Abstract
Purpose
To measure and analyse national EQ-5D data and to provide norms for the Chinese general population by age, sex, educational level, income and employment status.
Methods
The EQ-5D instrument was included in the National Health Services Survey 2008 (n = 120,703) to measure health-related quality of life (HRQoL). All descriptive analyses by socio-economic status (educational level, income and employment status) and by clinical characteristics (discomfort during the past 2 weeks, diagnosed with chronic diseases during the past 6 months and hospitalised during the past 12 months) were stratified by sex and age group.
Results
Health status declines with advancing age, and women reported worse health status than men, which is in line with EQ-5D population health studies in other countries and previous population health studies in China. The EQ-5D instrument distinguished well for the known groups: positive association between socio-economic status and HRQoL was observed among the Chinese population. Persons with clinical characteristics had worse HRQoL than those without.
Conclusions
This study provides Chinese population HRQoL data measured by the EQ-5D instrument, based on a national representative sample. The main findings for different subgroups are consistent with results from EQ-5D population studies in other countries, and discriminative validity was supported.
Electronic supplementary material
The online version of this article (doi:10.1007/s11136-010-9762-x) contains supplementary material, which is available to authorized users.
Keywords: China, EQ-5D, General population, Health surveys, Inequalities, Socio-economic status
Introduction
China has been undergoing a period of rapid economic growth with dramatic social and political transitions since its market-oriented reforms were launched in the 1980s. On average, during the past 30 years, China’s GDP has grown by 9.4% per year, and the proportion of the population in absolute poverty has decreased from 31 to 3% [1]. Great achievements have been made in education, e.g. the literacy rate reached the same level as that of middle-income countries. But at the same time, disparities in education and income are increasing, and unemployment appeared with the collapse of state-owned enterprises [2]. The dramatic socio-economic transitions during the past decades have had major impacts on health: overall, the Chinese live longer and are healthier, average life expectancy increased from 67.9 years in 1981 to 72.5 years in 2008 [3], but health inequalities between groups with different educational levels, income and employment status are increasing [1, 4–6]. Those inequalities are considered a serious problem and may impact heavily on the country’s future development. In order to reduce inequalities in health, a recent Government Report from the National Congress Meeting (Beijing, April 2009) set the following target for the health care reform: “By 2020, build a basic health care system that can provide safe, effective, convenient and affordable health services to urban and rural residents” [7]. Hence, measuring health, and its distribution among different sub-groups, would provide valuable information for policy-makers in their efforts to reduce inequalities in health.
Educational level, income and employment status are the socio-economic status indicators most commonly used [8, 9]. In China, studies on health inequalities have been carried out, focusing mainly on inequalities between rural and urban areas [10, 11], socio-economic inequalities [2, 4, 12–14] and gender inequalities in health [15–17].
Population health studies in China have mostly used mortality [14, 18], life expectancy [15] and usage of health care as health indicators [4, 18]. Mortality and life expectancy may not adequately reflect health and its development over time, because the disease pattern has changed from acute infectious diseases to chronic non-communicable diseases [19], and the proportion of persons living with ill-health has increased. Mortality measures do not take health status into consideration: while mortality decreases, the fraction of people living with ill-health might increase at the same time. The usage of health care does not necessarily reflect health status. Individuals with poor health tend to consume more health care, but on the other hand, those with poor health could not afford health care, especially in a country like China where health care is provided largely based on out-of-pocket payments.
The global self-rated health question—“How is your health today? Good, bad or in-between?”—is commonly used to obtain health status, also in China [12, 20]. However, this measure does not take the multi-dimensions of health into consideration.
Health-related quality of life (HRQoL) is a subjective account of health assessment, which reflects the multi-dimensions of health, such as physical, psychological, social, cognitive and role function, as well as general well-being [21]. In China, some studies are also based on HRQoL data [13, 17]. Numbers of instruments have been developed to measure HRQoL, but not all the instruments cover all these health dimensions [22]; for example, the EQ-5D does not include a cognitive dimension.
The EQ-5D instrument has been used for measuring population health status in many countries, in Europe and the USA, Canada and Zimbabwe, and population norms have been established by age, sex and socio-economic status [23–31]. Norms data can be used to compare health status of specific groups with that of the general population.
There is an increasing interest in applying the EQ-5D instrument to Asia. Most studies are performed among patients, e.g. in Singapore [32], Japan [33], Bangladesh [34], Malaysia [35], South Korea [36], mainland China [37] and Thailand [38]. Studies have been performed among the general population in Japan [39], mainland China [40], Taiwan [41] and South Korea [42]. Studies among Chinese populations have also been performed in Singapore [32], the USA [26, 43] and Canada [44]. An EQ-5D study in Beijing was performed among 2,994 individuals from one district [40]. The results suggested that EQ-5D is valid for measuring health status in the Chinese population.
In 2008, for the first time, the EQ-5D was included in the National Health Services Survey (NHSS) to measure population health status in all 31 provinces in mainland China.
The aim of the study was to measure and analyse national EQ-5D data and to provide norms for the Chinese general population by age, sex, educational level, income and employment status.
Materials and methods
Study sample and design
Data were derived from the 2008 National Health Services Survey (NHSS), which has been organised by the Chinese Ministry of Health (MoH) every fifth year since 1993. The surveys were carried out from mid-June till mid-July, and face-to-face interviews were conducted by trained local interviewers [45]. The NHSS 2008 questionnaire includes more than 200 questions, on acute diseases and injuries, chronic and other diseases, hospitalisation, health-related behaviour, educational level, family income and employment status, social relations, safety and security, medical care fees, accessibility (distance and time) and satisfaction with health service, insurance coverage, vaccination and disease control, woman and child health services. In 2008, the EQ-5D was included for the first time.
In NHSS 2008, 56,400 households were sampled using a multi-stage stratified cluster random sampling [46]. In the first sample stage, 2,400 counties were stratified based on socio-economic, health care and population structure to sample 94 counties. In the second stage, 2,350 streets (urban area) and townships (rural area) in the 94 counties were stratified based on population size and income per capita to sample 470 streets and townships. In the third stage, 940 residential committees (urban area) and villages (rural area) were sampled using the same criteria as in the second stage. In each residential committee or village, 60 households were randomly selected, and all family members in a sampled household were interviewed individually. EQ-5D was asked among persons aged 15 years and over, and no upper-age limit was applied. However, the instrument can be used in younger age groups, and the newly developed child-friendly version of the EQ-5D, named EQ-5D-Y [47, 48], is available in some language versions, but not yet in Chinese. Hence, persons aged under 15 years were not included in this study.
