Abstract
Background
A substantial group of patients with gallstone disease experience negative outcome after surgical removal of the gallbladder (cholecystectomy). Early identification of these patients is important.
Purpose
The aim of the study is to identify predictors (clinical symptoms and trait anxiety) of negative symptomatic outcomes at 6 weeks after cholecystectomy.
Methods
Consecutive patients (n = 133), 18–65 years, with symptomatic gallstone disease, completed symptom checklists and the state-trait anxiety inventory preoperatively and at 6 weeks after cholecystectomy.
Results
High trait anxiety was the only predictor of persistence of biliary symptoms at 6 weeks after cholecystectomy (OR = 6.88).
Conclusion
In addition to clinical symptoms, high trait anxiety is a predictor of negative symptomatic outcome at 6 weeks after cholecystectomy. Trait anxiety should be evaluated to aim at a patient-tailored approach in gallstone disease.
Keywords: Cholecystectomy, Trait anxiety, Symptomatic gallstone disease
Introduction
Surgical removal of the gallbladder (cholecystectomy) is the standard procedure in case of symptomatic gallstone disease. Positive outcomes are reported after cholecystectomy, such as relief of biliary pain (74–96%), a decrease of lower abdominal pain (66–91%), and less dyspepsia (46–89%) [1, 2], On the other hand, a substantial group of patients report disappointing results after cholecystectomy, such as the persistence and development of new symptoms and pain [2–7]. Early recognition of these patients is crucial to optimize clinical decision making.
Poor post-cholecystectomy outcome is associated with clinical factors, such as high comorbidity, heightened pain sensitivity, a long history of complaints (biliary pain, symptoms, attacks), preoperative dyspeptic symptoms, and the use of psychotropic medication [2, 5, 8–12]. Stable personality traits, such as neuroticism [13–15] and introversion [10, 15], also have a negative impact on long- and short-term outcomes, such as medication use and pain. Trait anxiety [16] is a dimensional aspect of personality related to neuroticism [17]. Trait anxiety is defined as a relatively stable individual difference in the tendency to react with heightened anxiety to threatening situations [16]. The impact of trait anxiety on post-cholecystectomy recovery is indistinct [15, 18–20], as studies investigated small populations [15, 18, 20] and focussed on the first 5 days after cholecystectomy only. Evidence of the impact of trait anxiety on post-cholecystectomy outcome is flawed as studies used different procedures and outcome variables, and controlled for different pre- and postoperative factors. We hypothesized that high trait anxiety is a risk factor of negative post-cholecystectomy outcome, next to clinical risk factors. Clinical experience teaches that the majority of patients report a relief of symptoms and return to work at 6 weeks after discharge [21]. Therefore, we investigated the impact of high trait anxiety on a symptomatic outcome at 6 weeks after discharge.
Methods
Patients
The current study was performed at the Department of Surgery of the St. Elisabeth Hospital in Tilburg, The Netherlands. Consecutive patients (18–65 years) with diagnosed symptomatic gallstone disease, awaiting an elective laparoscopic cholecystectomy, were eligible for the study. Exclusion criteria are: suffering from severe or life-threatening systemic diseases (American Society of Anaesthetists class III and IV), undergoing an emergency procedure or intended open cholecystectomy, insufficient knowledge of the Dutch language, choledocholithiasis, cholangitis, known pregnancy, known liver cirrhosis, history of abdominal malignancy, previous upper abdominal surgery (precluding laparoscopic approach), and psychiatric diseases. All patients were subjected to a standard surgical and anaesthetic procedure.
Procedure
The protocol of the study was approved by the local ethics committee. Patients signed informed consent before participation. Medical records were checked for medical history and somatic comorbidities. Before admission and 6 weeks after cholecystectomy, patients completed and returned a set of self-report questionnaires.
Questionnaires
The demographic questionnaire that was completed preoperatively, asked about sex and age. Preoperatively and at 6 weeks after cholecystectomy, patients completed a symptom checklist. Patients were asked to indicate whether they were bothered by one or more symptoms related to gallstone disease in the past week. Categorisation into biliary, dyspeptic, and non-specific symptoms was based on the study of Weinert et al. [6].
After surgery, surgical reports were checked for the presence of gallstones/sludge and conversion for a laparoscopic procedure to open cholecystectomy. At 6 weeks postoperatively, medical reports were checked for the number and moment of surgical consultations after cholecystectomy, visits to the emergency ward, and admissions to the hospital in relation to the cholecystectomy.
