Abstract
We systematically reviewed the existing literature supporting the efficacy and safety of sinus preservation management for frontal sinus fractures in the modern era of endoscopic frontal sinus surgery. A systematic review of the English literature for the targeted objective was conducted using the PubMed database between January 1995 and August 2008. The PubMed database was queried using two major search terms of frontal sinus fracture or frontal sinus injury along with manual review of citations within bibliographies. Citations acquired from the primary search were filtered and relevant abstracts were identified that merited full review. Articles were identified that included any cohort of patients with frontal sinus fractures involving the frontal sinus outflow tract or posterior wall with sinus preservation management. A total of 231 citations were generated, and 56 abstracts were identified as potentially relevant articles. Sixteen articles merited full review, with seven articles meeting inclusion criteria for sinus preservation. There were 515 total patients in the studies with 350 patients managed with frontal sinus preservation. Similar short-term complications and effectiveness were found between fractures managed with sinus preservation and those with traditional management. Sinus preservation appears to be a safe and effective management strategy for select frontal sinus fractures. More transparent reporting of management strategies for individual cases or cohorts is needed. A standardized algorithm and categorization framework for future studies are proposed. Longer-term follow-up and larger prospective studies are necessary to assess the safety and efficacy of sinus preservation protocols.
Keywords: Frontal sinus trauma, frontal sinus outflow tract, endoscopic sinus surgery, sinus preservation, osteoplastic obliteration, sinus cranialization
The incidence of frontal sinus fractures ranges from 5 to 15% of all facial fractures.1,2 Motor vehicle crashes are the most common cause of frontal sinus fractures and often result in concomitant orbital, nasal, and midfacial fractures. Several options for management of frontal sinus fractures have been described in the literature based on fracture pattern and associated injuries. The degree of fracture displacement, status of the frontal sinus outflow tract (FSOT), and any associated intracranial injuries may dictate management by observation, open reduction and internal fixation (ORIF) of the anterior table, obliteration, or cranialization. Management of isolated anterior table fractures without FSOT involvement has generally met consensus in the literature.1,3 However, there is still controversy over the management of fractures with suspected involvement of the FSOT or posterior table. Fractures involving the FSOT have traditionally been obliterated or cranialized.4,5 Posterior table fractures associated with brain injury and persistent cerebrospinal fluid (CSF) leak often require dural repair and sinus cranialization.5,6
The goal of this work was to systematically review the literature to identify the effectiveness and safety of sinus preservation for management of frontal sinus fractures. Specifically, we narrowed our study to address the question: “In the era of endoscopic sinus surgery, what is the role of sinus preservation in the management of frontal sinus fractures?” In the past 15 years, endoscopic technology has become standard in the management of sinus disease and has more recently been utilized in facial fractures repair.7,8 We limited our literature search to articles published from January 1995 to the present, which we arbitrarily defined as the “endoscopic sinus surgery era.”
In addition, we propose a reporting system that may help standardize classification of frontal sinus fractures based on degree of anterior table, posterior table, and FSOT involvement. Ultimately, patient outcomes should include any complications with specific management, as well as information about frontal sinus ventilation. This reporting system may help standardize patient reporting and outcomes, which will facilitate comparison of patient cohorts across institutions and the development of a uniform treatment algorithm for management of frontal sinus fractures.
METHODS
Article Selection Process
The literature was searched for articles that contained patient data regarding management of frontal sinus fractures, with an emphasis on preservation of the frontal sinus. A multistep search of the PubMed database was performed using the major search terms of frontal sinus fracture or frontal sinus injury. The initial search was limited to include articles published between January 1995 and September 2008. Citations acquired from the primary search were filtered; all non-English and nonrelevant articles were excluded at this time. Citations that did not appear to focus on the management of frontal sinus fractures were deemed nonrelevant. Abstracts were eliminated if they did not address the target question or did not contain patient data. Articles were included if they reported patients with FSOT or posterior table fractures managed with sinus preservation. Sinus preservation included all fractures managed by observation, endoscopic or open reduction of the anterior and/or posterior table, and ORIF of the anterior table. Frontal sinus fractures that were managed by obliteration, osteoneogenesis, ablation, or cranialization did not meet the definition of sinus preservation. If the surgical management could not be determined based on fracture classification, the study was not included for review. Citations, abstracts, and articles were independently reviewed by two reviewers (K.C. and D.P.). Once potential full articles were identified, they were reviewed by a third reviewer (J.R.). All selected articles were published in peer-reviewed journals and contained new patient data on management of frontal sinus fractures.
