Abstract
This article is a review of the literature and update for management of medial orbital wall fractures. A retrospective review of the literature was performed via PubMed to review the diagnosis and management of medial wall orbital fractures. Medial wall orbital fractures though commonly accompanying orbital floor fractures can also occur alone. There are two primary theories explaining the pathophysiology of medial wall fractures: the hydraulic theory and buckling theory. Most fractures do not require treatment. “White-eyed” trapdoor fractures necessitate immediate surgery to reduce the risk of muscle fibrosis. Trapdoor fractures are more common in the pediatric population. The vast majority of nondisplaced fractures without entrapment do not require surgery. Evaluating patients with medial wall fractures requires evaluation of muscle motility and relative enophthalmos. Patients with entrapped muscles require immediate treatment to prevent permanent injury to the muscle.
Keywords: Orbital fracture, medial wall, extraocular muscle entrapment, enophthalmos, surgical repair, diplopia
Orbital floor fractures are a common sequela of blunt trauma to the face. Floor fractures may be accompanied by medial orbital wall fractures in 7 to 53% of cases.1,2,3,4 However, isolated fractures of the medial orbital wall are an uncommon occurrence and are oftentimes asymptomatic. Although the indications for management of orbital floor fractures have been extensively discussed,5,6,7,8,9,10,11 isolated medial wall fractures have received less attention in the published literature.
The medial orbital wall differs from the floor in that there are multiple bony septae within the ethmoid sinus that provide reinforcement and support to the thin medial wall. This is felt to decrease the incidence of fracture of the medial wall.12 Similar to the orbital floor, there are two primary theories as to the mechanism of fractures to the medial wall. The “buckling theory” holds that there is transmission of force from an anterior blow that deforms but does not fracture the bony rim, which then causes the thinner medial orbital wall to fracture.13 “The hydraulic theory” maintains that a traumatic impact to the soft tissue of the orbit displaces the tissue into the orbital cavity, resulting in fracture of the orbital bones. Though cadaveric studies have supported the hydraulic theory most recently,2 it is more likely that a combination of these two mechanisms plays a role in the pathophysiology of the fractures depending on the mechanism of the trauma. Medial wall fractures combined with orbital floor fractures have been shown in cadaveric studies to require an increase in energy from 4900 millijoules to 6860 millijoules.14 Additionally, it has been hypothesized that certain ethnic groups such as patients of black descent may be anatomically predisposed toward medial wall fractures.15,16
Often, medial wall fractures are diagnosed as incidental findings on computed tomographic (CT) scans in asymptomatic patients. In addition, unsuspected medial wall fractures may manifest if the patient blows his nose after trauma and develops subcutaneous emphysema. Less common, but of greater concern, are patients who present with abduction or adduction deficit from incarceration of the medial rectus in a medial wall fracture. Although “trapdoor” blowout fractures of the orbital floor commonly present with entrapment and limitation of vertical motility, medial wall fractures less often present with medial rectus incarceration. Unlike orbital floor fractures, where an entrapped inferior rectus is usually manifest by restriction of elevation of the globe, patients with medial rectus entrapment in isolated medial wall fractures are more likely to present with findings consistent with paresis of the entrapped muscle rather than restrictive limitation of excursions. The motility dysfunction caused by an entrapped medial rectus muscle also has been reported to have a delayed onset several days following the initial trauma. This is felt to presumably be due to ischemia of the entrapped muscle with loss of function.17
Medial wall fractures should be suspected in any patient who has suffered blunt periocular trauma. Examination of these patients should include a full ophthalmic exam to rule out associated ocular injuries. Special attention should be paid toward evaluation of horizontal motility and measurement of globe displacement and enophthalmos. Although soft tissue signs of medial wall fracture, including periorbital edema and ecchymosis, subcutaneous emphysema, and epistaxis, may be present,18 many patients with medial wall fractures are asymptomatic, and imaging may pick up the fracture as an incidental finding.
