Abstract
Objective
The objective of the study was to determine whether physician–scientists in psychiatry in Canada are in decline, as was reported for medicine overall during the 1990s in the United States.
Design
Federal databases were searched to study grant applications in the area of mental health submitted by physician–scientists compared with PhD–scientists for the period 1985–2001. A survey of Canadian Residency Training Program Directors was carried out for the graduating class of 2000.
Setting
The Canadian publicly funded university system.
Participants
Applicants to the Medical Research Council of Canada and its successor, the Canadian Institutes of Health Research, for operating grant support and Residency Training Program Directors.
Interventions
None.
Outcome measures
Comparison over time between MD and PhD applicants regarding the number of grant applications submitted, the proportion of applications funded and the number of new applications submitted, with separation of applications submitted to a predominantly “biomedical” peer review committee and to a predominantly “clinical research” peer review committee. The survey obtained information about a number of variables related to research training.
Results
The situation for physician–scientists in psychiatry in Canada appeared remarkably similar to general findings in US studies. Relative to PhD applicants, fewer grant proposals were being made by physicians (paired t16 = 7.08, p < 0.001) and, in consequence, fewer proposals were funded. The proportion of proposals funded was similar for MD and PhD applicants (paired t16 = 0.27, p = 0.79). Grant applications made to the predominantly biomedical committee were more likely to be funded than applications to the committee with an orientation toward clinical research (paired t7 = 5.53, p < 0.001). Applications by PhD–scientists to the biomedical committee showed the largest increase over time and were the most successful. From the survey of graduating classes, close to one-third of residents had authored or co-authored a publication during residency. Only 7% were proceeding to research fellowship training. The remuneration available for fellowship training was about one-third of what graduating classmates could expect to earn in the first year of practice.
Conclusions
Quantitative data indicate that physician–scientists in psychiatry in Canada are experiencing the same pressures and challenges as physician–scientists in the United States. A plan of action tailored to the needs of the psychiatric community in Canada needs to be developed.
Medical subject headings: education, medical; internship and residency; policy making; research
Abstract
Objectif
L'étude visait à déterminer si les médecins chercheurs en psychiatrie au Canada sont à la baisse comme on l'a signalé dans le cas de la médecine dans son ensemble au cours des années 1990 aux États-Unis.
Conception
On a effectué des recherches dans des bases de données fédérales afin d'étudier les demandes de subventions dans le domaine de la santé mentale présentées par des médecins chercheurs comparativement à celles qu'ont présentées des chercheurs titulaires d'un doctorat pendant la période de 1985 à 2001. On a effectué un sondage auprès des directeurs de programmes canadiens de formation en résidence au sujet de la promotion de 2000.
Contexte
Le réseau universitaire canadien financé par le secteur public.
Participants
Auteurs de demandes de subvention de fonctionnement présentées au Conseil de recherches médicales du Canada de l'époque et aux Instituts de recherche en santé du Canada, et directeurs de programmes de formation en résidence.
Interventions
Aucune.
Mesures de résultats
Comparaison chronologique entre les candidats médecins et titulaires d'un doctorat quant au nombre de demandes présentées, aux proportions des demandes de subvention acceptées et au nombre de nouvelles demandes présentées, et séparation des demandes présentées à un comité d'examen critique par des pairs à prédominance «biomédicale» et à un comité axé avant tout sur la «recherche clinique». Le sondage a produit des renseignements sur de nombreuses variables reliées à la formation en recherche.
Résultats
La situation des médecins chercheurs en psychiatrie au Canada semblait remarquablement semblable aux constations générales tirées des études américaines. Les médecins ont présenté moins de demandes de subventions que les candidats titulaires d'un doctorat (t16 apparié = 7,08, p < 0,001) et, par conséquent, le nombre de propositions subventionnées a été moins élevé. Le pourcentage des propositions subventionnées se ressemblait chez les médecins et les titulaires de doctorat (t16 apparié = 0,27, p = 0,79). Les demandes de subventions présentées au comité à prédominance biomédicale étaient plus susceptibles d'être acceptées que les demandes présentées au comité axé sur la recherche clinique (t7 apparié = 5,53, p < 0,001). Les demandes présentées au comité biomédical par des chercheurs titulaires d'un doctorat ont augmenté le plus au fil du temps et ont connu le plus de succès. Le sondage sur les promotions permet de conclure que presque un tiers des résidents avaient été l'auteur ou le co-auteur d'une publication au cours de leur résidence. Seulement 7 % poursuivaient ensuite une formation supérieure en recherche. La rémunération disponible pour une formation supérieure s'établissait au tiers environ de ce que les membres de la même promotion pouvaient s'attendre à gagner au cours de leur première année d'exercice.
