Abstract
The temporomandibular joint (TMJ) has many essential functions. None of its components are exempt from injury. Facial asymmetry, malocclusion, disturbances in growth, osteoarthritis, and ankylosis can manifest as complications from trauma to the TMJ. The goals of initial treatment include achievement of pretraumatic function, restoration of facial symmetry, and resolution of pain. These same objectives hold true for late repairs and reconstruction of the TMJ apparatus. Treatment is demanding, and with opposing approaches. The following article explores various treatment options for problems presenting as a result of a history of trauma to the TMJ.
Keywords: TMJ, posttraumatic TMJ disorders, facial asymmetry, malocclusion, growth disturbance, osteoarthritis, ankylosis
The temporomandibular joint (TMJ) plays a critical role in speech, mastication, and swallowing. This bilateral, diarthrodial, and ginglymoid joint is not exempt to injury. The structures that can be damaged include the bony components (the condyle and the glenoid fossa) and their associated fibrocartilage articular surfaces; the articular disk; and the synovial lining of the superior and inferior joint space.
Condylar fractures are common injuries, comprising approximately 25% of all mandibular fractures.1 Late complications of traumatic TMJ injuries include facial asymmetry, malocclusion, growth disturbance, osteoarthritis, and ankylosis. Potential functional problems include limitation in opening, limitation in excursive movements, deviation on opening, and malocclusion manifesting late as a crossbite on the fracture side and hypereruption of the teeth on the opposite side. In addition, a decrease in mandibular ramus height can result in a shorter lower facial third on the fracture side.
The management of injury to the TMJ complex has sparked an ongoing debate in the literature.2,3,4,5 Regardless of whether surgical or nonsurgical means in initial treatment of condylar fractures are employed, the goals are essentially the same: achievement of pretraumatic function, restoration of facial symmetry, and resolution of pain. These same objectives hold true for late repairs and reconstruction of the TMJ apparatus. Depending on the particular problem, various treatment options have been proposed and will be presented.
FACIAL ASYMMETRY
Asymmetry after condylar fracture is common and is influenced by the degree of displacement. This is exemplified as a decrease in mandibular ramus height, resulting in a shorter lower facial third on the fracture side. Also, the mandibular midline may deviate toward the fracture side during opening, due to the unopposed pull of the contralateral lateral pterygoid muscle (Fig. 1).
Figure 1.
Facial asymmetry following condylar fracture. The mandibular midline deviates toward the fracture side during opening.
In 2000, Ellis and Throckmorton quantitatively compared vertical height and facial morphology following mandibular condylar fracture in patients treated with or without surgery.6 Their study included a total of 146 patients (81 treated nonsurgically, 65 treated surgically). They measured ramus heights and occlusal plane angles from posteroanterior cephalograms and panoramic X-rays. At 2 or more years after treatment, they found a mean difference in posterior facial height (nonfractured side minus fractured side) of 4.72 mm in the nonsurgery group versus 0.08 mm in the surgery group. Furthermore, the range of this difference was much greater in the nonsurgery group. Mean shortening in ramus height was also greater in the nonsurgery group. In another study, preoperatively, 77 fractures (74.03%) had loss of ramus height, with a maximum of 15 mm and a mean of 5.4 ± 3.12 mm.7 Postoperatively, including both closed and open treatment, the mean loss of ramus height was 4.25 ± 3.22 mm.7
MALOCCLUSION
The type of malocclusion observed depends on the injury pattern. For instance, a unilateral condylar fracture usually results in ipsilateral premature contact and a contralateral open bite of the posterior teeth. The mandibular midline deviates toward the fracture side during opening due to the unopposed pull of the contralateral lateral pterygoid muscle (Fig. 2). On the other hand, bilateral condylar fractures usually result in an anterior open bite.
Figure 2.
(A,B) Malocclusion following condylar fracture. This manifests late as a crossbite on the fracture side and hypereruption of the teeth on the opposite side.
Optimally, if treated at initial presentation, anatomic reapproximation of a condylar fracture can be accomplished via surgical intervention, resulting in a closer reestablishment of preinjury occlusion versus nonsurgical or closed treatment.8 In 2000, Ellis and Throckmorton studied 137 patients with unilateral mandibular condylar fractures (77 treated nonsurgically and 65 treated with surgery).9 Those treated nonsurgically had a significantly greater percentage of malocclusion when observers compared them with patients treated surgically, utilizing minidynamic compression plates for fixation. However, the majority of condylar fractures are treated employing a nonsurgical approach. The incidence of posttraumatic malocclusion is reported to range from 1.4 to 13%.5,10 Bilateral condylar fractures result in the most malocclusions, characterized by an anterior open bite.11 The more displaced the condylar fracture, the more adaptations are necessary to reestablish the preinjury occlusal relationship.6
Treatment
Treatment of facial asymmetry and malocclusion can be accomplished with dental occlusal equilibration, extraction of interfering teeth, prosthodontic rehabilitation,12 orthodontics, orthognathic surgery6,13 (Fig. 3), alloplastic TMJ reconstruction, or combinations of these options. Becking et al treated 15 patients with late unilateral condylar fractures and asymmetric malocclusions with mandibular ramus osteotomies (unilateral or bilateral, depending on the severity of the asymmetry).13 With a minimum follow-up of 1 year, a stable occlusion was noted in all of their patients. This same group treated four patients, who had late bilateral condylar fractures and an anterior open bite, with a LeFort I maxillary posterior impaction, resulting in a stable occlusion. However, restoration of mandibular ramus height is not achieved with this method. Reestablishment of ramus height can be accomplished with bilateral osteotomies of the mandible, but with a subsequent increased relapse rate.14,15,16,17
Figure 3.
