Endoscopy is not a new concept to medicine. It is, however, relatively new to the field of craniomaxillofacial surgery. The first endoscope was introduced in 1805 and was used to visualize the bladder.1 Use of endoscopes was such a help to diagnosis and treatment that very quickly additional scopes were developed and used to visualize the cervix and the larynx. These scopes, however, were limited because light sources were poor and often internal. They produced a great deal of heat and could burn the tissues surveyed. It wasn't until Harold Hopkins developed the glass rod endoscope in 1966 (which bears his name) that the modern era of bright, cold light began.2 The “Hopkins rod” replaced the thin, fragile rod with glass ends with a more durable glass tube that had intervening air spaces. The newer design provided a clearer, brighter view and was more durable than the previous endoscopes.
Although gynecologists, orthopedists, and other surgeons quickly adapted to these devices and used them in every real and virtual space in the body, maxillofacial surgeons rarely used them. There are no preformed cavities in the head and neck, other than the inside of the sinuses and pharynx, which are mainly the concern of the otolaryngologist. It was not until the 1990s that endoscopic sinus surgery techniques entered maxillofacial surgery. The techniques used were modifications (1) of plastic surgery techniques for brow lifting and (2) of otolaryngology techniques for sinus surgery. The instrumentation is virtually identical. These techniques were first used for endoscopic subcondylar repair3 and are now also used for transantral orbital floor reconstruction, zygomatic arch, and frontal sinus repair. Subcondylar fractures are difficult to treat openly in even the best of circumstances, and seeing and treating the condyle in its native position has numerous advantages. Once this use became more common, other facial fractures began to be examined from an endoscopic perspective.
Fractures of the frontal sinus and orbit are relatively common in facial trauma patients (5 to 15% of all maxillofacial trauma).4 Although a significant percentage of these fractures can be managed nonoperatively, operative intervention is often required to avoid late complications. Some of the more typical complications of orbital fractures are diplopia from muscle entrapment, visual loss, and enophthalmos from volume expansion into the surrounding sinus leading to pseudoptosis. The typical complications from frontal sinus injuries are much less common but much more significant when encountered. These include frontal contour irregularities, spinal fluid leak (possibly resulting in meningitis), ocular complications including vision loss and blindness, and the late complication of mucocele.
Surgeons in general weigh the risk of an operation and its approach against the benefits of preventing complications, and recommend surgery based on this analysis. In general, if a procedure has a lower risk of complications, it is more widely applied. Endoscopic techniques may provide lower rates of complications and higher acceptance rates in patients, and, therefore, they may be more widely employed. Because these techniques are very detailed and have a steep “learning curve,” surgeons should be patient in their evaluation and use.
The risks of the surgical access approach for orbital procedures can infrequently be more significant than the complications of the fracture. Any transcutaneous approach can result in poor scaring that leads to ectropion and to poor lower lid position.5 In its most serious form, the poor lid position could cause dry eye, tearing, corneal ulceration, and corneal scarring with resulting loss of vision. Lid malposition occurs in 5 to 10% of postoperative patients.6 This may result in a poorer outcome than if the surgeon had just left the fracture alone. For this reason, approaches that avoid skin incisions have been devised. Transconjunctival incisions have the advantage of greatly limiting ectropion. They do, however, require that most of the postinjury swelling has disappeared. These approaches can cause muscle injury or entropion—a difficult complication to manage. These complications are much less frequent than the complications of the transcutaneous approach, but much more significant. A prominent oculoplastic surgeon has led me to believe that entropion is one of the most difficult situations to correct in lid surgery (N. Illiff, M.D., Johns Hopkins Hospital, personal communication).