Patients completed the 20-item trait scale of the state-trait anxiety inventory preoperatively. Trait anxiety reflects the extent of anxiety that patients generally feel and remains stable over time and between pre- and postoperative conditions [16]. The trait anxiety measure of the state-trait anxiety inventory has good test–retest reliability and internal consistency [22]. Patients with a score above the 80th percentile cutoff score were indicated as patients with high trait anxiety [23, 24]. The size of the subgroup provided sufficient statistical power.
Statistical Analyses
Chi-square and Student’s t tests were used to investigate differences between participating patients and patients who refused or ended participation sooner than 6 weeks (dropouts) and differences between patients with and without high trait anxiety. Changes in the report of categories of symptoms over time were calculated using McNemar tests. Persistence of symptoms was defined as patients reporting one or more symptoms within a specific category both before and after cholecystectomy. Emergence was defined as patients not reporting one or more symptoms within a specific category before cholecystectomy, but reporting symptoms within this category at 6 weeks. Persistence and emergence rates were calculated using frequencies. Predictors of the persistence and emergence of symptoms were calculated by multivariate logistic regression, inserting sex, age, the report of preoperative biliary, dyspeptic and non-specific symptoms, and high trait anxiety (Method Enter).
Results
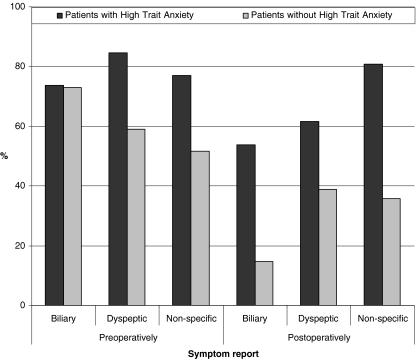
In total, 239 patients were found eligible for this study. Six patients were not contacted before cholecystectomy, 23 patients were treated expectantly, and 15 patients refused to participate. Preoperatively, 195 patients received the first questionnaire, which was not returned by 28 patients. In the course of 6 weeks, six patients ended the participation. At 6 weeks postoperatively, patients received a second questionnaire, which 25 patients did not return. Only patients who returned both questionnaires were included (n = 136; response rate 69.7%). Because of missing data, statistical analyses were performed on 133 patients. Clinical and demographic characteristics are shown in Table 1. All included patients had experienced biliary or dyspeptic symptoms before surgical consultation. Gallstones or sludge were demonstrated in 90.4% and 8.8% of the patients, respectively. In five patients, laparoscopic cholecystectomy was converted to an open procedure. No differences were found between participating patients and patients who did not return their questionnaires or ended participation within 6 weeks. Preoperatively, 12.5% of the male patients and 24.7% of the female patients had high trait anxiety. Patients with high trait anxiety did not differ from other patients on clinical and demographic characteristics and time frame before completion of the postoperative questionnaire. Preoperatively, the report of biliary, dyspeptic, and non-specific symptoms was the same for patients with and without high trait anxiety ((n = 26) and (n = 95), respectively). These results are shown in Fig. 1.
Table 1.
Baseline characteristics (n = 133)
| Demographic characteristics | |
|---|---|
| Male patients (%) | 24.1 |
| Age (M ± SD) | 47.2 ± 12.1 |
| Preoperative biliary symptoms (%) | 72.0 |
| Upper abdominal pain (%) | 65.9 |
| Nausea (%) | 39.1 |
| Vomiting (%) | 16.5 |
| Preoperative dyspeptic symptoms (%) | 64.7 |
| Bad taste (%) | 25.6 |
| Heartburn (%) | 26.3 |
| Lower abdominal pain (%) | 22.6 |
| Diarrhoea (%) | 14.3 |
| Flatulence (%) | 35.5 |
| Preoperative non-specific symptoms (%) | 54.1 |
| General malaise (%) | 10.5 |
| Fatigue (%) | 46.6 |
| Weight change (%) | 3.0 |
| Decreased sexual functioning (%) | 7.5 |
| Other health complaints (%) | 13.5 |
| Time between cholecystectomy and surgical consultation (M ± SD, days) | 39.44 ± 23.44 |
Fig. 1.