LeFort I maxillary osteotomy and bilateral mandibular ramus osteotomies to treat asymmetry and malocclusion from old left subcondylar mandible fracture. (A,B) Preoperative. (C,D) Postoperative.
GROWTH DISTURBANCE
Asymmetrical mandibular growth has been observed in about 25% of children who have sustained condylar fractures.18 The development of mandibular asymmetry is thought to result from growth disturbance from either injury to the condylar cartilaginous cap or from disruption in function due to ankylosis and hypomobility. Functional disturbances and esthetic deformities can result (Fig. 4). If growth is disrupted, the affected ramus height is decreased, resulting in a shorter facial lower third, while the unaffected side grows normally. Also, the chin will deviate toward the affected side. Furthermore, dental compensations, crossbites on the ipsilateral side and hypereruption of the teeth on the contralateral side, producing an occlusal cant, will eventually occur to reestablish a functional occlusion.
Figure 4.
(A,B) Growth disturbance with condylar fracture.
Several factors are found to influence growth including age, the severity of the injury, and the period of immobility. The earlier in life a condylar process fracture occurs, the greater the resultant skeletal changes.19,20 Moreover, the younger the individual, the more complete and rapid the restitution of a morphologically, anatomically, and functionally normal condylar articulation. In adolescents, the potential for significant restitution and remodeling is still present but not to the degree seen in children under 12 years of age. In adults, functional adaptation of the TMJ occurs. Lindahl and Hollender studied the radiographs of 67 patients with 76 condylar fractures.21 In the patients 3 to 11 years old, 20 of 27 patients showed complete remodeling of the condyle-fossa relationship by 48 months. In another study, Dahlström and associates followed 36 patients (22 adults, 14 children) with nonsurgically treated condylar fractures.8 Radiographic evaluation revealed the ability of the children to regenerate a morphologically normal condyle and a less dramatic capacity in adults.6
OSTEOARTHRITIS
Osteoarthritis or degenerative joint disease of the TMJ is attributed to articular cartilage failure. It develops as a result of a complex interaction of multiple factors. Direct trauma to the mandible producing condylar fractures, subcondylar fractures, other mandibular fractures, or no fractures has been implicated as one of the initiating factors of osteoarthritis. Trauma to the mandible can induce a joint effusion acutely.22 In 1988, Harris et al studied 13 patients who had sustained trauma to the mandible and found abnormal uptake in their TMJ scintiscans.23 More recently, Yun and Kim described evidence of acute synovitis, such as fibrillation and ecchymosis, with arthroscopic examination of patients who had mandibular fractures not directly involving the condyles.24 Furthermore, cytological and biochemical analysis from the synovial fluids of these patients demonstrated the presence of degenerated cells, inflammatory cells, crystals, and a considerable amount of pain-related mediators, such as prostaglandin E2 and leukotriene B4. Also, Seligman and Pullinger showed in a multiple stepwise logistic regression analysis that trauma history is a moderate differentiating feature in patients with intracapsular TMJ disorder.25
Due to the complex and multifactorial etiology of this particular disease process, the actual incidence of osteoarthritis directly related to trauma to the mandible is difficult to determine, especially in traumatic events that do not result in fractures. The existing literature reports a wide range. It has been estimated that in anywhere from 9 to 85% of patients, condylar fractures result in degenerative disease of the TMJ.11 One study reports that 38.3% of patients, with histologically confirmed TMJ osteoarthritis have a history of trauma to the mandible.26 Probert et al reported that 16 of their 28 patients (57%) who were treated for temporomandibular pain dysfunction disorder following road traffic accidents had associated facial injury.27 In a study by Miller and Bodner, 40% of the patients were diagnosed with arthogenous temporomandibular disorder 6 months after oromaxillofacial trauma, with or without mandible fractures.28
The clinical presentation of patients with posttraumatic TMJ osteoarthritis is nondiscernable from TMJ osteoarthritis of other etiologies. The predominant symptoms include constant preauricular pain, with or without radiation, and crepitus. Other symptoms and signs are TMJ clicking, popping, locking, and deviation on opening.26
Treatment
Nonsurgical modalities are usually first utilized in the treatment of TMJ osteoarthritis. Multiple studies have shown that monoplane bite appliances, diet modification, nonsteroidal anti-inflammatory medications, muscle relaxants, moist heat or ice, and physical therapy are effective.29 If nonsurgical modalities fail, then surgical options may be considered. Depending on the clinical presentation of each individual patient, minimally invasive procedures, such as arthrocentesis and/or arthoscopy, should be considered prior to open arthroplasty.30 Open arthoplasty with or without total joint replacement is reserved for end-stage TMJ disease.
ANKYLOSIS
The most devastating complication of posttraumatic TMJ injury is craniomandibular ankylosis (Fig. 5). In the adult population, it manifests as an inability to obtain adequate mouth opening, with subsequent difficulties in oral hygiene, mastication, and speech, as well as, psychosocial distress.31,32 In the growing child, fusion of the TMJ can result in profound growth disturbances. This includes facial asymmetry, retrognathism, and secondary midface growth deficiency.32,33
Figure 5.
