Abstract
Orbital floor fractures are the most commonly encountered traumatic fractures in the facial skeleton. Mydriasis that is detected during orbital floor fracture reconstruction may cause significant distress to surgeons, as it may be associated with sinister events such as visual loss. It is not an uncommon problem; previous studies have shown the incidence of mydriasis to be 2.1%. The combination of careful preoperative evaluation and planning, as well as specific intraoperative investigations when mydriasis is encountered, can be immensely valuable in allaying surgeons' anxiety during orbital floor fracture reconstruction. In this review article, the authors discuss the common causes of mydriasis and present a novel systematic approach to its diagnostic evaluation devised by our unit that has been successfully implemented since 2008.
Keywords: Orbital floor fracture, mydriasis, anisocoria, ciliary ganglion, optic nerve
Pupillary mydriasis during repair of an orbital fracture can be a distressing event. This is not an uncommon phenomenon—in a previous study published by Lim et al, 8 of 387 patients undergoing orbital floor fracture fixation through a subconjunctival approach were found to have intraoperative mydriasis (2.1%).1 In our unit, care of patients with orbital floor fractures is shared between the oculoplastic and craniomaxillofacial trauma services. In our experience, careful preoperative evaluation and planning can be immensely valuable in allaying anxiety when mydriasis is encountered during fracture fixation. Although disconcerting, mydriasis does not signify visual loss in most clinical situations. In this review article, the authors describe the neuroanatomy of the pupil and discuss the common causes of mydriasis and present a novel systematic approach to its diagnostic evaluation devised by our unit.
NEUROANATOMY AND STRUCTRAL ANATOMY OF THE PUPILLARY REFLEX
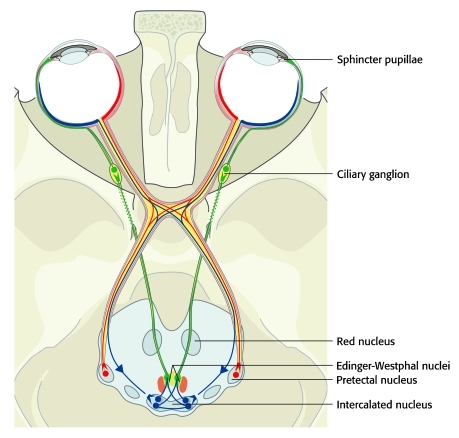
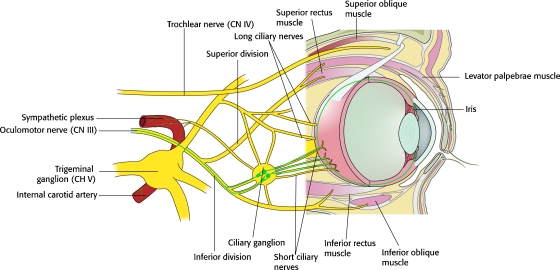
Pupillary constriction is mediated by the parasympathetic system. This is a two-neuron pathway involving the oculomotor nerve and the short ciliary nerve.2 Efferent pupillomotor axons originate in the visceral nuclei of the oculomotor nucleus, which consist of the Edinger-Westphal nuclei, the anterior median nuclei, and the nucleus of Perlia3 (Fig. 1). These pupillomotor fibers exit the midbrain and travel with the ipsilateral oculomotor nerve along the median wall of the cavernous sinus, enter the orbit via the superior orbital fissure inferiorly within the annular tendon of Zinn, along with the inferior division of the oculomotor nerve. Within the orbit, branches from the inferior division innervate the medial rectus and the inferior rectus intraconally before continuing as a mixed nerve with the parasympathetic fibers exiting to synapse at the ciliary ganglion. The remaining motor fibers innervate the inferior oblique. The inferior division of the oculomotor nerve travels adjacent to the lateral border of the inferior rectus before reaching the inferior oblique muscle, where the parasympathetic fibers pass through the ciliary ganglion (Fig. 2). The parasympathetic fibers leave the ganglion via the short ciliary nerves and penetrate the sclera near the optic nerve before terminating in the sphincter pupillae muscle.
Figure 1.
Afferent and efferent visual pathways.
Figure 2.
Ciliary ganglion and innervation to the muscles of the eye.
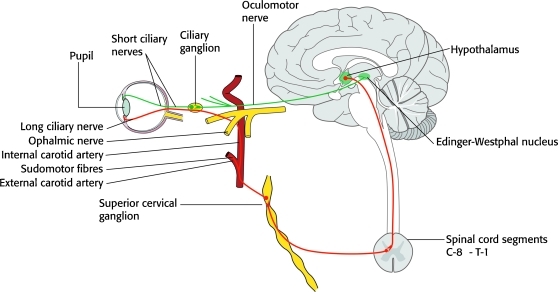
Sympathetic innervation to the pupillodilator is a three-neuron pathway.2 The first-order neuron originates in the hypothalamus and synapses in the lower cervical cord. The second-order preganglionic neuron ascends in the neck to synapse in the superior cervical ganglion. The third-order postganglionic neuron carries the oculosympathetic and facial vasomotor impulses. The vasomotor fibers travel with the external carotid artery, while the oculosympathetic fibers travel on the internal carotid artery. In the orbit, the postganglionic oculosympathetic fibers travel with the long ciliary nerves to innervate the pupillodilator muscle (Fig. 3).
