Abstract
Facial fracture management is often complex and demanding, particularly within the pediatric population. Although facial fractures in this group are uncommon relative to their incidence in adult counterparts, a thorough understanding of issues relevant to pediatric facial fracture management is critical to optimal long-term success. Here, we discuss several issues germane to pediatric facial fractures and review significant factors in their evaluation, diagnosis, and management.
Keywords: Pediatric facial fracture management
The pediatric facial fracture is frequently a daunting injury within a challenging patient population. However, with further advances in imaging modalities, bone fixation technology, microsurgical technique, and distraction osteogenesis, the management of these injuries continues to evolve at a rapid pace. Although a high level of adult supervision, increased flexibility of the facial skeleton, small sinus dimensions, relatively larger fat pads, and unerupted, buttressing teeth may greatly decrease the frequency in which injury translates into fracture, these defects commonly face today's pediatric surgeons. Exemplary management of fractures within this group is directly dependent upon thorough initial evaluation, correct injury assessment, and timely initiation of chosen therapy. Although optimal treatment of these injuries frequently involves a wide array of specialties, plastic surgeons are unique in their management capability. Although fractures to the pediatric facial skeleton are infrequent relative to the incidence of such injuries in adults, a thorough knowledge of their management is critical for optimal outcome. Here, we discuss several issues relevant to pediatric facial fractures and review significant factors in their evaluation, diagnosis, and management.
ISSUES UNIQUE TO PEDIATRIC TRAUMA
Several characteristics of the pediatric patient contribute to higher rates of hypothermia, hypotension, and hypoxia after trauma. Children have a higher surface-to-body volume ratio, metabolic rate, oxygen demand, and cardiac output than do adults. They also have lower total blood volumes than do adults. For these reasons, maintenance of the airway and breathing, control of hemorrhage, and early resuscitation are even more time critical in this population. At birth, the ratio between cranial to facial volume is ~8:1. However, by adulthood, this ratio approximates 2.5:1.3 The retruded position of the face relative to the skull contributes to a lower incidence of midface and mandibular fractures and a higher incidence of cranial injuries in children less than 5 years of age.1,2 With facial growth progression in a downward and forward direction, increased midfacial prominence directly corresponds with an increased rate of injuries to this area and to the mandible.3 Because of a thicker layer of adipose tissue coverage, more elastic bones, and flexible suture lines, facial fractures in children are often minimally displaced. In addition, structural stability is increased by the lack of sinus pneumatization and presence of tooth buds within the jaws.3,4,5 Despite these advantages of pediatric facial structure, potential growth disturbances must be considered when planning treatment, particularly that of nasal septal and condylar injuries.6
EPIDEMIOLOGY OF FACIAL FRACTURES IN CHILDREN
Incidence
Pediatric facial fractures comprise less than 15% of all facial fractures6,7,8 and are rare below age 5 (0.6 to 1.4%).6,7 With increased unsupervised physical activity and involvement in sports, a peak in fracture incidence occurs during puberty and adolescence.6,7,8 Seasonal variations are also evident, with peak frequencies during summer months when outdoor activity is greatest.8
Gender
Male facial fracture patients outnumber their female counterparts in all age groups worldwide.4,8 Although gender differences are less significant and etiologies more similar in both sexes at younger ages, more substantial variations are seen between the sexes during adolescence. These later differences in gender-related fracture incidence are often attributed to more frequent involvement in sports, physical activity, and dangerous behavior among boys.5
Etiology
The majority of facial fractures in children result from falls and sports-related injuries.2,3,4,5 Whereas young children usually sustain injuries from low-velocity forces, such as falls, older children are more commonly exposed to high-velocity forces. In those under 6 years of age, falls at home represent the most common etiology of facial fractures.6,8 With increasing age, facial fractures tend to occur outside the protected area of parental supervision.6 As motor skills improve between the ages of 10 and 14 years, sporting injuries become more prevalent.8,9 Motor vehicle accidents are the leading cause of death in children after the perinatal period9 and remain a common cause of facial fractures in children 6 years of age and above.6,7,9 In contrast with adults, interpersonal violence is an unusual cause of facial fractures in the pediatric population. Though these injuries occur more commonly in adolescents,8 facial fractures occur in 2.3% of child-abuse victims.7 Repeated injuries, multiple injury sites, or questionable circumstances surrounding the injury should raise suspicion of possible abuse.