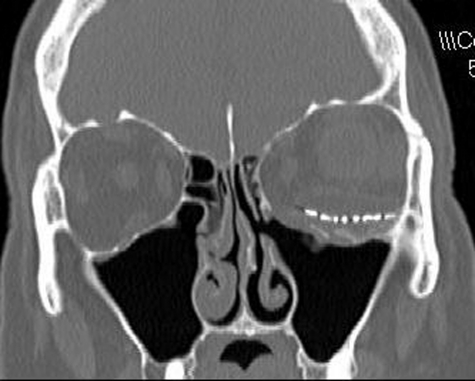
CT scans with coronal and axial views are the imaging modality of choice in suspected orbital fracture cases. On CT scan, subtle medial wall fractures can be detected by comparing the distance from the midline to the medial wall on the injured and uninjured sides. The fractured side will often show a decreased distance in comparison to the unaffected side (Fig. 1). However, CT scan may show minimal displacement of the medial wall if the elastic bone returns back to its original position once the deforming pressure is released and the medial wall defect may “self-seal.” Plain film imaging for medial wall fractures is considered obsolete and can only detect less than 50% of fractures.18
Figure 1.
Computed tomographic scan of a patient who had undergone left orbital floor repair with a previously undiagnosed left medial wall fracture. Note distance from nasal septum to medial orbital wall is much reduced compared with the right side.
“Trapdoor fracture” of the orbital floor is well described. This occurs more commonly in the pediatric population, which tends to have more elastic and thicker bones.8,17,19 Similarly, medial wall orbital fractures with entrapment of extraocular muscle are largely limited to the pediatric population.17 In this situation, the initial blow may cause the orbital contents to be displaced into the sinus through a bone that has partially fractured and formed a hinge. Once the pressure from the blow is released, the bone returns to its original position, trapping the orbital contents in the ethmoid sinus. Patients with orbital floor trapdoor fractures often present with minimal soft tissue signs of trauma, leading Jordan et al to designate them as “white-eyed blowout” fractures.8 We have similarly found that patients with isolated medial wall trapdoor fractures also have minimal ecchymosis or swelling.17 These patients may show limitations of both abduction and adduction.
Patients with medial wall fractures may present with varying motility deficits. Although most patients with isolated medial wall fractures without entrapment are not expected to have motility deficits, patients with incarceration of the medial rectus within the fracture site will experience limitation of movement on horizontal versions. This may present either as a limitation of abduction, adduction, or both. Although one would expect limited abduction due to mechanical restriction of the entrapped medial rectus muscle to dominate, surprisingly, this is less common than paretic limitation of adduction of the affected eye.17 The variable degree of abduction limitation probably reflects the variable amount of “slack” medial rectus anterior to the site of entrapment. If there is a surplus of muscle length present anterior to the entrapment site, then there will be little or no restriction of abduction. If there is little excessively “slack” muscle present anterior to the fracture site, then restriction of the abduction will be more prominent. Patients with a tightly entrapped medial rectus in the fracture site can also demonstrate retraction of the palpebral fissure associated with their restricted lateral gaze9 due to the force generated by the lateral rectus muscle tugging against the tightly entrapped medial rectus.
Limitation of adduction may reflect either paresis of the medial rectus muscle or loss of mechanical advantage to generate force to adduct the globe. Often, the adduction deficit reflects a combination of anterior displacement of the effective point of origin from the orbital apex up to the fracture site, in combination with paresis due to ischemia and/or neuropraxia of the entrapped and ischemic medial rectus muscle.17 This may occur due to a relative “compartment syndrome” caused by tight incarceration of the muscle within the fracture sight.10 This may have delayed onset and progress over time as progressive ischemia develops.17
The pattern of motility dysfunction in patients with incarcerated medial wall fractures likely depends on the location of the entrapment along the medial wall and the relative laxity of muscle anterior to this point. More anterior fractures will have an effective anterior origin of the muscle, which will limit adduction. In addition, greater laxity of the medial rectus anterior to the entrapment will also minimize adduction due to a reduced force vector generated by contracture. The amount of laxity also will affect the abduction deficit. Patients with minimal laxity anterior to the fracture will show mechanical restriction of abduction, and patients with relative laxity of the medial rectus may retain normal adduction17 (Fig. 2).
Figure 2.
Diagram showing (A) anterior entrapment of the taut medial rectus muscle resulting in (B) limited abduction. (C) Entrapment with slack of the medial rectus muscle will allow abduction but less effective adduction. (D) No limitation of abduction.
Exophthalmometry is also used to measure relative enophthalmos or exophthalmos in patients with medial wall fractures. Without an exophthalmometer, this can be evaluated by allowing patients to lean their head back and viewing relative globe position from below (Fig. 3). Enophthalmos after orbital fracture can be the result of fat necrosis and atrophy, entrapment of tissues within a fracture causing retention of the globe in a recessed position, cicatricial contracture of tissue, or prolapse of orbital contents.6
Figure 3.
Patient with right-sided enophthalmos, most easily seen with patient leaning his head back.