Computed tomography scan depicting craniomandibular ankylosis.
Acceptable surgical management of these patients has proven difficult, as evidenced by the number of treatment modalities and controversies surrounding this topic. Surgical intervention offers additional challenges in airway management during anesthesia induction and perioperative care.34 Fortunately, this is a rare complication following condylar injury. As a result, few conclusive studies have been written, with most of the available literature filled with case series and retrospective analysis. Current treatment options range from gap athroplasty with alloplastic or autogenous grafting, costochondral grafting, distraction osteogenesis, and total joint replacement.32,35,36,37 The growing patient offers additional reconstructive challenges and often requires further corrective surgeries, as a result of dynamic changes in the patient.
Treatment goals of joint reconstruction should include adequate mouth opening for mastication and speech, restoration of facial symmetry, and reduction of pain.38 Additional requirements for the pediatric patient include maximization of growth potential and allocation for additional corrective surgical procedures.38
CLASSIFICATION
Immobility of the TMJ results largely from a combination of fibrous, cartilaginous, fibro-osseous, and bony union. Complete bony union is atypical as depicted by the average maximal incisal opening of the typical patient being between 4 and 20 mm.33,39,40,41 This suggests the presence of a pseudoarthosis or incomplete fusion. The most widely accepted classification of TMJ ankylosis was presented by Sawhney, who classified four types of pathological changes.20 Type 1 includes dense fibrous adhesions, which surround the joint, and flattening of the condylar head. Type 2 includes a flattened or deformed condylar head, with close proximity to the articular surface, and an evident, but limited, bony fusion of the outer anterior or posterior surface. Type 3 includes a bony bridge across the mandible and the zygomatic arch, with the displaced articular head fused to the medial side of the ramus, or the presence of an atrophic condylar head. Finally, type 4, the most common pattern in his series, exhibits a large bony block, which completely replaces the usual joint architecture. Another classification scheme proposed by El-Hakim and Metwalli is based on the proximity of the ankylosed mass to surrounding vital structures, particularly to the maxillary artery.42
RADIOLOGICAL EVALUATION
Most authors agree that computed tomography (CT) evaluation is necessary for surgical planning. When comparing CT with conventional plain films, CT provides superior resolution and imparts the best assessment of the union.11,20,43 In addition, the CT study may be combined with angiography to better delineate vascular structures. Magnetic resonance imaging offers no additional information in the management of ankylosis.43 Recently, several authors have reported on the use of CT navigation systems for preoperative planning and precise surgical guidance in real time.44 This technology is just beginning to be introduced into maxillofacial surgery.
INITIAL SURGICAL MANAGEMENT
In 1990, Kaban et al proposed a protocol for the management of TMJ ankylosis.45 Since then, most authors have reported cases that followed the basic tenets of the principles for management suggested in that series.35,41 Disagreement still persists concerning the optimal reconstructive method utilized.37,38,39,41,46,47 In this algorithm, the first step is aggressive resection of the ankylotic mass. This is followed by ipsilateral coronoidectomy and stripping of the pterygomasseteric sling, in order to accomplish an intraoperative incisal opening of 35 mm. If this is not achieved, contralateral coronoidectomy is performed. This is followed by lining of the joint space with either temporalis muscle and fascia or cartilage, reconstruction of the ramus with a costochondral graft, rigid fixation of the graft, and finally, early immobilization. It has long been recognized that prolonged immobilization of the mandible results in fibrosis or atrophy of the associated muscles of mastication.48 If this is not addressed, mouth opening will be hindered, despite adequate release of the ankylotic joint. Therefore, coronoidectomy and muscular release must be performed. A jaw mobilizer may also be utilized to release scar tissue and to obtain optimum mobility prior to reconstruction.
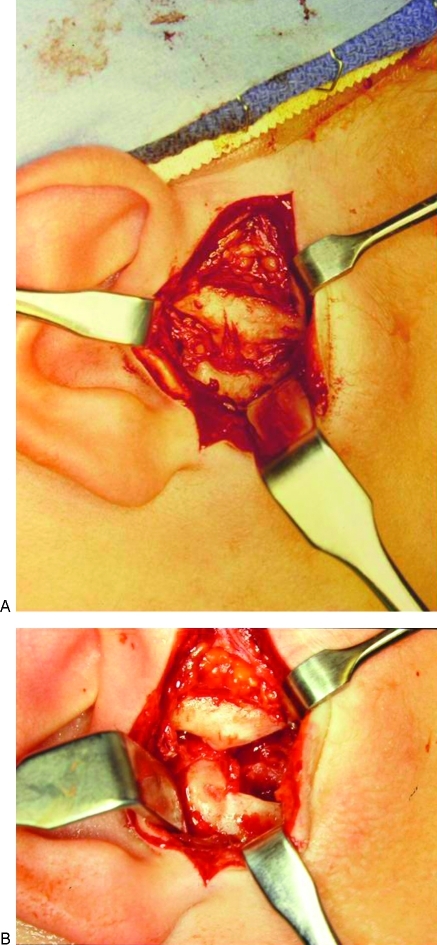
The critical surgical defect required has not been fully elicited with respect to TMJ ankylosis. The necessary resection of bone to prevent reankylosis has been reported to be anywhere from 0.5 to 4.0 cm.49 Increased bony resection theoretically decreases the likelihood of reankylosis, but at the expense of ramus height47 (Fig. 6).