Conclusion
Les données quantitatives indiquent que les médecins chercheurs en psychiatrie au Canada connaissent les mêmes pressions et doivent relever les mêmes défis que leurs homologues des États-Unis. Il faut élaborer un plan d'action axé sur les besoins des milieux de la psychiatrie au Canada.
Introduction
The role of physicians in medical research, and the place of clinical research in medicine, is in what some consider to be a very tenuous position. Physician–scientists are described as “endangered and essential,”1 and academic medicine is said to be in “an embattled state.”2 In this context, one of us (W.G.H.) was asked by the Association of Chairs of Psychiatry of Canada to prepare a report on the state of clinician–scientists in Departments of Psychiatry in Canada.
For the purposes of the report, we examined the role of physician–scientists compared with PhD–scientists. This approach was taken for several reasons, mostly pragmatic. Most of the available literature compares researchers with MDs to those with PhDs. Statistics on grant applications allow the comparison of MD applicants with PhD applicants. Clinical psychologists and other clinicians are important contributors to psychiatric research, but the data available for the present study did not separate clinician–PhD research from basic science–PhD research. However, through analysis of different grant-awarding committees, we attempted to obtain results allowing for the comparison of clinical with basic research in mental health. For the purposes of the present report, the term “clinician–scientist” is therefore used to refer to medically trained clinicians. The important role of nonmedical clinicians in psychiatric research deserves consideration elsewhere.
Clinician–scientists: definitions and observations in the United States
The “handshake test” (direct contact between patient and investigator) has been used as the criterion for defining clinical research.3 Another definition restricts the concept to research of a translational nature, moving from laboratory bench to bedside. A broader definition includes clinical trials and epidemiologic, health services and behavioural studies.2 Disease-oriented or basic research that can be carried out in cell lines or animal models is excluded by some;4 however, others argue that clinical training brings a different perspective to even these research strategies.5
US data for medicine as a whole are available and were recently summarized.1,2 These observations indicated a significant decline in the proportion of MD-trained compared with PhD-trained investigators applying for National Institutes of Health (NIH) operating grants, a very negative trend in the number of first-time applications from MDs and a declining proportion of MDs entering research fellowship training positions. Finally, a substantial decline among medical students in interest in a career in research was described.