Frontal Sinus Fracture Algorithm Synthesis
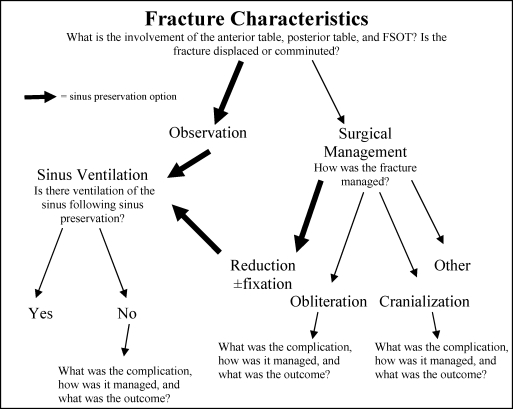
In our proposed algorithm, the fracture was initially classified by anterior and/or posterior table involvement, involvement of the FSOT, and degree of table displacement or comminution. Management was further stratified into observation versus surgical management. For patients managed surgically, the type of operation performed was listed under the surgical management heading. Fractures managed by observation or reduction (with or without fixation) without obliteration or cranialization were classified as sinus preservation. For sinus preservation to be considered a viable alternative to more traditional management, data should be collected regarding complications that can affect sinus ventilation. Therefore, short-term and long-term complications following sinus preservation such as persistent CSF leak, recurrent sinusitis, and mucocele formation were recorded. If spontaneous sinus ventilation was not achieved, then the complication affecting sinus ventilation was recorded, as well as management of the complication and eventual outcome. Similarly, complications following the traditional sinus obliteration or cranialization protocol were recorded in the algorithm (Fig. 1).
Figure 1.
Proposed algorithm for reporting management of frontal sinus fractures. FSOT, frontal sinus outflow tract.
RESULTS
Article Selection
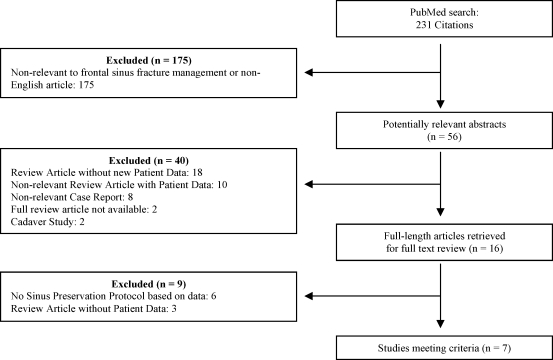
The initial search of the PubMed database yielded 231 citations. There were 175 citations that were eliminated, leaving a total of 56 abstracts for review after the primary search. Eliminated abstracts included 18 review articles that did not include new patient data, 18 articles that were not relevant to our clinical question, and two cadaveric studies. There were 16 articles that merited full-text review. Six studies were eliminated after full review because inclusion criterion for sinus preservation was either not met or could not be determined from the results presented in the studies. Three articles were eliminated because they were not primary studies. A total of seven articles met full criteria (Fig. 2). Six of the articles were retrospective case series1,3,6,9,10,11and one article was a prospective study.7
Figure 2.
Selection of articles for inclusion in review.