Injury Site and Pattern
In contrast with more constant patterns of facial fracture observed in adults, the wide variety of pediatric injuries represent a combination of mechanism, force, and anatomic features unique to the child's stage of development. Below age 2, infants more commonly sustain injuries to the frontal region.3,4,8 In addition, this population usually sustains isolated, nondisplaced fractures caused by low-impact/low-velocity forces.7 Older children are more prone to injuries of the chin/lip region.7 Although fractures of the cranial vault are uncommon in pediatrics, the most commonly involved site is the prominent frontal bone.6 Before age 6, the cherry-sized frontal sinus has yet to reach the orbital roof4,5; frontal sinus involvement is generally not seen below this age.6 With pubertal pneumatization of the frontal sinus, the incidence of frontal sinus fractures increases.5 One must be aware that frontal bone fractures are often associated with other facial fractures, as well as significant central nervous system injury.5 As in adults, the nasal bones are the least resistant of the facial skeleton.6 Yet, because a majority of these injuries are treated in an office setting, nasal fractures are not listed among the most common pediatric facial fractures in large, urban-based studies.5,7 When specifically evaluated, nasal fractures constitute nearly 50% of all facial fractures in children.7 Whereas nasal and dentoalveolar fractures are commonly managed in the outpatient setting, mandibular fractures are the most common facial fractures requiring hospitalization.4,8 Presenting as a bilateral injury in 20% of cases, the condylar region is the most frequently fractured site.6 Because of the thin neck and highly vascularized nature of the pediatric condyle, children below 6 years of age more often experience intra- rather than extracapsular condylar fractures. Above this age, condylar fractures more frequently occur in the neck region.5 Whereas body fractures are relatively uncommon in this population, symphyseal and parasymphyseal fractures of the mandible are also typical.4 With the exception of nasal and maxillary alveolar defects, midface fractures are rare in children.2,4 Of these injuries, zygomatic complex fractures are the most frequent.5 Le Fort fractures (at all levels) are almost never seen before age 2. Over age 5, as the maxillary sinuses expand and the permanent teeth erupt, the incidence of midface fractures increases.4 The highest frequency of these injuries within the pediatric population occurs in children 13 to 15 years of age.7 Orbital injuries constitute 20% of pediatric facial fractures.2,5 Most often, these injuries result from transmission of force directly from the orbital ring to the thin orbital walls or indirect, hydraulic pressure effect of displaced orbital soft tissues.3 Prior to frontal sinus development, orbital roof fractures are comparatively more frequent in the very young. However, due to maxillary sinus expansion beyond the equator of the globe, orbital floor fractures are more common in older children.5 The age at which the probability of an orbital floor fracture exceeds that of orbital roof fracture is 7 years.6
DIAGNOSIS OF THE PEDIATRIC FACIAL FRACTURE
Physical Examination
Accurate and prompt diagnosis is critical in the optimal management of pediatric facial fractures. Initial evaluation of potential injuries to the facial skeleton should begin with close physical examination. Children are more difficult to examine than adults, and sedation must be considered if necessary. Orbital examination should include an evaluation of visual acuity, pupil size and response, as well as visual fields, diplopia (double vision), and extraocular muscle function. Subconjunctival hemorrhage and chemosis (bulbar conjunctival swelling) are common in patients with periorbital fractures. Care must be taken not to miss diagnosing hyphema (blood in the anterior chamber of the eye) due to the possible long-term effects on vision. In the presence of any visual defect, consultation with an ophthalmologist is indicated. Palpation of the orbital margins may identify step deformities indicating the point of fracture. Nasal examination should include an assessment of symmetry, dorsal deformity, and intranasal obstruction. In addition, septal hematoma must be ruled out to avoid further structural complication. Enophthalmos or inferior displacement of the globe, or both, can result from orbital floor disruption. The zygoma should be assessed for malar depression, and infraorbital paresthesia may indicate underlying zygomatic fracture. Fractures of the zygomatic arch may result in significant facial asymmetry or trismus as a result of masseter impingement. Examination of the maxilla and mandible should begin with evaluation of dental occlusion. Inspection of the occlusal plane and intraoral soft tissue for the presence of gingival tears or ecchymosis can provide evidence of jaw fractures.