Figure 6.
Resection of ankylotic mass. (A) Ankylotic mass. (B) Surgical defect following resection.
An alternative approach to the above protocol includes creating an osteotomy and subsequent pseudoarthosis below the ankylotic mass, as described by Salins.47 Because with this technique there is less exposed raw bone, the incidence of reankylosis is reportedly decreased.47 Conversely, reconstruction without lining of the joint space, particularly in the pediatric population, has been presented.33 This allows for additional reconstructive options in the event of reankylosis. As noted previously, the most controversial aspect of TMJ reconstruction following ankylosis is the final reconstructive method.
RECONSTRUCTIVE OPTIONS
The reconstructive goals differ in the adult versus the growing patient. When ankylosis occurs in the skeletally mature patient, the ensuing deficit is limited to trismus and its subsequent sequelae. The goals are complete and definitive reconstitution of form and function. In the growing patient, the resulting pathology secondarily affects growth of the maxilla and the ipsilateral mandible, causing facial disharmony. In addition to affording a functional joint, the surgeon has to contend with the continued maturation of the patient. This makes the problem of ankylosis in the pediatric population a much greater challenge, often requiring multiple corrective surgeries before definitive treatment is rendered. Several treatment options will be discussed here.
Gap Arthroplasty with Interpositional Grafting
Gap arthroplasty with interpositional grafting remains the mainstay of join reconstruction following ankylosis.50,51,52 In 1966, Topazian compared 40 patients treated with gap athroplasty, with and without the use of interpositional grafting. He found that half of the patients without grafting had reankylosis, and those who were grafted had no recurrence.49 It was hypothesized that interpositional grafting shields the exposed bony surface, preventing reankylosis.
Since then, many different materials, including autogenous tissues, such as fat, dermis, temporalis muscle and fascia, and auricular cartilage, have been used as interpositional grafts.41,53 Alloplastic materials have included silastic, silicone, acrylic, and various metals.41 The most popular autogenous interpositional graft reported is the temporalis myofascial flap. The advantages of this flap include its good vascular supply, durability, and relative proximity to the surgical site.54,55 In their study of 115 reconstructed joints using magnetic resonance imaging evaluation, Umeda et al reported on the long-term (mean follow-up of 1.7 years) viability of this flap.55 Failures secondary to pain and flap necrosis have been reported.53 Recent reports of disc salvage and repositioning, which allow for more manageable secondary procedures to occur if necessary, have been met with some success.50,56,57,58 At this institution, a temporary silastic implant is utilized. The graft is left in place long enough to allow fibrotic encapsulation of the silastic. The second stage, typically under conscious sedation, is then undertaken to remove the silastic sheet, leaving behind the autogenous fibrotic capsule.
Costochondral Grafting
Costochondral grafting has been the primary treatment option in the growing pediatric patient. This type of graft has been utilized because of its ideal shape, remodeling capacity, growth potential, and good bony union. Furthermore, the use of autogenous tissues prevents the potential for foreign body reaction.52 Recent reports have questioned the utility of costochondral grafts due to their unpredictable growth characteristics, necessitating secondary corrective surgeries.56,59 Other disadvantages include donor site morbidity, including the possible need for chest tubes and excessive lateral bulkiness of the graft.56,59
Distraction Osteogenesis
Following gap arthoplasty with interpositional grafting, residual facial and skeletal deformities may be corrected with distraction osteogenesis. Distraction osteogenesis consists of replacing costochondral grafting as the preferred treatment option, due to its more controlled and predictable growth potential.60,61,62 However, a second surgical procedure is required for removal of the distraction device. Also, patient cooperation and compliance is relied upon while the device is in place. It is undetermined whether to initiate immediate or delayed distraction until after joint reconstruction.60,62,63 Lastly, distraction osteogenesis is still a relatively new treatment method for ankylosis, and more long-term follow-up studies are needed to evaluate relapse rates.