Psychiatry compared with other medical specialties
In the 1980s, 34% of US faculty in a range of medical and surgical specialties had postdoctoral research training compared with only 12% in departments of psychiatry.6 In consequence, although two-thirds of faculty in other departments participated in research, only one-half of faculty in psychiatry appeared to have research involvement. In terms of federal grant funding, the percentages were 13% overall versus only 5% in psychiatry. The results of a subsequent study with a different methodology were similar,7 and more recent data have indicated that psychiatry continues to lag behind other branches of medicine.8 Lack of research involvement by faculty members contributes to a shortage of mentors, which serves to perpetuate these difficulties. Training in research for at least 24 months following specialty training in psychiatry was a threshold required to predict more involvement in research as a career choice.9
Canadian perspectives on clinician–scientists
Overall, the Canadian situation appears similar to that in the United States. The proportion of physicians holding Medical Research Council of Canada (MRC) grants declined by one-third from 1986 to 1996.10 Psychiatry in Canada also shows parallels with the United States. In 1987, at the University of Toronto, 10% of faculty in the Department of Psychiatry held peer- reviewed grants; of psychiatrists within the department, this was 9%.11,12 In 1996, a survey of training and productivity in Canadian departments of psychiatry was published.13,14 Research was defined as “systematic study performed with the objective of developing knowledge, which usually leads to publication and which may be the basis for funding support.”13,14 Of all MDs on faculty, 48% reported no research involvement and 41%, limited involvement (less than 20% of their time). For full-time MD faculty, only 24% reported spending more than 20% of their time doing research. The report then defined researchers as faculty who spent more than 20% of their time in research, had authored or co-authored 1 article within the past 2 years and had research space assigned or external funding. Of all MD faculty, 16% met these criteria; and of full-time MDs, only 29% could be described as researchers even by these very broad criteria. This was in contrast with full-time PhD members of these departments, for whom 82% satisfied these criteria. In this study, factors related to level of involvement of faculty in research were as follows:
· research experience during medical school
· availability of mentoring
· gender (women were less involved than men)
Factors unrelated to level of research involvement were as follows:
· medical or residency training abroad; however, medical and residency training abroad was positively related to research involvement, suggesting the importance of being able to recruit from outside Canada
· subspecialty training
In a survey of graduating residents in 1975, Leichner identified definite interest in full-time research in 8.9%, with definite interest in part-time research in 29%.15,16 In a 1980 study, definite interest in a career related to research was described by 4%,17 and by 1985 the combined definite interest in full-time or part-time research had declined to 10%.
Concern about the state of physician–scientists is not new.18,19 For the present report, we reviewed a subset of operating-grant applications to the MRC from 1985– 1999 and its successor, the Canadian Institutes of Health Research (CIHR), from 2000–2001. From 1985–1993, operating grants related to psychiatry and mental health were reviewed by 1 committee, Behavioural Sciences (BS). From 1994–2001, due to the increase in the number of grant applications submitted, 2 committees reviewed grants in this area. The Behavioural Sciences A (BSA) committee reviewed grants in the biomedical category, including studies of animal models and of brain mechanisms in healthy human subjects. The Behavioural Sciences B (BSB) committee reviewed grants in the clinical research category, including studies of subjects with mental disorders. There are other grant review committees in the MRC/CIHR that may have reviewed grants related to psychiatric disorders (such as the Clinical Trials and Neurosciences Committees). It was not feasible to do an all-inclusive review, because other committees have mandates that are not restricted to mental health. A brief survey of postgraduate training programs in Departments of Psychiatry in Canada was also carried out.
Methods
Survey of grant applications and funding from the MRC/CIHR
The database of operating-grant applications submitted to MRC/CIHR was used to determine, on a year-by-year basis, the number of grant applications submitted to the BS/BSA/BSB committees. The database also contains information concerning the degree(s) held by the principal investigator. For this purpose, we grouped applicants as holding an MD, an MD and a PhD, or a PhD (specific degree equivalents used in the search appear in Appendix 1). A limited number of comparisons of MD with MD/PhD applications were made to investigate the possible role of formal postgraduate training in research. For the purposes of most comparisons, we grouped MD and MD/PhD applicants for comparison with PhD applicants.
In addition to the number of grant applications submitted, we recorded the number of grants awarded. The number of first-time applications was also determined. The database extends back to 1985 only, so reapplications may be identified as first-time applications for those who held a grant before 1985. For this reason, we considered 1990–2001 to be the sampling frame for this analysis.
As an approximation, grant applications submitted to the BSA committee could be considered biomedical research and grant applications to the BSB committee, clinical research in orientation. Comparison of the number of grants between committees is of limited value, however, because equalizing the workload of the committees did play a role in assignment by the MRC/CIHR. We compared the proportion of MD with PhD applicants within each committee. Our assumption was that PhD applicants to BSA would probably represent the best measure of biomedical research grants, and PhD or MD applications to BSB would reflect the clinical research grants.
