Abstract
Objective
To compare multi-detector CT (MDCT) using 128-slice coronary CT angiography (Definition AS+, Siemens Medical Solution, Forchheim, Germany) with ECG-based maximum tube current modulation with echocardiography for the determination of left ventricular ejection fraction (LVEF), end-diastolic volume (EDV), end-systolic volume (ESV), as well as assessing coronary artery image quality and patient radiation dose.
Materials and Methods
Thirty consecutive patients (M:F = 20:10; mean age, 57.9 ± 11.4 years) were referred for MDCT for evaluation of atypical chest pain. EF, EDV and ESV were determined for both MDCT and echocardiography, and the correlation coefficients were assessed. Coronary artery segment subjective image quality (1, excellent; 4, poor) and radiation dose were recorded.
Results
Left ventricular EF, EDV, and ESV were calculated by MDCT and echocardiography and the comparison showed a significant correlation with those estimated by echocardiography (p < 0.05). Consistently, the LVEFs calculated by MDCT and echocardiography were not statistically different. However, LV, EDV and ESV from MDCT were statistically higher than those from echocardiography (p < 0.05). The average image quality score of the coronary artery segment was 1.10 and the mean patient radiation dose was 3.99 ± 1.85 mSv.
Conclusion
Although LV volume was overestimated by MDCT, MDCT provides comparable results to echocardiography for LVEF and LVV, with a low radiation dose.
Keywords: MDCT, Coronary Artery Disease, Left ventricular function, Echocardiography, Radiation
INTRODUCTION
In recent years, the multi-detector CT (MDCT) has been used with increasing frequency as a non-invasive modality for the assessment of coronary artery diseases (CAD). In addition to CAD assessment, MDCT allows left ventricular (LV) function and volume assessment (1-4). As well, the accurate evaluation of LV function and volumes is likely to optimize the clinical evaluation of patients with CAD (5). However, radiation hazard has been a reason for concern in the performance of coronary CT angiography (CCTA). In order to minimize the exposed radiation dose during examination of CCTA using MDCT, several strategies have been developed including retrospective electrocardiography (ECG)-dependent tube current modulation, tube voltage reduction, attenuation-based tube current modulation, and prospective ECG triggering (step-and-shoot mode) techniques (6-8).
Prospective ECG triggering (step-and-shoot) techniques are one of these low-dosed CCTA techniques, but it does not give information about LV function and volume because it does not cover 100% of the cardiac phase despite the lower radiation dose. Recently developed CT scanners such as dual source MDCT and 128-slice MDCT, have allowed the ability to perform CCTA with low patient radiation exposure levels by decreasing the tube current to 4% during the non-reconstructed phase (mindose®) in all scanned phases (9). Accordingly, we supposed that CCTA with mindose® would allow for the assessment of both the coronary artery anatomy, LV function, and volume with low patient radiation exposure.
The aim of this study was to compare 128-slice coronary CT angiography with mindose® with echocardiography with respect to LVEF and LV volume in patients with chest pain, and to assess coronary artery image quality and patient radiation dose in a group of patients who underwent 128-slice CCTA with mindose®.
MATERIALS AND METHODS
Study Design and Population
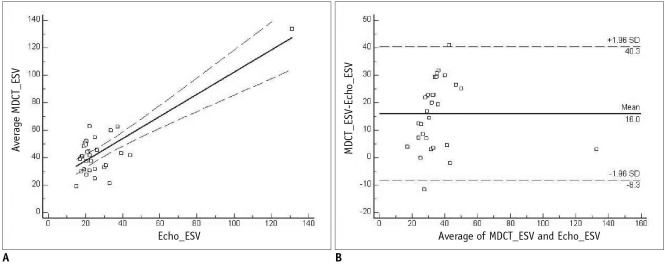
We retrospectively analyzed 30 consecutive patients (M:F = 20:10; mean age, 57.9 ± 11.4 years) who presented at our hospital with atypical chest pain and underwent both CCTA and subsequent echocardiography between January 2009 and March 2009. All patients underwent CCTA and echocardiography on the same day. Exclusion criteria were unstable angina or acute coronary syndrome, previous history of percutaneous coronary stent implantation or coronary bypass graft surgery, atrial fibrillation or other cardiac arrhythmia, hypersensitivity to iodinated contrast media, absolute contraindication to β-blocker, impaired renal function (serum creatinine level > 1.5 mg/dL), pregnancy or lactation, and the inability to hold the breath for 15 seconds. Table 1 lists the clinical characteristics of the patients. All patients signed informed consent forms for CCTA and echocardiography, and the Institutional Review Board approved this study.