Fracture Classification
In the seven studies included for full review, there were a total of 515 patients with frontal sinus fractures. There were 242 isolated anterior table fractures, 261 combined anterior/posterior table fractures, and 12 isolated posterior table fractures. Suspicion for involvement of the FSOT was generally determined by preoperative computed tomography (CT) imaging using traditional axial and coronal CT scan images. In four of the studies, suspected involvement of the FSOT was specifically reported.1,6,10,11 In those four studies, there were 74 isolated anterior table fractures that did not involve the FSOT and 24 isolated anterior table fractures involving the FSOT. Only two studies classified combined anterior/posterior table fractures into those with and without suspected FSOT involvement.6,10 In the combined anterior/posterior table fractures, 71 fractures did not have suspected FSOT involvement and 62 fractures had suspected FSOT involvement. Although Chen et al classified combined anterior/posterior table fractures into those with and without suspected FSOT involvement, their study did not separately report the management of combined fractures with suspected FSOT involvement compared with combined fractures without suspected FSOT involvement.6 The three studies with patients found to have isolated posterior table fractures did not specifically note the status of the FSOT in those individuals. If data could not be extracted from individual studies, it was listed as not available (Table 1).
Table 1.
Frontal Sinus Fracture Classification
| Study | n | Isolated Anterior Table | Isolated Anterior Table − FSOT | Isolated Anterior Table + FSOT | Anterior/ Posterior Table | Anterior/ Posterior Table − FSOT | Anterior/ Posterior Table + FSOT | Isolated Posterior Table |
|---|---|---|---|---|---|---|---|---|
| Xie 200010 (1967–1997) | 150 | 64 | 52 | 12 | 77 | 43 | 34 | 9 |
| Bell 20071 (1995–2005) | 116 | 69 | n/a | n/a | 46 | n/a | n/a | 1 |
| Gossman 20069 (1990–2003) | 96 | 48 | n/a | n/a | 48 | n/a | n/a | 0 |
| Chen 20066 (1994–2002) | 78 | 22 | 19 | 3 | 56 | 28 | 28 | 0 |
| McRae 20085 (1995–2002) | 63 | 27 | n/a | n/a | 34 | n/a | n/a | 2 |
| Smith 20027 (1999–2001) | 7 | 7 | 0 | 7 | 0 | 0 | 0 | 0 |
| Steiger 200611 (2003–2005) | 5 | 5 | 3 | 2 | 0 | 0 | 0 | 0 |
| Total | 515 | 242 | 74 | 24 | 261 | 71 | 62 | 12 |
n/a, not available.
Management
The management of fractures was stratified into observation and surgical management, including reduction with or without fixation of the anterior table, obliteration, and cranialization. A total of 199 patients were observed and did not undergo surgical management. Three patients underwent reduction without fixation of the anterior table, and 148 patients underwent ORIF of the anterior table. In total, there were 350 patients who had preservation of the sinus. Seventy-seven patients had the frontal sinus obliterated, and 75 had the frontal sinus cranialized (Table 2).
Table 2.
Management of Frontal Sinus Fractures
| Study | n | Observation | Surgery | Reduction ± Fixation of Anterior Table | Sinus Preservation Total | Obliteration | Cranialization |
|---|---|---|---|---|---|---|---|
| Xie 200010 (1967–1997) | 150 | 56 | 94 | 27 | 83 | 39 | 15 |
| Bell 20071 (1995–2005) | 116 | 66 | 50 | 29 | 95 | 5 | 16 |
| Gossman 20069 (1990–2003) | 96 | 48 | 48 | 29 | 77 | 8 | 11 |
| Chen 20066 (1994–2002) | 78 | 6 | 72 | 40 | 46 | 18 | 14 |
| McRae 20085 (1995–2002) | 63 | 23 | 40 | 14 | 37 | 7 | 19 |
| Smith 20027 (1999–2001) | 7 | 0 | 7 | 7 | 7 | 0 | 0 |
| Steiger 200611 (2003–2005) | 5 | 0 | 5 | 5 | 5 | 0 | 0 |
| Total | 515 | 199 | 316 | 151 | 350 | 77 | 75 |
Complications
There were multiple reporting systems for complications among the included studies. The most commonly reported complications included mucocele, sinusitis, meningitis, osteomyelitis, wound infection, encephalocele, CSF leak, chronic pain, cosmetic deformity, and death. Table 3 illustrates the complications from each study based on management strategy.
Table 3.
