Abstract
We describe lessons learned from a national HIV prevention research program grounded in community-based participatory research, the Men of Asia Testing for HIV (MATH) Study, which targeted self-identified Asian/Pacific Islander men in the United States who have sex with men. We discuss the genesis of and impetus for the study and then describe its various facets, including accomplishments, challenges, and unanticipated consequences. We conclude with a discussion about the real-world practice of community-based participatory research with respect to the MATH Study in particular and similar research in general.
ASIAN/PACIFIC ISLANDERS are the fastest-growing racial/ethnic minority group in the United States, having increased from 1.5% of the total population (3.5 million people) in 1980 to 4.1% (11.8 million) in 2004. Of the 11.8 million Asian/Pacific Islanders living in the country, an estimated 6.7 million (61.4%) are foreign born, and 7 million (63.7%) are older than 5 years and speak an Asian/Pacific Islander language at home. Almost 70% of Asian/Pacific Islanders in the United States reside in areas of the East Coast (particularly in the greater metropolitan areas of Boston, Massachusetts; New York, New York; Philadelphia, Pennsylvania; and Washington, DC), West Coast (particularly in the San Francisco, California, Bay Area and the Los Angeles and San Diego, California, metropolitan areas), or US Pacific (including Hawaii).1
Asian/Pacific Islanders represent 1.1% of all reported AIDS patients in the United States; the Centers for Disease Control and Prevention (CDC) reported in 2005 that the population of men who have sex with men (MSM) accounts for 67% of cumulative AIDS cases among Asian/Pacific Islanders.2 Despite these trends, many Asian/Pacific Islander MSM residing in the United States have never undergone serological testing. One recent study showed that 61.5% of Asian/Pacific Islander MSM with HIV were unaware of their infection at the time of testing.3
Because delayed testing is often associated with an initial presentation of advanced disease, higher health care costs, and disease morbidity, studies of testing behaviors are vital.4 Moreover, Asian/Pacific Islanders are more likely than all other US ethnic groups to be diagnosed with AIDS at the time of HIV diagnosis. As many as 45.6% of Asian/Pacific Islanders with AIDS cite illness as their initial reason for HIV testing (as compared with 38.0% of Whites).5,6 Members of this group are also more likely to have an AIDS-defining Pneumocystis carinii pneumonia diagnosis on first learning of their HIV infection and to initiate AIDS care later than are members of other racial/ethnic groups.7
Delayed HIV/AIDS diagnosis and treatment among Asian/Pacific Islanders are consistent with general health services research findings indicating that immigration status and language barriers in this population are frequently associated with late access to and use of health care services.8–11 In addition, the 1996 Personal Responsibility and Work Opportunity Reconciliation Act (Pub L No. 104-193) has further limited immigrants’ access to many public benefits. Under this act, undocumented aliens and legal immigrants who have been in the United States for 5 years or less are barred from receiving services other than emergency care.12 An unintended consequence of the law has been less than optimal health status among legal immigrants.13,14
Historically, HIV prevention efforts as well as research (both scientific and operational) targeting Asian/Pacific Islanders have been limited in scope.15 For example, to our knowledge, only 1 scientifically based HIV intervention16 and 1 HIV prevention program (as part of the CDC-funded Young Man's Survey)17,18 have targeted Asian/Pacific Islanders.
Under the leadership of the Asian and Pacific Islander American Health Forum (APIAHF), a national advocacy organization dedicated to promoting policy, programs, and research efforts to improve the health and well-being of individuals in Asian/Pacific Islander communities, the first national program directly funded by the CDC (known as Empowerment Through Training and Assistance, or ETTA) was established in 1993. From 1993 to 1999, ETTA built the capacity (e.g., the facility or power to produce, perform, or deploy) of community organizations and health departments to conduct and administer HIV prevention programs targeting Asian/Pacific Islanders. ETTA provided technical assistance and training to community-based organizations (CBOs) working with specific Asian/Pacific Islander populations.
Although the pioneering ETTA program was successful in empowering local communities, many of the specific prevention programs it implemented were not empirically based. In an attempt to fill this void, the Men of Asia Testing for HIV (MATH) Study, a national research and practice model for HIV prevention, collected HIV-related data on Asian/Pacific Islander MSM from 2004 through 2009. In addition to describing the study's conceptual model and operational frame, we discuss lessons learned through achievements and challenges in the first 3 years of the study.
