Abstract
Objectives. We examined the relationships between substance abuse treatment, abstinence, and mortality in a sample of individuals entering treatment. We also estimated overall mortality rates and the extent to which they varied according to demographic, clinical severity, and treatment variables.
Methods. We used data from a 9-year longitudinal study of 1326 adults entering substance abuse treatment on the west side of Chicago, of whom 131 died (11.0 per 1000 person-years). Baseline predictors, initial and long-term treatment response, and substance use patterns were used to predict mortality rates and time to mortality.
Results. Older age, health problems, and substance use were associated with an increased risk of mortality, and higher percentages of time abstinent and longer durations of continuous abstinence were associated with a reduced risk of mortality. Treatment readmission in the first 6 months after baseline was related to an increased likelihood of abstinence, whereas readmission after 6 months was related to a decreased likelihood of abstinence, suggesting that treatment timing is significant.
Conclusions. Our findings suggest the need to shift the addiction treatment field from an acute care model to a chronic disease management paradigm and the need for more aggressive screening, intervention, and addiction management over time.
The strong association of illicit drug use with other prominent causes of mortality (e.g., tobacco and alcohol use, accidents, and high-risk sexual behaviors), as well as its contribution to significant chronic health problems (e.g., cancer, heart disease, liver disease, and respiratory illness), renders it one of the most fundamental mortality risks.1,2 The statistics are staggeringly clear: individuals with a drug dependence diagnosis die on average 22.5 years earlier than those without such a diagnosis.3 Furthermore, mortality in the subgroup of individuals with substance use disorders who enter substance abuse treatment is 3 or more times higher than that in the US population as a whole after adjustment for age.4–15
How should US public health officials address the insidious mortality risk associated with illicit drug use, which currently threatens the approximately 6.9 million people (2.8% of the US population) who meet the diagnostic criteria for substance use disorders?2,16 Before a coherent and effective public health strategy to address the mortality risk associated with drug use can be formulated, the research community must achieve a greater understanding of the specific mechanisms that drive the association between addiction treatment and reduced mortality.
Although the relationship between addiction treatment, abstinence, and mortality is complex, we do know that the variables that may affect this relationship include the point in their addiction career at which people enter treatment and the amount of treatment they receive. A large number of studies as well as expert reviews of the literature in the past 2 decades have consistently concluded that participation in substance abuse treatment increases the likelihood of short-term abstinence.17–25 Particularly, more intense initial treatment, higher cumulative treatment dosage, and early reintervention have been associated with sustained abstinence over multiple years.26–29 A smaller body of evidence also indicates that those who enter treatment sooner and stay in longer are less at risk for mortality.26,30
In addition, the US Preventive Services Task Force, which is charged with evaluating the benefits of strategies that address the leading causes of mortality, found “good evidence” that drug use is related to mortality and that various treatments designed to reduce illicit drug use in the short term are effective.31 Nevertheless, it concluded that insufficient evidence exists to link treatment to longer term improvements in morbidity (prevalence and duration of abstinence) and, consequently, reduced mortality.
A rigorous examination of the relationships between illicit drug use, treatment, and long-term outcomes, including mortality, requires consideration of the variables that affect these relationships not only in the short term but also in the long term. One such group of variables consists of an individual's characteristics upon entering treatment: age, gender, living arrangements, employment, criminal justice history, substance use history, and preexisting health conditions.6,7,32–34
In addition to this first set of variables, results from a range of studies indicate the need to consider various aspects of treatment participation. Because substance use disorders are best conceptualized as chronic conditions, a number of addiction scientists have argued that research in this area adopt a life course, developmental perspective to assess the role of treatment in substance use and related outcomes.35–39 From this perspective, mortality risk among substance users may be related to their initial response to treatment and their cumulative duration of abstinence. Duration of sustained abstinence may also play a role in mortality risk.
Finally, previous studies have shown that longer periods of abstinence (% of days whether consecutive or not) and longer durations of sustained abstinence (consecutive days only) yield benefits in a wide array of physical, psychological, and social functioning domains, including social network improvements, increased vocational involvement, and better mental health.27,28,40–43 Despite the knowledge that such changes represent an increase in recovery capital that may be related to a wide range of health outcomes with an impact on mortality risk, it remains unclear whether characteristics of an individual's abstinence (e.g., timing or duration), the proximal goal of treatment, mediate that association.
Capitalizing on a 9-year longitudinal investigation of individuals presenting to community-based substance abuse treatment facilities, we addressed 2 research questions in this study: (1) What are the overall mortality rates in this sample, and how do they vary according to demographic, clinical severity, and treatment variables? and (2) How and to what extent do treatment and abstinence (i.e., the proximal outcome of treatment) mediate these relationships?