Complications
| Complications | |||
|---|---|---|---|
| Study | Management (Total Patients) | Type | n |
| Bell 20071 | Preservation (95) | Mucocele | 1 |
| CSF leak | 1 | ||
| Obliteration (5) | Mucocele | 1 | |
| Cosmesis | 1 | ||
| Cranialization (16) | Brain abscess | 1 | |
| Osteomyelitis | 1 | ||
| Cosmesis | 1 | ||
| Unclassified | Meningitis | 1 | |
| Death | 6 | ||
| Chen 20066 | Preservation (46) | Sinusitis | 1 |
| Obliteration (18) | Mucocele | 1 | |
| Cranialization (14) | Meningitis | 1 | |
| Unclassified | Wound infection | 4 | |
| CSF leak | 5 | ||
| Cosmesis | 17 | ||
| Gossman 20069 | Preservation (74) | Sinusitis | 3 |
| Chronic pain | 5 | ||
| Cosmesis | 2 | ||
| Obliteration (8) | Sinusitis | 1 | |
| Wound infection | 1 | ||
| Cranialization (11) | Wound infection | 1 | |
| CSF leak | 2 | ||
| Chronic pain | 2 | ||
| Unclassified | Death | 3 | |
| McRae 20085 | Preservation (38) | CSF leak | 1 |
| Obliteration (7) | None | ||
| Cranialization (18) | CSF leak | 2 | |
| Unclassified | Mucocele | 1 | |
| Sinusitis | 1 | ||
| Meningitis | 1 | ||
| Cosmesis | 4 | ||
| Death | 2 | ||
| Smith 20027 | Preservation (7) | Sinusitis | 2 |
| Obliteration (0) | None | ||
| Cranialization (0) | None | ||
| Steiger 200611 | Preservation (5) | None | |
| Obliteration (0) | None | ||
| Cranialization (0) | None | ||
| Xie 200010 | Preservation (83) | Mucocele | 7 |
| Meningitis | 2 | ||
| Encephalocele | 1 | ||
| Wound infection | 1 | ||
| Empyema | 1 | ||
| Obliteration (39) | Mucocele | 3 | |
| Cranialization (15) | None | ||
CSF, cerebrospinal fluid.
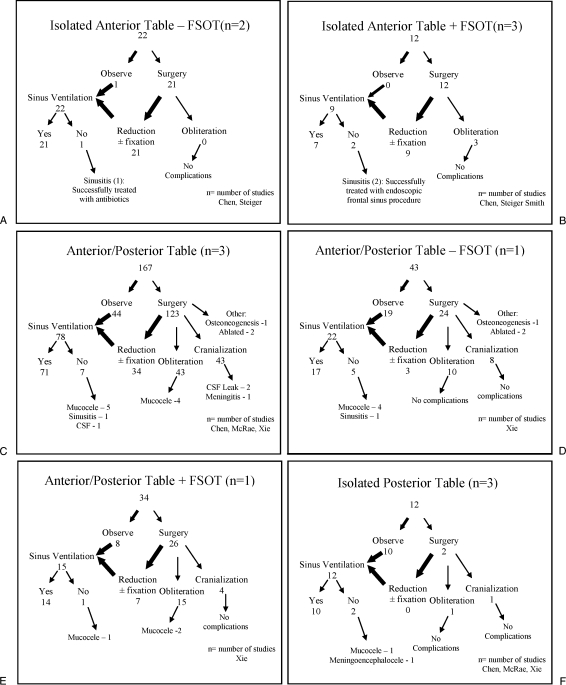
Algorithm Application
The previously described frontal sinus fracture algorithm was applied to the study cohort. Studies were included in the respective flow diagram when all of the data for fracture classification, management, and outcomes were available or able to be extrapolated from the article. Management of complications was not always reported in the studies. The pooled number of patients and lead author of the studies in each flow diagram are listed in Figs. 3A to 3F.
Figure 3.
(A–F) Fracture classification and management strategy using proposed algorithm for included studies. CSF, cerebrospinal fluid; FSOT, sinus outflow tract.
