Abstract
Traumatic superior orbital fissure syndrome is an uncommon complication of craniomaxillofacial trauma with an incidence of less than 1%. The syndrome is characterized by ophthalmoplegia, ptosis, proptosis of eye, dilation and fixation of the pupil, and anesthesia of the upper eyelid and forehead. This article describes a detailed anatomy of the superior orbital fissure as it related to pathophysiology and clinical findings. Etiology and diagnosis are established after detailed physical and radiographic examination. On the basis of our clinical experience in the management of superior orbital fissure syndrome and from the data reported previously in the literature, an algorithm for treatment of traumatic superior orbital fissure syndrome including use of steroid, surgical decompression of superior orbital fissure, and reduction of concomitant facial fracture is presented and its rationale discussed.
Keywords: Superior orbital fissure, optic nerve, orbital apex syndrome, cranial nerve, steroid
The superior orbital fissure syndrome (SOFS) is an uncommon complication after craniofacial trauma. According to Banks,1 Hirschfeld first described a trauma patient with the physical sign of SOFS in 1858. Lakke2 further defined the complete SOFS, which consisted of paresis of the ocular muscle, sensory disturbance in the distribution of the first branch of trigeminal nerve, and retroorbital pain. With better understanding of the characteristics of SOFS, more sporadic cases were reported in the literature.
ANATOMIC CONSIDERATIONS
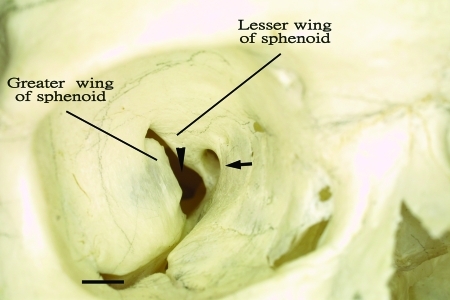
The superior orbital fissure (SOF) is bound laterally by the greater wing of the sphenoid, medially by the lesser wing of sphenoid, and superiorly by the frontal bone (Fig. 1). It lies at the apex of the orbit and at the border between the roof and the lateral orbital wall. SOF serves as a pathway between the orbit and middle cranial fossa. The shape of SOF is like an elongated pear with the broadest part at the nasal side. The long axis extends upward from nasal to lateral at an angle of 45 degrees.2 Detailed anatomic studies of the SOF regarding the contents, size, and the positional relationship with neighboring structures have been reported.3,4 The size of the SOF is around 22 mm in length, 2–3 mm in width in the narrow part, and 7–8 mm in the broader part.2,5 Fujiwara et al further investigated the anatomic width of the SOF using the cadavers and computed tomographic (CT) scan. The width of SOF in the cadavers (3.21 ± 1.09 mm) was similar to that found in the CT scans (3.73 ± 1.64 mm).6 They concluded that narrow SOF (less than 1.6 mm) was a risk factor for SOFS in some anatomic variation.
Figure 1.
Frontal view of right internal orbit indicated optic foramen (arrow), superior orbital fissure (arrowhead), and inferior orbital fissure (line).
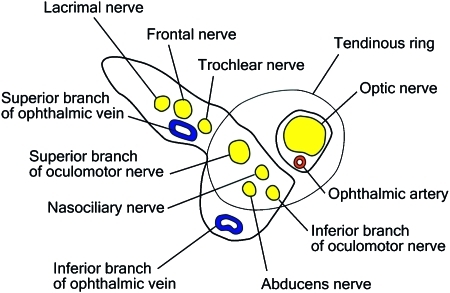
The motor nerves to the eye with the ophthalmic branch of the fifth nerve are grouped together in the wall of the cavernous sinus. This may explain that any pathologic process in the cavernous sinus such as traumatic carotid-cavernous sinus fistula (CCSF) can produce SOFS. The above-mentioned nerves transverse the fissure into the periorbital tissue. The fissure also contains superior and inferior orbital veins, as well as some sympathetic filaments from the cavernous plexus.7 The tendons of the lateral rectus muscle divide the fissure into two parts: the superior part containing trochlear, the frontal, and the lacrimal branches of the ophthalmic division of the trigeminal nerve, and the superior orbital vein; and the inferior part containing the superior and inferior branches of the oculomotor, the abducens, and the nasociliary nerves, and the inferior orbital vein (Fig. 2).5 These structures in the inferior part of SOF are confined within the tendinous ring, which makes the oculomotor, the abducent, and the nasociliary nerves more susceptible to shearing injury during craniofacial trauma. On the contrary, the trochlear nerve passing superiorly above the tendinous ring has anatomically enhanced protection from the traction injury.