METHODS
The data we used were from a study that included a stratified sample of 1326 adults (participation rate: 85%) recruited between 1996 and 1998 from sequential patients admitted to a network of 22 addiction treatment programs operating on the west side of Chicago (10 outpatient drug-free programs, 5 intensive outpatient drug-free programs, 3 methadone maintenance clinics, 2 short-term inpatient clinics, 1 long-term inpatient program, and 1 halfway house).28,35,44–47 Participants were reinterviewed at 6 months, 2 years, and annually thereafter for 9 years (follow-up rates per wave were 92%–96%). The follow-up was conducted from 1996 to 2007.
Baseline data on all 1326 participants and 131 deaths (9.9%) over the course of the 9-year follow-up were available to address our first research question (centering on mortality rates overall and by subgroup). To address our second research question (centering on multivariate relationships between baseline and intervening variables), we focused on a subset of 1222 (92%) participants for whom we had all data from baseline, from the 6-month follow-up, and from at least 1 follow-up from the year before death or the final study observation (i.e., so that we could estimate the risk of mortality in the subsequent 12 months).
Sample
Baseline data showed that participants were mostly women (59.2%), aged between 30 and 49 years (68.7%; mean = 34.3 years), African American (87.5%), and unemployed (92.0%); most had never been married (65.3%). About half had earned a high school degree or its equivalent (48.7%), and 32.2% considered themselves homeless, with 11.7% having lived on the street or in a homeless shelter in the 6 months prior to intake. Sizable percentages of the participants reported histories of physical (24.3%), emotional (34.6%), and sexual (18.8%) victimization.
On average, participants had initiated drug use at age 16.8 years, had used regularly for 14.4 years, and had used regularly for 18 of the preceding 30 days. Most (53.2%) reported prior addiction treatment, including 27.4% with 2 or more prior treatment episodes. More than 98% of participants had used multiple substances in their lifetime, and 76% had done so in the 30 days before intake. The most common substances used 5 or more times in the 30 days before intake were cocaine (34.8%), alcohol (20.7%), heroin (31.1%), and marijuana (8.5%). Few participants (3.8%) reported injecting drugs in the 6 months prior to intake. Other problems included major depression (36.4%); generalized anxiety disorder (36.3%); a history of criminal justice involvement, including arrests (76.9%), convictions (49.9%), and incarceration of 1 or more months (39.1%); and current probation or parole status (25.0%).
Data Collection
The main study instrument was an augmented version of the Addiction Severity Index,48,49 which includes questions on age, lifetime and past-month problem severity, employment, family situation, and psychiatric functioning. We modified the instrument to collect more detailed data on treatment and incarceration histories, service use, high-risk behaviors, mental distress, pregnancy, illegal activity, criminal justice involvement, recovery environment, drug use practices (or lack thereof) of friends, impact of substance use on relationships, type of disability or chronic condition, body mass index, motivation, and coping.
The Addiction Severity Index drug (α = 0.71), alcohol (α = 0.86), and psychiatric (α = 0.83) composites have been shown to have good internal consistency,28,47 with self-reported use of outpatient, methadone, and residential treatment in the first 6 months after intake correlating well (> 0.7) with treatment records. In a substudy of 259 participants, there was good concordance between urine tests and self-reported rates of substance use both overall (73%) and specifically with respect to opioids (82%), cocaine (68%), and marijuana (68%). The test–retest reliability was also good (κ values ranged from 0.62–0.86) across the subscales, meeting or exceeding the instrument's published rates of internal consistency (0.6–0.9) and test-retest reliability (0.5–0.9).49 The Addiction Severity Index composite scores and other measures have been shown to be sensitive to duration of abstinence as well.35
The follow-up protocol50 involved routine contact with each participant between interviews. If the participant could not be contacted, we attempted to reach collaterals and service agencies with which the participant had dealings to reestablish contact. If we learned from these sources or public records that a client had died, we recorded the period of death (i.e., at what point in the study the death occurred); however, we did not record the date of death or information on the cause of death. Participants received $50 for completing for the interview, $10 for completing it on time, $15 for a urine sample, and $5 for confirming their appointment.
Analytic Approach
For our first research question (focusing on mortality rates overall and by subgroup), we limited the analysis to baseline predictors measured at study intake. For our second research question (focusing on multivariate relationships between baseline and intervening variables), we included variables from baseline, the first 6 months of treatment, and the remaining months of the study (months 7–96) so that we could distinguish between early and later treatment. These variables were used to predict the likelihood of achieving at least 1 year of abstinence. Only variables that remained significant in the multivariate model were included. This analysis was then repeated with the addition of variables representing percentage of time abstinent and years of continuous abstinence to predict the risk of mortality in the subsequent 12 months. SPSS version 17 (SPSS Inc, Chicago, IL) was used to conduct all logistic regression analyses.
