are later given a diagnosis of depression or PTSD. However, a recent study of validity of screening instruments reported sensitivity and specificity of the two-item depression screen (score ≥3) ranging from 76% to 93% sensitive and 89% to 95% specific.27 One study of the four-item PTSD screen in OEF/OIF veterans found a sensitivity from 46% to 73% and a specificity as high as 86%.28
As the VA plans for staffing and structure of women's health programs, it will be important to consider gender-specific treatment for certain mental health conditions. Because of the higher prevalence of positive screening for depression and MST in women, the integration of primary care, gynecological care, and mental health services may be particularly important for female veterans. In the past, VA hospitals have cared primarily for male veterans. Many VA healthcare providers are unfamiliar with women veterans' health issues. To attend to this problem, some VA hospitals have opened women's health clinics where women receive full-service care, including primary care, gynecological care, and mental healthcare. Our data underscore the high prevalence of positive screens for depression and military sexual trauma in female veterans and support the need to further evaluate whether women's clinics will be increasingly useful for the treatment of complex and co-occurring physical and mental health issues that may result from military service.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Meehan SM. Improving health care for women veterans. J Gen Intern Med. 2006;21:S1–S2. [Google Scholar]
- 2.Yano E. What does women's health care look like in the Veterans Health Administration?. Results of a national organizational survey; Presented at Academy Health Annual Research Meeting; Jun 10;2008 . [Google Scholar]
- 3.Hoge CW. Clark JC. Castro CA. Commentary: Women in combat and the risk of post-traumatic stress disorder and depression. Int J Epidemiol. 2007;36:327–329. doi: 10.1093/ije/dym013. [DOI] [PubMed] [Google Scholar]
- 4.Weissman MM. Bland RC. Canino GJ, et al. Cross national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–299. [PubMed] [Google Scholar]
- 5.Kessler RC. Sonnega A. Bromet E, et al. Post traumatic stress disorder in the National Co-Morbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 6.Anderson HI. Ejlertsson G. Leden I. Rosenberg C. Chronic pain in a geographically defined general population: Studies of differences in age, sex, social class and pain localization. Clin J Pain. 1993;9:174–182. doi: 10.1097/00002508-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Van Korff M. Dworkin SF. LeResche L. Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988;32:173–183. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 8.LeResch L. Von Korff M. Epidemiology of chronic pain. In: Block AR, editor; Kremer EF, editor; Fernandez E, editor. Handbook of pain syndromes: Biopsychosocial perspectives. Mahwah, NJ: Lawrence Erbaum Associates Inc; 1999. [Google Scholar]
- 9.Gureje O. Von Korff M. Simon GE. Gater R. Persistent pain and well being: A World Health Organization study in primary care. JAMA. 1998;280:147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 10.Crook J. Rideout E. Browne G. The prevalence of pain complaints in a general population. Pain. 1984;18:299–314. doi: 10.1016/0304-3959(84)90824-8. [DOI] [PubMed] [Google Scholar]
- 11.Kimerling R. Gima K. Smith MW. Street A. Frayne S. The Veterans Health Administration and Military Sexual Trauma. Am J Public Health. 2007;97:2160–2166. doi: 10.2105/AJPH.2006.092999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y. Beydoun MA. The obesity epidemic in the United States—Gender, age, socioecomonic, racial/ethnic and geographic characteristics. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 13.Rona RJ. Fear NT. Hull L. Wessely S. Women in novel occupational roles: Mental health trends in UK Armed Forces. Intl J Epidemiol. 2007;36:319–326. doi: 10.1093/ije/dyl273. [DOI] [PubMed] [Google Scholar]
- 14.Seal KH. Bertenthal D. Miner CR. Saunak S. Marmar C. Bringing the war back home. mental health disorders among 103,788 U.S. veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs Facilities. Arch Intern Med. 2007;167:470–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 15.Haskell SG. Heapy A. Reid MC. Papas RK. Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health. 2006;15:862–869. doi: 10.1089/jwh.2006.15.862. [DOI] [PubMed] [Google Scholar]
- 16.Kerns RD. Otis J. Rosenberg R. Reid MC. Veterans' reports of pain and associations with ratings of health risk behaviors: Affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40:371–379. doi: 10.1682/jrrd.2003.09.0371. [DOI] [PubMed] [Google Scholar]
- 17.Lipari RN. Lancaster AR. Armed Forces 2002 Sexual Harassment Survey. Arlington, VA: Defense Manpower Center; [Google Scholar]
- 18.Hankin CS. Skinner KM. Sullivan LM. Miller DR. Frayne S. Tripp TJ. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. J Trauma Stress. 1999;12:601–612. doi: 10.1023/A:1024760900213. [DOI] [PubMed] [Google Scholar]
- 19.Frayne SM. Skinner KM. Sullivan LM, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault while in the military. J Womens Health Gend Based Med. 1999;8:835–845. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- 20.McAuley P. Myers J. Abella J. Froelicher V. Body mass, fitness, and survival in veteran patients: Another obesity paradox? Am J Med. 2007;120:518–524. doi: 10.1016/j.amjmed.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 21.Das S. Kinsinger L. Yancy W, Jr, et al. Obesity prevalence among veterans at Veterans Affairs medical facilities. Am J Prev Med. 2003;28:291–294. doi: 10.1016/j.amepre.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 23.SQL server 2005Microsoft SQL Server 2005 Home. www.microsoft.com/SQL/default.mspx www.microsoft.com/SQL/default.mspx
- 24.Larson GE. Highfill-McRoy RM. Booth-Kewley S. Psychiatric diagnoses in historic, contemporary military cohorts: Combat deployment and the healthy warrior effect. Am J Epidemiol. 2008;167:1269–1276. doi: 10.1093/aje/kwn084. [DOI] [PubMed] [Google Scholar]
- 25.Hedley AA. Ogden CL. Johnson CC. Carroll MD. Curtin LR. Flegal KM. Prevalence of obesity among US children and adolescents and adults 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 26.Vieweg WV. Julius DA. Bates J, et al. Posttraumatic stress disorder as a risk factor for obesity among male military veterans. Acta Psychiatr Scand. 2007;116:483–487. doi: 10.1111/j.1600-0447.2007.01071.x. [DOI] [PubMed] [Google Scholar]
- 27.Corson K. Gerrity MS. Dobscha SK. Screening for depression and suicidality in a VA setting: 2 items are better than one item. Am J Managed Care. 2004;10:839–845. [PubMed] [Google Scholar]
- 28.Bliese PD. Wright KM. Adler AB. Thomas JL. Psychological screening validation with soldiers returning from combat. In: Roy MJ, editor. Novel approaches to the diagnosis and treatment of posttraumatic stress disorder. Amsterdam: IOS Press; 2006. [Google Scholar]