Figure 2.
Contents of right superior orbital fissure.
ETIOLOGY
A previous study reported several causal factors, including inflammation, tumors, and trauma apart from unspecific etiology,8 causing SOFS. Inflammation and infection of the central nervous system meninges, cavernous sinus, or retrobulbar space caused by syphilis and tuberculosis have been reported as a cause in the literature.2,9,10 Neoplasms arising from the meninges, bone, and the cerebral tissue near the site of SOF or tumors from remote primary site are capable of producing SOFS.11,12 In addition to medical etiology, craniofacial trauma including skull fracture, zygomaticomaxillary complex, and orbit, and LeFort II and LeFort III fractures account for a major cause of SOFS.1,7,13,14,15,16,17,18,19,20,21,22,23,24,25 In posttraumatic SOFS, the contents of the fissure may be severed or compressed by displaced bone fragments.7,19 However, an increase in the internal orbital pressure caused by edema or bleeding at the moment of trauma may compress the nerves against the bony margin of the fissure. The extent of involvement would depend on the pressure created. Therefore, the recovery also relied on the speed of absorption of the extravasated fluids.7,20 Banks first reported a case of SOFS association with a maxillofacial injury. He proposed that a blow on the skull bone might radiate forward to the roof of the orbit involving the greater wing of the sphenoid and result in hematoma formation around the SOF.1 Aneurysm of the internal carotid artery or CCSF induced by trauma has been reported as another cause in the literature.26,27,28 SOFS may also occur after repair of midfacial fractures in patients with congenitally narrow SOF.6
The incidence of traumatic SOFS is 1 (0.8%) in every 130 cases of facial fractures according to Zachariades. He had encountered 5 cases of SOFS from 452 cases of zygomaticomaxillary complex and 186 diagnosed as LeFort II and LeFort III fractures in a period of 5 years.18 Antonyshyn et al19 reported four cases of traumatic SOFS in a series of 841 complex facial injuries, including 41 blow-in fractures of the orbit. Recently, we retrospectively reviewed 11,284 patients with craniomaxillofacial fractures and identified 33 cases (0.3%) of SOFS. It is reasonably presumed that more impact force close to the orbit during trauma gives rise to a higher incidence of SOFS.
DIAGNOSIS
The clinical symptoms of SOFS can be explained by the nerve involvement on an anatomic basis. External ophthalmoplegia is secondary to impairment of the oculomotor, trochlear, and abducens nerves. Ptosis develops because of lost tension and function of the levator palpebrae superior muscle involving the superior branch of the oculomotor nerve, and loss of tone in Muller's muscle involving the sympathetic fiber arising from the cavernous sinus. Proptosis is caused by a decreased tension of the extraocular muscles, which normally are globe retractors, thereby allowing forward movement of the globe. The fixed dilated pupil with loss of accommodation arises from disruption of the parasympathetic fibers coursing with the oculomotor nerve.17 Compromise of the lacrimal and frontal nerves of the ophthalmic branches of the trigeminal nerve results in anesthesia of the forehead and upper eyelid, lacrimal hyposecretion, and possibly in retro-orbital pain and neuralgia along the path of the nerve.15 Because of the disruption of the sensory nasociliary nerve, there may be anesthesia of the cornea and the bridge of the nose with loss of the corneal reflex.23 When the disruption is partial, the corneal reflex remains intact. If the optic nerve is also involved including the above-mentioned symptoms, it is known as the orbital apex syndrome, a term coined by Kjaer.29
These symptoms are present in various degrees, depending on the severity of the damaged structures and the stage of healing at the time of examining the patient. The term “partial superior orbital fissure syndrome”14,23 indicated partial or complete involvement of the third and sixth cranial nerves along with the nasociliary nerve. These three structures passing inside the tendinous ring are more susceptible to compression injury than other contents of SOFS.