In total, 177,501 respondents were included in NHSS 2008. Of these, about 18% aged below 15 years were excluded, since EQ-5D questions should only be administered to respondents aged 15 years and over. Respondents not answering the questions by themselves were excluded (13%). In total, less than 2% of the respondents had missing answers on age, sex, in at least one of the EQ-5D dimensions, on VAS or reported VAS higher than 100. After applying the previous exclusion criteria, 120,703 respondents were included in this study.
Ethical permission was granted by the Regional ethics committee, Stockholm, Sweden, for analyses of this study (Dnr: 2009/1892–31).
Interview procedure
The interviewers were recruited from local health workers. The supervisors for interviewers were trained at the national level (4 supervisors per county, recruited from local health authority staff and county interviewers). The supervisors then trained the interviewers in each county (30 interviewers per county). An instruction for performing face-to-face interviews on NHSS questions was provided by MoH.
As a quality control, the supervisors checked the completeness of the questionnaire at the end of each day. If information was missing, the interviewer went back during the same day or next day to ask the missing questions again.
Measurements
Variables for socio-economic status
The highest accomplished educational level was classified into below primary school, primary school, junior middle school, senior middle school, college and above. An individual’s annual income was assessed by dividing household annual income by the numbers of persons living in the family within the last half-year, regardless of age and employment status. Respondents were then ranked from lowest to highest by their annual income and divided into five groups of equal size: the lowest income group had an income below 2,500 RMB; the second group from 2,500 to 3,999 RMB; the third group from 4,000 to 5,999 RMB; the fourth group from 6,000 to 9,999 RMB; the fifth and highest income group 10,000 RMB and above. Employment status was categorised into employed, unemployed, student and retired.
Health outcome measure
The EQ-5D instrument is a generic HRQoL outcome measure [23] that classifies respondent’s present-day health status in five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression); each dimension is represented by one question with three severity levels (no problems, some problems and severe problems). The EQ-5D instrument in total defines 243 health states.
A visual analogue scale (VAS) was used in the survey, with anchor points 0 (worst health state) and 100 (best health state). The scale consisted of a horizontal line where every 10th was marked and labelled 0, 10, 20,…, 100. The question was framed: “On the scale please point out which point best represents your own health state today.” The scale was harmonised to fit in the NHSS questionnaire and hence slightly differs from the EQ VAS.
Clinical characteristic
Respondents who answered “yes” to the questions “Have you had discomfort during the past 2 weeks?” or “Have you been diagnosed with chronic disease during the past 6 months?” or “Have you been hospitalised during the past 12 months” were defined as having a clinical characteristic.
Statistical analyses
Data were entered at the provincial level, two persons independently entered the same data using a software provided by the MoH, and disagreements were checked and corrected. Each province reported the data to MoH, where data were cleaned and a national data set was created.
All descriptive analyses by socio-economic status and by clinical characteristics were performed stratified by age and sex. Age groups 15–44 years, 45–64 years and 65+ were used for age categorisation. Calculations of percentage of respondents reporting problems in each EQ-5D dimension, VAS score (mean) and multiple regression analyses were performed in SAS 9.1 [49]. To test the statistical significance of the difference between groups in the percentage of reported problems, χ2 tests were used. Multiple regression analyses were used to estimate how VAS scores varied with age, sex, educational level, income group and employment status. Dummy variables were created for 5-year age groups except for the oldest, 85–103 years. Dummy variables were created for educational level, income group, employment status and clinical characteristics. In order to keep the observation number the same in all the models, dummies for missing values were entered for each categorisation, except for missing in diagnosed with chronic disease within last 6 months due to the low missing number (n = 2). A 5% significance level was used for all analyses.
Results
Characteristics of respondents
Characteristics of respondents are presented for men and women, respectively (Table 1). The proportion of women in the study was 52%. Educational level below junior middle school was reported by 44% of the respondents, unemployment was reported by 15% of the respondents, and both rates were higher among women than men.
Table 1.
Characteristics of respondents, total and by sex, China 2008
| Total | Men | Women | ||||
|---|---|---|---|---|---|---|
| % | n | % | n | % | n | |
| Sex | ||||||
| Men | 48.2 | 58,163 | – | – | – | – |
| Women | 51.8 | 62,540 | – | – | – | – |
| Age group (years) | ||||||
| 15–44 | 48.0 | 57,958 | 46.9 | 27,258 | 49.1 | 30,700 |
| 45–64 | 37.6 | 45,408 | 38.5 | 22,365 | 36.8 | 23,043 |
| 65+ | 14.4 | 17,337 | 14.7 | 8,540 | 14.1 | 8,797 |
| Education | ||||||
| Below primary school | 15.6 | 18,840 | 9.1 | 5,298 | 21.7 | 13,542 |
| Primary school | 27.9 | 33,627 | 28.1 | 16,343 | 27.6 | 17,284 |
| Junior middle school | 35.7 | 43,040 | 39.4 | 22,912 | 32.2 | 20,128 |
| Senior middle school | 14.9 | 17,941 | 16.4 | 9,561 | 13.4 | 8,380 |
| College and above | 5.9 | 7,160 | 6.9 | 4,008 | 5.0 | 3,152 |
| Missing | 0.1 | 95 | 0.1 | 41 | 0.1 | 54 |
| Income groups | ||||||
| First group (low) | 22.8 | 27,558 | 23.2 | 13,492 | 22.5 | 14,066 |
| Second group | 21.6 | 26,036 | 21.7 | 12,619 | 21.5 | 13,417 |
| Third group | 18.9 | 22,789 | 18.7 | 10,860 | 19.1 | 11,929 |
| Fourth group | 17.7 | 21,417 | 17.6 | 10,237 | 17.9 | 11,180 |
| Fifth group (high) | 19.0 | 22,903 | 18.8 | 10,955 | 19.1 | 11,948 |
| Occupational status | ||||||
| Employed | 70.6 | 85,155 | 74.7 | 43,419 | 66.8 | 41,736 |
| Retired | 10.2 | 12,313 | 9.7 | 5,613 | 10.7 | 6,700 |
| Student | 4.4 | 5,322 | 4.6 | 2,695 | 4.2 | 2,627 |
| Unemployed | 14.6 | 17,627 | 10.8 | 6,306 | 18.1 | 11,321 |
| Missing | 0.2 | 286 | 0.2 | 130 | 0.2 | 156 |
| Clinical characteristics | ||||||
| Discomfort within 2 weeks | ||||||
| Yes | 20.3 | 24,551 | 18.4 | 10,681 | 22.2 | 13,870 |
| No | 79.5 | 95,911 | 81.4 | 47,355 | 77.6 | 48,556 |
| Missing | 0.2 | 241 | 0.2 | 127 | 0.2 | 114 |
| Diagnosed with chronic disease during the past 6 months | ||||||
| Yes | 20.1 | 24,275 | 18.6 | 10,840 | 21.5 | 13,435 |
| No | 79.9 | 96,426 | 81.4 | 47,322 | 78.5 | 49,104 |
| Missing | 0.0 | 2 | 0.0 | 1 | 0.0 | 1 |
| Hospitalised within 12 months | ||||||
| Yes | 6.3 | 7,625 | 5.2 | 3,010 | 7.4 | 4,615 |
| No | 93.7 | 113,078 | 94.8 | 55,153 | 92.6 | 57,925 |
Health-related quality of life by age group and sex
There was an age-gradient in health status: moderate and severe problems reported in each EQ-5D dimension increased and mean VAS score decreased with age (Table 2). In the anxiety/depression dimension, the increase with age was less steep compared with the other dimensions. Women usually reported more problems in EQ-5D dimensions and had lower mean VAS score in all age groups than men.