The risks of the approach in frontal sinus surgery are less significant than those that may occur in lower eyelid surgery, and most patients with frontal sinus injuries are operated on to prevent contour irregularities and to eliminate sinus outflow tract obstruction. However, the price these patients pay in the location and appearance of the incision line is great. There is also a small, but present risk to the frontal branch of the facial nerve.4 Patients that present with thinning hair or who keep their hair very short or shaved often would accept a small depression in the lower forehead over a 10-inch coronal scar across the top of the head. As surgeons, we must always be aware of the “fourth dimension” of surgery and realize that some patients who undergo coronal incisions at a young age will come to lose their hair later in life. For this reason, every surgeon should try to shorten or minimize surgical scars. Unicoronal incisions give poor exposure and frequently have to be extended toward the upper forehead to provide exposure of the relevant anatomy. Addition of the stealth incision (zigzag) actually increases the length of scar and can camouflage the scar if, and only if, the patient has hair.7 Extension of the coronal scar behind the ear is an excellent way to prevent the visible scar on the face. Rarely does one need this for non–skull base exposures. The final way to limit the scar is the use of the endoscope to aid in visualization. This is technology that has been used for years in the treatment of the upper third aging face. This essentially decreases the need for incisions to two or three 1-inch incisions, limiting the scar by 70 to 80%. The downside is that in most cases a small counter incision at the brow level is needed to manipulate the fracture and place the plates and screws. These are acceptable scars and heal with minimal scarring. The approval by the U.S. Food and Drug Administration (FDA) of a right-angled drill and screwdriver by Synthes (Brandywine, PA) may make the counter incision unnecessary in some cases.
This article reviews the current literature and provides an outline for the management we are currently using at the Johns Hopkins Hospital for application of these techniques in our management of these patients. These techniques don't eliminate current standard approaches, but they extend the ability of the surgeon to offer minimal morbidity with maximal outcome. These techniques are typically employed in patients with fractures that are either limited or would not have previously been repaired—in the case of the frontal sinus fracture—due to patient nonacceptance of the coronal incision, or would not have been repaired due to the limited nature of the orbital floor fractures and increased morbidity of lid incisions.
STATE OF THE ART
It is the nature of surgery to go through patterns of change. Initially, treatment of facial fractures involved minimal exposure and closed reduction techniques because the fractures were not treated early and techniques for internal fixations weren't present. Results, particularly in the upper face, were dismal at best. In fact, before Tessier's work it was thought that enophthalmos was untreatable.8 It was only after his conversations with Converse and others that any attempt at treatment was undertaken. These initial treatments were all done with autologous bone grafts, and, although this is an excellent way to treat these fractures, it does require a coronal or lid incision, which can be undesirable. For this reason, more and more prosthetics are used to repair the orbital floor. Also, as treatment, diagnosis, and outcomes improved, so did the timing of early intervention before wound contracture.
The idea of transantral surgery for orbital floor fractures is not new. It was initially reported in 1972 and involved treatment via an open incision, large antrostomy, and finger reduction of the orbital contents.9 The area was then supported with packing that was removed weeks later. This allowed scar tissue formation and fixation of the floor. Articles continued to be published throughout the 1970s that even recommended doing the procedure blindly with a Foley catheter. Both manual and Foley catheter reductions of the orbital content could potentially and unknowingly move shards of the orbital floor into the orbital soft tissue or periorbital musculature. This could lead to blindness or fibrosis of the muscle, causing permanent diplopia. For this reason, such techniques were largely abandoned for the transcutaneous placement of orbital floor plates in the 1980s.
In the 1990s endoscopic sinus surgery became popular, and direct, close-up evaluation of sinus structures became widespread. For this reason, Strong and others advocated the re-emergence of transantral treatment of the orbital floor fracture.10 This technique was initially accepted with great reverence, but its widespread use never took off, likely because of the limited experience that other specialties had with endoscopic instrumentation in the head and neck. Ear, nose, and throat specialists used the device for sinus surgery, and plastic surgeons were beginning to use the device for forehead lift and for endoscopic nerve harvest, and oral and maxillofacial surgeons rarely used endoscopes. Ophthalmologists also rarely used scopes. For this reason, the initial enthusiasm waned. Now that more and more experience has been obtained with scopes, this method has returned as an important method for repair of the small fracture in patients who have no other fractures.
Patients who have minimally displaced frontal sinus fractures are excellent candidates for the endoscopic techniques.11 These are especially good in a patient who has a receding hairline or a family history of balding. These patients are wary of receiving coronal incisions no matter how skillfully these incisions are closed and repaired. These incisions can be minimized to a great degree by treating the patient with two or three endoscopic ports, which can be less than 3 cm each. This provides visualization and access for the patient, and a small counter incision in the brow can provide access to place the screws. The latter incision is often inconspicuous. These patients are also good candidates for scalp advancement, and, if symmetric incisions are made, this can be done at the same time.