Odds ratios (ORs) significantly greater than 1 suggest an increased likelihood of the respective dependent variable, and odds ratios significantly less than 1 suggest a reduced likelihood of the respective dependent variable. To test the extent to which years of sustained abstinence mediated the outcomes assessed, we followed the recommendations of Baron and Kenny51 and tested the final model for predicting mortality with and without this variable to evaluate the impact on the overall fit and individual parameters.
RESULTS
We assessed mortality rates (overall and by subgroup) in the study sample as well as relationships between the different categories of variables assessed.
Baseline Predictors of Mortality
Of the 1326 participants, 131 (9.9%) died over the course of the 9-year study (11.0 per 1000 person-years). Table 1 presents mortality rates and bivariate odds of mortality over the course of the study as a function of sociodemographic characteristics and functioning at intake. Being older than 30 years nearly doubled the risk of mortality (OR = 1.98), whereas being African American was associated with reduced odds of mortality (OR = 0.52).
TABLE 1.
Mortality Rates by Intake Characteristics: Adults in Addiction Treatment Programs, Chicago, IL, 1996–2007
| Characteristic | Participants, No. (%) | Person-Years | No. of Deaths | Deaths per 1000 Person-Years | OR (95% CI) |
| Total | 1326 (100) | 11 934 | 131 | 11.0 | |
| Gender | |||||
| Men | 541 (41) | 4869 | 64 | 13.1 | 1.39 (0.99, 1.96) |
| Women (Ref) | 785 (59) | 7065 | 67 | 9.5 | 1.00 |
| Age, y | |||||
| >30 | 892 (67) | 8028 | 105 | 13.1 | 1.98* (1.29, 3.04) |
| 18–30 (Ref) | 434 (33) | 3906 | 26 | 6.7 | 1.00 |
| Race/ethnicity | |||||
| African American | 1160 (87) | 10 440 | 103 | 9.9 | 0.52* (0.34, 0.80) |
| Other (Ref) | 166 (13) | 1494 | 28 | 18.7 | 1.00 |
| Alcohol/other drug use, y | |||||
| ≥20 | 344 (26) | 3096 | 44 | 10.7 | 1.64* (1.04, 2.58) |
| 10–19 | 561 (42) | 5049 | 54 | 10.7 | 1.23 (0.80, 1.90) |
| 0–9 (Ref) | 421 (32) | 3789 | 33 | 8.7 | 1.00 |
| Alcohol use only, y | |||||
| ≥20 | 636 (49) | 5724 | 54 | 9.4 | 0.97 (0.67, 1.54) |
| 10–19 | 364 (28) | 3726 | 30 | 8.1 | 1.85* (1.21, 2.83) |
| 0–9 (Ref) | 300 (23) | 2700 | 44 | 16.3 | 1.00 |
| Opioid use only, y | |||||
| ≥20 | 1058 (80) | 9522 | 86 | 10.1 | 1.68* (1.01, 2.80) |
| 10–19 | 162 (12) | 1458 | 21 | 14.4 | 3.31* (2.00, 5.48) |
| 0–9 (Ref) | 106 (8) | 954 | 24 | 25.2 | 1.00 |
| Years to first treatment episode | |||||
| ≥20 | 451 (34) | 4059 | 59 | 14.5 | 1.97* (1.14, 3.38) |
| 10–19 | 621 (47) | 5589 | 55 | 9.8 | 1.33 (0.77, 2.29) |
| 0–9 (Ref) | 254 (19) | 2286 | 17 | 7.4 | 1.00 |
| History of overdose or delirium tremens | |||||
| Yes | 160 (12) | 1440 | 25 | 17.4 | 1.73* (1.12, 2.69) |
| No (Ref) | 1166 (88) | 10 494 | 106 | 10.1 | 1.00 |
| Physical disability | |||||
| Yes | 216 (16) | 1944 | 38 | 19.5 | 2.12* (1.45, 3.10) |
| No (Ref) | 1110 (84) | 9990 | 93 | 9.3 | 1.00 |
| History of chronic illness | |||||
| Yes | 491 (37) | 4419 | 76 | 17.2 | 2.37* (1.67, 3.36) |
| No (Ref) | 835 (63) | 7515 | 55 | 7.3 | 1.00 |
| Hospitalization in prior 6 mo | |||||
| Yes | 193 (15) | 1737 | 40 | 23.0 | 2.62* (1.80, 3.81) |
| No (Ref) | 1133 (85) | 10 197 | 91 | 8.9 | 1.00 |
| Addiction Severity Index score | |||||
| Above median medical | 420 (32) | 3780 | 59 | 15.6 | 1.78* (1.26, 2.52) |
| Below median medical (Ref) | 906 (68) | 8154 | 72 | 8.8 | 1.00 |
| Living arrangement | |||||
| Living alone | 330 (25) | 2970 | 47 | 15.8 | 2.12* (1.29, 3.47) |
| Living with other adults | 642 (48) | 5778 | 60 | 10.4 | 1.38 (0.86, 2.22) |
| Living with any children (Ref) | 354 (27) | 3186 | 24 | 7.5 | 1.00 |
| Poverty status | |||||
| Below 50% of poverty linea | 228 (17) | 2052 | 46 | 22.4 | 2.64* (1.84, 3.80) |
| Above 50% of poverty linea (Ref) | 1098 (83) | 9882 | 85 | 8.6 | 1.00 |
| Any illegal acts for money in prior 6 mo | |||||
| Yes | 233 (18) | 2097 | 29 | 13.8 | 1.38 (0.89, 2.14) |
| No (Ref) | 1093 (82) | 9837 | 102 | 10.4 | 1.00 |
| History of violent offense | |||||
| Yes | 392 (30) | 3528 | 50 | 14.2 | 1.48* (1.04, 2.11) |
| No (Ref) | 934 (70) | 8406 | 81 | 9.6 | 1.00 |
Note. CI = confidence interval; OR = odds ratio.