Table 2.
Percentage of respondents reporting moderate and severe problems in each EQ-5D dimension, VAS score (mean), by age group and sex, China 2008
| EQ-5D Dimension | Age group (years) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85+ | Total 15–103 | |
| % | % | % | % | % | % | % | % | % | % | % | % | % | % | % | % | |
| Men (n) | 3,618 | 2,952 | 3,497 | 4,057 | 6,269 | 6,845 | 5,658 | 6,824 | 5,746 | 4,137 | 3,121 | 2,679 | 1,604 | 819 | 317 | 58,163 |
| Mobility | ||||||||||||||||
| Moderate problems | 0.4 | 0.7 | 0.5 | 1.1 | 1.2 | 2.1 | 3.0 | 3.3 | 4.8 | 6.9 | 10.5 | 14.0 | 19.8 | 25.5 | 30.0 | 4.0 |
| Severe problems | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.3 | 0.2 | 0.4 | 0.5 | 0.8 | 1.4 | 1.4 | 2.7 | 5.4 | 0.3 |
| Self-care | ||||||||||||||||
| Moderate problems | 0.4 | 0.5 | 0.4 | 0.5 | 0.7 | 0.9 | 1.5 | 1.7 | 2.6 | 4.1 | 5.5 | 9.0 | 12.2 | 17.5 | 20.8 | 2.3 |
| Severe problems | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.3 | 0.5 | 0.7 | 1.1 | 1.6 | 1.9 | 3.1 | 5.1 | 0.4 |
| Usual activities | ||||||||||||||||
| Moderate problems | 0.4 | 0.8 | 0.4 | 0.9 | 1.1 | 1.5 | 2.5 | 2.9 | 3.8 | 5.4 | 8.2 | 12.1 | 16.5 | 22.5 | 25.6 | 3.3 |
| Severe problems | 0.1 | 0.1 | 0.2 | 0.3 | 0.2 | 0.3 | 0.5 | 0.5 | 0.9 | 1.2 | 1.9 | 2.9 | 2.8 | 6.0 | 10.7 | 0.7 |
| Pain/discomfort | ||||||||||||||||
| Moderate problems | 1.0 | 1.4 | 1.1 | 2.1 | 3.1 | 3.9 | 6.1 | 7.8 | 10.8 | 13.2 | 16.1 | 20.3 | 23.9 | 26.0 | 28.1 | 6.9 |
| Severe problems | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.2 | 0.4 | 0.7 | 0.7 | 1.2 | 1.3 | 1.8 | 1.9 | 0.3 |
| Anxiety/depression | ||||||||||||||||
| Moderate problems | 0.7 | 1.3 | 1.9 | 2.9 | 2.9 | 3.8 | 4.7 | 5.3 | 6.8 | 8.5 | 9.9 | 12.0 | 14.7 | 15.8 | 15.8 | 4.9 |
| Severe problems | 0.1 | 0.2 | 0.1 | 0.3 | 0.2 | 0.2 | 0.4 | 0.3 | 0.4 | 0.5 | 0.7 | 1.1 | 1.1 | 1.3 | 0.6 | 0.3 |
| VAS score (mean) | 89.8 | 88.8 | 87.8 | 86.0 | 84.8 | 83.4 | 81.4 | 79.3 | 77.4 | 75.1 | 72.5 | 70.1 | 68.4 | 66.2 | 66.1 | 80.9 |
| Women (n) | 3,427 | 3,525 | 3,986 | 4,894 | 7,274 | 7,594 | 6,121 | 7,143 | 5,731 | 4,048 | 3,004 | 2,723 | 1,736 | 871 | 463 | 62,540 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | ||||||||||||||||
| Moderate problems | 0.5 | 0.5 | 0.6 | 0.9 | 1.3 | 2.0 | 3.2 | 4.3 | 5.4 | 9.0 | 11.9 | 16.3 | 22.7 | 30.8 | 36.7 | 5.0 |
| Severe problems | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.5 | 0.5 | 0.8 | 0.9 | 1.3 | 2.1 | 6.1 | 0.4 |
| Self-care | ||||||||||||||||
| Moderate problems | 0.4 | 0.2 | 0.5 | 0.5 | 0.9 | 1.1 | 1.3 | 2.3 | 3.1 | 5.0 | 7.5 | 10.0 | 14.1 | 21.0 | 28.9 | 3.0 |
| Severe problems | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.3 | 0.3 | 0.6 | 0.5 | 1.0 | 1.1 | 1.6 | 3.0 | 7.6 | 0.4 |
| Usual activities | ||||||||||||||||
| Moderate problems | 0.5 | 0.5 | 0.5 | 0.9 | 1.4 | 1.8 | 2.7 | 3.6 | 4.6 | 7.5 | 10.1 | 13.9 | 17.8 | 26.5 | 33.7 | 4.3 |
| Severe problems | 0.1 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | 0.4 | 0.6 | 0.9 | 1.0 | 1.8 | 2.4 | 3.2 | 6.1 | 12.3 | 0.8 |
| Pain/discomfort | ||||||||||||||||
| Moderate problems | 0.8 | 1.0 | 1.5 | 3.2 | 4.6 | 6.1 | 9.3 | 11.4 | 13.9 | 18.0 | 20.8 | 25.0 | 27.8 | 31.9 | 38.0 | 10.0 |