Total Joint Replacement
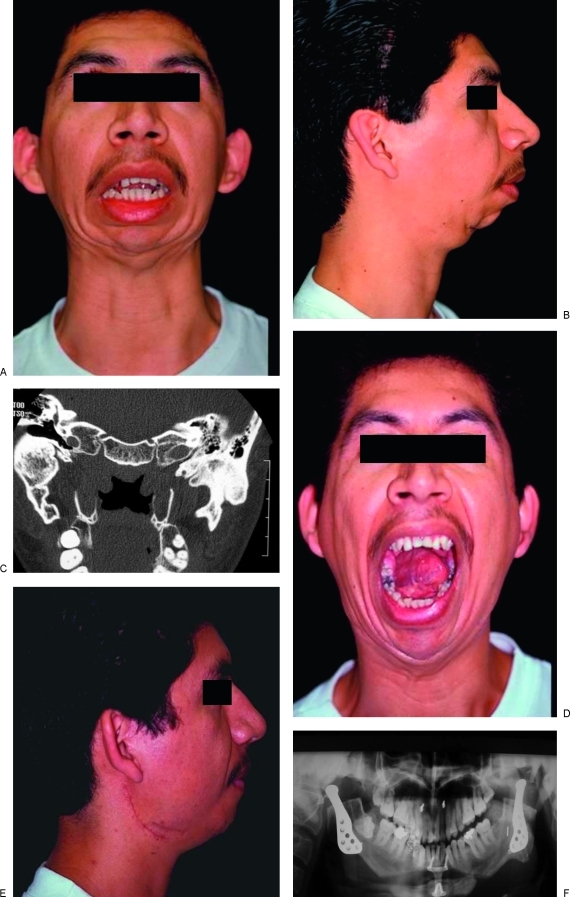
Historically, TMJ replacement has included the use of fossa-only prostheses, condyle-only designs, and finally, total joint replacement.64 Past experiences have proven that the entire joint requires prosthetic reconstruction in order to avoid unacceptable bone resorption and prosthetic failures.64 Total joint replacement offers the advantage of immediate function, the ability to correct bony defects and facial asymmetry, and lack of donor site morbidity (Fig. 7). It also has been reported to have a reduced incidence of reankylosis.46,51,52,65 Disadvantages include potential wear debris and associated tissue reaction, finite durability of the prosthesis, potential need for replacement, and associated costs. For the pediatric patient, alloplastic joint reconstruction offers less than satisfactory outcomes, as there is no growth potential with prosthetic implants. Not surprisingly, many surgeons still approach alloplastic TMJ reconstruction with caution.66
Figure 7.
Management of ankylosis with total temporomandibular joint replacement. (A) Preoperative maximal incisal opening. (B) Preoperative patient profile. (C) Preoperative computed tomography scan depicting bilateral temporomandibular joint ankylosis. (D) Postoperative maximal incisal opening. (E) Postoperative patient profile. (F) Postoperative panorex X-ray with Lorenz temporomandibular joint prosthesis.
Experience with the problems associated with the proplast implant failures has resulted in new insight into TMJ reconstruction. Studies comparing joint reconstruction in these multioperated patients and improved implant prostheses have given surgeons a fresh perspective into the utility of total alloplastic joints for the reconstruction of TMJ ankylosis.65,67,68 There are several commercially available total joint replacement systems available in the United States. In general, these systems come as either “off-the-shelf” and are fitted intraoperatively or a custom joint is fabricated from a protocol specific CT scan. Saeed and Kent retrospectively compared joint reconstruction with alloplastic versus autogenous (costochondral) grafts.46 In this study of 100 patients, neither group achieved a significant reduction in reported symptoms, and only the alloplastic group had a significant improvement in incisal opening. Also, both groups had similar complication rates. However, the autogenous group's complications were deemed to be more significant. This included a high rate of reankylosis (37%). The complications associated with alloplastic reconstruction were primarily temporary. The most common complication noted was temporary seventh cranial nerve palsy.46 Henry and Wolford reported on 62 patients who underwent TMJ reconstruction, following proplast/Teflon implant removal, with either autogenous or alloplastic means, and found higher success rates (88%) with the total joint prosthesis.67 Long-term studies (10 to 14 years) of total joint implants have recently been reported.69 They have shown significant increases in quality of life scores and proven the durability of currently available implants, without the foreign body reaction seen in previous implant failures. Continued investigation is required to ensure safe reconstruction for these individuals.
POSTOPERATIVE MANAGEMENT
Despite the method chosen for joint reconstruction, the most critical component in the successful reconstruction of the TMJ is early joint mobilization and physical therapy. Early mobilization prevents fibrosis from developing, as well as the formation of bony bridges. Commercially available devices are available to help stretch the musculature and surrounding tissue and also to aid patients in achieving adequate opening goals. Alternatively, tongue blade therapy, with sequential increases in the number of tongue blades tolerated until satisfactory opening is achieved, can be utilized. During the immediate postoperative period, it is imperative to provide adequate pain control, which helps to ensure that patients will be able to mimic intraoperative functioning. Nonsteroidal anti-inflammatory drugs are an ideal choice, as evidence exists to suggest that they play a role in preventing reankylosis.70
MANAGEMENT OF REANKYLOSIS
The most devastating complication for patients following joint reconstruction is reankylosis. Usually, the most prudent option for these patients is additional surgical intervention, either with the same reconstructive method or with the utilization of other options, depending on the individual needs of the patient. For those patients who have experienced multiple bouts of reankylosis despite appropriate interventions, radiation therapy is a viable treatment option. Typically, a protocol of 1000 rads in five fractioned doses following surgical reexcision has been found to be successful when compared with controls.71
CONCLUSION
The anatomic complexity of the TMJ makes diagnosis difficult and treatment demanding and controversial. Inevitably, secondary repairs and reconstruction are even more challenging. Posttraumatic complications include facial asymmetry, malocclusion, growth disturbance, osteoarthritis, and ankylosis. As fracture fixation mechanisms and alloplastic materials have evolved, the surgeon has more feasible treatment modalities to treat these injuries, both primarily and secondarily.