Symptom report of patients with and without high trait anxiety
Benefit of Surgery
At 6 weeks, patients with high trait anxiety more often experienced biliary and non-specific symptoms than patients without high trait anxiety ((53.8% versus 14.7%, χ 2 = 15.43, p < 0.001) and (80.8% versus 35.8%, χ 2 = 14.89, p < 0.001), respectively; Fig. 1). In the course of 6 weeks after cholecystectomy, the report of biliary and dyspeptic symptoms did not change in patients with high trait anxiety. In contrast, the percentages of patients without high trait anxiety experiencing biliary and dyspeptic symptoms reduced from 73.1% to 14.7% (χ 2 = 46.75, p < 0.001) and from 64.7% to 46.6% (χ 2 = 9.12, p = 0.003), respectively. In both groups of patients, the report of non-specific symptoms did not change. Compared with other patients, patients with high trait anxiety more often reported the persistence and emergence of biliary symptoms postoperatively ((18.6% versus 57.9%, χ 2 = 10.70, p = 0.001) and (4.0% versus 42.9%, χ 2 = 4.42, p = 0.025), respectively). The persistence and emergence of dyspeptic symptoms and persistence of non-specific symptoms were equally reported in patients with and without high trait anxiety. However, at 6 weeks post-cholecystectomy, patients with high trait anxiety reported the emergence of new non-specific symptoms more often (95.0% versus 49.0%; χ 2 = 10.93, p = 0.001).
Prediction of Postoperative Symptoms
Multivariate logistic regression analyses showed that high trait anxiety was the only predictor of persisting biliary symptoms at 6 weeks after cholecystectomy (Table 2). Preoperative biliary symptoms and high trait anxiety both predicted the persistence of non-specific symptoms. No predictors could be identified for the persistence of dyspeptic symptoms or the emergence of new symptoms at 6 weeks post-cholecystectomy.
Table 2.
Predictors of symptomatic outcomes at 6 weeks post-cholecystectomy (only significant results are reported)
| Symptomatic outcome | Preoperative predictor | OR | 95% CI | p |
|---|---|---|---|---|
| Persistent biliary symptoms | High trait anxiety | 6.88 | 1.78–26.58 | 0.005 |
| Persistent non-specific symptoms | Biliary symptoms | 5.22 | 1.03–26.45 | 0.046 |
| High trait anxiety | 45.86 | 4.31–488.51 | 0.002 |
Multivariate logistic regression, method enter was used entering sex, age, high trait anxiety, preoperative biliary, dyspeptic, and non-specific symptoms as variables
Discussion
Although cholecystectomy is the treatment of choice in symptomatic gallstone disease, many patients report persisting symptoms. The key issue is to identify patients with a heightened risk of negative outcomes. Preoperative symptoms have been investigated most thoroughly, and dyspeptic symptoms are found to be risk factors for long-term outcomes after cholecystectomy (>6 months) [6, 9, 10]. This prospective follow-up study provides evidence that personality, in this case high trait anxiety (>80th percentile score on the trait scale of the state-trait anxiety inventory), has an impact on post-cholecystectomy recovery after controlling for preoperative symptom report. In fact, high trait anxiety is the only predictor of persistent biliary symptoms after cholecystectomy, whereas preoperative symptoms are not. The odds that patients with high trait anxiety reported persistent biliary symptoms was 6.88 times the odds observed for patients without high trait anxiety.
Former studies on the impact of personality on outcomes after cholecystectomy led to inconclusive evidence. Preoperative neuroticism was a predictor of short-term outcomes, such as pain, mood, and the use of narcotics <7 days after cholecystectomy [15, 25], but was not associated with persisting pain at 1 year [26]. In addition, introversion predicts pain at 1 year after cholecystectomy [10]. Findings from the current study suggest that trait anxiety may be a predictor of long-term outcomes after cholecystectomy. Previous studies on trait anxiety did not provide strong support for an impact on post-cholecystectomy outcomes [15, 19, 20]. These studies generated inconsistent findings, were based on small populations, and focussed on short-term post-cholecystectomy outcomes (<5 days post-operatively) only. Patients with high scores on trait anxiety have higher pain sensitivity [27] and suffer from gastro-intestinal conditions more often [28]. Besides, high trait anxiety may lead to an attentional bias on bodily sensations and symptoms [29]. As diagnosing symptomatic gallstone disease is complex and patients with gastro-intestinal symptoms are erroneously indicated for cholecystectomy, patients with high trait anxiety may be at risk for poor decision making. Negative symptomatic outcomes may be the result.
This study has a prospective follow-up design, which enables us to follow the course of symptoms across time. Inclusion of consecutive patients visiting the outpatient clinic in the study prevented a selection bias and minimized the influence of confounding variables at 6 weeks postoperatively. Participants, non-participants and dropouts did not differ on demographic and clinical characteristics. Furthermore, participants and dropouts did not differ on the report of symptoms and high trait anxiety. However, as data on the report of preoperative symptoms and high trait anxiety were not collected, a bias cannot be precluded. We used a self-constructed symptom checklist, based on literature, clinical experience, and information from focus groups. Furthermore, as the number of patients above the 80th percentile score is relatively small, some results of this study may not reach significance because of the limited sample size. Six weeks after discharge is chosen as moment of follow-up, as patients experience greatest symptomatic improvement within this period [21]. Although this time point is suitable for a first inventory of post-cholecystectomy outcomes, further research is needed to establish a relationship between high trait anxiety and long-term post-cholecystectomy outcomes and to corroborate the following recommendations.