| Severe problems | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 0.5 | 0.4 | 0.6 | 0.9 | 1.2 | 1.5 | 1.4 | 2.0 | 1.7 | 0.5 |
| Anxiety/depression | ||||||||||||||||
| Moderate problems | 1.2 | 1.5 | 1.9 | 3.2 | 4.1 | 5.1 | 6.5 | 7.6 | 8.4 | 10.6 | 12.9 | 14.4 | 16.4 | 17.6 | 23.1 | 6.7 |
| Severe problems | 0.0 | 0.1 | 0.0 | 0.2 | 0.2 | 0.2 | 0.5 | 0.4 | 0.5 | 0.5 | 0.9 | 1.0 | 0.9 | 1.8 | 1.9 | 0.4 |
| VAS score (mean) | 89.6 | 88.2 | 86.7 | 84.8 | 83.2 | 81.5 | 79.2 | 77.2 | 75.2 | 72.8 | 70.2 | 68.5 | 66.9 | 65.5 | 64.3 | 79.4 |
Health-related quality of life by socio-economic status
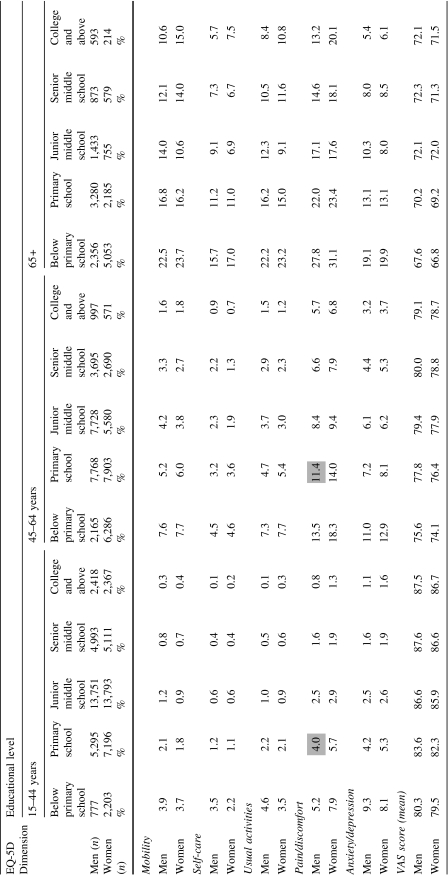
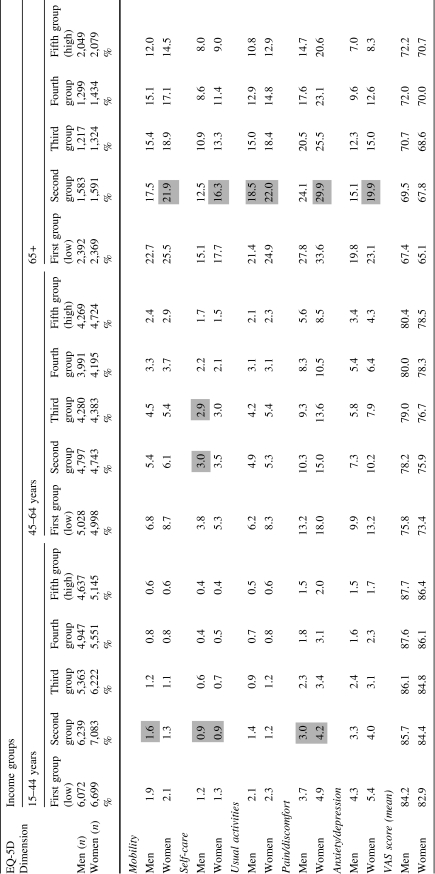
Overall, respondents with a lower educational level reported more problems in EQ-5D dimensions and lower VAS scores than those with higher educational levels (Table 3), except for women aged 65 years and above, where those with junior middle school educational level reported the best health status. Respondents in lower income groups reported more problems in EQ-5D dimensions and had lower VAS scores than those in the higher income groups (Table 4).
Table 3.
Percentage of respondents reporting moderate or severe problems in each EQ-5D dimension [χ2 tests were performed, and for each age group, respondents with below primary school educational level were used as reference group. All results were statistically significant except those shaded (P<0.05)], VAS score (mean), by educational level, age group and sex, China 2008
Table 4.
Percentage of respondents reporting moderate or severe problems in each EQ-5D dimension [χ2 tests were performed, and for each age group, respondents in the first income group (low) were used as reference group. All results were statistically significant except those shaded (P<0.05)], VAS score (mean), by income group, age group and sex, China 2008
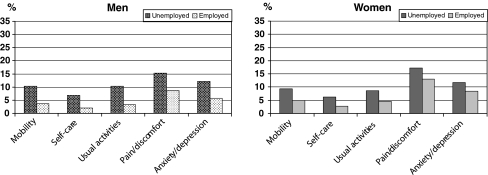
Unemployed persons reported more problems in all EQ-5D dimensions and had lower mean VAS scores than those who were employed (online resource, Table 5). The differences in health between different socio-economic groups increased with age. Percentage of problems in each dimension for the age group 45–64 years is presented in Fig. 1. The mean VAS score for unemployed men was 74.0 compared with 79.5 for employed men. Corresponding figures for women were 74.1 and 77.2, respectively.
Fig. 1.
Percentage of respondents reporting moderate or severe problems in each EQ-5D dimension, by employment status, 45–64 years, China 2008
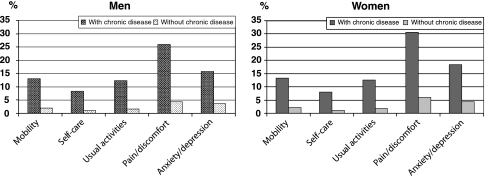
Health-related quality of life by clinical characteristics
Respondents who reported a discomfort during the past 2 weeks or that they having been diagnosed with chronic disease during the past 6 months or hospitalised during the past 12 months reported more problems in all EQ-5D dimensions and had lower mean VAS scores than those not reporting any of these clinical characteristics (online resource, Table 6). Percentage of problems in each dimension for the age group 45–64 years is presented in Fig. 2. The mean VAS score for men reporting a chronic disease was 70.4 compared with 81.2 for men not reporting a chronic disease. Corresponding figures for women were 69.0 and 79.6, respectively.
Fig. 2.