DISCUSSION
The goals of frontal sinus fracture repair include restoration of frontal contour and cosmesis, establishment of normal sinus ventilation, isolation of intracranial contents, and most importantly, prevention of the numerous complications that can arise in the setting of frontal sinus injury.10,12 In this report, we have reviewed the literature since 1995, which we have arbitrarily designated as the beginnings of the modern era of endoscopic frontal sinus surgery. We have identified numerous cases of frontal sinus preservation in the setting of frontal sinus fracture management that may have traditionally been obliterated or cranialized. The data presented in the studies were not uniformly reported; therefore, pooling of the data for a meta-analysis could not be performed.
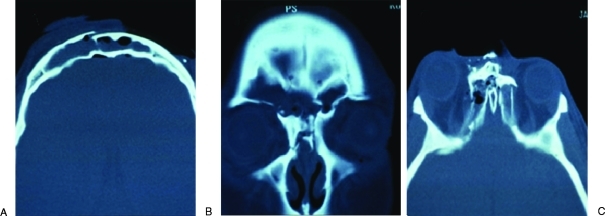
Throughout all surgical fields, less invasive approaches have been employed to decrease the potential morbidity of traditional open procedures. Endoscopic management of sinus disease exemplifies this evolution. With the widespread acceptance of endoscopic management of sinus disease, endoscopic techniques directed at the frontal sinus have gained acceptance. Procedures such as the Draf type III or frontal sinus “drillout” have been well established and accepted.13 These techniques have been proven effective in management of frontal sinus mucoceles and chronic sinusitis, both known complications frontal sinus fractures.14 These procedures can also be used in conjunction with frontal sinus trephinations to address both anterior table fractures as well as complications that arise from frontal sinus fractures.11,15 These techniques have also been effectively used to manage complications from failed attempts at frontal sinus obliteration.16 The establishment of these procedures and their application for management of frontal sinus fractures allows for more conservative management and sinus preservation in these patients. Figures 4 to 6 outline the case of a 22-year-old woman involved in a motor vehicle collision who sustained an open, displaced anterior table fracture with associated naso-orbital ethmoid fracture. She had successful ventilation of her frontal sinus following endoscopic unilateral extended frontal sinusotomy (Draf type III).
Figure 4.
(A) Preoperative axial computed tomography (CT) demonstrating a displaced fracture of the anterior table of the frontal sinus. (B) Preoperative coronal CT demonstrating extensive fractures in the region of the frontal sinus outflow tract (FSOT). (C) Preoperative axial CT demonstrating associated naso-orbital ethmoid fracture and likely FSOT.
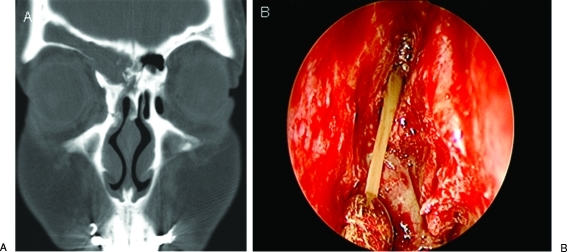
Figure 5.
Patient at 3 months postoperatively with persistent frontal sinus outflow tract obstruction even with maximal medical therapy. (A) Coronal computed tomography demonstrating residual right frontal sinus opacification after open reduction and internal fixation of anterior frontal sinus table and naso-orbital ethmoid fracture repair with sinus preservation. (B) Intraoperative nasal view of purulent discharge being suctioned from the nonventilated frontal sinus during the endoscopic frontal sinus surgery.