ANATOMY AND EMBRYOLOGY
The orbit is a complex relation of seven bones. It essentially is the fusion of all portions of the midface. Textbooks have been dedicated to periorbital surgery and anatomy, so any description here is only superficial. The most important concept in an orbital fracture is that most fractures are inferior wall or medial wall fractures. These are both easily accessible via transantral or transnasal approaches, and neither requires any skin incisions. This anatomy is essentially that of an optic cavity waiting to be accessed for repair of these fractures.
The frontal sinus is the next to last sinus to fully aerate. The frontal sinuses develop from an outpouching of the anterior ethmoid group of cells, which expands slowly into the frontal bone, with the final size occurring at approximately age 18 years. The size, however, is quite variable and as many as 15% of people will have only a single frontal sinus. The average frontal sinus measures 28 mm in height, 27 mm in width, and 17 mm in depth. Asymmetry between the right and left sides of the frontal sinus is extremely common.4 The shape of the sinus is approximately triangular, and most of the floor is the roof of the orbit, except for the medial part, which overlies the fovea ethmoidalis. The anterior wall of the sinus is thicker and stronger than the posterior wall. Frontal sinus anatomy is, like all sinus anatomy, variable and the sinus is surrounded by structures that have poor tolerance for insult. They are absent in 5% of the population. The amount of aeration is so highly variable that a person may have a 1.5-cm gap between the two tables or as little as a few millimeters. The nasofrontal ducts are present in ∼10% of people, with the rest of us having a recess that clearly drains into the middle meatus.12
FRACTURES
Orbital fractures are common and typically occur as blowout fractures. Blowout fractures are fractures that result in trauma directly over the orbital rim. These fractures are not associated with the typical zygomaticomaxillary complex fractures. The second type of fracture commonly treated via an endoscope is the frontal sinus fracture. If the fracture is a simple type that places a small depression on the forehead, it is very amenable to endoscopic techniques.
Frontal sinus fractures essentially come in four types. The first type is anterior table only, which is perfect for endoscopic technique because these fractures are the easiest to treat and the most conspicuous. The fragments must be evaluated with anatomic precision. The bony fragments may be reduced in situ or, more likely, removed, plated, and replaced either through a scalp or a brow incision. The second most common fracture affects the anterior and posterior tables. Because a large amount of energy is required to cause this type of fracture, patients are often comatose or require c-spine precautions and wound care until open reduction and internal fixation (ORIF) and intermaxillary fixation (IMF) can be done. These fractures are often associated with spinal fluid leak and need not only facial and sinus surgery, but also dural repairs and brain surgery. Patients often require cranialization of the sinus and cannot be treated with endoscopic techniques. The third type of fracture is the posterior table itself. These fractures are rare, but when they occur they require a craniotomy for repair. The fourth and final type of fracture is one that disrupts the ducts. If the duct is damaged, the patient would benefit from some procedure to defunctionalize the sinus. This could be cranialization (if a craniotomy is required) or obliterations with bone or fat.
TECHNIQUE
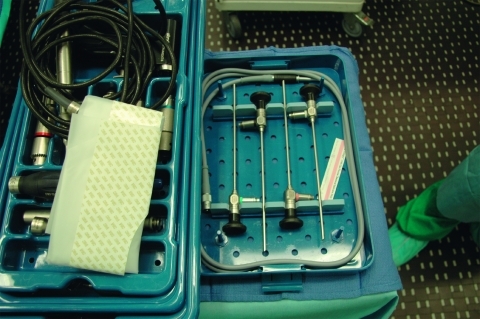
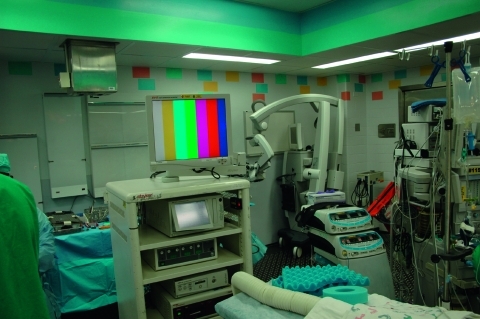
The techniques for endoscopic surgery are the same as for any open procedure, and the instrumentation for endoscopic techniques are frequently similar to open instruments. The main additions are the endoscopes, tower, camera and video monitors. The scopes today are typically Hopkins rods and come in different sizes (2.7 to 4 mm for head and neck purposes) and different angulations (0, 30, 45, and 70 degrees). The diameter of the glass rode can have a profound affect on the amount of light and visualization provided. The angle can also affect visualization. The camera is an industrial quality, 3-chip CCD (charge-coupled device), which is the type used for recording movie-quality videos. It is attached directly to the Hopkins rod and transmits the video signal to a tower. The tower has the printer, video equipment, light source, and monitor necessary to show the image to the surgeon. Figs. 1–3 show the typical instrumentation needed for any endoscopic case.