Percentage of respondents reporting moderate or severe problems in each EQ-5D dimension, with and without chronic disease during the past 6 months, 45–64 years, China 2008
Variation in VAS score controlling for other factors
The variation of VAS score by educational level, income group and employment status was analysed controlling for age and sex (online resource, Table 7). Model 1 showed that the VAS scores decreased with age, and that women had significantly lower VAS scores than men. In model 2, the VAS scores were significantly lower for lower levels of education, the difference between the highest and lowest educational level being 4.28. In model 3, the VAS scores were significantly lower in lower income groups, with a difference of 4.30 between the highest and lowest income groups. In model 5, the unemployed had significantly lower VAS scores than those employed with a difference of 2.84.
In model 4, when dummy variables for both educational level and income were entered, the effect of income was relatively stable, while the effects of education were reduced. The education gradient was clear for respondents with below junior middle school educational level but did not differ between those with above junior middle school educational level. In model 6, when employment status was added into the model, the gradient of education and income was similar to that in model 4.
The variation of VAS score by the clinical characteristics was analysed, controlling for age and sex (online resource, Table 8). According to the regression analysis, the VAS scores were 8.9 lower for respondents with discomfort during the past 2 weeks compared with respondents not reporting discomfort. The difference in VAS scores for those with and without chronic disease was 10.0, and respondents who had been hospitalised in the last 12 months had a 6.9 lower VAS scores than those who had not been hospitalised.
Discussion
This study provides Chinese population HRQoL data measured by the EQ-5D instrument, based on a national representative sample. These norms can be used as reference values when comparing different groups’ health status with the general population in China.
Health status decreased with age and women reported worse health status than men, which is in line with EQ-5D population health studies in other countries [23–31] and previous population health studies in China [15, 16, 40]. The EQ-5D instrument distinguished well for the known groups: the positive association between socio-economic status (educational level, income and unemployment status) and HRQoL was observed among the Chinese population. Persons with clinical characteristics had worse HRQoL than those without, and discriminate validity of the EQ-5D was assessed.
The positive association between socio-economic status and health has been shown in Europe over decades [8, 9, 50–52], and previous studies in China also showed similar results [12, 13, 18]. Our study has similar findings, and socio-economic inequalities in HRQoL in China could be observed. All analyses by educational level, income and employment status have been investigated in a nationally representative sample, where effects of age and sex were taken into consideration. As this is a cross-sectional study, no causality relation between health and socio-economic status can be applied.
Several limitations needed to be addressed. The sampling design was complex, using a multi-stage sampling with both stratification and clustering. This made it difficult to take the effects of the sampling design into consideration for all stages in the analyses. This might have an effect on the precision of our estimates. However, the NHSS sampling design was examined by the MoH for all waves of the surveys, and the representativeness of the sample was considered good [46].
Face-to-face interviews have been used in several EQ-5D population studies [24, 26, 30]; however, whether face-to-face interviews influence the EQ-5D self-reported health was not discussed in those studies. Several studies using other instruments suggest that respondents reported better health during face-to-face interview situations than in postal surveys [53–56]. There are very few studies comparing mode of administration of the EQ-5D instrument in population studies. One study showed that among AIDS patients, self-administration and interview-administration yielded similar results [57], but little is known regarding the general population. The NHSS has been performed in three waves and all applied the face-to-face interviews, which makes it possible to collect information from those who have difficulty with reading the questionnaire by themselves. The way in which this might influence respondents’ answers in the EQ-5D dimensions will be discussed in the following paragraph, where we consider the ceiling effect. The NHSS is a comprehensive study that involved nearly 2,000 interviewers located in different areas. In order to reduce interview bias, the MoH provided an interview protocol and trainings for all the questions in NHSS [46], where the importance of avoiding interference between family members was emphasised. However, in reality, such interference could not be avoided in all situations, e.g. a family might have only one room, or an old person might need assistance from other family members during the interview. In a large country like China, where dialects, customs and living circumstances vary considerably from region to region, the way in which this might affect interviews requires further investigations.
A large proportion of the population tend to report good health (report no problem on any of the EQ-5D dimension), which might be due to the fact of a majority of the population being healthy but also can be due to a ceiling effect. The ceiling effect might be caused by the design of the instrument, e.g. if the instrument is not sensitive enough to discriminate between severity levels [58], or due to culture differences, e.g. the ceiling effect may be even higher among the Asian population [25, 40, 59, 60]. Mode of administration can also influence results, and face-to-face interviews impact survey results from two opposite aspects: on the one hand with face-to-face interviews, persons with ill-health could be more easy to reach than in a postal survey [28, 55], but on the other hand in a face-to-face interview situation, respondents answer questions more optimistically than in a postal survey [53, 54]. Further research should investigate comparing different modes of administration for EQ-5D instrument among Chinese population. The study with face-to-face interviews in Beijing showed that the Chinese population generally reported a smaller proportion of problems in EQ-5D dimensions than Spain, the United Kingdom, the USA and Canada, and a slightly smaller proportion than Japan [40]. This difference was especially pronounced in the pain/discomfort and anxiety/depression dimensions. Within a country, the Chinese were also found more likely to report better health status than Whites; this was reported in studies regarding cross-ethnic comparisons of health in the US population [25, 59, 60] and Canada [44].
The individual annual income was assessed from average income for each family member living in a household and therefore reflects the economic situation of a household rather than that of the individual. The differences by income group might be underestimated. Persons with the same income might have different employment status and occupation; therefore, their health insurance and social security net could be different, and these factors might also influence health. Our way of converting household income into individual income was rather crude, as no account is taken of economics of scale, or of the possibility of consumption might varying with age in the household. However, we are not aware of any equivalence scale for converting household income into individual income for China. To create a measure of absolute income, i.e. consumption possibilities, we ranked respondents from highest to lowest by their annual income and divided the population into five income groups of equal size for China as a whole. A drawback to this measure is that it does not adjust for regional differences, e.g. the cost of living, but adjustments of this kind are hard to make. An alternative could have been to divide the population into groups based on localised cut-offs. However, such a measure would capture the relative rank in income in each region, rather than the absolute consumption possibilities for China as a whole.
Employment status in China is not easy to pin down. Official rules regarding retirement age are only established for the urban area (men retire at 60, women non-manual workers at 55 and women manual workers at 50) [61]. In rural areas, there are no strict rules regarding retirement age, as old people do not receive pensions from the government. This makes it difficult to apply a universal retirement age to the entire population. For this reason, when persons aged over 60 reported themselves employed or unemployed, we include them in the analyses in the way they reported.