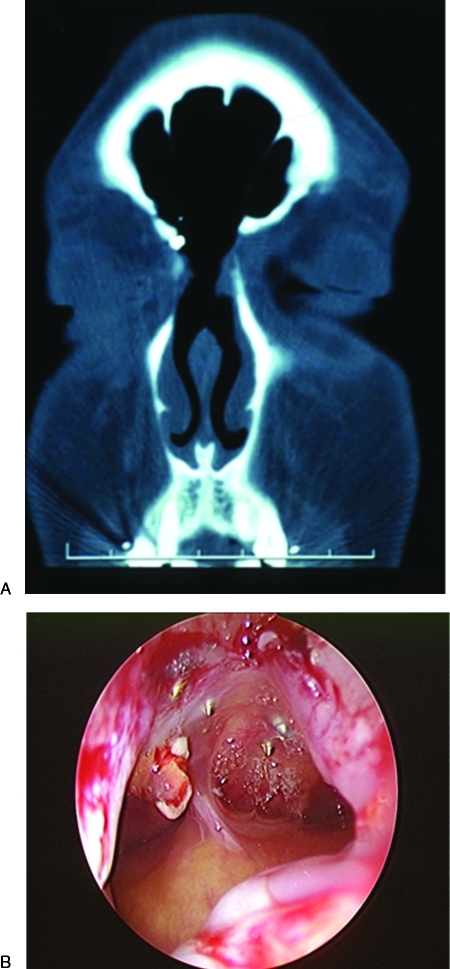
Figure 6.
(A) Postoperative coronal computed tomography scan after unilateral extended frontal sinusotomy (Draf type III) demonstrating frontal sinus ventilation. (B) Endoscopic examination in the office at 6 months demonstrating patency of the open reduction and internal fixation. The screws used for fixation of the anterior table fracture are seen penetrating the wall of the frontal sinus.
Three of the studies in our review employed or mentioned endoscopic techniques as options for management of the FSOT.7,9,11 In their prospective series, Smith et al suggested sinus preservation in patients with displaced anterior table fractures with suspected injury to the FSOT who are likely to follow up and be compliant with subsequent care.7 Seven patients were managed with ORIF of the anterior table and a 4-week course of antibiotics. Serial postoperative scans were performed, and two patients with persistent frontal sinusitis were successfully treated with endoscopic management of the FSOT. In the Steiger study, a frontal sinusotomy or endoscopic-assisted trephination was initially used to gain access to the frontal sinus fracture and the FSOT.11 Gossman and colleagues did not specifically report endoscopic management, but they did support its use in managing the FSOT after ORIF of the anterior table.9 Recently, Hueman and Eller described a case of an anterior frontal sinus fracture involving the FSOT that was successfully managed using a balloon catheter to reduce the fracture.17
Traditionally, it was recommended that patients undergo immediate cranialization of the frontal sinus if the fractured posterior table was displaced greater than one table width, due to the high suspicion of intracranial or dural injury or fear of possible long-term intracranial infection.2 However, Chen et al found that the degree of posterior table displacement did not correlate with CSF leak resolution. They recommended an observation period of 4 to 7 days for patients with closed frontal sinus fractures accompanied by CSF leak. If the CSF leak resolved, the patient would be managed with open reduction, internal fixation of the anterior table, and sinus preservation.6
Sinus preservation offers several advantages over traditional management with obliteration or cranialization. Patients with frontal sinus fractures often have multiple injuries, including serious intracranial injuries. Reduction of the anterior table with sinus preservation requires shorter operative time and exposure to anesthesia. In sinus obliteration, wide exposure is necessary to gain access to the sinus to effectively remove all sinus mucosa. This carries the risk of bone fragment devitalization and subsequent resorption.7 In addition, patients with extensively pneumatized frontal sinuses pose an even greater challenge in the acute traumatic setting when attempting to remove all of the sinus mucosa with a traditional obliteration or cranialization procedure.
Patients managed with sinus preservation or traditional management require long-term follow-up to identify complications that can occur years after the initial injury. Imaging studies of the frontal sinus in patients treated with sinus obliteration can be difficult to interpret. The appearance of fat and other materials used for obliteration of the sinus can vary on imaging, potentially posing a challenge to identify suppurative complications when they occur.18 Complications that arise in the setting of a preserved sinus would be more apparent on imaging studies and potentially identified sooner. In addition, the status of the frontal sinus can be evaluated in the clinic with endoscopic examination. Ultimately, the management of frontal sinus fractures should result in a “safe sinus.”1 There are not enough data available to determine if sinus preservation or traditional management most effectively achieves this goal.