The poverty line is based on the US Department of Health and Human Services (HHS) poverty guidelines.51
*P < .05.
The risk of mortality increased with more years of alcohol use and more years of opioid use prior to baseline. We also found positive relationships between mortality and a longer amount of time from first use to first seeking treatment and having a history of overdose or delirium tremens. In addition, individuals with physical disabilities, chronic medical illnesses (e.g., seizures, asthma, emphysema, high blood pressure, heart disease, cirrhosis, pancreatitis, diabetes), hospitalizations in the 6 months before intake, and Addiction Severity Index medical composite scores above the median were at significantly increased risk of mortality, as were those who were living alone, were living below the poverty line (as defined by the US Department of Health and Human Services52), had engaged in any illegal acts for money, or had been charged with a violent act in the 6 months before intake.
Predictors of Sustained Abstinence
Although percentage of time abstinent in the overall sample increased from 55% during the 6 months before intake to 79% at the end of the study period, only 418 of the 1222 participants (34%) included in the multivariate analysis achieved 1 or more years of abstinence. Odds ratios for the multivariate logistic regression tests associated with sustained abstinence or death in the subsequent 12 months are displayed in Table 2. The rows show the predictors that were significant in the multivariate model after stepwise selection. The predictors are organized by time frame: baseline, months 0 to 6 (initial treatment response), and months 7 to 96 (long-term response). At baseline all measures from Table 1 were considered, but only those that remained statistically significant in the multivariate model are included in Table 2. For the latter 2 time periods, we also considered number of substance abuse treatment episodes, percentage of time in treatment and in the hospital, and involvement in illegal activity for money.
TABLE 2.
Predictors of Sustained Abstinence and Mortality: Adults in Addiction Treatment Programs, Chicago, IL, 1996–2007 (n = 1222)
| Predictor | Sustained Abstinence,a OR (95% CI) | Death in the Subsequent 12 Mo,b OR (95% CI) |
| Baseline | ||
| Age at or before intake | … | 1.82 (1.40, 2.37) |
| Any preexisting chronic illness (yes vs other) | … | 1.85 (1.21, 2.84) |
| Illegal activity for money in prior 6 mo | … | 1.14 (1.00, 1.30) |
| Mo 0–6: no. of treatment episodes | 1.32 (1.11, 1.56) | … |
| Mo 7–96c | ||
| % of time hospitalized | 0.14 (0.03, 0.70) | 14.45 (3.89, 53.70) |
| % of d of illegal activity for money | 0.77 (0.66, 0.90) | … |
| No. treatment episodes | 0.75 (0.69, 0.81) | 0.68 (0.59, 0.79) |
| % of time in treatment | 1.42 (1.14, 1.77) | 1.68 (1.24, 2.25) |
| % of time abstinentd | … | 0.74 (0.69, 0.79) |
| Year before final observation or death: y of sustained abstinenced | … | 0.81 (0.71, 0.93) |
Note. CI = confidence interval; OR = odds ratio. All ORs are significant at P < .05. Sustained abstinence refers to abstinence of 12 months or more. An ellipsis indicates that the variable is not in this particular equation.
OR of 1 or more represents increased likelihood of achieving 1 or more years of abstinence.
OR of 1 or more represents increased likelihood of mortality in the subsequent 12 months.
Measured in the year before final observation or death (n = 1222).
Not used to predict 1 or more years of abstinence to avoid being circular.
Examination of the model including proximal measures revealed that no baseline risk factors were significantly related to the likelihood of achieving sustained abstinence. However, a higher number of substance abuse treatment episodes during the first 6 months of the study (OR = 1.32 per episode) and a longer amount of time spent in treatment over the course of the study (OR = 1.42) increased the likelihood of achieving sustained abstinence. By comparison, after the first 6 months of the study, the likelihood of sustaining abstinence decreased as the number of subsequent treatment episodes increased (OR = 0.75 per episode), the percentage of time spent hospitalized increased (OR = 0.14 per 10-percentage-point change), and the percentage of days involved in illegal activity for money increased (OR = 0.77 per 10-percentage-point change).