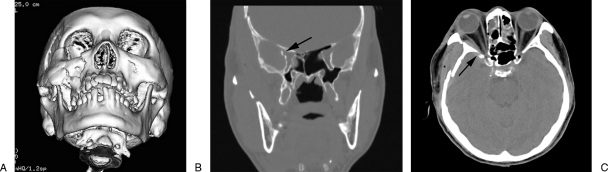
Diagnosis of traumatic SOFS is based on the clinical symptoms, signs mentioned above, and radiographic examination. Optimal plain film viewing of the SOF with a posterior/anterior orbital projection can be obtained in a 20-25 degree tilt of the head (Caldwell projection)23 before CT emerged. However, in severely traumatized patients, plain films are often difficult to obtain and can be hazardous especially when there is a concomitant cervical trauma. Angiography is a useful tool in revealing the traumatic CCSF or carotid aneurysm causing SOFS.28,30 CT scan is an excellent tool for radiologic diagnosis in the traumatized patients. In contrast to plain radiographs, small bony fragments or retroorbital hematoma with compression around SOF can be visualized by fine-cut CT scan (2 mm slices). CT scan demonstrates that fractures in the region of the orbital apex seem to exist more often than thought previously.31 The new spiral CT equipment is a promising tool to improve the diagnostic accuracy, which can provide a detailed information of SOF in the axial plane, coronal projection, and three-dimensional CT reformatted images (Fig. 3). It can help avoid the discomfort of neck hypertension while obtaining the coronal CT slices by the traditional CT machine, and also provide information related to neighboring brain injury and concomitant craniofacial fractures. Nowadays, the technique of measuring the width of SOF using CT scans is simple and compatible to the real width in cadavers.6
Figure 3.
Fractures of right temporal, sphenoid, and zygomatic bone are observed on the computed tomographic (CT) scan. The superior orbital fissure (arrow) becomes narrow and compressed by the sphenoid fracture. (A) Submental view on three-dimensional CT (3D-CT). (B) Coronal plane. (C) Horizontal plane.
TREATMENT
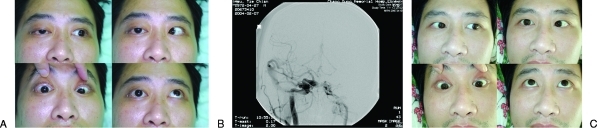
Treatment of the syndrome depends on the cause, if it can be ascertained. Patients present chemosis, pulsating exophthalmos, orbital or frontal bruit, and deterioration of vision in addition to clinical finding compatible with SOFS; traumatic CCSF26,32 should be highly suspected as a cause of SOFS. Prompt carotid angiography is conducted to confirm CCSF, which can be successfully embolized with detachable balloon or coils.32,33 The symptoms of ptosis, facial numbness, and ophthalmoplegia usually resolved progressively within few months after embolization (Fig. 4).
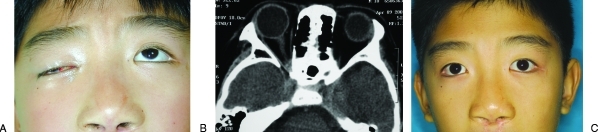
Figure 4.
A 32-year-old male with traumatic superior orbital fissure syndrome (SOFS) caused by carotid-cavernous sinus fistula (CCSF). (A) Patient presented the symptoms of SOFS along with orbit bruit. (B) Anterior-posterior right carotid angiogram showing a large CCSF. (C) One month after embolization, the eye movements are almost back to normal, except the abducens nerve.
Except the etiology of traumatic CCSF, proper management of traumatic SOFS is not clearly defined in the literature because of the relatively small number of reported cases. Treatment varied from conservative treatment to steroid administration, and surgical intervention is reported. Conservative treatment with observation alone has been proposed because complete or partial spontaneous recovery of the motor and sensory functions usually occurs when the syndrome results from trauma.15,17 Moreover, the hazard of further hemorrhage or injury to nerve and operative difficulties are the major drawback of surgical exploration.20 Nineteen previously reported cases of SOFS secondary to craniofacial trauma were treated conservatively (Table 1).1,7,13,14,15,16,17,18,19,20,21,25 Concomitant facial fractures and skull fractures were found in 16 and 7 cases, respectively, and 13 patients received an open reduction of facial fractures. The symptoms of SOFS resolved completely in 8 (42.1%) of the 19 cases.