The proportion of persons with different educational level and the average household annual income are similar to the data reported in official statistics [62]. However, the proportion of unemployed was higher in the NHSS than in the official statistics. This might be due to different definitions of unemployment. The NHSS is designed to reflect the socio-economic status of the Chinese population.
It would be interesting to compare the magnitude of socio-economic gradient in health in China with other countries. However, the health outcome measures used in other studies were different, and in the studies that applied the EQ-5D instrument age group and socio-economic status were stratified in a different way, which makes it difficult to do a direct comparison.
The following findings are similar to the EQ-5D population studies from other countries: most problems were reported in pain/discomfort dimension and followed by anxiety/depression dimension; problems reported in the EQ-5D dimensions increase with age, and women reported more problems than men [24–31]. However, the proportion of respondents reporting having problems in EQ-5D dimensions is different from country to country. This might be due to several reasons: health status is different across countries; or age and sex structure are different across countries; or people in different countries refer to levels of health differently [25, 30, 58]; or the mode of administration varies from one survey to another; or some countries include proxy respondents. One therefore needs to be cautious when performing international comparison of population health status. A related concern is linked to expectations of health and that HRQoL is a subjective assessment of health status. Studies have suggested that respondents with lower socio-economic status might have lower expectation of health and therefore might rate their own health status higher than respondents in higher socio-economic groups, given the same health condition [63, 64]. This issue requests further investigation.
Given the caveats, the EQ-5D distinguished well between the known groups among the Chinese population. Our study provides a population EQ-5D health status norm for mainland China, based on a national representative sample. A socio-economic difference in health status could be observed, which might suggest that policies aiming to reduce socio-economic inequalities are important. Knowledge from our study might provide a deeper understanding regarding HRQoL in China. In a subsequent paper, we will discuss regional differences in HRQoL using the EQ-5D in China [65].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We would like to thank the Ministry of Health in China for data collection and their support of data analysis work. We acknowledge financial support from the Swedish Research Council (Swedish Research Links programme 348-2009-6538). We are also grateful for the helpful comments and suggestions received on earlier versions of this paper from the Equity and Health Policy Research Group, Department of Public Health Sciences, Karolinska Institutet, at the 26th EuroQol Plenary Meeting in Paris in 2009, at the 7th World Congress of Health Economics (iHEA) in Beijing in 2009, at the 16th Annual Conference of the International Society for Quality of Life Research (ISOQOL) in New Orleans in 2009, and from the Health Economics Research Group, Medical Management Centre, Karolinska Institutet. We would also like to thank three anonymous reviewers and the editor, for their valuable comments and constructive suggestions.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- HRQoL
Health-related quality of life
- NHSS
National Health Services Survey
- MoH
Ministry of Health
- VAS
Visual analogue scale
- RMB
Ren Min Bi (Chinese currency)
Footnotes
The EQ-5D is a copyrighted instrument, and all requests for using it should be sent to the EuroQol Executive Office in Rotterdam, the Netherlands (userinformationservice@euroqol.org).
Contributor Information
Sun Sun, Phone: +46-8-52484779, Email: sun.sun@ki.se.
Jiaying Chen, Phone: +86-25-86862950, Email: jychen@njmu.edu.cn.
Magnus Johannesson, Email: magnus.johannesson@hhs.se.
Paul Kind, Email: pk1@york.ac.uk.
Ling Xu, Email: xuling@moh.gov.cn.
Yaoguang Zhang, Email: zhangyg@moh.gov.cn.
Kristina Burström, Email: kristina.burstrom@ki.se.
References
- 1.Office of the WHO representative in China and Social Development Department of China State Council Development Research Center (2006). China: Health, poverty and economic development. Beijing: WHO representative in China. http://www.wpro.who.int/NR/rdonlyres/A1F18401-BE93-44EF-9F76-55DDA2C6E12D/0/hped_en.pdf. Accessed June 7, 2010.
- 2.Dollar D. Poverty, inequality and social disparities during China’s economic reform. Washington DC: World Bank. http://www.wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2007/06/13/000016406_20070613095018/Rendered/PDF/wps4253.pdf. Accessed June 7, 2010.
- 3.WHO. Geneva: World Health Organization. http://www.who.org/. Accessed June 7, 2010.
- 4.Liu Y, Hsiao WC, Eggleston K. Equity and health care: The Chinese experience. Social Science & Medicine. 1999;49:1349–1356. doi: 10.1016/S0277-9536(99)00207-5. [DOI] [PubMed] [Google Scholar]
- 5.UNDP (2005). New York: United Nations Development Programme. China Human Development Report 2005: Development with Equity. http://ch.undp.org.cn/downloads/nhdr2005/c_NHDR2005_complete.pdf. Accessed June 7, 2010.
- 6.UNDP (2007/8). New York: United Nations Development Programme. China Human Development Report 2007/8: Access for all: Basic public services for 1.3 billion people. http://www.undp.org.cn/downloads/nhdr2008/NHDR2008_en.pdf. Accessed June 7, 2010.
- 7.National Development and Reform Commission (2009). Opinions of the China People’s Congress Central Committee and State Council on deepening the health care system reform. Beijing: National Development and Reform Commission. http://shs.ndrc.gov.cn/ygjd/ygwj/t20090408_271138.htm. Accessed June 7, 2010.