Predicting Time to Mortality
Table 2 also provides odds ratios significantly associated with mortality in the subsequent 12 months. This analysis included all of the variables from the baseline model just discussed, percentage of time abstinent in the initial and subsequent periods (as measures of harm reduction), and years of sustained abstinence at the final observation before mortality or the final observation minus 1 year. Mortality in the subsequent 12 months was associated with older age at intake (OR = 1.82), the presence of a preexisting chronic illness (OR = 1.85), and the amount of time a person engaged in illegal activity for money in the 6 months prior to intake (OR = 1.14).
Although none of the initial treatment response variables remained significant in the multivariate model, mortality in the subsequent 12 months was associated with percentage of time spent in the hospital (OR = 14.45) and in substance abuse treatment (OR = 1.68) over the long term (months 7–96). We interpreted these 2 findings as markers of nonresponse to treatment. Over the long term, the likelihood of mortality decreased with additional substance abuse treatment episodes (OR = 0.68), more time abstinent (OR = 0.74), and more years of continuous abstinence (OR = 0.81). Thus, the extent to which people with substance abuse problems were readmitted combined with their response to treatment (as both a percentage of time and a continuous period) was associated with a reduced risk of mortality.
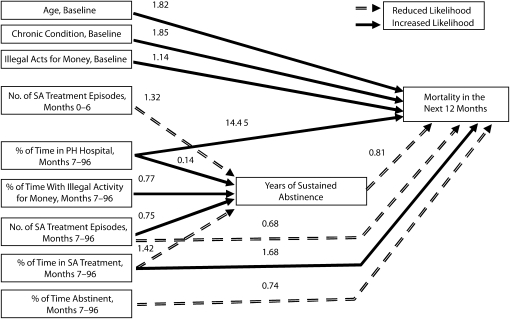
Relationships Between Risk, Treatment, Abstinence, and Mortality
Figure 1 provides a graphic summary of the numeric findings presented in Table 2 to help illustrate the complex relationships described here. A complex relationship existed between treatment, abstinence, and mortality in the multivariate analyses. The likelihood of mortality decreased directly as the total number of treatment episodes increased (OR = 0.68 per episode) but increased with increasing percentage of time in treatment (OR = 1.68 per 10-percentage-point change). Treatment also had an indirect effect via the reduced risk of mortality associated with both continuous abstinence (OR = 0.81 per year) and percentage of time abstinent, even when it was episodic (OR = 0.74 per 10-percentage-point change). The likelihood of sustained abstinence increased with increases in the number of treatment episodes in the first 6 months (OR = 1.32 per additional episode) and in the percentage of time in treatment over the study period (OR = 1.42 per 10-percentage-point change). However, the number of times a person returned to treatment between 6 months and 8 years after intake was associated with a lower likelihood of eventually achieving sustained abstinence (OR = 0.75 per additional episode). Thus, the timing of readmission matters.
FIGURE 1.
Summary of the relationships observed: adults in addiction treatment programs, Chicago, IL, 1996–2007.
Note. PH = physical health; SA = sustained abstinence. Path coefficients are odds ratios from Table 2 (n = 1222). Odds ratio of 1 or more indicate higher rates of achieving 1 or more years of sustained abstinence or a high risk of mortality in the subsequent 12 months. All odds ratios are significant at P < .05.
We used Baron and Kenny's approach to assess the extent to which years of sustained abstinence mediated the relationships between risk, treatment, and mortality.51 According to the first criterion, the hypothesized mediator (years of abstinence) and each of the other predictors had to be significantly related to the dependent variable (mortality). The second criterion required 1 or more of the predictors to have a significant relationship with the mediator. As shown in Table 2 and Figure 1, these 2 criteria were met for a subset of 3 variables: percentage of time hospitalized, number of substance abuse treatment episodes, and percentage of time in treatment (10-percentage-point units).
The third criterion required a change in 1 or more of the relationships between these predictors and mortality when the model was estimated with and without the mediator (data not shown); it also required that there be a better overall fit with the mediator in the model. The odds ratios for predicting mortality in the subsequent 12 months changed significantly (from the model without the mediator to the model with the mediator in Figure 1) for each of these variables (from 18.4 to 14.45 for percentage of time hospitalized, from 0.71 to 0.68 for number of substance abuse treatment episodes in months 7 to 96, and from 1.63 to 1.68 for percentage of time in substance abuse treatment). Moreover, including years of sustained abstinence improved the overall model fit with respect to predicting mortality in the subsequent 12 months (χ21 = 12.11, P < .01). Thus, years of sustained abstinence qualified as a significant mediator of mortality risk in the subsequent 12 months.