Figure 1.
Photo of 4-mm endoscopes.
Figure 2.
Tower setup.
Figure 3.
Camera and light cord.
For endoscopic orbital cases, the patient is intubated and the head of the bed turned so the surgeon is on the patient's right side. The video monitors are placed at the patient's head for transantral orbital surgery and at the feet for endoscopic frontal sinus surgery. The gingivobuccal sulcus is then injected with local anesthetic containing 1:100,000 epinephrine. This requires ∼10 minutes to be maximally effective. Once the vasoconstriction is complete, a sulcus incision is made. The maxilla is stripped of periostium. Before beginning, we bend a plate for the end of the procedure. Then a 2-cm wide by 1-cm long Caldwell-Luc antrostomy is performed. We usually leave the bone as an osteoplastic flap for closure. Once the antrostomy is made, the intrasinus contents are cleared and decongested. After this is achieved, the nasal cavity is inspected. The roof of the sinus can now be visualized. If the patient has a trapdoor type fracture, the mucosal flaps can be raised and the bony fracture carefully opened so that the entrapped content can be replaced into the orbit. If the patient has a full-size defect, the opening should be inspected to ensure that none of the fragments are present within the orbital fat or in the inferior rectus muscle. Also of importance is the infraorbital nerve. It is extraorbital until the fissure is identified, and then it becomes intraorbital. Care should be taken not to entrap this structure by the plating system. Figs. 4–6 show an antrum and the fracture in the floor.
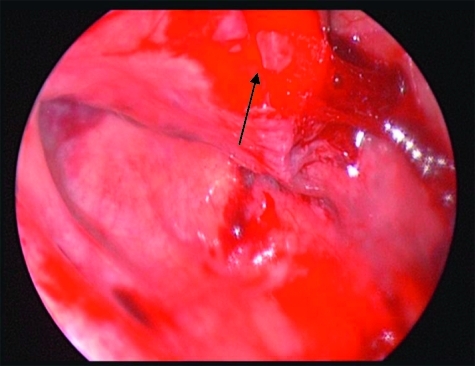
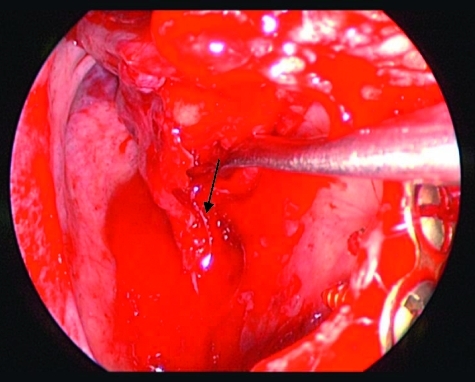
Figure 4.
Left orbit mucosal tear with inferiorly displaced medial segment (arrow).
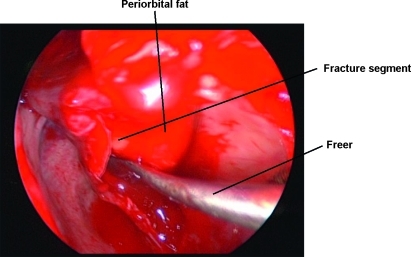
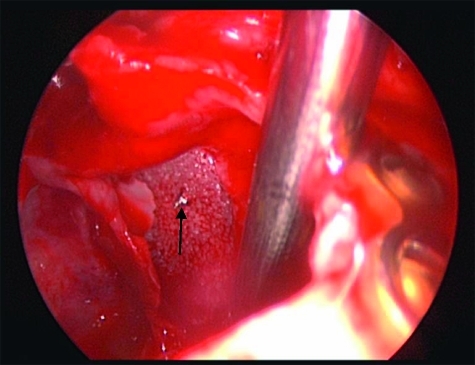
Figure 5.
Freeing up the periorbita and outlining the fracture.
Figure 6.
Identifying the infraorbital nerve (arrow) with a freer.