Table 1.
Clinical Characteristics of Study Population
Patient Preparation
Prior to CCTA examination, the blood pressure and heart rate of each patient were measured. In all patients with a resting heart rate exceeding 65 beats per minute, an oral dose of short-acting beta-blocker (propranolol 10-40 mg) was administered one hour before CT scan in order to obtain a heart rate below 65 beats per minute. No additional intravenous beta-blocker was administered at the time of the examinations. Vital signs including blood pressure, heart rate, oxygen saturation of arterial blood, and ECG were monitored in the scanning room.
128-Slice Multi-Detector CT Scanning Protocol
Coronary CT angiography examinations were performed on a 128-slice MDCT (Definition As+, Siemens Medical Solution, Germany) with a rotation time of 300 msec, and a slice collimation of 128 × 0.6 mm using a continuous helical scan mindose® technique. The CT scan was triggered automatically by the arrival of the main contrast bolus (automatic bolus tracking) technique. A region of interest was placed into the ascending aorta, and image acquisition began 6 seconds after the signal density level reached the predefined threshold of 100 Hounsfield units (HU). For all CT examinations, a dual-head power injector (Stellant D; Medrad, Indianola, IA) was used to administer a dual-phase bolus at a rate of 5 mL per second: At first, 70 mL of iopromide (ultravist 370, BSP, Germany) was administered and this was followed by the administration of 20 mL of an 80% to 20% mix of ultravist 370 and saline. Retrospective CCTA with mindose® was performed with the following parameters: helical scanning, 0.16-0.22 pitch, use of ECG-dependent tube current modulation (tube current of 160 mA during 50-80% of R-R interval and minimal tube current of 6.4 mA during the remainder of the R-R interval based on the patient's age and weight/height: 100 kVp when BMI was less than 25, 120 kVp when BMI was 25 or more).
128-Slice Multi-Detector Angiography Image Reconstruction and Analysis
Firstly, images were reconstructed at 50-80% of the R-R interval in 5% increments to obtain optimal coronary artery images and then other images were reconstructed at 10-100% of the R-R interval in 10% increments for the assessment of LV function and volume. For the reconstruction of axial images obtained by CT scan, we used a slice thickness of 0.7 mm and a slice width of 0.4 mm with the use of a small- or medium-sized cardiac field of view. A medium-hard algorithm was used for reconstruction and all CT data sets were transferred to a dedicated workstation (Leonard, Siemens Medical Solutions). All different 10 phase images were assessed if they could have a good enough quality for discriminating between the lumen and endocardium from two radiologists by consensus on a short axis image.
Left ventricular function and volume were evaluated by two independent radiologists at 10-100% of the R-R interval using dedicated software (Circulation, Siemens Medical Solutions) with a semiautomated LV endocardial and epicardial contour detection technique. Inter-observer variability was analyzed by comparing the parameter measurements of two radiologists with seven years and two years experience in cardiac imaging, respectively.