Imaging Evaluation
Modern computed tomography (CT) is the gold standard for viewing craniofacial fractures. CT images provide excellent detail of the cranium, midfacial structures, and the mandibular condyle. In addition to sagittal and coronal views, reformatting images into a three-dimensional reconstruction provides an improved perspective in complex injuries. For imaging the mandible, panoramic radiography is a particularly valuable adjunct to CT. Panorex images frequently provide detailed coverage of dental structures and may occasionally identify angle fractures unapparent on CT views.
PEDIATRIC FACIAL FRACTURE MANAGEMENT
There are several general differences in the approach to the pediatric patient with facial fractures. One is that they tend to be approached more conservatively than are adult injuries for many of the reasons previously discussed. Additionally, fixation is typically accomplished with 1.5- or 2.0-mm plates and monocortical screws. Larger fixation is generally not necessary and may interfere with developing tooth buds. Resorbable fixation is generally not recommended for pediatric trauma. And despite many surgeons' feelings otherwise, there is absolutely no reason to routinely remove fixation in children. Only in situations where the hardware is symptomatic should a second procedure for removal be undertaken. Not infrequently, this can be as difficult as the initial procedure to reduce and fixate the fracture.
Frontal Bone Injury
Until the age of 6, children rarely sustain injury penetrating into the frontal sinus. In addition to the durability of this bone, the infrequency of frontal injury in children is due to the fact that full sinus development does not occur until age 5 or 6. Nondisplaced injuries to the pediatric frontal bone typically do not require operative intervention. However, displaced fractures or fractures prompting suspicion for nasofrontal duct injury should be explored and reduced (Fig. 1). The coronal approach offers wide exposure of the orbital rims, zygomatic arches, and nasal root. Operative reduction is most commonly maintained with microplate fixation, although other techniques, such as drilling/wire fixation, also remain in use. Although the frontal sinus is anatomically negligible until the age of 5, traumatic penetration with severe disruption should prompt sinus destruction. After mucosal ablation, complete destruction of the nasofrontal duct must be ensured.10 As the sinus develops in older children, significant posterior wall involvement requires an interdisciplinary neurosurgical/craniofacial approach.
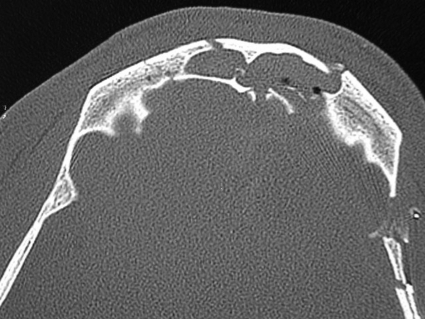
Figure 1.
Although rare in the pediatric population, frontal sinus fractures associated with a displaced posterior table should receive cranialization.