There are several limitations to our study. We arbitrarily defined 1995 as the beginning of the endoscopic sinus surgery era and limited our search to articles published after this date. Our time frame may not be universally accepted as the beginning of the endoscopic sinus surgery era. In addition, articles published after 1995 did not exclusively include patient cohorts from 1995 to 2008. For example, Xie et al published a 30-year retrospective study with most of their patients treated before our definition of the endoscopic sinus surgery era.10 We elected to include this article in our analysis because it was a well-designed study with defined management strategies and the respective complications. They also included some patients managed by a sinus preservation strategy.
In the review of the literature, there were not many articles that specifically addressed our target question. This may be representative of the low numbers of frontal sinus fractures in general or continued management of frontal sinus fractures with obliteration and/or cranialization across most institutions. As more centers begin to consider the option of sinus preservation, the number of studies available for comparison and analysis will hopefully continue to grow.
In the seven articles included in our review, the complications that occurred in the patients with preserved sinuses did not significantly vary from those treated with traditional management. In evaluating outcomes of frontal sinus repair, complications that can occur many years after the initial injury must be considered. This is especially important in sinus preservation protocols, as the long-term safety profile has not been established yet. Therefore, accurate documentation of outcomes is necessary to determine the efficacy and safety of sinus preservation protocols.
The studies reviewed illustrate that sinus preservation in frontal sinus fractures is a viable treatment option in select patients. Based on data from previous studies at our center and our review of the literature, sinus preservation may be considered in patients with frontal sinus fractures and the following characteristics: (1) nondisplaced or minimally displaced fractures of the anterior wall, (2) nondisplaced or minimally displaced posterior wall fractures without significant intracranial injury or persistent CSF leak (traditionally cranialized), (3) displaced anterior wall fractures with suspected FSOT involvement (traditionally obliterated), (4) displaced anterior and minimally displaced posterior wall fractures without significant intracranial injury or persistent CSF leak (traditionally obliterated or cranialized). The role of sinus preservation management in other clinical scenarios remains unclear and unproven.1,5,6,7
Finally, to standardize classification and outcomes, we have introduced an algorithm, which incorporates fracture classification, management, and outcomes including sinus ventilation (Fig. 1). We have demonstrated the utility of this algorithm in presenting management strategies and ultimate outcomes of patients with frontal sinus fractures. Our hope is that this algorithm will allow for standardization of reporting patient outcomes in frontal sinus fracture repairs and allow for comparisons of outcomes across different institutions. If this system of reporting becomes more universally adopted, the safety profile of sinus preservation could be evaluated on a larger scale.
CONCLUSIONS
Sinus preservation appears to be a safe and effective management strategy for select frontal sinus fractures. The importance of preserving the frontal sinus appears to be gaining some acceptance in the literature. Several recent studies have proposed sinus preservation protocols using endoscopic management of the FSOT as a viable alternative to frontal sinus obliteration. As more centers begin incorporating sinus preservation protocols into management of frontal sinus fractures, more data will be available for comparative analysis. More transparent reporting of management strategies and longer-term follow-up are necessary to assess the safety and efficacy of sinus preservation protocols.
NOTES
Submitted for presentation at the Triological Society Annual Meeting at the Combined Otolaryngology Spring Meeting (COSM) May 28 to May 31, 2009.