Two-Dimensional Transthoracic Echocardigraphy
Two-dimensional transthoracic echocardiography (2D-TTE) was performed with one machine (Acuson Sequoia, Siemens Medical Solution, USA) as a standard reference for the evaluation of LV function and volume. All patients were placed in the left lateral decubitus position for the examination. Images were obtained in the standard 4- and 2-chamber apical views with a 3.5-MHz transducer by a cardiologist with 10 years of experience and blinded to the MDCT data. LV function and volume were estimated according to the modified Simpson's method (10).
Radiation Dose
The dose-length product (DLP, measured in milligray-centimeters) is defined as the volume CT dose index multiplied by the scan length and is an indicator of the integrated radiation dose of the entire CT examination. DLP was displayed on the dose report on the CT scanner and was recorded. A reasonable approximation of the effective radiation dose (E) of coronary CT angiography was calculated by multiplying DLP by a conversion coefficient for the chest and coronary arteries (k = 0.014 mSv/[mGy × cm]) (11).
Statistical Analysis
All statistical analyses were performed with statistical software (SPSS, version 12.0 for Windows; SPSS, Chicago, IL). Continuous data were presented as the mean ± standard deviation (SD) and compared using the paired two-tailed Student's t-test. Agreement for the LVEF and volume by MDCT and TTE was assessed by Pearson's correlation coefficient for linear regression and Bland-Altman analysis. The Pearson's correlation coefficient was valued as follows: poor = 0; slight = 0.01-0.20; fair = 0.21-0.40; moderate = 0.41-0.60; good = 0.61-0.80; excellent = 0.80-1.00. Inter-observer variability of LVEF and LV were measured by two MDCT readers was also assessed using Pearson's correlation.
RESULTS
Left Ventricular Ejection Fraction
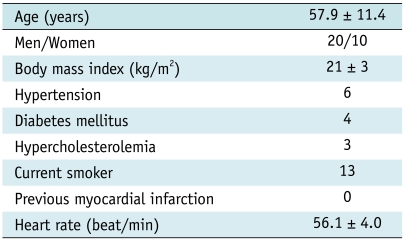
The average LVEF calculated by MDCT was 64.9 ± 9.60%, as opposed to 65.8 ± 8.68% by TTE (p = 0.53). The evaluation of LVEF by linear regression analysis demonstrated good correlation between MDCT and TTE (r2 = 0.68. p < 0.001) (Fig. 1A). A Bland-Altman analysis showed a mean difference of 0.9 ± 0.92% for LVEF between MDCT and TTE (Fig. 1B).
Fig. 1.
Comparison of multi-detector CT (MDCT) and two-dimensional echocardiography in assessment of left ventricular ejection fraction.
A. Linear regression plot shows correlation between left ventricular ejection fraction (EF) calculated by 128-slice multidetector CT and two-dimensional echocardiography. B. Bland-Altman plot of left ventricular ejection fraction shows difference between each pair plotted against average value of same pair and mean value of differences ± 2 standard deviations (SDs).
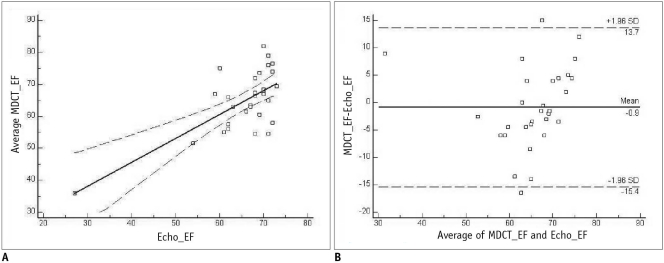
Left Ventricular End-Diastolic Volume
The average LVEDV by MDCT was 122.2 ± 22.01 mL, compared to 114.0 ± 19.19 mL by TTE. The average LVEDV measured by MDCT was significantly higher than LDEDV by TTE (p = 0.001). A linear regression analysis showed a good correlation between MDCT and 2D-echocardiography for the assessment of LVEDV (r2 = 0.82, p < 0.001) (Fig. 2A). For the Bland-Altman analysis, a mean difference of 9.0 ± 2.82 mL was observed between MDCT and TTE (Fig. 2B).