- 8.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Social Science & Medicine. 1991;33(5):545–557. doi: 10.1016/0277-9536(91)90212-U. [DOI] [PubMed] [Google Scholar]
- 9.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: An overview of available measures illustrated with two examples from Europe. Social Science & Medicine. 1997;44(6):757–771. doi: 10.1016/S0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 10.Shi LY. Health care in China: A rural urban comparison after the socioeconomic reforms. Bulletin of the World Health Organization. 1993;71(6):723–736. [PMC free article] [PubMed] [Google Scholar]
- 11.Henderson G, Akin J, Li ZM, Jin SG, Ma HJ, Ge KY. Equity and the utilization of health services: Report of an eight-province survey in China. Social Science & Medicine. 1994;39(5):687–699. doi: 10.1016/0277-9536(94)90024-8. [DOI] [PubMed] [Google Scholar]
- 12.Pei X, Rodriguez E. Provincial income inequality and self-reported health status in China during 1991–7. Journal of Epidemiology Community Health. 2006;60:1065–1069. doi: 10.1136/jech.2005.043539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anson O, Sun S. Health inequalities in rural China: Evidence from Hebei Province. Health Place. 2004;10:75–84. doi: 10.1016/S1353-8292(03)00048-0. [DOI] [PubMed] [Google Scholar]
- 14.Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372:1493–1501. doi: 10.1016/S0140-6736(08)61364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu MY, Sarri R. Women’s health status and gender inequality in China. Social Science & Medicine. 1997;45:1885–1898. doi: 10.1016/S0277-9536(97)00127-5. [DOI] [PubMed] [Google Scholar]
- 16.Anson O, Sun S. Gender and health in rural China evidence from HeBei Province. Social Science & Medicine. 2002;55:1039–1054. doi: 10.1016/S0277-9536(01)00227-1. [DOI] [PubMed] [Google Scholar]
- 17.Shi J, Liu M, Zhang Q, Lu M, Quan H. Male and female adult population health status in China: A cross-sectional national survey. BMC Public Health. 2008;8:277. doi: 10.1186/1471-2458-8-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao J, Qian JC, Tang SL, Eriksson B, Blas E. Health equity in transition from planned market economy in China. Health Policy Plan. 2002;17:20–29. doi: 10.1093/heapol/17.suppl_1.20. [DOI] [PubMed] [Google Scholar]
- 19.Yang GH, Zhao WH, Wan X, Zhai Y, Chen LC, Koplan JP. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372:1697–1705. doi: 10.1016/S0140-6736(08)61366-5. [DOI] [PubMed] [Google Scholar]
- 20.Xu J, Guo R, Huang HY, Zhang Q, Xu J. Self-rated health status of pregnant and postpartum women. Nan Fang Yi Ke Da Xue Xue Bao. 2006;26(7):984–986. [PubMed] [Google Scholar]
- 21.Spiker B, Revicki DA. Taxonomy of quality of life. In: Spiker B, editor. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lippingcott-Raven Publishers; 1996. pp. 25–32. [Google Scholar]
- 22.Hawthorne G, Richardson J, Day NA. A comparison of the assessment of quality of life (AQoL) with four other generic utility instruments. Annals of Medicine. 2001;33:358–370. doi: 10.3109/07853890109002090. [DOI] [PubMed] [Google Scholar]
- 23.Rabin R, de Charro F. EQ-5D: A measure of health status from the EuroQol Group. Annals of Medicine. 2001;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 24.Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: Results from a United Kingdom national questionnaire survey. British Medical Journal. 1998;316:736–741. doi: 10.1136/bmj.316.7133.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szende A, Williams A, editors. Measuring self-reported population health: An international perspective based on EQ-5D. Hungary: Spring Med Publishing Ltd; 2004. [PubMed] [Google Scholar]
- 26.Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utility index. Medical Care. 2005;43(11):1078–1086. doi: 10.1097/01.mlr.0000182493.57090.c1. [DOI] [PubMed] [Google Scholar]
- 27.Fryback DG, Dunham NC, Palta M, Hanmer J, Buechner J, Cherepanov D. US norms for six generic health-related quality of life indexes from the National Health Measurement Study. Medical Care. 2007;45(12):1162–1170. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burström K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Quality of Life Research. 2001;10:621–635. doi: 10.1023/A:1013171831202. [DOI] [PubMed] [Google Scholar]
- 29.Burström K, Johannesson M, Rehnberg C. Deteriorating health status in Stockholm 1998–2002: Results from repeated population surveys using the EQ-5D. Quality of Life Research. 2007;16:1547–1553. doi: 10.1007/s11136-007-9243-z. [DOI] [PubMed] [Google Scholar]
- 30.Sorensen J, Davidsen M, Gudex C, Pedersen KM, Bronnum-Hansen H. Danish EQ-5D population norms. Scandinavian Journal of Public Health. 2009;37:467–474. doi: 10.1177/1403494809105286. [DOI] [PubMed] [Google Scholar]
- 31.König HH, Bernert S, Angermeyer MC, Mattschinger H, Martinez M, Vilagut G. Comparison of population health status in six European countries. Medical Care. 2009;47(2):255–261. doi: 10.1097/MLR.0b013e318184759e. [DOI] [PubMed] [Google Scholar]
- 32.Luo N, Chew LH, Fong KY, Koh DR, Ng SC, Yoon KH. Validity and reliability of the EQ-5D self-report questionnaire in Chinese-speaking patients with rheumatic disease in Singapore. Journal of Rheumatology. 2003;30(10):2268–2274. [PubMed] [Google Scholar]
- 33.Sakamaki H, Ikeagami N, Uchigata Y, Iwamoto Y, Origasa H, et al. Measurement of HRQoL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Health. 2006;9(1):47–53. doi: 10.1111/j.1524-4733.2006.00080.x. [DOI] [PubMed] [Google Scholar]
- 34.Shaheen R, Lindholm L. Quality of life among pregnant women with chronic energy deficiency in rural Bangladesh. Health Policy. 2006;78(2–3):128–134. doi: 10.1016/j.healthpol.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Misajon R, Manderson L, Pallant JF, Omar Z, Bennett E, Rahim RB. Impact, distress and HRQoL among Malaysian men and women with morbidity impairment. Health Quality of Life Outcomes. 2006;12(4):95. doi: 10.1186/1477-7525-4-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park SM, Park MH, Won JH, Lee KO, Choe WS, Heo DS, et al. EuroQol and survival prediction in terminal cancer patients: A multicenter prospective study in hospice-palliative care units. Supportive Care in Cancer. 2006;14(4):329–333. doi: 10.1007/s00520-005-0889-1. [DOI] [PubMed] [Google Scholar]
- 37.Jia TW, Zhou XN, Wang XH, Utzninger J, Steinmann P, Wu XH. Assessment of the age-specific disability weight of chronic shcistosmiasis japonica. Bulletin of World Health Organization. 2007;85(6):458–465. doi: 10.2471/BLT.06.033035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sakthong P, Charoevnisuthiwongs R, Shabunthom R. A comparison of EQ-5D index scores using the UK, US, and Japan preference weights in a Thai sample with type 2 diabetes. Health Quality of Life Outcomes. 2008;23(6):71. doi: 10.1186/1477-7525-6-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, et al. Estimating an EQ-5D population value set: The case of Japan. Health Economics. 2002;11(4):341–353. doi: 10.1002/hec.673. [DOI] [PubMed] [Google Scholar]