Table 1.
Superior Orbital Fissure Syndrome—Literature Analysis
| Author | Number of Cases | Complete Recovery | Partial Recovery | Lost to Follow-up | Skull fx | Facial fx | Sphenoid fx | Retrobulbar Hematoma | ORIF of Facial fx | Surgical Decompression | Steroid |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Banks1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Bowerman7 | 2 | 0 | 2 | 0 | 0 | 2 | 1 | 0 | 2 | 0 | 0 |
| Robinson and Jarrett25 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Hedstromet al13 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 |
| Kurzer and Patel14 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Pogrel15 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| Sieverinkand van der Wal16 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 |
| Zachariades17 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 |
| Zachariades et al18 | 4 | 2 | 1 | 1 | 2 | 3 | 1 | 0 | 2 | 0 | 0 |
| Antonyshyn et al19 | 4 | 3 | 1 | 0 | 0 | 4 | 0 | 0 | 4 | 0 | 0 |
| Postma et al28 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 |
| Campiglio et al20 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Llorente Pendás and Albertos Castro21 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 |
| Bun et al23 | 2 | 0 | 2 | 0 | 1 | 2 | 0 | 0 | 2 | 0 | 1 |
| Rohrich et al22 | 2 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 2 | 0 | 2 |
| Giaoui et al34 | 4 | 0 | 4 | 0 | 0 | 3 | 1 | 0 | 3 | 0 | 1 |
| Acartürk et al24 | 5 | 5 | 0 | 0 | 0 | 5 | 0 | 0 | 4 | 0 | 5 |
| 33 | 15 | 16 | 2 | 8 | 29 | 9 | 2 | 24 | 0 | 10 | |
| 45.5% | 48.5% | 6.1% | 24.2% | 87.9% | 27.3% | 6.1% | 72.7% | 0.0% | 30.3% |
fx, fracture; ORIF, open reduction internal fixation.
On the other hand, steroid therapy may be beneficial in patients with SOFS caused by edema from craniofacial fracture.28 Postma et al first reported the short-term use of dexamethasone (4 mg every 6 hours) in patients with traumatic SOFS caused by zygomaticomaxillary complex fracture and sphenoid fracture. This patient was free from neurologic and ocular symptoms at the 3-month follow-up.28 Similar medical treatment with loading dose of 1 mg/kg dexamethasone followed by 0.5 mg/kg every 6 hours was reported by Rohrich et al22 to treat SOFS in addition to the reduction of associated facial fracture. Recently, Acartürk et al24 reported excellent outcome in five patients with traumatic SOFS using megadose steroid of 30 mg/kg methylprednisolone followed by 5.4 mg/kg per hour for 48 hours. All of them recovered completely by 6 months without any complications attributed to high-dose steroid. The literature on steroid treatment of traumatic SOFS is compressively reviewed,22,23,24,28,34 in which 7 (70%) of 10 cases of traumatic SOFS resolved completely after steroid treatment (Table 1). It seems that the patients treated with steroids have a better chance of neurologic recovery than those with observation alone (70% versus 42.1%). Currently, the authors administer megadose steroid with methylprednisolone (30 mg/kg intravenous loading dose followed by 15 mg/kg every 6 hours for 3 days) to help reduce the swelling that may worsen the symptoms of SOFS, if there is no contraindication of using steroid in the injured patients (Fig. 5).
Figure 5.
A 12-year-old boy fell down from a height that resulted in right periorbital trauma and superior orbital fissure syndrome (SOFS). (A) Palpebral ptosis and ophthalmoplegia were present. (B) Computed tomography (CT) showed a retrobulbar hematoma around the orbital apex. (C) View of patient revealing the functional recovery of the right eye 4 months after steroid treatment.
Retroorbital hematoma has been one of the causes of traumatic SOFS. Although some authors suggest aspiration of retrobulbar hematomas associated with fractures, hemorrhage generally resorbs spontaneously within 3 weeks to 4 months.15,18,25 Rohrich et al reported two cases of retrobulbar hematoma with SOFS caused by zygomatico-orbital fractures. Both of them were treated with open reduction of facial fractures and intravenous steroids without specific treatment of retrobulbar hematoma.22 However, hematoma may also organize to form an orbital blood cyst with no endothelial lining. Mortada35 recommended an exploration of the orbital apex that is indicated through a lateral transconjunctival orbitotomy to evacuate the blood if medical treatment is unsuccessful in approximately 4 months.