The Orbital Fracture
Operative indications for orbital fractures remain an area of great controversy. However, in cases of suspected traumatic optic neuropathy, surgery must be delayed in lieu of aggressive steroid therapy until vision stabilizes.11,12,13 In the absence of optic nerve compromise, there are several firm indications for surgery in the early postinjury phase. One of these is extraocular muscle entrapment. If left untreated, this may produce ischemia, fibrosis, and, ultimately, motility limitations. Evidence would suggest that results are best if the entrapment is released within 48 hours.12,13,14 The most common indication is typically a large floor defect, defined by many as greater than 1 cm2 (Fig. 2). Defects larger than this are likely to result in enophthalmos if not reconstructed. Additionally, any evidence of enophthalmos developing in the early postinjury period warrants intervention. In the surgical approach to orbital injuries, subciliary incisions are unacceptable as they are plagued by a high rate of lower lid retraction. Transconjunctival incisions with/without lateral canthotomy are preferred. Typically, the most difficult part of the operation is complete exposure. After identification of the fracture's dimension, template creation greatly augments implant formation. Simple and readily available, suture-foil packs or plastic from the saline basin can be easily shaped. Many surgeons prefer autogenous implants over alloplasts when managing the pediatric orbital floor fracture. Classically, bone grafts have been strongly advocated. However, many contemporary alloplastic materials perform superbly as well. Titanium mesh, high-density porous polyethylene implants, and even resorbable sheets have been used with a high degree of success. One material that should be discourage is Silastic (silicone) (Dow Corning Corporation, Midland, MI). Because of resistant bacterial colonization and capsule formation about this material, late infection and extrusion have been frequently described. Once trimmed to an appropriate size, the implant should be placed in the orbital cone completely overlying the defect. Most orbital floor implants do not need fixation as they are adequately stabilized by the overlying periorbita. At this point, the globe's anteroposterior position should be evaluated. With anticipation of eventual edema resolution, the operated eye should project more anterior than does the uninjured eye. If this overprojection is not achieved, it is likely that reconstruction is not anatomic, and enophthalmos should be expected. Finally, a forced duction test should be performed to identify potential extraocular muscle entrapment by the implant.
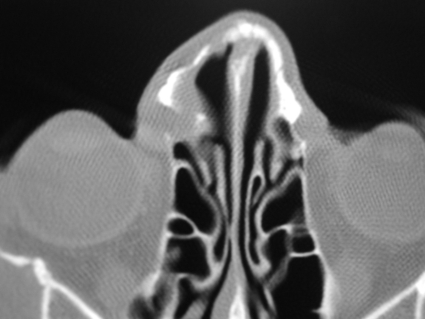
Figure 2.
The most common indication for repair is typically a large floor defect, defined by many as greater than 1 cm2.
Nasal Fracture
The diagnosis of nasal fracture is based on history and physical examination (Fig. 3). Because physical examination may be difficult, crepitation of the resilient bones may be absent, and edema may conceal structural deviation, these fractures can be easily missed in children. As in adults, septal hematoma requires immediate drainage to prevent septal cartilage necrosis, saddle-nose deformity, or potential midface growth retardation. Typically nonemergent, displaced fractures may be reduced acutely or after resolution of edema several days later.15 In a vast majority of cases, anatomic realignment, hemostasis, and fixation are achieved under general anesthesia by closed reduction.15,16
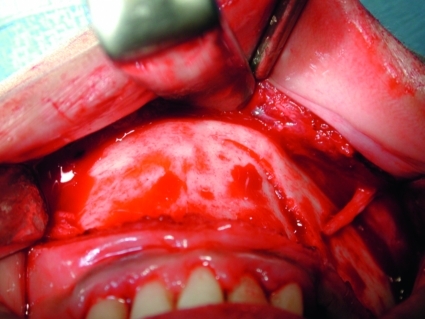
Figure 3.
The nasal fracture may be easily missed because of significant local edema and poor patient compliance during initial examination.
The Zygoma Fracture
Zygomatic fractures without displacement or functional defect, such as diplopia, may be observed.17 However, the comminuted fracture should receive open reduction and internal fixation18 (Fig. 4). The most frequent problems associated with zygomatic complex fractures include facial asymmetry, enophthalmos, and/or paresthesia in the infraorbital nerve (V2) distribution, and orbital floor defects.17,18,19 In the absence of related orbital entrapment, treatment should be performed after resolution of edema around 3 to 5 days. Access to the fracture may be achieved via several incisions; however, the subciliary approach must be avoided to minimize potential ectropion formation. Many surgeons now prefer the transconjunctival approach in lieu of the subciliary approach. A transoral buccal sulcus approach may also be helpful in repositioning the zygomatic buttress. In children, 1-point fixation typically suffices to stabilize the noncomminuted zygomatic injury.18 While plating the buttress, the surgeon must be aware of the risk for maxillary tooth bud injury, particularly in children below age 6.19 Microplates are often sufficient in children. In evaluating possible soft tissue entrapment in the orbital floor or malalignment of fracture segments, a low threshold of suspicion should prompt exploration of the orbital floor. Isolated zygomatic arch fractures without displacement may be best managed via observation and soft diet. Minimally displaced arch fragments that reduce upon intraoral approach and appear stable remain so without further intervention.19
Figure 4.