DISCUSSION
We set out to estimate the overall mortality rate in a longitudinal cohort of people with substance use disorders seeking treatment and to examine the risk associated with several baseline factors, as well as the complex interaction between baseline characteristics, treatment, and abstinence (the proximal outcome of treatment) in predicting mortality. The overall mortality rate in this sample was 11 per 1000 person-years, which is consistent with the prior treatment literature but more than twice the expected rate (4.4 per 1000 person-years) for a community sample in Cook County, Illinois (where this study was conducted), matched according to age, race, and gender with the Centers for Disease Control and Prevention Wonder tables.53
The individual baseline factors associated with enhanced mortality risk in our multivariate analyses (Table 2) were older age, preexisting chronic illness, and greater engagement in illegal activity for money in the 6 months before intake. Abstinence from drugs and alcohol (even intermittent abstinence) was associated with a lower risk of mortality.
The relationship of long-term treatment with mortality revealed both direct and indirect effects via the duration of sustained abstinence achieved. Participating in more treatment episodes (particularly in one's early years of drug use) is beneficial, but participating in treatment episodes in one's later years and spending a greater percentage of one's lifetime in treatment is not. This finding provides further evidence that the nature of the effects of substance abuse treatment on abstinence and mortality does not support an acute care or simple dosage model; rather, it supports a chronic disease model. In the case of cancer, for instance, early treatment and reintervention (when necessary) are generally associated with a reduced risk of mortality. However, the more instances in which patients relapse and require additional treatment and the more time they spend being treated, the lower their likelihood of achieving sustained remission and the higher their risk of mortality.
Strengths and Limitations
Although this study involved numerous strengths, including a large sample, long duration, repeated observations, high follow-up rates, detailed measurement, and multiple data sources, its limitations are important to note. Data were not readily available on causes of mortality. In addition, although we incorporated urine test data, these data were primarily relevant to past-week use and may have missed unreported use in the preceding year. The sample presenting to treatment was made up predominantly of African American inner-city residents with high rates of criminal justice system involvement. Consequently, the predictors of mortality for this largely African American sample are probably not generalizable to other sociodemographic groups in treatment.
Another limitation was the lack of available mortality data in the specific communities from which the sample was drawn. Although we compared our rates with those of Cook County, our rates were probably underestimated. However, the clinical case mix of the sample was similar to that of the US public treatment system as a whole54 in terms of median age at first use (16 vs 17 years), frequency of weekly or greater use (64% vs 66%), and prior treatment history (58% vs 54%). The patterns of primary substance use (alcohol, cocaine, opioids, marijuana, methamphetamines) were also consistent with those of the US treatment system. In the future, it would be useful to replicate our work with less severe clinical samples and in other locations.
Conclusions
Combined with previous studies involving highly marginalized samples that show that ongoing monitoring and early intervention over the life course of addiction37 are associated with fewer years of use, our results further indicate the need for the addiction field to shift to a more chronic disease management paradigm. Contrary to many current managed care practices, our findings indicate the need for more aggressive screening, early intervention, adequate initial treatment, ongoing monitoring, disease management skills, and better linkage to recovery support services and mutual aid groups that help sustain recovery.
To facilitate this paradigm shift in the private and public sectors, it is particularly important for the US Preventive Services Task Force, as well as accreditation groups and insurance groups, to recommend that drug use be added to the list of conditions for which regular screening and monitoring is expected. Such action is warranted given that drug use is one of the 10 leading causes of mortality and that treatment and subsequent abstinence are associated with a reduced risk of mortality.
Acknowledgments
This research was supported by the National Institute on Drug Abuse (grants DA15523 and DA11323).
We thank the clients and staff who participated in the study as well as Rachael Bledsaw, Nancy Dudley Mark Foss, Lilia Hristova, Joan Unsicker, and Belinda Willis for assistance in preparing the article.
Note. The opinions are those of the authors and do not represent official positions of the US government.