Surgical intervention may be indicated in the presence of significant narrowing of the SOF from the displaced fracture fragment.28 Murakami36 described four different routes for decompression of the SOFS: (1) the extranasal intraorbital route, for decompression of the lateral wall of the SOF, (2) the modified extranasal intraorbital route with protection of the trochlear nerve, (3) the extranasal transethmoidal route to decompress the medial wall of the SOF, and (4) the transtemporal route, which is indicated in case of fulminating suppuration around the SOFS. When orbital blow-in fracture fragment causes impingement of orbital contents at the SOF, a combination of intracranial and extracranial approach, described by Antonyshyn et al, is adopted for deep orbital decompression to treat SOFS. They reported that three of four patients with traumatic SOFS resolved completely after surgical intervention.19 However, this method did not specifically decompress the SOF. The author's surgical method is direct decompression of the SOF. When the patient has an evidence of significant depressed sphenoid fracture with compression at SOF, the coronal incision is used to approach the SOF. The dissection plane of the anterior scalp is at the subgaleal-supraperiosteal level centrally and at the temporal region just above the plane of the deep temporal fascia. The periosteum is incised at 2 cm above the supraorbital rim and the subperiosteal dissection proceeds until the supraorbital rim, lateral orbital rim, and the zygomatic arch are exposed. The zygoma osteotomy is performed, which mimics zygomatic fracture. If the concomitant zygomatic fracture exists, the zygomatic fracture segment is elevated laterally along its fracture line followed by temporal craniotomy with the assistance of a neurosurgeon. The globe is gently retracted with a malleable retractor to expose the displaced fracture segment of sphenoid bone near the SOF (Fig. 6). The narrow SOF is decompressed by removing the greater wing of the sphenoid bone whereas the temporal lobe is carefully protected. After adequate decompression of SOF is achieved, the bone flap and the zygomatic segment are anatomically placed back and fixed with miniplates. Following this operation, the movement of the eyeball and sensory function usually recover within 3 to 6 months (Fig. 7).
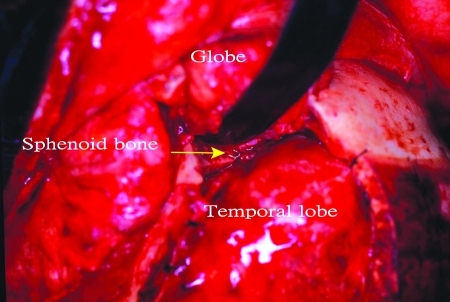
Figure 6.
Intraoperative view of left orbit after a combination of intracranial-extracranial approach. The depressed sphenoid bone is exposed (arrow).
Figure 7.
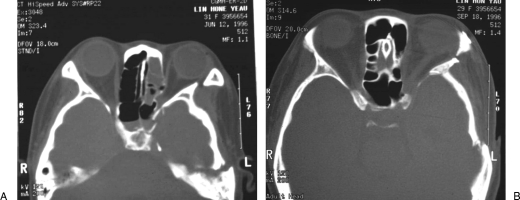
Example of the depressed left sphenoid and temporal bone fractures causing superior orbital fissure syndrome (SOFF). (A) Preoperative axial view of computed tomographic (CT) scan. (B) Postoperative CT scan demonstrating adequate decompression at the superior orbital fissure.
There is a high incidence of associated facial fracture in traumatic SOFS. Although some authors chose no treatment of midface fracture for fear of further worsening cranial nerve palsies from surgical reduction, most authors preferred the surgical intervention of concomitant facial fracture if reduction of the fracture was indicated. Twenty-four (82.7%) of the 29 previously reported cases with traumatic SOFS received surgical treatment of concomitant facial fractures (Table 1). Early reduction of blow-in fractures of the orbit resulting in solution of cranial nerve palsies was suggested by Antonyshyn et al.19 The interval from injury to surgical reduction of facial fractures ranged from 1 to 14 days.7,13,14,16,17,18,22,23 In the author's experience, all patients with associated facial fracture underwent open reduction, on an average of 10 days, after injury. None of them experienced aggravated neurologic signs after surgical repair.