Survey of Canadian Postgraduate Training Programs
We surveyed the Directors of Postgraduate Training Programs in Departments of Psychiatry in Canada concerning the graduating class of 2000. We asked for:
· the number of residents proceeding to fellowship training
· the number of residents proceeding to research fellowship training
· the number of residents listed as an author on a published paper
· the number of residents being offered faculty positions
· the remuneration offered residents and fellows
Results
Survey of grant applications and funding from the MRC/CIHR
Consistently more grant applications were submitted by MDs than by MD/PhDs (paired t16 = 7.08, p < 0.001); however, patterns of change over time appeared to be similar. There were no significant differences in the percentage of successful applications between MD and MD/PhD applicants. For purposes of comparison with PhD applications, MD and MD/PhD applicants were pooled.
Consistently more applications were submitted by PhD applicants than by the pooled MD group (paired t16 = 8.87, p < 0.001). As seen in Fig. 1, the slope of the increase in applications over time in the PhD group (6.6/yr) was about double that in the pooled MD group (3.0/yr). The same pattern is apparent in the number of funded grants. There was no statistically significant difference in the proportion of successful applications between PhD and pooled MD applicants (paired t16 = 0.27, p = 0.79) (Fig. 2).
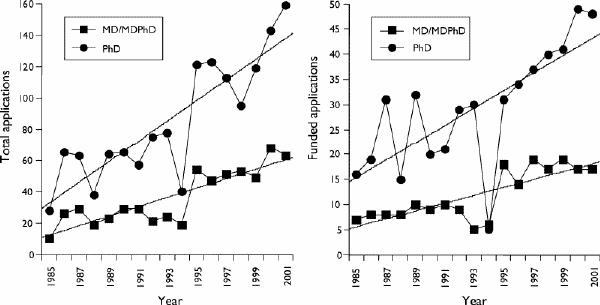
Fig. 1: Total (left panel) and funded (right panel) applications by PhD and MD/MD–PhD applicants from 1985 to 2001. The slope of the increase in applications from PhD candidates was steeper than that of the combined MD/MD–PhD applicants. Note that 1994 represented the last year with 1 yearly competition, subsequently competitions were twice per year. The number of grants submitted and funded in 1994 was therefore lower than expected compared with previous years, and the values for 1995 were probably slightly higher than expected compared with subsequent years.
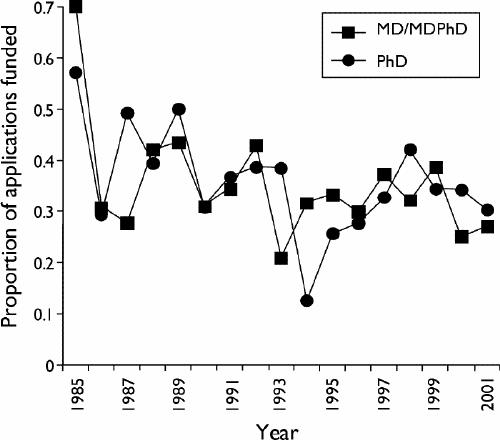
Fig. 2: Proportion of submitted applications that were funded, separated by PhD and MD/MD–PhD groupings. The quality of applications and likelihood of funding did not differ between the groups.
The number of first-time applications did not appear to show consistent changes over time for either the PhD or pooled MD groups.
Applications to BSA and BSB for the period 1995–2001 are illustrated in Fig. 3. The trend of increased grant applications and funded grants for PhD applicants identified previously appeared to be related primarily to biomedical applications submitted to the BSA committee. Submissions from pooled MD applicants showed little change in either committee.
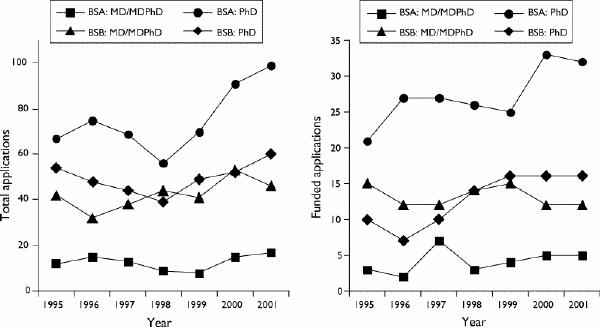
Fig. 3: Total (left panel) and funded (right panel) applications to 2 MRC/CIHR peer-review committees, Behavioural Sciences A (BSA) and Behavioural Sciences B (BSB). Although not an absolute distinction, BSA tended to review biomedical applications involving studies on animals or fundamental processes in humans. BSB reviewed clinical applications involving studies on humans or directly related to disease mechanisms. Over time, more applications were submitted to BSA by PhD applicants, and these were more likely to be funded than other types of applications regardless of the degree held by the applicant. Note: MRC = Medical Research Council of Canada; CIHR = Canadian Institutes of Health Research.