- 40.Wang H, David A, Mullahy K, Mullahy J. Variation in Chinese population health related quality of life: Results from a EuroQol study in Beijing, China. Quality of Life Research. 2005;14:119–132. doi: 10.1007/s11136-004-0612-6. [DOI] [PubMed] [Google Scholar]
- 41.Ting JC, Tarn YH, Ching LH, Liou WS, Shaw JW, Chiou XG. Taiwanese version of the EQ-5D: Validation in a representative sample of the Taiwanese population. Journal Formosan Medical Association. 2007;106(12):1023–1031. doi: 10.1016/S0929-6646(08)60078-9. [DOI] [PubMed] [Google Scholar]
- 42.Kil SR, Lee SI, Yun SC, An HM, Jo MW. The decline of health-related quality of life associated with some diseases in Korean adults. Journal of Preventive Medical Public Health. 2008;41(6):434–441. doi: 10.3961/jpmph.2008.41.6.434. [DOI] [PubMed] [Google Scholar]
- 43.Lubetkin EL, Jia H, Gold MR. Construct validity of the EQ-5D in low-income Chinese American Primary care patients. Quality of Life Research. 2004;13(8):1459–1468. doi: 10.1023/B:QURE.0000040793.40831.72. [DOI] [PubMed] [Google Scholar]
- 44.Leung B, Luo N, So L, Quan H. Comparing three measures of health status (perceived health with Likert-type scale, EQ-5D, and number of chronic condition) in Chinese and white Canadians. Medical Care. 2007;45(7):610–617. doi: 10.1097/MLR.0b013e3180331f58. [DOI] [PubMed] [Google Scholar]
- 45.Centre for Health Statistics, Information of Ministry of Health of People’s Republic of China . An analysis report of National Health Services Survey in China, 2008. Beijing, China: Centre for Health Statistics and Information of Ministry of Health of People’s Republic of China; 2009. [Google Scholar]
- 46.Centre for Health Statistics, Information of Ministry of Health of People’s Republic of China . The protocol and guidelines for the 4th National Health Service Survey. Beijing, China: Centre for Health Statistics and Information of Ministry of Health of People’s Republic of China; 2008. [Google Scholar]
- 47.Ravens-Sieberer U, Wille N, Badia X, Bonsel G, Burström K, Cavrini G, et al. Feasibility, reliability, and validity of the EQ-5D-Y: Results from a multinational study. Quality of Life Research. 2010;19(6):887–897. doi: 10.1007/s11136-010-9649-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burström, K., Egmar, A.C., Lugnér, A., Eriksson, M., & Svartengren, M. (2010). A Swedish child-friendly pilot version of the EQ-5D instrument—the development process. European Journal of Public Health. doi:10.1093/eurpub/ckq037. [DOI] [PubMed]
- 49.SAS Institute Inc. (2006). Base SAS®9.1.3 Procedures Guide (Second Ed, Vols. 1, 2, 3, and 4). Cary, NC: SAS Institute Inc.
- 50.Marmot M. The status syndrome: How social standing affects our health and longevity. London: Bloomsbury Publishing Plc.; 2004. [Google Scholar]
- 51.Dahlgren., G., & Whitehead, M. European strategies for tackling social inequalities in health: Levelling up Part II. http://euro.who.int/document/e89384.pdf. Accessed June 7, 2010.
- 52.Whitehead, M., & Dahlgren., G. Concepts and principles for tackling social inequities in health: Levelling up Part I. http://euro.who.int/document/e89383.pdf. Accessed June 7, 2010.
- 53.Bowling A, Bond M, Jenkinson C, Lamping DL. Short form 36 (SF-36) health survey questionnaire: Which normative data should be used? Comparisons between the norms provided by the Omnibus Survey in Britain, the Health Survey for England and the Oxford Health Life Survey. Journal of Public Health Medicine. 1999;21(3):255–270. doi: 10.1093/pubmed/21.3.255. [DOI] [PubMed] [Google Scholar]
- 54.Weinberger M, Oddone EZ, Samsa GP, Landsman PB. Are health-related quality of life measures affected by the mode of administration? Journal of Clinical Epidemiology. 1996;49(2):135–140. doi: 10.1016/0895-4356(95)00556-0. [DOI] [PubMed] [Google Scholar]
- 55.Bowling A. Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health (Oxf) 2005;27:281–291. doi: 10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
- 56.Norman R, King M, Clarke D, Viney R, Cronin P, Street D. Does mode of administration matter? Comparison of on line and face-to-face administration of a time trade-off task. Quality of Life Research. 2010;19:499–508. doi: 10.1007/s11136-010-9609-5. [DOI] [PubMed] [Google Scholar]
- 57.Wu AW, Jacobson DL, Berzon RA, Revicki DA, van der Horst C, Fichtenbaum CJ, et al. The effect of mode of administration of medical outcomes study health ratings and EuroQol scores in AIDS. Quality of Life Research. 1997;6:3–10. doi: 10.1023/a:1026471020698. [DOI] [PubMed] [Google Scholar]
- 58.Bharmal M, Thomas J. Comparing the EQ-5D and SF-6D descriptive systems to assess their ceiling effects in the US general population. Value in Health. 2006;9(4):262–271. doi: 10.1111/j.1524-4733.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- 59.Lubetkin EI, Jia HM, Franks P, Gold MR. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: Examining the EQ-5D in the U.S. general population. Quality of Life Research. 2005;14:2187–2196. doi: 10.1007/s11136-005-8028-5. [DOI] [PubMed] [Google Scholar]
- 60.Fu AZ, Kattan MW. Racial and ethnic differences in preference-based health status measure. Current Medical Research Opinion. 2006;22(12):2348–2349. doi: 10.1185/030079906X148391. [DOI] [PubMed] [Google Scholar]
- 61.Central People’s Government of the People’s Republic of China (2004). Zhongguo de she hui bao zhang zhuang kuang he zheng ce. Situation and policy regarding China’s social welfare. (In Chinese).
- 62.National Bureau of Statistics of China (2009). China Statistic Yearbook 2008. http://www.stats.gov.cn/tjsj/ndsj/2009/indexeh.htm. Accessed August 24, 2010.
- 63.Sen A. Health: Perception versus observation: Self reported morbidity has severe limitations and can be extremely misleading. British Medical Journal. 2002;324:860–861. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Symon Z, Daignault S, Symon R, Dunn RL, Sanda MG, Sandler HM. Measuring patient’s expectations regarding health-related quality-of-life outcomes associated with prostate cancer surgery or radiotherapy. Urology. 2006;68(6):1224–1229. doi: 10.1016/j.urology.2006.08.1092. [DOI] [PubMed] [Google Scholar]
- 65.Sun, S., Chen, J., Johannesson, M., Kind, P., Xu, L., Zhang, Y., & Burström, K. (2010). Regional differences in health status in China: Population EQ-5D results from the National Health Services Survey 2008. (Submitted). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.