Fig. 2.
Comparison of multi-detector CT (MDCT) and two-dimensional echocardiography in assessment of left ventricular end-diastolic volume.
A. Linear regression plot shows correlation between left ventricular end-diastolic volume (EDV) calculated by 128-slice multidetector CT and two-dimensional echocardiography. B. Bland-Altman plot of left ventricular end-diastolic volume shows difference between each pair plotted against average value of same pair and mean value of differences ± 2 standard deviations (SDs).
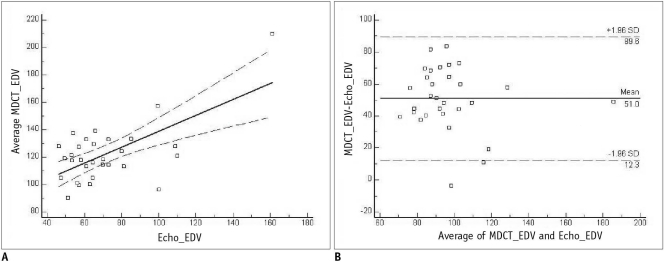
Left Ventricular End-Systolic Volume
For MDCT, the average LVESV was 43.9 ± 20.45 mL, while in comparison, was 41.4 ± 20.73 mL by TTE. Also the average LVESV measured by MDCT was significantly higher than by TTE (p = 0.001). Moreover, the comparison of the correlation coefficients between the two modalities for the assessment of LVESV was good (r2 = 0.97, p < 0.001) (Fig. 3A). The Bland-Altman analysis showed a mean difference of 2.5 ± 0.55 mL between MDCT and TTE (Fig. 3B).
Fig. 3.
Comparison of multi-detector CT (MDCT) and two-dimensional echocardiography in assessment of left ventricular end-systolic volume.
A. Linear regression plot shows correlation between left ventricular end-systolic volume (ESV) calculated by 128-slice multidetector CT and two-dimensional echocardiography. B. Bland-Altman plot of left ventricular end-systolic volume shows difference between each pair plotted against average value of same pair and mean value of differences ± 2 standard deviations (SDs).
The inter-observer agreements for LVEF, LVEDV, and LVESV by MDCT were 0.90, 0.94 and 0.97, respectively.
Overall Image Quality and Radiation Dose
All 10 of the different phase images assessed by the two radiologists by consensus were of good image quality for differentiating the lumen from the endocardium, and the mean radiation doses were 285.2 ± 132.1 mGy × cm in DLP (3.99 ± 1.85 mSv) and 16.8 ± 7.79 mGy for the CTDI vol.
DISCUSSION
The use of MDCT to assess LV function and volume is limited because of radiation hazard and contrast injection risk. The routine use of MDCT is not suggested for functional assessment (12, 13). However, the most obvious indications are the functional assessment of patients who will undergo MDCT for coronary anatomy assessment, particularly for patients in which the TTE images are inadequate, and for those with contraindications to other procedures (e.g., patients with a pacemaker who cannot undergo magnetic resonance imaging) (14).
This study shows that the evaluation of the coronary artery anatomy, LV function, and volume of the CCTA using the mindose® technique for radiation dose saving, are useful for patients that are clinically referred for CT coronary angiography. Good correlations were observed between MDCT and TTE for LVEF, LVEDV, and LVESV. In addition, for all of the coronary artery anatomy, except the anatomical absence or small vessel size, was assessed with a significantly lower radiation dose compared with previous studies.