STUDY DESCRIPTION
Given the disproportional impact of HIV among Asian/Pacific Islander MSM in the United States, there is a need for a national data set on MSM. The Asian/Pacific Islander HIV prevention community in the United States hopes to enter another era by building on the experiences of ETTA and developing a community-based participatory research (CBPR) program that will help with the needed data collection.
Coupling community empowerment and scientific principles, CBPR allows scientific inquiry to be conducted with community members in partnership with researchers. CBPR incorporates community members; individuals affected by the health condition, disability, or issue under study; and other key stakeholders in the community's health, all of whom participate fully in each phase of the study (conception, design, conduct, analysis, interpretation, conclusions, and communication of results).19
The CBPR model has been used successfully in various fields of health care ranging from HIV patient care in rural areas to diabetes prevention among adolescents.20 As a result of the growth of the HIV/AIDS epidemic in Asia and the Pacific and among the Asian/Pacific Islander population in the United States, the CBPR model may prove to be a very effective means of HIV prevention and facilitate greater understanding of the specific needs of Asian/Pacific Islanders. That is, Asian/Pacific Islanders, as a small and minority population in the United States, have historically lacked a sufficient voice in mainstream society; the CBPR premise of empowerment is well suited to correcting this inequality.
Goals of the MATH Study Consortium
With the CBPR model as a guide, the MATH Study Consortium sought to collect behavioral and serological data on Asian/Pacific Islander MSM via 7 CBOs in 5 major metropolitan areas. In addition, the MATH Study sought to describe and examine institutional capacity as well as community perceptions and responses to HIV prevention programs.
One of the primary goals of the MATH Study was to build mutually beneficial partnerships that would enhance community readiness to collect empirically based or scientific HIV-related data. National data on Asian/Pacific Islander MSM collected through the study's consortium can be used to augment both local and national HIV surveillance data. Incorporating community involvement into a research study optimizes its scientific relevance as well as the use of data and findings of the study (i.e., the ways in which data should be collected and interpreted that are appropriate and beneficial to a given community). The participation of members of the target population, community stakeholders, and service providers is vital in shaping a culturally relevant study design, producing useful data analyses, and disseminating findings appropriately.
More specifically, the 5 goals of the study were to enhance community-based infrastructure to conduct research in Asian/Pacific Islander communities, build or improve on sustainable HIV testing capacity in Asian/Pacific Islander communities, increase outreach to hard-to-reach populations, develop mutually beneficial partnerships between researchers and community stakeholders, and create relevant data to shape health policies and interventions that affect Asian/Pacific Islander MSM.
MATH Study Operation Framework
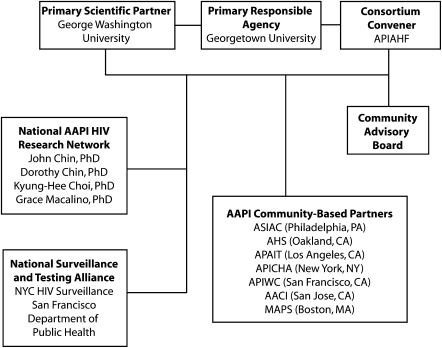
The MATH Study Consortium consisted of 2 principal scientific research partners, the consortium convener, 7 Asian/Pacific Islander community partners, and a community advisory board. These groups brought to the study lessons learned from ETTA with respect to delivering HIV prevention and treatment services to the Asian/Pacific Islander population as well as conducting scientific, community-based research (Figure 1).
FIGURE 1.
Men of Asia Testing for HIV (MATH) Study Consortium.
Note. APIAHF = Asian and Pacific Islander American Health Forum; AAPI = Asian American/Pacific Islander; ASIAC = AIDS Services in Asian Communities; AHS = Asian Health Services; APAIT = Asian Pacific AIDS Intervention Team; APICHA = Asian & Pacific Islander Coalition on HIV/AIDS; APIWC = Asian & Pacific Islander Wellness Center; AACI = Asian Americans for Community Involvement; MAPS = Massachusetts Asians and Pacific Islanders for Health.
Core scientific team.