Trait anxiety is a predictive factor worth paying attention to in clinical decision making. Integrating information about current symptoms, medical history, and level of trait anxiety may be essential to come to a genuine patient-tailored approach in gallstone disease. Patients with high trait anxiety should be informed about the high risk of persisting symptoms after cholecystectomy. Expectative management should be considered. To reduce the amount of clinically unsuccessful cholecystectomies, guidelines for the indication of a cholecystectomy may be tightened, integrating new insights on the impact of personality.
Acknowledgments
Conflicts of Interest
None
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Berger MY, Olde Hartman TC, Bohnen AM. Abdominal symptoms: Do they disappear after cholecystectomy? Surg Endosc. 2003;17(11):1723–8. doi: 10.1007/s00464-002-9154-6. [DOI] [PubMed] [Google Scholar]
- 2.Mertens MC, De Vries J, Scholtes VP, Jansen P, Roukema JA. Prospective 6 weeks follow-up post-cholecystectomy: The predictive value of pre-operative symptoms. J Gastrointest Surg. 2009;13(2):304–11. doi: 10.1007/s11605-008-0718-1. [DOI] [PubMed] [Google Scholar]
- 3.Ross E, Zambon D. Postcholecystectomy symptoms. A prospective study of gallstone patients before and two years after surgery. Gut. 1987;28:1500–4. doi: 10.1136/gut.28.11.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu Farsakh NA, Stietieh M, Abu Farsakh FA. The postcholecystectomy syndrome. A role for duodenogastric reflux. J Clin Gastroenterol. 1996;22(3):197–201. doi: 10.1097/00004836-199604000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Luman W, Adams WH, Nixon SN, McIntyre IM, Hamer-Hodges D, Wilson G, et al. Incidence of persistent symptoms after laparoscopic cholecystectomy: A prospective study. Gut. 1996;39(6):863–6. doi: 10.1136/gut.39.6.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinert CR, Arnett D, Jacobs D, Kane R. Relationship between persistence of abdominal symptoms and succesfull outcome after cholecystectomy. Arch Intern Med. 2000;160:989–95. doi: 10.1001/archinte.160.7.989. [DOI] [PubMed] [Google Scholar]
- 7.Vetrhus M, Berhane T, Søreide O, Søndenaa K. Pain persists in many patients five years after removal of the gallbladder: Observations from two randomized controlled trials of symptomatic, noncomplicated gallstone disease and acute cholecystitis. J Gastrointest Surg. 2005;6:826–31. doi: 10.1016/j.gassur.2005.01.291. [DOI] [PubMed] [Google Scholar]
- 8.Diehl AK. Symptoms of gallstone disease. Baillieres Clin Gastroenterol. 1992;6(4):635–57. doi: 10.1016/0950-3528(92)90044-F. [DOI] [PubMed] [Google Scholar]
- 9.McMahon AJ, Ross S, Baxter JN, Russell IT, Anderson JR, Morran CG, et al. Symptomatic outcome 1 year after laparoscopic and minilaparotomy cholecystectomy: A randomized trial. Br J Surg. 1995;82(10):1378–82. doi: 10.1002/bjs.1800821028. [DOI] [PubMed] [Google Scholar]
- 10.Borly L, Anderson IB, Bardram L, Christensen E, Sehested A, Kehlet H, et al. Preoperative prediction model of outcome after cholecystectomy for symptomatic gallstones. Scand J Gastroenterol. 1999;34(11):1144–52. doi: 10.1080/003655299750024968. [DOI] [PubMed] [Google Scholar]
- 11.Lyass S, Perry Y, Venturero M, Muggia-Sullam M, Eid A, Durst A, et al. Laparoscopic cholecystectomy: What does affect the outcome? A retrospective multifactorial regression analysis. Surg Endosc. 2000;14(7):661–5. doi: 10.1007/s004640000096. [DOI] [PubMed] [Google Scholar]
- 12.Bisgaard T, Rosenberg J, Kehlet H. From acute to chronic pain after laparoscopic cholecystectomy: A prospective follow-up analysis. Scand J Gastroenterol. 2005;40(11):1358–64. doi: 10.1080/00365520510023675. [DOI] [PubMed] [Google Scholar]