References
- Haug R H, Prather J, Indresano A. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- Chalmers J LC. Fractures involving the mandibular condyle: a post-treatment survey of 120 cases. J Oral Surg. 1947;5:45–73. [PubMed] [Google Scholar]
- De Riu G, Gamba U, Anghinoni M, Sesenna E. A comparison of open and closed treatment of condylar fractures: a change in philosophy. Int J Oral Maxillofac Surg. 2001;30:384–389. doi: 10.1054/ijom.2001.0103. [DOI] [PubMed] [Google Scholar]
- Konstantinovic V S, Dimitrijevic B. Surgical versus conservative treatment of unilateral condylar process fractures: CLINICAL and radiographic evaluation of 80 patients. J Oral Maxillofac Surg. 1992;50:349–352. doi: 10.1016/0278-2391(92)90395-g. [DOI] [PubMed] [Google Scholar]
- Silvennoinen U, Iizuka T, Oikarinen K, Lindqvist C. Analysis of possible factors leading to problems after nonsurgical treatment of condylar fractures. J Oral Maxillofac Surg. 1994;52:793–799. doi: 10.1016/0278-2391(94)90219-4. [DOI] [PubMed] [Google Scholar]
- Ellis E, Throckmorton G S. Facial symmetry after closed and open treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000;58:719–728. doi: 10.1053/joms.2000.7253. [DOI] [PubMed] [Google Scholar]
- Villarreal P M, Monje F, Junquera L M. Mandibular condyle fractures: determinants of treatment and outcome. J Oral Maxillofac Surg. 2004;62:155–163. doi: 10.1016/j.joms.2003.08.010. [DOI] [PubMed] [Google Scholar]
- Dahlström L, Kahnenberg K E, Lindahl L. 15-year follow-up on condylar fractures. Int J Oral Maxillofac Surg. 1989;18:18–23. doi: 10.1016/s0901-5027(89)80009-8. [DOI] [PubMed] [Google Scholar]
- Ellis E, Simon P, Throckmorton G. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000;58:260–268. doi: 10.1016/s0278-2391(00)90047-8. [DOI] [PubMed] [Google Scholar]
- de Amaratunga N A. Mouth opening after release of MMF in fracture patients. J Oral Maxillofac Surg. 1987;45:383–385. doi: 10.1016/0278-2391(87)90004-8. [DOI] [PubMed] [Google Scholar]
- Ellis E. Complications of mandibular condyle fractures. Int J Oral Maxillofac Surg. 1998;27:255–257. doi: 10.1016/s0901-5027(05)80506-5. [DOI] [PubMed] [Google Scholar]
- Laine P, Kontio R, Salo A, et al. Secondary correction of malocclusion after treatment of maxillofacial trauma. J Oral Maxillofac Surg. 2004;62:1312–1320. doi: 10.1016/j.joms.2004.02.014. [DOI] [PubMed] [Google Scholar]
- Becking A G, Zijderveld S A, Tuinzing D B. The surgical management of post-traumatic malocclusion. J Oral Maxillofac Surg. 1998;56:1370–1374. doi: 10.1016/s0278-2391(98)90394-9. [DOI] [PubMed] [Google Scholar]
- Proffit W R, Phillips C, Turvey T A. Stability following superior repositioning of the maxilla. Am J Orthod Dentofacial Orthop. 1987;92:151–163. doi: 10.1016/0889-5406(87)90370-2. [DOI] [PubMed] [Google Scholar]
- Schendel S A, Epker B N. Results after mandibular advancement surgery: an analysis of 87 cases. J Oral Surg. 1980;38:265–282. [PubMed] [Google Scholar]
- Will L A, West R A. Factors influencing the stability of sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1989;47:813–818. doi: 10.1016/s0278-2391(89)80039-4. [DOI] [PubMed] [Google Scholar]
- Proffit W R, Turvey T A, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11:191–204. [PubMed] [Google Scholar]
- Proffit W R, Vig K WL, Turvey T A. Early fracture of the mandibular condyles: frequently an unsuspected cause of growth disturbances. Am J Orthod. 1980;78:1–24. doi: 10.1016/0002-9416(80)90037-8. [DOI] [PubMed] [Google Scholar]
- Rowe N L. Fractures of the jaws in children. J Oral Surg. 1969;27:497–507. [PubMed] [Google Scholar]
- Sawhney C P. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986;77:29–40. [PubMed] [Google Scholar]
- Lindahl L, Hollender L. Condylar fractures of the mandible. II. A radiographic study of remodeling processes in the temporomandibular joint. Int J Oral Surg. 1977;6:153–165. doi: 10.1016/s0300-9785(77)80048-3. [DOI] [PubMed] [Google Scholar]
- Hettinga D L. Normal joint structures and their reaction to injury. J Orthop Sports Phys Ther. 1980;1:178–195. doi: 10.2519/jospt.1979.1.1.16. [DOI] [PubMed] [Google Scholar]
- Harris S A, Rood J P, Testa H J. Post-traumatic changes of the temporomandibular joint by bone scintigraphy. Int J Oral Maxillofac Surg. 1988;17:173–176. doi: 10.1016/s0901-5027(88)80025-0. [DOI] [PubMed] [Google Scholar]
- Yun P Y, Kim Y K. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder. J Oral Maxillofac Surg. 2005;63:1576–1583. doi: 10.1016/j.joms.2005.05.318. [DOI] [PubMed] [Google Scholar]
- Seligman D A, Pullinger A G. A multiple stepwise logistic regression analysis of trauma history and 16 other history and dental cofactors in females with temporomandibular disorders. J Orofac Pain. 1996;10:351–361. [PubMed] [Google Scholar]