Georgetown University provided scientific oversight for the MATH Study. George Washington University, replacing the University of California at San Francisco (see the “Structural–Organizational Challenges” section), became a scientific partner. Other original scientific partners included the National Asian/Pacific Islander HIV Research Network and the National Surveillance and Testing Alliance. In addition, APIAHF was a member of the core scientific team, contributing to the decision-making process and executing logistical goals related to CBO partner participation.
Consortium convener.
APIAHF created the MATH Study Consortium to facilitate communication (e.g., troubleshooting) among researchers, the community advisory board, and CBO partners to ensure operational consistency and scientific integrity. Specifically, APIAHF uses a peer-to-peer model that supports national and regional alliances and collaboration and promotes the need for multisector strategies that support and encourage community involvement and engagement. APIAHF has gained a high level of access to CBOs, health departments, and researchers working in Asian/Pacific Islander communities, as well as Asian/Pacific Islander community leaders and stakeholders. APIAHF used its existing infrastructure as well as its experience working with other community partners to strengthen the capacity of the MATH Study.
Responsibilities and associated activities of APIAHF included ensuring that all staff were trained in human participant requirements (e.g., how to handle adverse events), were knowledgeable about various reporting requirements (e.g., HIV reporting, behavioral assessments), and had basic knowledge of outreach strategies. Collectively, these activities promoted the capacity of CBOs to conduct research with a relatively high degree of fidelity.
Community partners.
Two broad criteria were used in selecting CBOs for study participation: first, location in a metropolitan statistical area with a large Asian/Pacific Islander population or a high incidence of AIDS cases among Asian/Pacific Islanders and, second, institutional capacities ranging from comprehensive services (including primary care) to targeted efforts in providing HIV prevention services to Asian/Pacific Islanders. The first criterion allowed maximum opportunities to recruit the proposed number of participants into the study. The second allowed the inclusion of a group of Asian/Pacific Islander CBOs with a varied degree of institutional capacity to conduct scientific or operational research.
Previous research on Asian/Pacific Islander CBOs has identified structural (e.g., funding and policy) and cultural (e.g., denial of risk, racism, and homophobia) barriers to delivering effective HIV/AIDS services and conducting collaborative research. Furthermore, a CBO's type, years of existence, number of full-time-equivalent personnel employed, and involvement in the community planning process are important determinants of its ability to conduct research and deliver services effectively to the diverse Asian/Pacific Islander population.
The 7 agencies in the consortium (Table 1) represented small to large CBOs in terms of overall capacity. Before the MATH Study was launched, all but 1 provided HIV testing, counseling, referral, and prevention services, and although few did so under conditions amenable to rigorous scientific research, most had experience in collaborative research.
TABLE 1.
Collaborating CBOs’ Organizational Capacities: Men of Asia Testing for HIV (MATH) Study
| Agency | Agency Type | Metropolitan Statistical Area | Year Founded | Approximate No. of FTE Employees | HIV Voluntary Counseling/Testing Offered | Populations Served | Language Capacity |
| AIDS Services in Asian Communities | CBO/ASO | Philadelphia | 1995 | 9.0 | On site, mobile | MSM, immigrants, LGBT individuals, API groups | Chinese, Filipino, Vietnamese, other API languages |
| Asian Americans for Community Involvement | CBO/CHC | San Francisco | 1973 | 120.0 | No; referrals | MSM, immigrants, LGBT individuals, people with AIDS | Chinese, Japanese, Vietnamese, other API languages |
| Asian & Pacific Islander Wellness Center | CBO/ASO | San Francisco | 1987 | 45.0 | On site | MSM, immigrants, LGBT individuals, API groups, people with AIDS, families and youth | Chinese, Filipino, Japanese, Korean, Vietnamese, other API languages |
| Asian Health Services | CHC | San Francisco | 1974 | 150.0 | On site | MSM, immigrants, API groups, families and youth | Chinese, Vietnamese, other API languages |
| Asian Pacific AIDS Intervention Team | CBO/ASO | Los Angeles | 1987 | 30.0 | On site, mobile | MSM, immigrants, LGBT individuals, API groups, people with AIDS | Chinese, Japanese, Korean, Vietnamese, other API languages |
| Asian & Pacific Islander Coalition on HIV/AIDS | CBO/ASO | New York City | 1989 | 30.0 | On site | MSM, immigrants, LGBT individuals, API groups, people with AIDS | Chinese, Korean, Vietnamese, other API languages |
| Massachusetts Asians and Pacific Islanders for Health | CBO/ASO | Boston | 1993 | 7.5 | On site, mobile | MSM, immigrants, LGBT individuals, API groups, families and youth | Chinese, Korean, Vietnamese, other API languages |
Note. API = Asian/Pacific Islander; ASO = AIDS service organization; CBO = community-based organization; CHC = community health center; FTE = full-time equivalents; LGBT = lesbian, gay, bisexual, transgender; MSM = men who have sex with men. Data are for 2002–2003. All of the CBOs had experience conducting HIV research.