Within the 2 committees, PhD and pooled MD applicants were equally likely to be successful (BSA paired t7 = 0.59, p = 0.58; BSB paired t7 = 1.60, p = 0.15). However, it was of interest that the overall rate of success in BSA (mean 34.4%, standard deviation [SD] 7.2%) was significantly greater than in BSB (mean 26.8%, SD 5.7%) (paired t7 = 5.53, p < 0.001).
Survey of Canadian Postgraduate Training Programs
Responses were obtained from Directors of Postgraduate Training in 14 of 16 Canadian Departments of Psychiatry. The total number of graduating residents represented in this sample was 97. Of this group, 39 (40%) were continuing training in a fellowship; however, only 7 (7%) were proceeding to a research fellowship. Twenty-nine (30%) individuals had authored or were co-authors on a published paper during residency, which provides an objective marker for interest and experience in research during residency training. Only 6 graduates applied for CIHR fellowships, and 7 applied for provincial fellowships (probably an overlapping group). We asked how many residents were being offered academic faculty positions (geographic full-time) directly following graduation. The number was 12, probably exceeding the number applying for fellowship training. The salary range for final-year residents during 2000 was $44 662–$56 820. The CIHR fellowship stipend that year was $45 000, and the remuneration for the first year of the CIHR Clinician–Scientist Award was $48 000. As a comparison, in British Columbia psychiatrists may choose to work sessionally (at a fixed rate of remuneration) in a hospital or community care team setting and earn in excess of $150 000 yearly, beginning immediately after graduation.
Discussion
The results of the present study indicate that trends concerning physician–scientists in Canadian psychiatry were very similar to those reported for all physician–scientists in the United States.1,2 Fewer applications than expected were made for operating-grant support from physician–scientists, in the presence of increased numbers of available grants. The quality of grant applications submitted did not appear to be at issue: physician–scientists' applications were as likely to be successful as PhD–scientists' applications. However, of concern for clinical research, increasing numbers of grant applications appeared to be directed toward more basic biomedical questions, at least as assessed by applications by PhD–scientists to the CIHR committee with this orientation (BSA). It is to the credit of these applicants that their proposals were of very high quality and were more likely to be funded than clinical grant applications.
The data presented here are largely descriptive, and their main value lies in documenting the problem. The survey of residency programs indicated that close to one-third of residents participated in research or scholarship during training, as evidenced by contributing to a publication. The potential to train more physician- scientists appears to be present. A brief summary of several issues related to problems in training clinician–scientists follows. This is far from comprehensive, and discussion within the academic psychiatry community will be needed before action can be taken.
Obstacles to training clinician–scientists
A report from the US Institute of Medicine identified the following obstacles to faculty participation in research:
· insufficient formal training of faculty in research methodology
· lack of mentors
· student debt
· emphasis on cellular/molecular research over patient-oriented research
Although many advocate incorporating research training into residency programs,20 there is also general agreement that a requirement for a successful career in research is a 2–3 year fellowship that emphasizes research.21 Important features of a clinician–scientist training program could include formal training in evidence-based medicine, biostatistics and epidemiology, research design and management, ethical conduct and grant application writing. Beyond this core, project-specific training would also be necessary. A significant role for obtaining MPH or PhD degrees as part of this training is suggested by some,22 as is spending at least 60% of time in course work and research training studies. Costs are likely to be high, as much as $70 000–$80 000 per fellow is estimated in US settings.