References
- Bell R B, Dierks E J, Brar P, Potter J K, Potter B E. A protocol for the management of frontal sinus fractures emphasizing sinus preservation. J Oral Maxillofac Surg. 2007;65:825–839. doi: 10.1016/j.joms.2006.05.058. [DOI] [PubMed] [Google Scholar]
- Rohrich R J, Hollier L H. Management of frontal sinus fractures. Changing concepts. Clin Plast Surg. 1992;19:219–232. [PubMed] [Google Scholar]
- McRae M, Momeni R, Narayan D. Frontal sinus fractures: a review of trends, diagnosis, treatment, and outcomes at a level 1 trauma center in Connecticut. Conn Med. 2008;72:133–138. [PubMed] [Google Scholar]
- Tiwari P, Higuera S, Thornton J, Hollier L H. The management of frontal sinus fractures. J Oral Maxillofac Surg. 2005;63:1354–1360. doi: 10.1016/j.joms.2005.05.308. [DOI] [PubMed] [Google Scholar]
- Manolidis S, Hollier L H., Jr Management of frontal sinus fractures. Plast Reconstr Surg. 2007;120(7 Suppl 2):32S–48S. doi: 10.1097/01.prs.0000260732.58496.1b. [DOI] [PubMed] [Google Scholar]
- Chen K T, Chen C T, Mardini S, Tsay P K, Chen Y R. Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast Reconstr Surg. 2006;118:457–468. doi: 10.1097/01.prs.0000227738.42077.2d. [DOI] [PubMed] [Google Scholar]
- Smith T L, Han J K, Loehrl T A, Rhee J S. Endoscopic management of the frontal recess in frontal sinus fractures: a shift in the paradigm? Laryngoscope. 2002;112:784–790. doi: 10.1097/00005537-200205000-00004. [DOI] [PubMed] [Google Scholar]
- Mueller R. Endoscopic treatment of facial fractures. Facial Plast Surg. 2008;24:78–91. doi: 10.1055/s-2008-1037452. [DOI] [PubMed] [Google Scholar]
- Gossman D G, Archer S M, Arosarena O. Management of frontal sinus fractures: a review of 96 cases. Laryngoscope. 2006;116:1357–1362. doi: 10.1097/01.mlg.0000226009.00145.85. [DOI] [PubMed] [Google Scholar]
- Xie C, Mehendale N, Barrett D, Bui C J, Metzinger S E. 30-year retrospective review of frontal sinus fractures: The Charity Hospital experience. J Craniomaxillofac Trauma. 2000;6:7–15. discussion 16–18. [PubMed] [Google Scholar]
- Steiger J D, Chiu A G, Francis D O, Palmer J N. Endoscopic-assisted reduction of anterior table frontal sinus fractures. Laryngoscope. 2006;116:1978–1981. doi: 10.1097/01.mlg.0000236508.50443.0d. [DOI] [PubMed] [Google Scholar]
- Gabrielli M F, Gabrielli M A, Hochuli-Vieira E, Pereira-Fillho V A. Immediate reconstruction of frontal sinus fractures: review of 26 cases. J Oral Maxillofac Surg. 2004;62:582–586. doi: 10.1016/j.joms.2003.08.026. [DOI] [PubMed] [Google Scholar]
- Weber R, Draf W, Kratzsch B, Hosemann W, Schaefer S D. Modern concepts of frontal sinus surgery. Laryngoscope. 2001;111:137–146. doi: 10.1097/00005537-200101000-00024. [DOI] [PubMed] [Google Scholar]
- Batra P S, Cannady S B, Lanza D C. Surgical outcomes of drillout procedures for complex frontal sinus pathology. Laryngoscope. 2007;117:927–931. doi: 10.1097/MLG.0b013e31803dd2ee. [DOI] [PubMed] [Google Scholar]
- Batra P S, Citardi M J, Lanza D C. Combined endoscopic trephination and endoscopic frontal sinusotomy for management of complex frontal sinus pathology. Am J Rhinol. 2005;19:435–441. [PubMed] [Google Scholar]
- Kanowitz S J, Batra P S, Citardi M J. Comprehensive management of failed frontal sinus obliteration. Am J Rhinol. 2008;22:263–270. doi: 10.2500/ajr.2008.22.3164. [DOI] [PubMed] [Google Scholar]
- Hueman K, Eller R. Reduction of anterior frontal sinus fracture involving the frontal outflow tract using balloon sinuplasty. Otolaryngol Head Neck Surg. 2008;139:170–171. doi: 10.1016/j.otohns.2008.02.003. [DOI] [PubMed] [Google Scholar]
- Weber R, Draf W, Keerl R, et al. Magnetic resonance imaging following fat obliteration of the frontal sinus. Neuroradiology. 2002;44:52–58. doi: 10.1007/s002340100635. [DOI] [PubMed] [Google Scholar]