We intentionally included smaller agencies possessing less capacity to conduct scientific or operational research so that we could describe and examine how formal linkages between these agencies and their larger counterparts might strengthen their ability to conduct such research. Where necessary, the consortium worked collaboratively to improve each CBO's research skills (including study protocol administration), capacity to incorporate various Asian/Pacific Islander languages, and HIV counseling, testing, and referral linkages.
Community advisory board.
The community advisory board consisted of members of the target population and served as the unique link between the community and researchers. The purpose of the board was to maximize the MATH Study's success and relevance by providing the study with the members’ unique perspectives and knowledge of the communities they represent, assisting in identifying outreach venues, and reviewing study materials such as the behavioral survey and protocols. Input from board members helped to identify the best practices for conducting the study, address challenges that might arise, and conduct brainstorming strategies when needed, all through consideration of the cultural attributes and needs of the target population.
ACHIEVEMENTS AND CHALLENGES
The achievements and challenges associated with the 5 goals of the consortium fall into 2 broad categories: structural–organizational (e.g., finances, intercommunication, and decision making) and technical (e.g., science and technology). Unanticipated events and natural group dynamics between collaborators related to these 2 broad categories resulted in a number of scientific or organizational realignments (Tables 2 and 3).
TABLE 2.
Achievements Associated With the Study Consortium's 5 Goals
| Goal | Structural | Organizational | Technical |
| Enhance community-based infrastructure to conduct research in API communities | X | X | X |
| Build or improve on sustainable HIV testing capacity in API communities | X | X | X |
| Increase outreach to hard-to-reach populations | X | X | To be determined |
| Develop mutually beneficial partnerships between researchers and community stakeholders | X | X | X |
| Create relevant data to shape health policies and interventions that affect API MSM | X | X | To be determined |
Note. API = Asian/Pacific Islander; MSM = men who have sex with men.
TABLE 3.
Specific Achievements of and Challenges Faced by the Men of Asia Testing for HIV (MATH) Study Partners
| Partner | Achievements | Challenges |
| Scientific partners | Have obtained consent and approval from all partners to realign the HIV testing component; have obtained consent and approval from all partners to use a paper-and-pencil methodology; have presented preliminary results in conferences; principal investigator has been invited to present the MATH model at several meetings | Limited financial resources; delay in arranging contract with Quest Diagnostics; computer and software problems; problems caused by scientific realignment and reorganization; high staff turnover (initial study period) |
| Consortium convener (Asian and Pacific Islander American Health Forum) | Has done an excellent job in creating a collaborative environment and maintaining the morale of all partners despite structural and technological challenges | Staff turnover |
| Community-based organizations | ||
| AIDS Services in Asian Communities | Has secured approval for anonymous HIV testing to augment existing confidential testing; experience in the use of OraQuick in the study has led to the local health department considering the approval of the use of the Trinity Unigold HIV Test as another testing technology; has enhanced translation capacity into several Asian languages; has served as a resource to recruit volunteers in HIV prevention | Lease problems at the agency's location, resulting in various operational delays |
| Asian Americans for Community Involvement | Has gained county approval to adopt the MATH Study protocol for alternative HIV testing | 3-year approval process resulting from the county having no prior alternative HIV testing model |
| Asian Health Services | Interagency resources embedded in a primary health care agency have been tremendously valuable; has coordinated with other Asian/Pacific Islander AIDS services organizations in the San Francisco Bay Area | High staff turnover (initial study period) |
| Asian & Pacific Islander Coalition on HIV/AIDS | With funding reductions targeting MSM at the city level, the MATH Study has served as a resource to ensure the maintenance of the agency's MSM program | Lease problems at the agency's location, resulting in various operational delays; a series of false-positive HIV test results in New York City prompting city officials to mandate that funded agencies modify their testing practices |
| Asian Pacific AIDS Intervention Team | Has developed an excellent HIV testing referral network in 2 counties | |
| Asian & Pacific Islander Wellness Center | Has integrated the MATH Study into its sexually transmitted infection testing program | High staff turnover (initial study period) |
| Massachusetts Asians and Pacific Islanders for Health | Has developed an excellent HIV testing referral network in the Greater Boston area | High staff turnover (initial study period) |
Note. MSM = men who have sex with men.