If the patient presents a decreased visual acuity with symptoms of SOFS, orbital apex syndrome should be considered. The treatment of traumatic optic neuropathy (TON) is still controversial with variable therapeutic approaches and different response rates. The details of different therapeutic management of TON are beyond the scope of this report. Our present treatment algorithm for TON is medical treatment first with megadose methylprednisolone as mentioned above. However, surgical decompression of TON using transconjunctival approach will proceed if the patient has the following conditions: (1) CT evidence of impingement of bony fragments to the optic nerve, (2) failure of improvement of vision after 3 days of megadose steroid therapy with visual impairment of finger counting or worse, or (3) progressive visual deterioration during steroid treatment.37 The documented visual improvement after a combination of steroid therapy and surgical decompression varied from 40 to 79%.37,38,39
OUTCOME
In the absence of compression by the fracture fragments, the patient's symptoms typically resolve over an extended period of up to 3 to 4 months.13,17,18,25 The prognosis may not be as good if symptoms are caused by displaced bony fragments.25 However, we observed that our patients with traumatic SOFS caused by displaced sphenoid fracture and subsequent surgical decompression recovered to the similar functional results compared to the patients without sphenoid fracture. In addition, recovery of cranial nerves III, IV, and VI reached a plateau around 6 months after the injury. A review of 17 reports from the literature1,7,13,14,15,16,17,18,19,20,21,22,23,24,25,28,34 including 33 cases of traumatic SOFS showed that 15 (45.5%) patients recovered completely and 16 (48.5%) patients resolved partially, whereas 2 patients were lost to follow-up (Table 1).
CONCLUSION
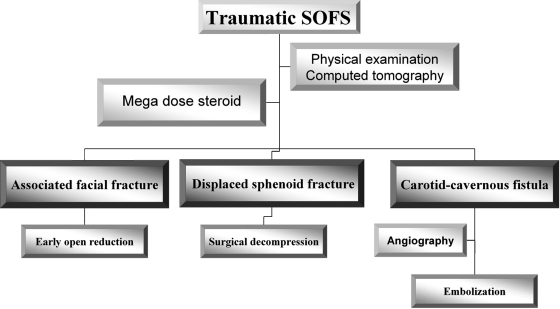
SOFS is a rare complication of craniofacial injury. Diagnosis is based on clinical presentation although it can be delayed by concomitant severe intracranial injury or abdominal injury in unstable patients. Therapeutic plane is initiated after adequate clinical and radiographic examination with fine-cut CT. Megadose steroid is administered if not contraindicated. If the patient is highly suspected with CCSF, angiography is performed to confirm the diagnosis followed by embolization. From the evidence of a displaced sphenoid fracture with impingement at SOF confirmed by CT scan, surgical decompression via a combination of extracranial and intracranial approach is performed. The associated facial fracture, especially orbital blow-in fracture, should be reduced early to relieve intraorbital pressure if the general condition is stable (Fig. 8). Partial to complete recovery of cranial nerve function can be expected after proper treatment.
Figure 8.
Algorithm for management of traumatic superior orbital fissure syndrome.