Displaced fractures of the zygomatic arch should undergo open reduction and internal fixation. During fixation, great care must be taken to re-create the arch as a column along the anteroposterior axis instead of as a rounded semicircle.
Maxillary Injury
Though particularly infrequent in the pediatric population, these fractures can often be managed effectively with maxillomandibular fixation (MMF) and elastic traction in the presence of adequately erupted teeth. If not, open reduction and fixation is necessary. After application of MMF via arch bar application to both upper and lower dental structures, occlusion should be optimized to identify optimal maxillary reduction. If the maxilla appears both displaced and impacted, efforts must be made to free the injured segment. If reduction is not possible with conservative methods, one should proceed with a Le Fort I osteotomy.
After exposure, potential fractures of the maxillomandibular, zygomaticomaxillary, or nasomaxillary buttresses should be reduced and stabilized. With MMF in place, identification and stabilization of the least displaced buttress first provides the most helpful guide to facial height restoration. Fixation with miniplates and screws is usually optimal. However, great care must be taken during fixation to minimize the potential for injury to the tooth germs or erupting teeth.20 At the Le Fort I level, miniplates are placed at each nasomaxillary and zygomaticomaxillary buttresses. For Le Fort II and III fractures, additional plating is necessary as indicated by the fracture pattern.
Severely damaged bone, or portions of crushed material greater than 0.5 cm, must be replaced at the time of reconstruction. In the event that one of the major buttresses of the maxilla requires reconstruction, bone grafts should be placed in conjunction with rigid fixation. Calvarial bone is a good source for reconstruction. Despite exposure to neighboring sinuses, autogenous bone grafts demonstrate an acceptably low incidence of infection (less than 5%). After reduction and stabilization, MMF should be released, mandible range assessed, and occlusion evaluated. Any malocclusion is indicative of either inaccurate reduction or fixation. In this event, plate fixation must be removed, MMF reapplied, and reconstruction repeated.
Mandible Fracture
The management of mandibular fractures in children depends on fracture site, stage of skeletal growth, and dental development.21,22 Generally, mandibular fractures without displacement or malocclusion are managed by close observation, a soft diet, avoidance of physical activities, and analgesics (Fig. 5). Typically, intracapsular condylar fractures are best approached with range of motion rehabilitation. Subcondylar injuries may also be managed conservatively in the absence of malocclusion. However, displacement of these fractures should be managed with 7 to 10 days of intermaxillary fixation (IMF) using 1 point of anterior wire stabilization. This is accomplished by placing a circummandibular wire at the symphysis and attaching this to a wire placed through a drill hole at the pyriform aperture. Of particular concern in the pediatric population, IMF should be used sparingly and for limited time periods as prolonged maxillomandibular stabilization may promote ankylosis. Elsewhere on the mandible, displaced fractures respond well to 2.0-mm miniplate fixation along the inferior mandibular border using monocortical screws, or placement of an acrylic lingual splint.
Figure 5.
The substantial resiliency of the child's mandible often results in incomplete fractures. These may be managed conservatively, including restricted diet, close observation, avoidance of physical activities, and analgesics.