The importance of mentors in research training was universally stressed. Components of this role may include clinical knowledge, methodology and general career planning. A single individual may not be the source of all of these aspects of mentoring for clinician–scientist trainees. At the present time, with the concentration of research faculty in a limited number of institutions, access to physician–scientist mentors is restricted considerably. A further consideration when trying to provide mentoring is that women may have differing needs regarding training and early career development compared with men.23,24,25
Debt may be of less concern at present in Canada compared with the United States; however, it is likely to play a larger role in the near future. Senior resident salaries in Canada in 2000 ranged from $44 662/yr to $56 820/yr. Due to the nature of the Canadian system, income immediately following certification can easily increase 3-fold. In contrast, the CIHR stipend for a clinically trained postgraduate fellow was $45 000/yr. This stipend requires that 75% of the fellow's time be spent on research, and compensation for clinical service outside of this is permitted according to the policies of the sponsoring institution. For a phase I clinician–scientist, the salary from CIHR was $48 000/yr.
Clearly, there is increasing competition for a shrinking pool of individuals with an orientation toward research careers. However, establishing a dichotomy between cell/molecular and clinical research has the potential to be counterproductive, when the more fundamental issue is the recruitment of physicians in general to research careers.
Clinical research and faculty
The importance of department heads in the research activities of faculty was stressed in several papers.12,26 Specific note was made of the need to lead by example, to establish hiring policies requiring research fellowship training and to create a training environment where mentoring of residents is feasible. It has been suggested that establishing clinical investigation units may be of considerable importance.11 Protected time for research must be available. A US study noted that for every 10 hours per week of clinical work, the odds of having grant support for research decreased 23%. Garfinkel et al11 suggested that 12–15 hours per week spent performing clinical work and supervising residents (while on a clinical investigation unit) was an appropriate amount of clinical responsibility.
In the United States, significant changes have been made to address some of these problems in order to reverse the downward trends in training clinician–scientists and to improve clinical research in general.2,27,28 Steps have been taken to improve this situation in clinical research as a whole in Canada by the CIHR,22 and the current draft version of the CIHR report on clinician–scientists is replete with 110 recommendations. Nathan29 provided a most interesting commentary on the history of careers in clinical research from the US perspective. The role of clinicians in research, emphasis on basic versus clinical research, the changing culture of medical school admission policies and methods of instruction, grant funding mechanisms and criteria for academic success are all important factors. In considering how to move forward in psychiatry, a similar examination and discussion might be of particular value.
Acknowledgments
Dr. Honer is supported by a Scientist Award from the Canadian Institutes of Health Research.
Appendix 1.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. William G. Honer, Centre for Complex Disorders, VGH Research Pavilion, 211–828 W. 10th Ave., Vancouver BC V5Z 1L8; fax 604 875-4376; honer@interchg.ubc.ca
Submitted Apr. 23, 2003; Accepted Sept. 22, 2003
References
- 1.Rosenberg LE. Physician-scientists: endangered and essential. Science 1999;283:331-2. [DOI] [PubMed]
- 2.Nathan DG. Clinical research: perceptions, reality, and proposed solutions. JAMA 1998;280:1427-31. [DOI] [PubMed]
- 3.Goldstein JL, Brown MS. The clinical investigator: bewitched, bothered, and bewildered-but still beloved. J Clin Invest 1997; 99: 2803-12. [DOI] [PMC free article] [PubMed]