Human Participant Protection
This study was approved by the institutional review board of Chestnut Health Systems. Participation was voluntary, and participants provided written informed consent.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245 [DOI] [PubMed] [Google Scholar]
- 2.Results From the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: Addiction and Mental Health Services Administration; 2008. DHHS publication SMA 08-4343 [Google Scholar]
- 3.Neumark YD, Van Etten ML, Anthony JC. Drug dependency and death: survival analysis of the Baltimore ECA sample from 1981 to 1995. Subst Use Misuse. 2000;35(3):313–327 [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, Randell D, Hall W, Law M, Butler T, Burns L. Mortality among clients of a state-wide opioid pharmacotherapy program over 20 years: risk factors and lives saved. Drug Alcohol Depend. 2009;105(1–2):9–15 [DOI] [PubMed] [Google Scholar]
- 5.Ferguson P, Lennox T, Letteri DJ. Drugs and Pregnancy: The Effects of Nonmedical Use of Drugs on Pregnancy, Childbirth, and Neonates. Washington, DC: National Institute on Drug Abuse Research; 1974 [Google Scholar]
- 6.Watterson O, Sells SB, Simpson DD. Death rates and causes of death among opiate addicts in the DARP during 1971–1972. : Sells SB, Studies of the Effectiveness of Treatment for Drug Abuse Volume 2: Research Patients, Treatments, and Outcomes. Cambridge, MA: Ballinger Press; 1974:281–335 [Google Scholar]
- 7.Joe GW, Lehman W, Simpson DD. Addict death rates after a four-year posttreatment follow up. Am J Public Health. 1982;72(7):703–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joe GW, Simpson DD. Mortality rates among opioid addicts in a longitudinal study. Am J Public Health. 1987;77(3):347–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58(5):503–508 [DOI] [PubMed] [Google Scholar]
- 10.Oppenheimer E, Tobutt C, Taylor C, Andrew T. Death and survival in a cohort of heroin addicts from London clinics: a 22-year follow-up study. Addiction. 1994;89(10):1299–1308 [DOI] [PubMed] [Google Scholar]
- 11.Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97(1):39–47 [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro M, Dunn J, Sesso R, Lima MS, Laranjeira R. Crack cocaine: a five-year follow-up study of treated patients. Eur Addict Res. 2007;13(1):11–19 [DOI] [PubMed] [Google Scholar]
- 13.Paulozzi L, Annest J. Unintentional poisoning deaths—United States, 1999–2004. MMWR Morb Mortal Wkly Rep. 2007;56(5):93–96 [PubMed] [Google Scholar]
- 14.Warner M, Chen LH, Makuc DM. Increase in Fatal Poisonings Involving Opioid Analgesics in the United States, 1999–2006. Hyattsville, MD: National Center for Health Statistics; 2009 [PubMed] [Google Scholar]
- 15.Cruts G, Buster M, Vicente J, Deerenberg I, Van Laar M. Estimating the total mortality among problem drug users. Subst Use Misuse. 2008;43(5):733–747 [DOI] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration 2007 National Survey on Drug Use and Health. Available at: http://www.icpsr.umich.edu/cgi-bin/bob/archive2?study=23782&path=SAMHDA. Accessed December 20, 2010
- 17.Cunningham JA. Untreated remissions from drug use: the predominant pathway. Addict Behav. 1999;24(2):267–270 [DOI] [PubMed] [Google Scholar]
- 18.Cunningham JA, Lin F, Ross HE, Walsh GW. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25(2):317–321 [DOI] [PubMed] [Google Scholar]
- 19.Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100(3):281–292 [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine Broadening the Base of Treatment for Alcohol Problems. Washington, DC: National Academy Press; 1990 [PubMed] [Google Scholar]
- 21.Kessler RC. The National Comorbidity Survey of the United States. Int Rev Psychiatry. 1994;6(4):365–376 [Google Scholar]
- 22.Kessler RC, Merikangas KR. Drug use disorders in the National Comorbidity Survey: have we come a long way?—Reply. Arch Gen Psychiatry. 2007;64(3):381–382 [DOI] [PubMed] [Google Scholar]
- 23.Lamb S, Greenlick MR, McCarty D, Bridging the Gap Between Practice and Research: Forging Partnerships With Community-Based Drug and Alcohol Treatment. Washington, DC: National Academy Press; 1998 [PubMed] [Google Scholar]
- 24.Robins LN, Regier DA. Psychiatric Disorders in America. New York, NY: Macmillan; 1991 [Google Scholar]
- 25.Weisner C, McLellan T, Barthwell A, et al. Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. Available at: http://www.drugabuse.gov/pdf/despr/HSRReport.pdf. Accessed December 20, 2010
- 26.Hser YI, Stark ME, Paredes A, Huang D, Anglin MD, Rawson R. A 12-year follow-up of a treated cocaine-dependent sample. J Subst Abuse Treat. 2006;30(3):219–226 [DOI] [PubMed] [Google Scholar]