References
- Banks P. The superior orbital fissure syndrome. Oral Surg Oral Med Oral Pathol. 1967;24:455–458. doi: 10.1016/0030-4220(67)90418-5. [DOI] [PubMed] [Google Scholar]
- Lakke J P. Superior orbital fissure syndrome. Report of a case caused by local pachymeningitis. Arch Neurol. 1962;7:289–300. doi: 10.1001/archneur.1962.04210040041004. [DOI] [PubMed] [Google Scholar]
- Govsa F, Kayalioglu G, Erturk M, Ozgur T. The superior orbital fissure and its contents. Surg Radiol Anat. 1999;21:181–185. doi: 10.1007/BF01630898. [DOI] [PubMed] [Google Scholar]
- Karakaş P, Bozkir M G, Oguz O. Morphometric measurements from various reference points in the orbit of male Caucasians. Surg Radiol Anat. 2003;24:358–362. doi: 10.1007/s00276-002-0071-0. [DOI] [PubMed] [Google Scholar]
- Morard M, Tcherekayev V, de Tribolet N. The superior orbital fissure: a microanatomical study. Neurosurgery. 1994;35:1087–1093. doi: 10.1227/00006123-199412000-00011. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Matsuda K, Kubo T, Tomita K, Yano K, Hosokawa K. Superior orbital fissure syndrome after repair of maxillary and naso-orbito-ethmoid fractures: a case study. J Plast Reconstr Aesthet Surg. 2009;62:e565–e569. doi: 10.1016/j.bjps.2008.11.052. [DOI] [PubMed] [Google Scholar]
- Bowerman J E. The superior orbital fissure syndrome complicating fractures of the facial skeleton. Br J Oral Surg. 1969;7:1–6. doi: 10.1016/s0007-117x(69)80053-3. [DOI] [PubMed] [Google Scholar]
- Mortada A. Superior orbital fissure syndrome of uncertain aetiology: report of ten cases. Br J Ophthalmol. 1961;45:662–671. doi: 10.1136/bjo.45.10.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J N, Coppeto J R, Lessell S. Chronic syphilitic meningitis resulting in superior orbital fissure syndrome and posterior fossa gumma. A report of two cases followed for 20 years. J Clin Neuroophthalmol. 1988;8:145–159. [PubMed] [Google Scholar]
- Clarke H, Clarke V, Gill J, St John A, Lashley M. Painful ophthalmoplegia secondary to a mucocele involving the sella turcica, superior orbital fissure, and sphenoid sinus. J Natl Med Assoc. 1992;84:279–280. [PMC free article] [PubMed] [Google Scholar]
- Hallpike J F. Superior orbital fissure syndrome. Some clinical and radiological observations. J Neurol Neurosurg Psychiatry. 1973;36:486–490. doi: 10.1136/jnnp.36.3.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phanthumchinda K, Hemachuda T. Superior orbital fissure syndrome as a presenting symptom in hepatocellular carcinoma. J Med Assoc Thai. 1991;74:679–682. [PubMed] [Google Scholar]
- Hedstrom J, Parsons J, Maloney P L, Doku H C. Superior orbital fissure syndrome: report of case. J Oral Surg. 1974;32:198–201. [PubMed] [Google Scholar]
- Kurzer A, Patel M P. Superior orbital fissure syndrome associated with fractures of the zygoma and orbit. Plast Reconstr Surg. 1979;64:715–719. [PubMed] [Google Scholar]
- Pogrel M A. The superior orbital fissure syndrome: report of case. J Oral Surg. 1980;38:215–217. [PubMed] [Google Scholar]
- Sieverink N P, van der Wal K G. Superior orbital fissure syndrome in a 7-year-old boy. Int J Oral Surg. 1980;9:216–220. doi: 10.1016/s0300-9785(80)80021-4. [DOI] [PubMed] [Google Scholar]
- Zachariades N. The superior orbital fissure syndrome. Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol. 1982;53:237–240. doi: 10.1016/0030-4220(82)90296-1. [DOI] [PubMed] [Google Scholar]
- Zachariades N, Vairaktaris E, Papavassiliou D, Papademetriou I, Mezitis M, Triantafyllou D. The superior orbital fissure syndrome. J Maxillofac Surg. 1985;13:125–128. doi: 10.1016/s0301-0503(85)80031-x. [DOI] [PubMed] [Google Scholar]
- Antonyshyn O, Gruss J S, Kassel E E. Blow-in fractures of the orbit. Plast Reconstr Surg. 1989;84:10–20. doi: 10.1097/00006534-198907000-00002. [DOI] [PubMed] [Google Scholar]