Once the antrostomy is performed and the defect visualized, the scope is usually changed to a 30-degree scope and work on the fracture begins. The periorbita is left intact, the bone is stripped down, and the stable ledges are identified. The infraorbital nerve can also be identified.
The defect size can be measured with a cut piece of ruler from a marking pen. We usually cut the Medpor ∼4 mm wider than the defect and a few millimeters shorter from front to back, and also cut a small notch for the nerve anteriorly (Fig. 7). We often put a screw through the Medpor to provide a handle. This is then inserted laterally and advanced and slipped over the edge medially. The eye is then checked for muscle entrapment and carefully balloted to ensure that the herniation of fat has been controlled. The sinus should be completely emptied of clot, bone fragments, and irrigated clean, and the Caldwell-Luc antrostomy closed. Initially, we taped the eye shut and placed a nasal trumpet; however, in the last few patients we have abandoned the taping and instructed the patients not to blow their nose, but rather gently suction the mucus back and spit it out of the mouth.
Figure 7.
Medpor with the screw placed as a handle (arrow). Medpor in place to hold periorbital fat above the floor defect.
Medial orbital fractures are treated similarly to floor fractures except that these require more extensive knowledge of intranasal anatomy. To undertake the endoscopic repair, you must be aware of endoscopic skull base anatomy and be comfortable taking or medializing the middle turbinate and taking the uncinate process and ethmoid bulla down (Fig. 8). If you can do this, you can have a full view of the lamina papyracea (Fig. 9). Once the lamina is identified, you can ballot and find the defect. This is then most easily repaired with a Silastic sheet of sufficient stiffness to prevent herniation of the orbital contents. A thin Medpor sheet may also be used (Fig. 10).
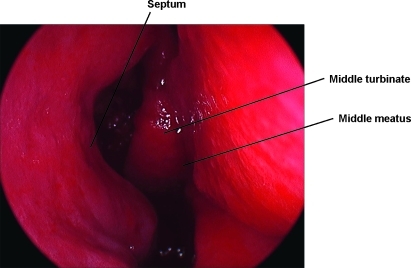
Figure 8.
Medial wall fractures are essentially an extended ethmoidectomy and placement of a Silastic sheet. This is a view of the septum to the left, inferior turbinate takeoff below, and the middle turbinate to the middle of the screen.
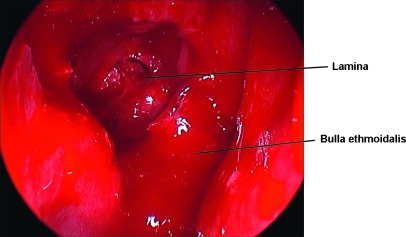
Figure 9.
Uncinate to the left upfront, bulla taken down, and the anterior ethmoid exposed.
Figure 10.
Medpor plate in place.
The endoscopic technique for frontal bone fracture repair is essentially the same as an open ORIF of the anterior table. Essentially, no posterior table, duct work or cranialization can be done through endoscopic techniques alone. The approach is very similar to the endoscopic brow lift. Two or three longitudinal incisions are planned and injected with epinephrine-containing solution. After adequate time for hemostasis, the incision is made through the galea and the periosteum is identified. The entire procedure in our hands is done subperiosteally. This makes protection of the frontal branch of the facial nerve completely safe. A great deal of the dissection can be done without scopes at all. Only the portion of the dissection around the lower forehead frontal nerves and the fractures themselves requires the endoscope. As the area of fracture is approached, the dissection is performed more slowly and more deliberately because these areas are often blood stained and many times anatomic planes are more difficult to define.
The fragments are then carefully elevated and reduced. To do this, the fragment reduction must be relatively straight forward. We usually limit the amount of fragmentation to three or fewer larger fragments for endoscopic approaches. A small counter incision is made in the brow or Lynch region, and the fragments are stabilized with a 1.0- or 1.3-mm plating system.
Once the fragments are reduced and plated, the brow incision is closed in layers and the endoscopic ports are closed. We usually put a single suction drain in the forehead to minimize bruising and fluid accumulation and hasten recovery. Then a light absorbent dressing is applied. The patient is kept overnight to observe visual acuity and discharged home the next day.
DISCUSSION
The use of endoscopes has become one of many standard methods for treatment of fractures within the head and neck. As the boundaries of endoscopic surgery reach further and further, patients will receive the benefits of shorter incisions, less pain, and earlier recovery. And, as the surgeons become more and more facile with the instruments, more indications for this type of repair are justified, and more patients ultimately benefit from less invasive surgery.