Structural–Organizational Achievements
Prior to the MATH Study, Asian Americans for Community Involvement (AACI) in San Jose, California, did not conduct HIV testing. In addition, the county of Santa Clara, of which San Jose is a part, had no alternative HIV testing protocol. After much deliberation and with advocacy from AACI, the county adapted the MATH protocol as the official alternative HIV testing model, resulting in a testing license being granted to AACI; other CBOs in the county are being encouraged to use the MATH protocol. This enhancement of AACI's infrastructure to conduct research involving Asian/Pacific Islanders, although it has taken more than 2 years to achieve, is a major health policy accomplishment.
Before the MATH Study, the Asian Pacific AIDS Intervention Team had an office only in Los Angeles. As a result of the MATH Study, the agency has been able to expand its referral network with other agencies and establish another office in Orange County.
Asian Health Services, a primary health care agency serving Asian/Pacific Islanders in Oakland, California, runs a small HIV prevention program and now is able to draw on regional referral and care resources such as those of the Asian & Pacific Islander Wellness Center in San Francisco as a result of its formal linkage to the MATH Study. The geographical proximity of the 2 agencies allows more proactive communication, leading to improved capacity for sustainable HIV testing in Asian/Pacific Islander communities.
Finally, AIDS Services in Asian Communities in Philadelphia has been able to integrate the MATH Study into other programs of the agency; notably, the translation program is an asset because it reaches out to members of linguistic minority groups to participate in HIV prevention. Other achievements include securing approval for anonymous testing and the potential approval of another alternative testing technology (the Trinity Unigold HIV Test).
Other Achievements
At the annual CDC National HIV Prevention Conference in 2007, the MATH Study team gave presentations focusing on capacity development for community–academic consortium research, findings from the pilot study, and the successes and challenges of pilot testing of the MATH Study consortium model.
Structural–Organizational Challenges
A number of unanticipated structural–organizational challenges (6 interrelated issues are reviewed here) affected implementation of the study. Foremost, budgetary constraints severely restricted a CBO's ability to engage in CBPR. As a result of major reductions in its budget (15%), the MATH Study was unable to fund dedicated staff members at each of the CBOs and instead had to superimpose its research activities onto existing programs.
CBOs were obliged to use existing staff infrastructure to conduct the study with a fee-for-service model. The negative consequences were numerous and included “burnout,” resulting in high staff turnover that hindered the day-to-day operation of the study. With each loss of a staff member, the core scientific team faced the need to find and train a new staff member.
Quest Diagnostics was contracted to conduct confirmatory testing on preliminary positive specimens and process specimens for transportation to the University of California, San Francisco, an original scientific partner. Negotiations to open accounts with Quest Diagnostics in San Francisco, Los Angeles, Philadelphia, Boston, and New York City were initiated in October 2005. Although Quest Diagnostics is a nationally known company, each locale conducts business under its own policies and procedures. After numerous legal delays between the departments of Quest Diagnostics and Georgetown University, the contracts ultimately were placed with the University of California, San Francisco. This step led to further delays in the study's pilot-testing phase until contracts were initiated and signed in September 2006. MATH personnel also had to provide technical assistance to the various Quest Diagnostics sites to bring them into compliance with the MATH protocols.
In addition, because each CBO also received funding from local, state, or national sources (or all of these sources) for HIV prevention and related programs, implementation of the MATH Study inadvertently resulted in additional institutional compliance requirements for HIV reporting. For example, if participants eligible for the MATH Study (a pure research endeavor) were also eligible for other HIV service programs often funded by local and state agencies, the challenge was to ensure that no “double counts” occurred. Consequently, the study's uniform protocol was adjusted to comply with local requirements.