Enophthalmos is an uncommon sign in patients with isolated medial wall fractures but is twice as common in patients with combined medial wall and floor fractures.18 In the largest series of isolated medial wall fractures, only one patient presented with enophthalmos.17
Entrapment of the inferior rectus has been reported to cause an oculocardiac reflex with globe excursions, and there has been one reported case of a similar bradycardiac response with attempted abduction with isolated medial wall fracture with medial rectus muscle entrapment.17,20 Patients who exhibit an oculocardiac reflex require immediate treatment. The increased vagal tone from soft tissue entrapment results from an altered trigeminal pathway via the reticular formation to the visceral motor nuclei. These patients are at risk for cardiac syncope and necessitate immediate surgery.5
Indications for surgical intervention with medial wall fractures include clinically significant enophthalmos, evidence of entrapment of medial rectus muscle on imaging associated with diplopia, and/or nausea, vomiting, or bradycardia with attempted eye movement. Patients with normal motility regardless of size of fracture may be followed to see if clinically significant enophthalmos develops. If it does, it can be repaired satisfactorily even after prolonged interval after injury.17 It has been our experience that large isolated medial wall fractures rarely lead to clinically significant enophthalmos. With long-term follow-up, these patients do not require any intervention and do well.
Patient with medial rectus entrapment trapdoor fractures need early intervention as there may be reduced blood flow and nerve compression leading to permanent injury to the muscle.8,19 Although traditionally a 2-week observation period was recommended in orbital blowout fractures to allow for posttraumatic edema to resolve, current management favors early intervention when frank extraocular muscle entrapment is present.7,19 In the largest published series of isolated medial wall fractures, early intervention resulted in ultimate resolution of diplopia in all patients with entrapment.17
Our favorite approach is a transcaruncular medial orbitotomy of the medial wall.17 This has replaced the traditional percutaneous frontoethmoidal approach. Others have advocated endoscopic endonasal fracture reduction, but we have no experience with this technique and favor the direct view of the fracture site and intraorbital contents afforded by the transcaruncular approach. In all surgical interventions, repositioning the prolapsed soft tissue into the orbit is a priority. Alloplastic material, if needed, may then be placed along the medial wall to retain the soft tissue in place in the orbit and prevent it from prolapsing back into the ethmoid sinus. Smaller fractures may benefit from release and repositioning of the prolapsed soft tissue and removal of the loose bone without implant placement. In the series presented by Brannan et al, eight of nine patients with medial wall fracture did not have an implant placed with minimal postoperative residual enophthalmos.17 After removal of the medial wall, enophthalmos did not develop in these patients. One patient, who had an implant placed, presented with enophthalmos and had sustained the injury several months prior. Use of autologous bone grafts is feasible but largely obsolete secondary to the development of excellent alloplastic materials. Endoscopic nasal approaches may also involve the placement of a temporary balloon to maintain the alloplastic graft in place.21 Surgical intervention is not without the complications of vision loss, worsening diplopia, and infection of implant material or implant migration.5
In summary, medial wall fractures can provide a diagnostic and management challenge to surgeons. Ocular motility and relative enophthalmos are critical components of the workup of these patients. The vast majority of nondisplaced fractures without entrapment do not require surgery. Of note, “trapdoor” fractures are much more likely to require early intervention to prevent permanent injury to the muscle. Once released, muscle function and resulting diplopia are expected to improve over time.