Traditional lid incisions may lead to rates as high as 5 to 10% of lid malposition, which is quite high, considering that the fractures in themselves have a very low rate of complications. Initial reports on transantral approaches were met with some skepticism, but new endoscopic techniques are much easier to perform and interest in this technique has re-emerged. The main advantages of these endoscopic techniques for the orbital fractures are: no skin incisions, easy visualization of the defect, and direct view of the posterior ledge.
Medial wall fractures involve a direct approach that is easy for the skilled otolaryngologist to understand. Most plastic surgeons will find it difficult to understand the anatomy of this area, but if the area is approached and the ethmoid cells opened cleanly, the fracture is easily seen and repaired.
The frontal sinus is the last frontier for the head and neck endoscopist. Isolated anterior table fractures are the most suitable for the endoscopic approach. These areas can be overlaid, or by reduction and fixation of the fracture, these depressed fractures can be treated to prevent or repair the depressed forehead. This approach is borrowed from the endoscopic brow lift, and the technique is easily understood and taught to younger residents and fellows. These techniques significantly reduce scarring, limit swelling, and allow quicker recovery.
References
- Linder T E, Simmen D, Stool S E. Revolutionary inventions in the 20th century: the history of endoscopy. Arch Otolaryngol Head Neck Surg. 1997;123:1161–1163. doi: 10.1001/archotol.1997.01900110011001. [DOI] [PubMed] [Google Scholar]
- Eaves F F, III, Price C. Equipment and instrumentation. In: In: Bostwick J III, Eaves FF III, Nahai F, editor. Endoscopic Plastic Surgery. Vol. 23 St. Louis: Quality Medical Publishing; 1995. [Google Scholar]
- Lee C, Mueller R V, Lee K, Mathes S J. Endoscopic subcondylar fracture repair: functional, aesthetic, and radiographic outcomes. Plast Reconstr Surg. 1998;102(5):1434–1443. discussion 1444–1445. doi: 10.1097/00006534-199810000-00016. [DOI] [PubMed] [Google Scholar]
- Manolidis S, Hollier L H., Jr Management of frontal sinus fractures. Plast Reconstr Surg. 2007;120(suppl 2):32S–48S. doi: 10.1097/01.prs.0000260732.58496.1b. [DOI] [PubMed] [Google Scholar]
- Mackenzie D J, Arora B, Hansen J. Orbital floor repair with titanium mesh screen. J Craniomaxillofac Trauma. 1999;5(3):9–16. discussion 17–18. [PubMed] [Google Scholar]
- Zingg M, Chowdhury K, Lädrach K, Vuillemin T, Sutter F, Raveh J. Treatment of 813 zygoma-lateral orbital complex fractures. New aspects. Arch Otolaryngol Head Neck Surg. 1991;117(6):611–629. doi: 10.1001/archotol.1991.01870180047010. [DOI] [PubMed] [Google Scholar]
- Munro I R, Fearon J A. The coronal incision revisited. Plast Reconstr Surg. 1994;93:185–187. doi: 10.1097/00006534-199401000-00031. [DOI] [PubMed] [Google Scholar]
- Wolfe S A. The influence of Paul Tessier on our current treatment of facial trauma, both in primary care and in the management of late sequelae. Clin Plast Surg. 1997;24:515–518. [PubMed] [Google Scholar]
- Walter W L. Early surgical repair of blowout fracture of the orbital floor by using the transantral approach. South Med J. 1972;65(10):1229–1243. doi: 10.1097/00007611-197210000-00014. [DOI] [PubMed] [Google Scholar]
- Strong E B, Kim K K, Diaz R C. Endoscopic approach to orbital blowout fracture repair. Otolaryngol Head Neck Surg. 2004;131(5):683–695. doi: 10.1016/j.otohns.2004.05.017. [DOI] [PubMed] [Google Scholar]
- Strong E B, Buchalter G M, Moulthrop T H. Endoscopic repair of isolated anterior table frontal sinus fractures. Arch Facial Plast Surg. 2003;5(6):514–521. doi: 10.1001/archfaci.5.6.514. [DOI] [PubMed] [Google Scholar]
- Cummings C W, Schuller D E, Thomas J R, Robbins K T, Harker L A. Otolaryngology: Head and Neck Surgery. Philadelphia: Mosby; 2004.