Based on empirical evidence and population statistics, the study's original proposal identified Koreans as one of the target groups. Many agencies, however, did not believe that they possessed the capacity to provide outreach to this group. Although Korean communities share many of the characteristics of other Asian/Pacific Islander communities, they are somewhat distinct in that churches are their primary social outlets. The CBOs we studied, however, had only limited access to Korean churches, and as a result the consortium decided to exclude the Korean community as a target group and replaced it with the South Asian community.
Native Hawaiians and Pacific Islanders were another population that could not be effectively recruited because of the lack of a study CBO in Hawaii, where the majority of these populations are concentrated. The small number of Native Hawaiians and Pacific Islanders recruited at San Francisco sites did not provide sufficient statistical power for cross-population analyses.
Although the funding agency, the National Institutes of Health, endorses and encourages CBPR, its organizational structures are not set up in this manner, and the MATH Study ultimately employed a hierarchical structure (i.e., Georgetown University acted as the study's prime agency) so that the partnership would be equal in principle if not necessarily in practice. Use of the fee-for-service model further reinforced the study's hierarchical inclinations. In light of the overall structural–organizational constraints, some of the study's protocols had to be modified, which at times fomented tension between members of the consortium given that such decisions were ultimately made by the principal investigator.
One consequence of these modifications and the resulting tension was that the principal investigator, in consultation with the National Institutes of Health, replaced the University of California, San Francisco, with George Washington University. To encourage continued support from the CBOs, the principal investigator recruited a prominent and well-respected community leader, Daniel Bao, to serve as senior strategic advisor and liaison to the community during the difficult transition period. Bao was able to persuade all of the partners to continue their strong support of this historic project.
Technical Challenges
The study experienced numerous unanticipated technical challenges. For example, the automatic data collection technology (audio computer-assisted self-interview) initially used in the study hindered its progress, in part because CBO staff members were not familiar with the technology. In the course of using the technology to implement the MATH Study, programming the behavioral survey instrument into the study computers presented time-consuming and costly challenges. The difficulties associated with the protocol changes stemming from these challenges were compounded by translation and software issues beyond our control, causing delays to the pilot-testing phase of the study and in turn delaying the start of data collection.
The cost of translating the behavioral survey instrument into Chinese, Vietnamese, and Japanese far exceeded the amount budgeted, primarily as a result of inconsistencies with back-translation from those languages into English as well as the discovery that entering Vietnamese characters mimicked commands for the survey software. This situation further complicated and delayed the programming of the behavioral survey instrument and added costs.
Consequently, the protocol was modified so that rather than housing the database within the tablet PCs distributed to the CBOs and subsequently transferring it to our central servers as previously planned, MATH data collected from participants via a Web-based survey were entered and stored in central servers. During the initial stages of data collection, we found that if a study participant did not engage in computer activity for more than 10 minutes (e.g., he or she took too long to respond to a question or temporarily stopped the survey for a bathroom break), the computer timed out. The participant then was asked to log in again and to restart the survey where he or she left off.
Although MATH Study staff members were able to assess and address most of the challenges just described, subsequently it was discovered that the study computers’ hardware was flawed. This flaw was not disabling initially, but if it had been left unaddressed there was a strong possibility that the study's computers would have crashed, at which point the study would have come to a complete halt.
After weighing the pros and cons of various options, the MATH Core Scientific Team decided to move from the computerized behavioral survey instrument to a more traditional paper-and-pencil version. Georgetown University's institutional review board approved the streamlined instrument, and staff and materials were prepared for a relaunch of the data collection process. Among the advantages of moving to a paper-based study were the ability to use the existing translations in the behavioral survey instrument and the capability to offer the survey in Chinese and Vietnamese.
During a March 2008 site visit by the principal investigator to our Los Angeles site, staff members consistently praised the user-friendly nature of the paper-and-pencil survey methodology. In fact, the amount of data collected in the 6-month period between October 2007 and March 2008 was 4 times the volume collected via the computer-assisted survey methodology.