- Campiglio G L, Signorini M, Candiani P. Superior orbital fissure syndrome complicating zygomatic fractures. Pathogenesis and report of a case. Case report. Scand J Plast Reconstr Surg Hand Surg. 1995;29:69–72. doi: 10.3109/02844319509048427. [DOI] [PubMed] [Google Scholar]
- Llorente Pendás S, Albertos Castro J M. Traumatic superior orbital fissure syndrome: report of case. J Oral Maxillofac Surg. 1995;53:934–936. doi: 10.1016/0278-2391(95)90285-6. [DOI] [PubMed] [Google Scholar]
- Rohrich R J, Hackney F L, Parikh R S. Superior orbital fissure syndrome: current management concepts. J Craniomaxillofac Trauma. 1995;1:44–48. [PubMed] [Google Scholar]
- Bun R J, Vissink A, Bos R R. Traumatic superior orbital fissure syndrome: report of two cases. J Oral Maxillofac Surg. 1996;54:758–761. doi: 10.1016/s0278-2391(96)90698-9. [DOI] [PubMed] [Google Scholar]
- Acartürk S, Seküçoğlu T, Kesiktäs E. Mega dose corticosteroid treatment for traumatic superior orbital fissure and orbital apex syndromes. Ann Plast Surg. 2004;53:60–64. doi: 10.1097/01.sap.0000106424.54415.dc. [DOI] [PubMed] [Google Scholar]
- Robinson D C, Jarrett W J. Superior orbital fissure syndrome with Bell's palsy: report of case. J Oral Surg. 1973;31:203–206. [PubMed] [Google Scholar]
- Zachariades N, Papavassiliou D. Traumatic carotid-cavernous sinus fistula. J Craniomaxillofac Surg. 1988;16:385–388. doi: 10.1016/s1010-5182(88)80086-6. [DOI] [PubMed] [Google Scholar]
- Diaz F G, Ohaegbulam S, Dujovny M, Ausman J I. Surgical alternatives in the treatment of cavernous sinus aneurysms. J Neurosurg. 1989;71:846–853. doi: 10.3171/jns.1989.71.6.0846. [DOI] [PubMed] [Google Scholar]
- Postma M P, Seldomridge G W, Vines F S. Superior orbital fissure syndrome and bilateral internal carotid pseudoaneurysms. J Oral Maxillofac Surg. 1990;48:503–508. doi: 10.1016/0278-2391(90)90241-s. [DOI] [PubMed] [Google Scholar]
- Kjaer I. A case of orbital apex syndrome in collateral pansinusitis. Acta Ophthalmol (Copenh) 1945;23:257. [Google Scholar]
- Lenzi G L, Fieschi C. Superior orbital fissure syndrome. Review of 130 cases. Eur Neurol. 1977;16:23–30. doi: 10.1159/000114876. [DOI] [PubMed] [Google Scholar]
- Unger J M. Orbital apex fractures: the contribution of computed tomography. Radiology. 1984;150:713–717. doi: 10.1148/radiology.150.3.6695072. [DOI] [PubMed] [Google Scholar]
- Paza A O, Farah G J, Passeri L A. Traumatic carotid cavernous fistula associated with a mandibular fracture. Int J Oral Maxillofac Surg. 2008;37:86–89. doi: 10.1016/j.ijom.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Das S, Bendok B R, Novakovic R L, et al. Return of vision after transarterial coiling of a carotid cavernous sinus fistula: case report. Surg Neurol. 2006;66:82–85. discussion 85. doi: 10.1016/j.surneu.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Giaoui L, Lockhart R, Lafitte F, et al. [Traumatic superior orbital fissure syndrome: report of 4 cases and review of literature] J Fr Ophtalmol. 2001;24:295–302. [PubMed] [Google Scholar]
- Mortada A. Unilateral proptosis of unexplained origin and superior orbital fissure syndrome of uncertain aetiology. Bull Ophthalmol Soc Egypt. 1969;62:191–204. [PubMed] [Google Scholar]
- Murakami I. Decompression of the superior orbital fissure. Am J Ophthalmol. 1965;59:803–808. doi: 10.1016/0002-9394(65)93009-6. [DOI] [PubMed] [Google Scholar]
- Chen C T, Huang F, Tsay P K, et al. Endoscopically assisted transconjunctival decompression of traumatic optic neuropathy. J Craniofac Surg. 2007;18:19–26. discussion 27–28. doi: 10.1097/01.scs.0000248654.15287.89. [DOI] [PubMed] [Google Scholar]
- Luxenberger W, Stammberger H, Jebeles J A, Walch C. Endoscopic optic nerve decompression: the Graz experience. Laryngoscope. 1998;108:873–882. doi: 10.1097/00005537-199806000-00016. [DOI] [PubMed] [Google Scholar]
- Levin L A, Joseph M P, Rizzo J F, III, Lessell S. Optic canal decompression in indirect optic nerve trauma. Ophthalmology. 1994;101:566–569. doi: 10.1016/s0161-6420(94)31299-1. [DOI] [PubMed] [Google Scholar]