POTENTIAL GROWTH DISTURBANCES AFTER PEDIATRIC FACIAL FRACTURE
Despite the resiliency of the pediatric facial skeleton, the potential for long-term growth defects is a particular concern in this population. Because of the contribution of the ethmoid, vomer, septum, and maxilla to facial projection, midface injuries may result in long-term skeletal deformities. In addition, naso-orbital-ethmoid or severe nasal fractures can progress to saddle-nose deformity or septal deviation.23 Although mandibular condylar fractures usually heal well in children, parents must understand the risk of long-term growth restriction. This may manifest as deviation of the chin point to the affected side and may not be manifest for quite some period of time.22
COMPLICATIONS OF PEDIATRIC FACIAL FRACTURE MANAGEMENT
Postoperative complications after facial fracture or repair are uncommon in children. Because of the child's greater osteogenic potential, faster healing response, and less frequent need for open reduction and rigid fixation, postoperative infections, malunions, and nonunions are all less frequent than that seen in the adult population.2,7,11 Perhaps of greatest importance, a relatively greater number of fractures are minimally displaced to nondisplaced and may require no further treatment other than expectant observation. As in adults, enophthalmos and persistent diplopia may develop after orbital fracture. However, with the increased incidence of orbital roof injury observed in the very young, the phenomenon of the “growing” orbital roof fracture deserves special mention. Though still relatively uncommon, the “growing” fracture may occur quite some time after orbital roof injury as the brain continues to grow. In the setting of a significantly weakened orbital roof structure, increasing brain volume may continuously extend into the affected orbit producing globe protrusion.12,13 At a minimum, these children must be followed with CT scanning to ensure that this is not a problem. In general, complications of midface fractures are rare but may include telecanthus, nasolacrimal obstruction, and nasal collapse. In addition, asymmetric nasal deformity, septal deviation, and nasal airway obstruction may result after disturbance of the nasoethmoid or septovomerine sutures.15,16 Secondary rhinoplasty may be required; however, this should be delayed until completion of midfacial growth in the mid-teen years. As a result of maxillary or mandibular fractures, malocclusion is rare. There is typically complete dental compensation for any skeletal malalignment in the young child. In the not infrequent case of intracapsular condylar injury, mandibular asymmetry may result due to growth disturbance. Most disturbingly, temporomandibular joint ankylosis is seen in 1 to 7% of condylar fractures.21,22 The risk of ankylosis increases with bilateral condylar fractures, in children between ages 2 and 5, and with delayed treatment21 or prolonged MMF.21,22
CONCLUSION
With advances in prevention, imaging evaluation, and bone fixation technology, the management of pediatric facial fractures continues to evolve at a rapid pace. Although often complex, effective management of fractures within this challenging population is directly dependent upon thorough initial evaluation, correct injury assessment, and timely initiation of chosen therapy. Although facial fractures in this group are uncommon relative to their adult counterparts, a thorough understanding of issues relevant to pediatric facial fractures is critical in providing ideal acute management and optimizing long-term success.
References
- Acton C H, Nixon J W, Clark R C. Bicycle riding and oral/maxillofacial trauma in young children. Med J Aust. 1996;165:249–251. doi: 10.5694/j.1326-5377.1996.tb124957.x. [DOI] [PubMed] [Google Scholar]
- Gussack G S, Luterman A, Powell R W, Rodgers K, Ramenofsky M L. Pediatric maxillofacial trauma: unique features in diagnosis and treatment. Laryngoscope. 1987;97:925–930. [PubMed] [Google Scholar]