References
- Dodick J M, Galin M A, Littleton J T, Sod L M. Concomitant medial wall fracture and blowout fracture of the orbit. Arch Ophthalmol. 1971;85:273–276. doi: 10.1001/archopht.1971.00990050275003. [DOI] [PubMed] [Google Scholar]
- Jank S, Schuchter B, Emshoff R, et al. Clinical signs of orbital wall fractures as a function of anatomic location. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:149–153. doi: 10.1016/s1079-2104(03)00317-2. [DOI] [PubMed] [Google Scholar]
- Rauch S D. Medial orbital blow-out fracture with entrapment. Arch Otolaryngol. 1985;111:53–55. doi: 10.1001/archotol.1985.00800030087013. [DOI] [PubMed] [Google Scholar]
- Thering H R, Bogart J N. Blowout fracture of the medial orbital wall, with entrapment of the medial rectus muscle. Plast Reconstr Surg. 1979;63:848–852. [PubMed] [Google Scholar]
- Burnstine M A. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol. 2003;14:236–240. doi: 10.1097/00055735-200310000-00002. [DOI] [PubMed] [Google Scholar]
- Converse J M. On the treatment of blow out fractures of the orbit. Plast Reconstr Surg. 1978;62:100–104. doi: 10.1097/00006534-197807000-00016. [DOI] [PubMed] [Google Scholar]
- Egbert J E, May K, Kerten R C, et al. Pediatric orbital floor fractures: direct extraocular muscle involvement. Ophthalmology. 2000;107:1875–1879. doi: 10.1016/s0161-6420(00)00334-1. [DOI] [PubMed] [Google Scholar]
- Jordan D R, Allen L H, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthal Plast Reconstr Surg. 1998;14:379–390. doi: 10.1097/00002341-199811000-00001. [DOI] [PubMed] [Google Scholar]
- Miller G R, Glaser J S. The retraction syndrome and trauma. Arch Ophthalmol. 1966;76:662–663. doi: 10.1001/archopht.1966.03850010664006. [DOI] [PubMed] [Google Scholar]
- Smith B, Lisman R D, Simonton J, Della Rocca R. Volkmann's contracture of the extraocular muscles following blowout fracture. Plast Reconstr Surg. 1984;74:200–216. doi: 10.1097/00006534-198408000-00004. [DOI] [PubMed] [Google Scholar]
- Smith B, Regan W F., Jr Blow-out fracture of the orbit; mechanism and correction of internal orbital fracture. Am J Ophthalmol. 1957;44:733–739. doi: 10.1016/0002-9394(76)90774-1. [DOI] [PubMed] [Google Scholar]
- Davidson T M, Olesen R M, Nahum A M. Medial orbital wall fracture with rectus entrapment. Arch Otolaryngol. 1975;101:33–35. doi: 10.1001/archotol.1975.00780300037009. [DOI] [PubMed] [Google Scholar]
- Warwar R E, Bullock J D, Ballal D R, Ballal R D. Mechanisms of orbital floor fractures: a clinical, experimental, and theoretical study. Ophthal Plast Reconstr Surg. 2000;16:188–200. doi: 10.1097/00002341-200005000-00005. [DOI] [PubMed] [Google Scholar]
- Rhee J S, Kilde J, Yoganadan N, Pintar F. Orbital blowout fractures: experimental evidence for the pure hydraulic theory. Arch Facial Plast Surg. 2002;4:98–101. doi: 10.1001/archfaci.4.2.98. [DOI] [PubMed] [Google Scholar]
- Gittinger J W, Jr, Hughes J P, Suran E L. Medial orbital wall blow-out fracture producing an acquired retraction syndrome. J Clin Neuroophthalmol. 1986;6:153–156. doi: 10.3109/01658108608997345. [DOI] [PubMed] [Google Scholar]
- Merle H, Gerard M, Raynaud M. Isolated medial orbital blow-out fracture with medial rectus entrapment. Acta Ophthalmol Scand. 1998;76:378–379. doi: 10.1034/j.1600-0420.1998.760328.x. [DOI] [PubMed] [Google Scholar]
- Brannan P A, Kersten R C, Kulwin D R. Isolated medial orbital wall fractures with medial rectus muscle incarceration. Ophthal Plast Reconstr Surg. 2006;22:178–183. doi: 10.1097/01.iop.0000217565.69261.4f. [DOI] [PubMed] [Google Scholar]
- Nolasco F P, Mathog R H. Medial orbital wall fractures: classification and clinical profile. Otolaryngol Head Neck Surg. 1995;112:549–556. doi: 10.1177/019459989511200408. [DOI] [PubMed] [Google Scholar]
- Bansagi Z C, Meyer D R. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology. 2000;107:829–836. doi: 10.1016/s0161-6420(00)00015-4. [DOI] [PubMed] [Google Scholar]
- McCulley T J, Yip C-C, Kersten R C, Kulwin D R. Medial rectus muscle incarceration in pediatric medial orbital wall trapdoor fractures. Eur J Ophthalmol. 2004;14:330–333. doi: 10.1177/112067210401400409. [DOI] [PubMed] [Google Scholar]
- Lee M J, Kang Y S, Yang J Y, Lee D Y, Chung Y Y, Rohrich R J. Endoscopic transnasal approach for the treatment of medial orbital blow-out fracture: a technique for controlling the fractured wall with a balloon catheter and Merocel. Plast Reconstr Surg. 2002;110:417–426. doi: 10.1097/00006534-200208000-00006. [DOI] [PubMed] [Google Scholar]