- 13.Dalrymple DG, Parbrook G, Steel DF. Factors predisposing to postoperative pain and pulmonary complications: A study of female patients undergoing elective cholecystectomy. Br J Anaesth. 1973;45(6):589–98. doi: 10.1093/bja/45.6.589. [DOI] [PubMed] [Google Scholar]
- 14.Parbrook GD, Dalrymple D, Steel DF. Personality assessment and postoperative pain and complications. J Psychosom Res. 1973;17(4):277–85. doi: 10.1016/0022-3999(73)90104-9. [DOI] [PubMed] [Google Scholar]
- 15.Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986;24(3):331–42. doi: 10.1016/0304-3959(86)90119-3. [DOI] [PubMed] [Google Scholar]
- 16.Spielberger CD. Emotional reactions to surgery. J Consult Clin Psychol. 1973;40(1):33–8. doi: 10.1037/h0033982. [DOI] [PubMed] [Google Scholar]
- 17.Reiss S. Trait Anxiety: It’s not what you think it is. J Anxiety Dis. 1997;11(2):201–14. doi: 10.1016/S0887-6185(97)00006-6. [DOI] [PubMed] [Google Scholar]
- 18.Scott LE, Clum GA, Peoples JB. Preoperative predictors of postoperative pain. Pain. 1983;15(3):283–93. doi: 10.1016/0304-3959(83)90063-5. [DOI] [PubMed] [Google Scholar]
- 19.Levesque L, Grenier R, Kerouac S, Reidy M. Evaluation of a pre-surgical group program given at two different times. Res Nurs Health. 1984;7:227–36. doi: 10.1002/nur.4770070311. [DOI] [PubMed] [Google Scholar]
- 20.Boeke S, Stronks D, Verhage F, Zwaveling A. Psychological variables as predictors of the length of post-operative hospitalization. J Psychosom Res. 1991;35(2–3):281–8. doi: 10.1016/0022-3999(91)90082-Y. [DOI] [PubMed] [Google Scholar]
- 21.Donceel P, Du Bois M. Fitness for work after laparoscopic and open cholecystectomy. Acta Chir Belg. 1997;97(4):168–72. [PubMed] [Google Scholar]
- 22.Van de Ploeg HM. De Zelf-Beoordelings Vragenlijst (STAI-DY) De ontwikkeling en validatie van een Nederlandstalige vragenlijst voor het meten van angst. Tijdschrift voor psychiatrie. 1982;24(9):576–88. [Google Scholar]
- 23.Mertens MC, Roukema JA, Scholtes VP, De Vries J. Trait anxiety predicts unsuccessful surgery in gallstone disease. Psychosom Med. 2010;72(2):198–205. doi: 10.1097/PSY.0b013e3181cb65b4. [DOI] [PubMed] [Google Scholar]
- 24.van der Steeg AF, De Vries J, van der Ent FW, Roukema JA. Personality predicts quality of life six months after the diagnosis and treatment of breast disease. Ann Surg Oncol. 2007;14(2):678–85. doi: 10.1245/s10434-006-9175-9. [DOI] [PubMed] [Google Scholar]
- 25.Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001;90(3):261–9. doi: 10.1016/S0304-3959(00)00406-1. [DOI] [PubMed] [Google Scholar]
- 26.Jess P, Jess T, Beck H, Bech P. Neuroticism in relation to recovery and persisting pain after laparoscopic cholecystectomy. Scand J Gastroenterol. 1998;33(5):550–3. doi: 10.1080/00365529850172151. [DOI] [PubMed] [Google Scholar]
- 27.Watson D, Pennebaker JW. Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychol Rev. 1989;96(2):234–54. doi: 10.1037/0033-295X.96.2.234. [DOI] [PubMed] [Google Scholar]
- 28.Addolorato G, Mirijello A, D’Angelo C, Leggio L, Ferrulli A, Abenavoli L, et al. State and trait anxiety and depression in patients affected by gastrointestinal diseases: Psychometric evaluation of 1641 patients referred to an internal medicine outpatient setting. Int J Clin Pract. 2008;62(7):1063–9. doi: 10.1111/j.1742-1241.2008.01763.x. [DOI] [PubMed] [Google Scholar]
- 29.Eifert G, Coburn K, Seville J. Putting the client in control: The perception of control in the behavioral treatment of anxiety. Anxiety, Stress and Coping. 1992;5:165–76. doi: 10.1080/10615809208250495. [DOI] [Google Scholar]