Unanticipated Challenges
A few of the CBOs experienced building rental problems (e.g., the landlord selling the building), thus resulting in various operational delays. More serious was that a number of agencies in New York City experienced a series of false-positive HIV test results when the OraQuick oral HIV testing technology was used. In response, New York City health officials mandated that their funded agencies (including our New York City partner, the Asian & Pacific Islander Coalition on HIV/AIDS) switch to finger-stick testing. Although the MATH Study was a scientific investigation, all of our partners had to balance local practices and mandates with the study's objectives.
DISCUSSION
After dealing with many early challenges, the MATH Study was fully under way in 2008. The momentum created by accelerating data collection reenergized staff members of the CBOs. The user-friendly nature of both the paper-and-pencil survey methodology and the streamlined protocols was welcomed by CBO staff. In addition to their success in collecting data intended to meet 2 of the study's scientific aims (determining HIV prevalence rates among Asian/Pacific Islander MSM and examining sociocultural factors associated with HIV risks among these individuals), all community partners believed that they were prepared to engage in a systematic evaluation of the consortium model (a by-product of developing mutually beneficial partnerships between the researchers and community stakeholders, one of the study's goals).
In addition to increasing the body of knowledge on HIV/AIDS risk behaviors among Asian/Pacific Islanders, the MATH Study provides pragmatic insights into the CBPR model for conducting research. Yet, despite CBPR's strengths and potential for enhancing multisite research, the model was unable to anticipate large structural issues or barriers. The MATH Study has demonstrated that shifts in external (political) dynamics can profoundly affect researchers’ ability to conduct scientific research uniformly. For example, as mentioned, the consortium was obliged to modify the study protocol to accommodate activities of CBOs required by other funding sources. It is likely that changes in state and federal policies would produce similar effects.
Funding was the primary determinant of such operational variables as staffing levels and availability of study materials in foreign languages. Because of limited funding, coupled with the multitude of Asian/Pacific Islander languages and differing CBO language capacities, the consortium had to choose certain languages for translation of study materials while excluding others. Fortunately, other studies targeting communities that speak the same language will not be forced to deal with this specific challenge.
Cultural norms and values also can act as obstacles to executing CBPR. For example, despite their relatively large presence in the Asian/Pacific Islander community, Koreans were difficult to recruit through the existing paradigm because much of the community's social life centers around church activities, where our CBO partners had limited access.
Finally, because of its strongly collaborative nature, CBPR in particular must pay attention to the need to balance operational efficacy and scientific rigor. Although the symbiosis gained through partnerships is one of the primary strengths of CBPR, differing priorities between partners can sometimes create problems (e.g., strained relationships). Still, we believe there is little doubt that the benefits of partnerships strongly outweigh any handicaps and that the CBPR model of research has the potential to benefit many communities in addition to Asian/Pacific Islanders.
The ultimate beneficiaries of the MATH Study are Asian MSM who have gained access to early HIV testing and will be given feedback on the social–behavioral and psychological risk factor portion of the study. With the study's achievements in mind, the consortium continues to work on survey data and HIV testing services with the support of the National Institutes of Health.
Acknowledgments
Preparation of this article was supported in part by grants from the National Institutes of Health (R01HD046354) and the Emory Center for AIDS Research (P30 AI050409).
The MATH Study Consortium consists of the following organizations: AIDS Services in Asian Communities (Philadelphia, PA), Asian Americans for Community Involvement (San Jose, CA), Asian Health Services (Oakland, CA), the Asian & Pacific Islander Coalition on HIV/AIDS (New York, NY), the Asian Pacific AIDS Intervention Team (Los Angeles, CA), the Asian and Pacific Islander American Health Forum (San Francisco, CA), the Asian & Pacific Islander Wellness Center (San Francisco, CA), Massachusetts Asians and Pacific Islanders for Health (Boston, MA), Georgetown University, George Washington University, and Emory University.
Note. All opinions are those of the authors and do not necessarily reflect the positions of the funding agencies.
Human Participant Protection
This study was approved by Georgetown University's institutional review board.