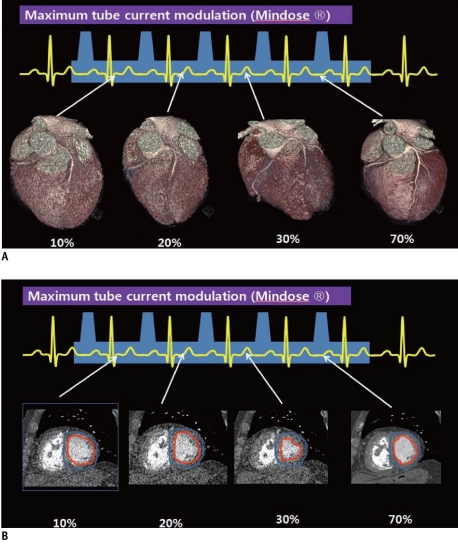
Electrocardiography-based tube current modulation, like the mindose® technique employed in our study, is used with spiral data acquisition to significantly decrease radiation exposure. The tube current is at a maximum only (100% of maximum tube current) during the cardiac phase of interest (mid-diastole) and is reduced substantially outside this phase (4% of maximum tube current). Although coronary artery image quality during periods of low current is limited (Fig. 4A), data for the evaluation of LVEF and volume are available during the entire cardiac cycle (Fig. 4B). Similar to typical CCTA, CCTA with ECG-based tube-current modulation have limitations when scanning patients with arrhythmia. Because tube-current modulation is prescribed before scanning, changes in the heart rate could result in unintended lowering of the tube current during a desired phase of reconstruction for a given cardiac cycle. For this reason, ECG-based tube modulation is not often used with helical imaging for such patients with severe arrhythmia, thus resulting in a very high radiation dose (15).
Fig. 4.
Difference of image quality depending on exposed maxinum tube current.
A. Coronary artery anatomy quality was good at 100% of maximum tube current during mid-diastole and poor outside this phase with 4% of maximum tube current. B. Differentiating endocardium from lumen is available during all cardiac phase including phase with 4% of maximum tube current
In our study, we found that MDCT overestimated LVEDV and LVESV relative to the TTE technique. This finding was consistent to previous studies (1, 3). De Graaf et al. (16) recently suggested that several factors might contribute to the overestimation of LV volumes by MDCT. First, the use of dose modulation is associated with a slight decrease in image quality in images acquired during decreased tube current. However, it is unlikely that this minor decrease in image quality would have affected the global LV volume measurements. Even in our data, ESV, which was probably scanned by low radiation dose, showed a better correlation with TTE than EDV, which was probably scanned with a full radiation dose. Second, the overestimation in MDCT may be explained by differences in the definition of the upper limits of the left ventricle, which can be set at different levels depending on the technique used. Currently, there are no clear guidelines on the systematic analysis of MDCT data for the purpose of cardiac function assessment. Finally, the LV volume calculation differs between MDCT and TTE. While the LV volume measurement is based on geometric assumptions from 2D images in TTE (modified Simpson method), MDCT allows high-resolution endocardial border definition using true 3D reconstruction.
Although the assessment of LVEF, LV volume, and coronary artery anatomy are feasible with CCTA at a low radiation dose, there were several limitations in our study. First, the patients enrolled in this study represent a relatively small group with atypical chest pain. A large prospective study should therefore be performed in both patients with cardiac disease and those without cardiac disease. Second, the use of a beta-blocker in patients with heart rates of more than 65 bpm might affect the assessment of LV function and volume in MDCT. Next-generation CT with high temporal resolution such as wide detector dual-source CT could solve these problems.
In conclusion, the calculation of LVEF, LVEDV, and ESV by 128-slice CCTA with mindose® showed a significant correlation with the estimates by echocardiography and 128 slice-CCTA with mindose® presented coronary artery anatomy with a low radiation dose. In addition, there were no statistical differences between methods for LVEF. However, EDV and ESV from CCTA were significantly higher than those from echocardiography.