- Haug R H, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:126–134. doi: 10.1067/moe.2000.107974. [DOI] [PubMed] [Google Scholar]
- Baumann A, Troulis M J, Kaban L B. Facial trauma I: midfacial fractures. In: In: Kaban LB, Troulis MJ, editor. Pediatric Oral and Maxillofacial Surgery. Philadelphia, PA: Saunders; 2004. pp. 425–440. [Google Scholar]
- Adams C D, Januszkiewcz J S, Judson J. Changing patterns of severe craniomaxillofacial trauma in Auckland over eight years. Aust N Z J Surg. 2000;70:401–404. doi: 10.1046/j.1440-1622.2000.01836.x. [DOI] [PubMed] [Google Scholar]
- Dodson T B, Kaban L B. California mandatory seat belt law: the effect of recent legislation on motor vehicle accident related maxillofacial injuries. J Oral Maxillofac Surg. 1988;46:875–880. doi: 10.1016/0278-2391(88)90054-7. [DOI] [PubMed] [Google Scholar]
- Kaban L B. Diagnosis and treatment of fractures of the facial bones in children. J Oral Maxillofac Surg. 1993;51:722–729. doi: 10.1016/s0278-2391(10)80409-4. [DOI] [PubMed] [Google Scholar]
- Mulliken J B, Kaban L B, Murray J E. Management of facial fractures in children. Clin Plast Surg. 1977;4:491–502. [PubMed] [Google Scholar]
- Muraoka M, Nakai Y, Nakagawa K, et al. Fifteen-year statistics and observation of facial bone fracture. Osaka City Med J. 1995;41:49–61. [PubMed] [Google Scholar]
- Adekeye E O. Pediatric fractures of the facial skeleton: a survey of 85 cases from Kaduna, Nigeria. J Oral Surg. 1980;38:355–358. [PubMed] [Google Scholar]
- Anderson P J. Fractures of the facial skeleton in children. Injury. 1995;26:47–50. doi: 10.1016/0020-1383(95)90552-9. [DOI] [PubMed] [Google Scholar]
- Dulley B, Fells P. Long-term followup of orbital blow-out fractures with and without surgery. Mod Probl Ophthalmol. 1975;14:467–470. [PubMed] [Google Scholar]
- Lukas J, Rambousek P. Injuries of the upper and middle thirds of the face: analysis of the cause of injury. Cas Lek Cesk. 2001;140:47–50. [PubMed] [Google Scholar]
- Raflo G T. Blow-in and blow-out fractures of the orbit: clinical correlations and proposed mechanisms. Ophthalmic Surg. 1984;15:114–119. [PubMed] [Google Scholar]
- Mustoe T A, Kaban L B, Mulliken J B. Nasal fractures in children. Eur J Plast Surg. 1987;10:135–138. [Google Scholar]
- Precious D S, Delaire J, Hoffman C D. The effects of nasomaxillary injury on future facial growth. Oral Surg Oral Med Oral Pathol. 1988;66:525–530. doi: 10.1016/0030-4220(88)90369-6. [DOI] [PubMed] [Google Scholar]
- Heitsch M, Mohr C, Schettler D. Indications for the surgical treatment of midfacial fractures in children. Dtsch Zahnarztl Z. 1990;45:803–805. [PubMed] [Google Scholar]
- Fortunato M A, Fielding A F, Guernsey L H. Facial bone fractures in children. Oral Surg Oral Med Oral Pathol. 1982;53:225–230. doi: 10.1016/0030-4220(82)90294-8. [DOI] [PubMed] [Google Scholar]
- Kaban L B. Facial trauma I: midface fractures. In: In: Kaban LB, editor. Pediatric Oral and Maxillofacial Surgery. Philadelphia, PA: WB Saunders; 1990. pp. 209–232. [Google Scholar]
- Iizuka T, Thoren H, Annino D J, Jr, Hallikainen D, Lindqvist C. Midfacial fractures in pediatric patients: frequency, characteristics, and causes. Arch Otolaryngol Head Neck Surg. 1995;121:1366–1371. doi: 10.1001/archotol.1995.01890120026005. [DOI] [PubMed] [Google Scholar]
- Baumann A, Troulis M J, Kaban L B. Facial trauma II: dentoalveolar injuries and mandibular fractures. In: In: Kaban LB, Troulis MJ, editor. Pediatric Oral and Maxillofacial Surgery. Philadelphia, PA: Saunders; 2004. pp. 441–460. [Google Scholar]
- Demianczuk A N, Verchere C, Phillips J H. The effect on facial growth of pediatric mandibular fractures. J Craniofac Surg. 1999;10:323–328. doi: 10.1097/00001665-199907000-00007. [DOI] [PubMed] [Google Scholar]
- Hartel J, Pohl A, Greve J W. Fractures of the facial skull in the growth period and concomitant injuries. Unfallchirurg. 1994;97:991–993. [PubMed] [Google Scholar]