References
- 1.Current Population Survey, Annual Social and Economic Supplement. Washington, DC: US Census Bureau, Population Division; 2004 [Google Scholar]
- 2.Centers for Disease Control and Prevention HIV/AIDS Among Asians and Pacific Islanders. Available at: http://www.cdc.gov/hiv/resources/factsheets/PDF/API.pdf. Accessed April 9, 2010
- 3.Do TD, Choi K-H, Chen S. Unrecognized HIV infection and barriers to testing among young Asian and Pacific Islander men who have sex with men. Paper presented at: International Conference on AIDS, July 2002, Barcelona, Spain [Google Scholar]
- 4.Centers for Disease Control and Prevention Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–332 [PubMed] [Google Scholar]
- 5.Wong FY, Campsmith ML, Nakamura GV, Crepaz N, Begley E. Reasons for testing and awareness of care-related services among a group of HIV-positive Asian Americans and Pacific Islanders in the United States: findings from a supplemental HIV/AIDS surveillance project. AIDS Educ Prev. 2004;16(5):440–447 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Diagnosis and reporting of HIV and AIDS in states with HIV/AIDS surveillance—United States, 1994–2000. MMWR Morb Mortal Wkly Rep. 2002;51(27):595–598 [PubMed] [Google Scholar]
- 7.Eckholdt HM, Chin JJ, Manzon-Santos JA, et al. The needs of Asians and Pacific Islanders living in New York City. AIDS Educ Prev. 1997;9(6):493–504 [PubMed] [Google Scholar]
- 8.Huang ZJ, Yu SM, Ledsky BSK. Health status and health service access and use among children in U.S. immigrant families. Am J Public Health. 2006;96(4):634–640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu SM, Huang ZJ, Singh GK. Health status and health services utilization among US Chinese, Asian Indian, Filipino, and other Asian/Pacific Islander children. Pediatrics. 2004;113(1):101–107 [DOI] [PubMed] [Google Scholar]
- 10.Yu SM, Bellamy H, Schwalberg RH, Drum M. Factors associated with use of preventive dental and health services among U.S. adolescents. J Adolesc Health. 2001;29(6):395–405 [DOI] [PubMed] [Google Scholar]
- 11.Yu SM, Huang ZJ, Schwalberg RH, Nyman RM. Parental English proficiency and children's health services access. Am J Public Health. 2006;96(8):1449–1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guendelman S, Schauffler HH, Pear M. Unfriendly shores: how immigrant children fare in the U.S. health system. Health Aff. 2001;20(1):257–266 [DOI] [PubMed] [Google Scholar]
- 13.Kandula NR, Grogan CM, Rathouz PJ, Lauderdale DS. The unintended impact of welfare reform on the Medicaid enrollment of eligible immigrants. Health Serv Res. 2004;39(5):1509–1526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kullgren JT. Restrictions on undocumented immigrants’ access to health services: the public health implications of welfare reform. Am J Public Health. 2003;93(10):1630–1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong FY, Chng CL, Low W. A profile of six community-based HIV prevention programs targeting Asian and Pacific Islander Americans. AIDS Educ Prev. 1998;10(suppl 3):61–76 [PubMed] [Google Scholar]
- 16.Choi K-H, Lew S, Vittinghoff E, et al. The efficacy of brief group counseling in HIV risk reduction among homosexual Asian and Pacific Islander men. AIDS. 1996;10(1):81–87 [DOI] [PubMed] [Google Scholar]
- 17.Do TD, Hudes ES, Proctor K, Han C-S, Choi K- H. HIV testing trends and correlates among young Asian and Pacific Islander men who have sex with men in two U.S. cities. AIDS Educ Prev. 2006;18(1):44–55 [DOI] [PubMed] [Google Scholar]
- 18.McFarland W, Chen S, Weide D, Kohn RP, Klausner JD. Gay Asian men in San Francisco follow the international trend: increases in rates of unprotected anal intercourse and sexually transmitted diseases, 1999–2002. AIDS Educ Prev. 2004;16(1):13–18 [DOI] [PubMed] [Google Scholar]
- 19.National Institute of Environmental Health Sciences Environmental justice and community-based participatory research. Available at: http://www.niehs.nih.gov/research/supported/programs/justice/. Accessed April 9, 2010
- 20.Westfall JM, VanVorst RF, Main DS, Herbert C. Community based participatory research in practice based research networks. Ann Fam Med. 2006;4(1):8–14 [DOI] [PMC free article] [PubMed] [Google Scholar]