- Norman J E. Post-traumatic disorders of the jaw joint. Ann R Coll Surg Engl. 1982;64:29–36. [PMC free article] [PubMed] [Google Scholar]
- Probert T C, Wiesenfeld D, Reade P C. Temporomandibular pain dysfunction disorder resulting from road traffic accidents—an Australian study. Int J Oral Maxillofac Surg. 1994;23:338–341. doi: 10.1016/s0901-5027(05)80049-9. [DOI] [PubMed] [Google Scholar]
- Miller V J, Bodner L. The long-term effect of oromaxillofacial trauma on the function of the temporomandibular joint. J Oral Rehabil. 1999;26:749–751. doi: 10.1046/j.1365-2842.1999.00418.x. [DOI] [PubMed] [Google Scholar]
- Okeson J. Nonsurgical treatment of internal derangements. Oral Maxillofac Surg Clin North Am. 1995;7:63–71. [Google Scholar]
- Goudot P, Jaquinet A R, Hugonnet S, et al. Improvement of pain and function after arthroscopy and arthrocentesis of the temporomandibular joint: a comparative study. J Craniomaxillofac Surg. 2000;28:39–42. doi: 10.1054/jcms.1999.0103. [DOI] [PubMed] [Google Scholar]
- Chidzonga M M. Temporomandibular joint ankylosis: review of thirty-two cases. Br J Oral Maxillofac Surg. 1999;37:123–126. doi: 10.1054/bjom.1997.0089. [DOI] [PubMed] [Google Scholar]
- Rowe N L. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:67–79. [PubMed] [Google Scholar]
- Posnick J C, Goldstein J A. Surgical management of temporomandibular joint ankylosis in the pediatric population. Plast Reconstr Surg. 1993;91:791–798. doi: 10.1097/00006534-199304001-00006. [DOI] [PubMed] [Google Scholar]
- Rowe N L. Ankylosis of the temporomandibular joint part 3. J R Coll Surg Edinb. 1982;27:209–218. [PubMed] [Google Scholar]
- Chossegros C, Guyot L, Cheynet F, et al. Full-thickness skin graft interposition after temporomandibular joint ankylosis surgery. Int J Oral Maxillofac Surg. 1999;28:330–334. [PubMed] [Google Scholar]
- Ortak T, Ulusoy M G, Sungur N, et al. Silicon in temporomandibular joint ankylosis surgery. J Craniofac Surg. 2001;12:232–236. doi: 10.1097/00001665-200105000-00007. [DOI] [PubMed] [Google Scholar]
- Zhang Y, He D M. Clinical investigation of early post-traumatic temporomandibular joint ankylosis and the role of repositioning discs in treatment. Int J Oral Maxillofac Surg. 2006;35:1096–1101. doi: 10.1016/j.ijom.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Rowe N L. Ankylosis of the temporomandibular joint part 2. J R Coll Surg Edinb. 1982;27:167–173. [PubMed] [Google Scholar]
- Ferretti C, Bryant R, Becker P, et al. Temporomandibular joint morphology following post-traumatic ankylosis in 26 patients. Int J Oral Maxillofac Surg. 2005;34:376–381. doi: 10.1016/j.ijom.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Saeed N, Hensher R, Mcleod N, et al. Reconstruction of the temporomandibular joint autogenous compared with alloplastic. Br J Oral Maxillofac Surg. 2002;40:296–299. doi: 10.1016/s0266-4356(02)00139-0. [DOI] [PubMed] [Google Scholar]
- Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg. 2001;30:189–193. doi: 10.1054/ijom.2001.0047. [DOI] [PubMed] [Google Scholar]
- El-Hakim I E, Metwalli S A. Imaging of temporomandibular joint ankylosis: a new radiographic classification. Dentomaxillofac Radiol. 2002;31:19–23. doi: 10.1038/sj/dmfr/4600660. [DOI] [PubMed] [Google Scholar]
- Aggarwal S, Mukhopadhyay S, Berry M, et al. Bony ankylosis of the temporomandibular joint: a computed tomography study. Oral Surg Oral Med Oral Pathol. 1990;69:128–132. doi: 10.1016/0030-4220(90)90281-v. [DOI] [PubMed] [Google Scholar]
- Malis D D, Xia J J, Gateno J, et al. New protocol for 1-stage treatment of temporomandibular joint ankylosis using surgical navigation. J Oral Maxillofac Surg. 2007;65:1843–1848. doi: 10.1016/j.joms.2005.11.080. [DOI] [PubMed] [Google Scholar]
- Kaban L B, Perrott D H, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–1151. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- Saeed N R, Kent J N. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg. 2003;32:606–609. doi: 10.1054/ijom.2003.0418. [DOI] [PubMed] [Google Scholar]
- Salins P C. New perspectives in the management of craniomandibular ankylosis. Int J Oral Maxillofac Surg. 2000;29:337–340. [PubMed] [Google Scholar]
- Guralnick W C, Kaban L B. Surgical treatment of mandibular hypomobility. J Oral Surg. 1976;34:343–348. [PubMed] [Google Scholar]
- Topazian R G. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;24:405–409. [PubMed] [Google Scholar]
- Li Z, Li Z-B, Li J-R. Surgical management of post-traumatic temporomandibular joint ankylosis by functional restoration with disk repositioning in children. Plast Reconstr Surg. 2007;119:1311–1316. doi: 10.1097/01.prs.0000254550.75633.60. [DOI] [PubMed] [Google Scholar]