- 27.Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment re-entry, and recovery. Drug Alcohol Depend. 2005;78(3):325–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scott CK, Foss MA, Dennis ML. Pathways in the relapse, treatment, and recovery cycle over three years. J Subst Abuse Treat. 2005;28(suppl 1):S63–S72 [DOI] [PubMed] [Google Scholar]
- 29.Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Arch Gen Psychiatry. 2002;59(6):538–544 [DOI] [PubMed] [Google Scholar]
- 30.Langendam MW, van Brussel GHA, Coutinho RA, van Ameijden EJC. The impact of harm-reduction-based methadone treatment on mortality among heroin users. Am J Public Health. 2001;91(5):774–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Preventive Services Task Force Screening for illicit drug use. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrug.htm. Accessed December 20, 2010
- 32.Sells SB, Chatham LR, Retka RL. A study of differential death rates and causes of death among 9276 opiate addicts during 1970–1971. Contemp Drug Probl. 1972;1(4):665–706 [Google Scholar]
- 33.Watterson O, Simpson DD, Sells SB. Death rates and causes of death among opioid addicts in community drug treatment programs during 1970–1973. Am J Drug Alcohol Abuse. 1975;2(1):99–111 [DOI] [PubMed] [Google Scholar]
- 34.Kuh D. A life course approach to healthy aging, frailty, and capability. J Gerontol. 2007;62A(7):717–721 [DOI] [PubMed] [Google Scholar]
- 35.McLellan AT, Lewis D, O'Brien CP, Hoffman NG, Kleber HD. Drug dependence, a chronic mental illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695 [DOI] [PubMed] [Google Scholar]
- 36.Anglin MD, Hser Y, Grella CE. Drug addiction and treatment careers among clients in DATOS. Psychol Addict Behav. 1997;11(4):308–323 [Google Scholar]
- 37.Dennis ML, Scott CK, Funk R, Foss MA. The duration and correlates of addiction and treatment careers. J Subst Abuse Treat. 2005;28(suppl 1):S51–S62 [DOI] [PubMed] [Google Scholar]
- 38.Hser YI, Anglin MD, Grella CE, Longshore D, Pendergast ML. Drug Treatment Careers: A Conceptual Framework and Existing Research Findings. Los Angles, CA: Drug Abuse Research Center; 1997 [DOI] [PubMed] [Google Scholar]
- 39.Hser Y, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval Rev. 2007;31(6):515–547 [DOI] [PubMed] [Google Scholar]
- 40.Humphreys K, Moos RJ, Cohen C. Social and community resources and long-term recovery from treated and untreated alcoholism. J Stud Alcohol. 1997;58(1):1–8 [DOI] [PubMed] [Google Scholar]
- 41.Moos RH, Moos BS. Protective resources and long term recovery from alcohol disorders. Drug Alcohol Depend. 2007;86(1):46–54 [DOI] [PubMed] [Google Scholar]
- 42.Schutte KK, Byme FE, Brennan PL, Moos RH. Successful remission of late-life drinking problems: a 10 year follow up. J Stud Alcohol. 2001;62:322–334 [DOI] [PubMed] [Google Scholar]
- 43.Dennis ML, Foss MA, Scott CK. An 8-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Eval Rev. 2007;31(6):585–612 [DOI] [PubMed] [Google Scholar]
- 44.Scott CK, Muck RD, Foss MA. The impact of centralized intake on access to treatment and satisfaction with intake procedures. : Levy JA, Stephens RC, McBride DC, Advances in Medical Sociology, Volume 7: Emergent Issues in the Field of Drug Abuse. Stamford, CT: JAI Press; 2000:131–150 [Google Scholar]
- 45.Scott CK, Foss MA, Sherman RE. Effects of centralized intake on participant satisfaction with treatment and ancillary services. : Stephens RC, Scott CK, Muck RD, Clinical Assessment and Addiction Treatment: The Target Cities Experience. Albany, NY: State University of New York Press; 2003:149–164 [Google Scholar]
- 46.Scott CK, Foss MA, Sherman RE. Outcomes before and after implementing centralized intake services. : Stephens RC, Scott CK, Muck RD, Clinical Assessment and Addiction Treatment: The Target Cities Experience. Albany, NY: State University of New York Press; 2003:7–15 [Google Scholar]
- 47.Scott CK, Foss MA, Dennis ML. Factors influencing initial and longer-term responses to addiction treatment: a path analysis. Eval Program Plann. 2003;26(3):287–295 [Google Scholar]
- 48.Scott CK, Dennis ML, Godley MD, Foss MA. Intake Augmented—Addiction Severity Index. Chicago, IL: Chestnut Health Systems; 1999 [Google Scholar]
- 49.McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213 [DOI] [PubMed] [Google Scholar]
- 50.Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of addictions. Drug Alcohol Depend. 2004;74(1):21–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182 [DOI] [PubMed] [Google Scholar]
- 52.US Dept of Health and Human Services. Poverty Guidelines, Research, and Measurement. Available at: http://aspe.hhs.gov/poverty/poverty.shtml. Accessed January 25, 2011.
- 53.Centers for Disease Control and Prevention CDC Wonder tables. Available at: http://wonder.cdc.gov/cmf-icd10.html. Accessed December 20, 2010
- 54.Office of Applied Studies Treatment Episode Data Set: admissions series. Available at: http://www.icpsr.umich.edu/icpsrweb/SAMHDA/series/00056. Accessed December 20, 2010