- 4.Nathan DG. Educational-debt relief for clinical investigators: a vote of confidence. N Engl J Med 2002;346:372-4. [DOI] [PubMed]
- 5.Ley TJ, Rosenberg LE. Removing career obstacles for young physician-scientists: loan-repayment programs. N Engl J Med 2002;346:368-72. [DOI] [PubMed]
- 6.Burke JD, Pincus HA, Pardes H. The clinician-researcher in psychiatry. Am J Psychiatry 1986;143:968-75. [DOI] [PubMed]
- 7.Pincus HA, Dial TH, Haviland MG. Research activities of full-time faculty in academic departments of psychiatry. Arch Gen Psychiatry 1993;50:657-64. [DOI] [PubMed]
- 8.Kupfer DJ, Hyman SE, Schatzberg AF, Pincus HA, Reynolds CF. Recruiting and retaining future generations of physician scientists in mental health. Arch Gen Psychiatry 2002;59:657-60. [DOI] [PubMed]
- 9.Pincus HA, Haviland MG, Dial TH, Hendryx MS. The relationship of postdoctoral research training to current research activities of faculty in academic departments of psychiatry. Am J Psychiatry 1995;152:596-601. [DOI] [PubMed]
- 10.Roy CC. Survival of clinican scientists. Clin Invest Med 1997; 20:283-8. [PubMed]
- 11.Garfinkel PE, Kennedy SH, Kaplan AS, Goldbloom DS. The clinician-investigator interface in psychiatry: II–the role of the clinical investigation unit. Can J Psychiatry 1989;34:364-8. [DOI] [PubMed]
- 12.Garfinkel PE, Goldbloom DS, Kaplan AS, Kennedy SH. The clinician-investigator interface in psychiatry I–values and problems. Can J Psychiatry 1989;34:361-3. [DOI] [PubMed]
- 13.El-Guebaly N, Atkinson M. Physician resource variables and their impact on the future pool of research expertise among psychiatrists: the Canadian Association of Professors of Psychiatry and Canadian Psychiatric Association Survey. Can J Psychiatry 1996;41:150-5. [DOI] [PubMed]
- 14.El-Guebaly N, Atkinson M. Research training and productivity among faculty: the Canadian Association of Professors of Psychiatry and the Canadian Psychiatric Association Survey. Can J Psychiatry 1996;41:144-9. [DOI] [PubMed]
- 15.Leichner PP. Present psychiatric postgraduate education and future professional trends in Canada: a survey of the opinions of fourth-year residents. Part I—Evaluation of psychiatric training for Canadian residents. Can J Psychiatry 1977;22:123-30. [DOI] [PubMed]
- 16.Leichner PP. Present psychiatric postgraduate education and future professional trends in Canada: a survey of the opinions of fourth-year residents. Part II—Future career intentions. Can J Psychiatry 1977;22:131-6. [DOI] [PubMed]
- 17.El-Guebaly N, Leichner P. Psychiatric manpower in Canada-the 1980 surveys. Part III: Future career intentions of psychiatric residents. Can J Psychiatry 1982;27:502-9. [DOI] [PubMed]
- 18.Gill GM. The end of the physician-scientist? Am Scholar 1984;53:353-68.
- 19.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med 1979;301:1254-9. [DOI] [PubMed]
- 20.Gibson K, Addington D, Brager N, Fauvel T, O'Malley K. Psychiatry training and research. Can J Psychiatry 1989;34:182-5. [DOI] [PubMed]
- 21.Ringel SP, Steiner JF, Vickery BG, Spencer SS. Training clinical researchers in neurology: we must do better. Neurology 2001; 57:388-92. [DOI] [PubMed]
- 22.Philipson E, Silverman M. Clinical research in a CIHR world. Clin Invest Med 2002;25:26-46. [PubMed]
- 23.Nonnemaker L. Women physicians in academic medicine. N Engl J Med 2000;342:399-405. [DOI] [PubMed]
- 24.Whiteside C, Dessureault S, Dickstein J, Tibbles LA, Torrance S, Boynton E, et al. Women in biomedical research: addressing the challenges. Clin Invest Med 1997;20:268-72. [PubMed]
- 25.De Angelis CD. Women in academic medicine: new insights, same sad news. N Engl J Med 2000;342:426-7. [DOI] [PubMed]
- 26.Rieder RO. The recruitment and training of psychiatric residents for research. Psychopharmacol Bull 1988;24:288-90. [PubMed]
- 27.Cech TR, Egan LW, Doyle C, Gallin E, Lichtman MA, Queenan CJ 3rd, et al. The biomedical research bottleneck. Science 2001;293:573. [DOI] [PubMed]
- 28.Nathan DG, Varmus HE. The National Institutes of Health and clinical research: a progress report. Nat Med 2000;6:1201-4. [DOI] [PubMed]
- 29.Nathan DG. Careers in translational clinical research: historical perspectives, future challenges. JAMA 2002;287:2424-7. [DOI] [PubMed]