- Mercuri L G. Alloplastic temporomandibular joint reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:631–637. doi: 10.1016/s1079-2104(98)90028-2. [DOI] [PubMed] [Google Scholar]
- Mercuri L G. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:70–75. doi: 10.1016/s0278-2391(00)80020-8. [DOI] [PubMed] [Google Scholar]
- MacIntosh R B. The use of autogenous tissues for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:63–69. doi: 10.1016/s0278-2391(00)80019-1. [DOI] [PubMed] [Google Scholar]
- Pogrel M A, Kaban L B. The role of a temporalis fascia and muscle flap in temporomandibular joint surgery. J Oral Maxillofac Surg. 1990;48:14–19. doi: 10.1016/0278-2391(90)90173-y. [DOI] [PubMed] [Google Scholar]
- Umeda H, Kaban L B, Pogrel M A, et al. Long-term viability of the temporalis muscle/fascia flap used for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1993;51:530–533. doi: 10.1016/s0278-2391(10)80509-9. [DOI] [PubMed] [Google Scholar]
- Ko E W, Huang C S, Chen Y-R. Temporomandibular joint ankylosis in children using costochondral grafts. J Oral Maxillofac Surg. 1999;57:789–798. doi: 10.1016/s0278-2391(99)90816-9. [DOI] [PubMed] [Google Scholar]
- Long X, Li X, Cheng Y, et al. Preservation of disc for treatment of traumatic temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2005;63:897–902. doi: 10.1016/j.joms.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Miyamoto H, Kurita K, Ogi N, et al. The role of the disk in sheep temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:151–158. doi: 10.1016/s1079-2104(99)70109-5. [DOI] [PubMed] [Google Scholar]
- Guyuron B, Lasa C I. Unpredictable growth patterns of costochondral graft. Plast Reconstr Surg. 1992;90:880–886. [PubMed] [Google Scholar]
- Bartlett S P, Losee J, Quinn P D. Severe proliferative congenital temporomandibular joint ankylosis: a proposed treatment protocol utilizing distraction osteogenesis. J Craniofac Surg. 2006;17:605–610. doi: 10.1097/00001665-200605000-00040. [DOI] [PubMed] [Google Scholar]
- Gabbay J S, Heller J B, Sing Y Y, et al. Temporomandibular joint bony ankylosis: comparison of treatment with transport distraction osteogenesis or the Matthews device arthroplasy. J Craniofac Surg. 2006;17:516–522. doi: 10.1097/00001665-200605000-00022. [DOI] [PubMed] [Google Scholar]
- Kwon T G, Park H S, Kim J B, et al. Staged surgical treatment for temporomandibular joint ankylosis: intraoral distraction after temporalis muscle flap reconstruction. J Oral Maxillofac Surg. 2006;64:1680–1683. doi: 10.1016/j.joms.2006.03.029. [DOI] [PubMed] [Google Scholar]
- Lopez E N, Dogliotti P L. Treatment of temporomandibular joint ankylosis in children: is it necessary to perform mandibular distraction simultaneously? J Craniofac Surg. 2004;15:879–884. doi: 10.1097/00001665-200409000-00037. [DOI] [PubMed] [Google Scholar]
- Loon J P van, de Bont G M, Boering G. Evaluation of temporomandibular joint prostheses: review of the literature from 1946-1994 and implications for future prosthesis designs. J Oral Maxillofac Surg. 1995;53:984–996. doi: 10.1016/0278-2391(95)90110-8. [DOI] [PubMed] [Google Scholar]
- Quinn P D. Lorenz prosthesis. Oral Maxillofac Surg Clin North Am. 2000;12:93–103. [Google Scholar]
- Laskin D M, Rotskoff K S, Ryan D, et al. Recommendations for management of patients with temporomandibular joint implants. J Oral Maxillofac Surg. 1993;51:1164–1172. doi: 10.1016/s0278-2391(10)80464-1. [DOI] [PubMed] [Google Scholar]
- Henry C H, Wolford L M. Treatment outcomes for temporomandibular joint reconstruction after proplast-teflon implant failure. J Oral Maxillofac Surg. 1993;51:352–358. doi: 10.1016/s0278-2391(10)80343-x. [DOI] [PubMed] [Google Scholar]
- Kearns G J, Perrott D H, Kaban L B. A protocol for the management of failed alloplastic temporomandibular joint disc implants. J Oral Maxillofac Surg. 1995;53:1240–1247. doi: 10.1016/0278-2391(95)90577-4. [DOI] [PubMed] [Google Scholar]
- Mercuri L G, Edibam N R, Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007;65:1140–1148. doi: 10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Vuolteenaho K, Moilanen T, Moilanen E. Non-steroidal anti-inflammatory drugs, cyclooxygenase-2 and the bone healing process. Basic Clin Pharmacol Toxicol. 2007;102:10–14. doi: 10.1111/j.1742-7843.2007.00149.x. [DOI] [PubMed] [Google Scholar]
- Reid R, Cooke H. Postoperative ionizing radiation in the management of heterotopic bone formation in the temporomandibular joint. J Oral Maxillofac Surg. 1999;57:900–905. doi: 10.1016/s0278-2391(99)90003-4. [DOI] [PubMed] [Google Scholar]