References
- 1.Juergens KU, Grude M, Maintz D, Fallenberg EM, Wichter T, Heindel W, et al. Multi-detector row CT of left ventricular function with dedicated analysis software versus MR imaging: initial experience. Radiology. 2004;230:403–410. doi: 10.1148/radiol.2302030042. [DOI] [PubMed] [Google Scholar]
- 2.Mahnken AH, Spuentrup E, Niethammer M, Buecker A, Boese J, Wildberger JE, et al. Quantitative and qualitative assessment of left ventricular volume with ECG-gated multislice spiral CT: value of different image reconstruction algorithms in comparison to MRI. Acta Radiol. 2003;44:604–611. doi: 10.1080/02841850312331287799. [DOI] [PubMed] [Google Scholar]
- 3.Mahnken AH, Koos R, Katoh M, Spuentrup E, Busch P, Wildberger JE, et al. Sixteen-slice spiral CT versus MR imaging for the assessment of left ventricular function in acute myocardial infarction. Eur Radiol. 2005;15:714–720. doi: 10.1007/s00330-004-2592-x. [DOI] [PubMed] [Google Scholar]
- 4.Dewey M, Muller M, Teige F, Hamm B. Evaluation of a semiautomatic software tool for left ventricular function analysis with 16-slice computed tomography. Eur Radiol. 2006;16:25–31. doi: 10.1007/s00330-005-2817-7. [DOI] [PubMed] [Google Scholar]
- 5.White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987;76:44–51. doi: 10.1161/01.cir.76.1.44. [DOI] [PubMed] [Google Scholar]
- 6.Abada HT, Larchez C, Daoud B, Sigal-Cinqualbre A, Paul JF. MDCT of the coronary arteries: feasibility of low-dose CT with ECG-pulsed tube current modulation to reduce radiation dose. AJR Am J Roentgenol. 2006;186:S387–S390. doi: 10.2214/AJR.05.0216. [DOI] [PubMed] [Google Scholar]
- 7.Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D. Step-and-shoot data acquisition and reconstruction for cardiac X-ray computed tomography. Med Phys. 2006;33:4236–4248. doi: 10.1118/1.2361078. [DOI] [PubMed] [Google Scholar]
- 8.Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002;12:1081–1086. doi: 10.1007/s00330-001-1278-x. [DOI] [PubMed] [Google Scholar]
- 9.Petersilka M, Bruder H, Krauss B, Stierstorfer K, Flohr TG. Technical principles of dual source CT. Eur J Radiol. 2008;68:362–368. doi: 10.1016/j.ejrad.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. American Society of Echocardiography Committee on Standards; Subcommittee on Quantitation of Two-Dimensional Echocardiograms. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr. 1989;2:358–336. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 11.Christner JA, Kofler JM, McCollough CH. Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 2010;194:881–889. doi: 10.2214/AJR.09.3462. [DOI] [PubMed] [Google Scholar]
- 12.Raff GL, Gallagher MJ, O'Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–557. doi: 10.1016/j.jacc.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann U, Moselewski F, Cury RC, Ferencik M, Jang IK, Diaz LJ, et al. Predictive value of 16-slice multidetector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease: patient-versus segment-based analysis. Circulation. 2004;110:2638–2643. doi: 10.1161/01.CIR.0000145614.07427.9F. [DOI] [PubMed] [Google Scholar]
- 14.Butler J, Shapiro MD, Jassal DS, Neilan TG, Nichols J, Ferencik M, et al. Comparison of multidetector computed tomography and two-dimensional transthoracic echocardiography for left ventricular assessment in patients with heart failure. Am J Cardiol. 2007;99:247–249. doi: 10.1016/j.amjcard.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 15.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 16.de Graaf FR, Schuijf JD, van Velzen JE, Nucifora G, Kroft LJ, de Roos A, et al. Assessment of global left ventricular function and volumes with 320-row multidetector computed tomography: a comparison with 2D-echocardiography. J Nucl Cardiol. 2010;17:225–231. doi: 10.1007/s12350-009-9173-y. [DOI] [PMC free article] [PubMed] [Google Scholar]