Figure 3.
Sympathetic innervation to the pupillodilator.
The ciliary ganglion is a small irregular structure ∼3 mm in size, situated near the orbital apex, posterolateral to the globe, in loose areolar tissue between the optic nerve and lateral rectus muscle.3 The ganglion lies 1 cm anterior the medial end of the superior orbital fissure and 1.5 to 2.0 cm posterior to the globe. Izci and Gonul4 performed cadaveric dissection studies to elucidate its relationship with the other intraorbital neural and vascular landmarks. The mean distance between the ganglion and optic nerve was 2.9 mm, and the mean distance between the lateral rectus muscle and ganglion was 10.4 mm. Six to 10 short ciliary nerves arise from the ganglion and run forward with the ciliary arteries above and the optic nerve below.
The capsulopalpebral fascia is a fascial slip analogous to the levator aponeurosis of the upper eyelid, originating from near the insertion of the inferior rectus muscle, enveloping the muscle belly of the inferior oblique, condensing anterior to it as the suspensory ligament of Lockwood.5,6 It is joined by the inferior tarsal (sympathetically innervated smooth muscle) before finally inserting onto the posterior, anterior, and inferior edge of the lower tarsus. The clinical relevance is that both the inferior rectus and inferior oblique are intimately joined in this slip, and manipulation of the inferior oblique during fracture exposure results in motion of the inferior rectus, on which the inferior division of the oculomotor nerve usually travels (toward the ciliary ganglion).
PREOPERATIVE EVALUATION
A previously published study showed that the detection of ocular injuries was significantly higher where the ophthalmologist was consulted preoperatively, as compared with a retrospective evaluation initiated by the plastic surgeon.7 This is attributed to the fact that many injuries may initially have minimal or subtle signs and are optimally detected by the ophthalmologist.8 The treatment protocol in our unit requires preoperative assessment of all orbital fractures by both the craniomaxillofacial trauma and oculoplastic services. Patients who had sustained major trauma are evaluated by the oculoplasty service within 24 hours of injury, and those with no manifest ocular disorder (as judged by the craniomaxillofacial surgeon) are evaluated in the ophthalmology clinic within a week.
A meticulous history taken from the patient may reveal invaluable clues in the evaluation of mydriatic patients. Important ophthalmic history that should be obtained includes previous refractive errors, strabismus, amblyopia, and ophthalmic surgeries done. Symptoms of diplopia and pain on ocular movements are noted. In addition, history pertaining to the initial trauma may be relevant, including mechanism of trauma, presence of any concomitant closed intracranial or other injury, and use of drugs (recreational or therapeutic use).
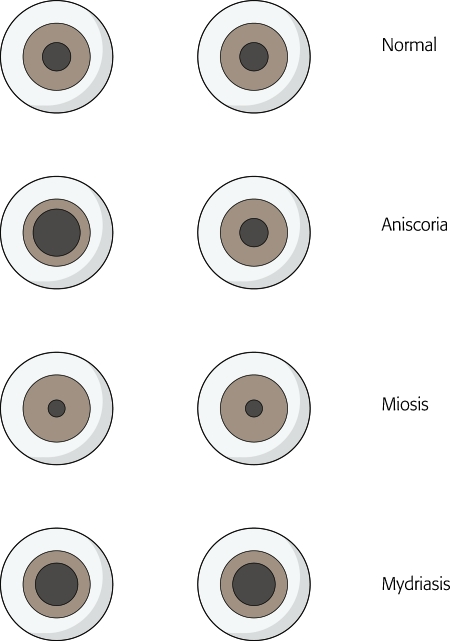
Detailed examination of both eyes including ocular movement, assessment of pupillary size, direct pupillary light reflex, testing for relative afferent pupillary defect (RAPD), indirect ophthalmoscopy, and screening for enophthalmos should be easily performed in an awake patient9 (Fig. 4). Similar assessment in a comatose patient may be difficult.10 In cases where mydriasis or RAPD in the ipsilateral pupil is diagnosed in a patient with an orbital fracture, a slit-lamp examination may be indicated to screen for tear of the iris sphincter. It is also important to avoid a missed diagnosis of injury to the contralateral eye, as associated facial fractures occur in up to 77.2% of patients.11
Figure 4.
Preoperative evaluation of papillary size.
The various causes of mydriasis are discussed below and abbreviated in Table 1.
Table 1.
Causes of Mydriasis during Orbital and Other Surgery
| 1. Preoperative |
| Systemic causes |
| Closed intracranial injuries |
| First rib fractures with Horner's syndrome |
| Drugs and pharmacological agents |
| Ocular causes |
| Traumatic mydriasis |
| Preexisting Adie's pupil |
| Postsurgical atonic pupil |
| Undiagnosed open globe injury |
| Topical cycloplegics |
| Physiological anisocoria |
| 2. Intraoperative |
| Systemic causes |
| Pharmacological agents: atropine, ephedrine, epinephrine, norepinephrine |
| Evolution of closed intracranial events: intracranial hemorrhage, rupture of intracranial aneurysm, cerebral anoxia, etc. |
| Ocular causes |
| Local anesthetic infiltration—eyelid, orbit, paranasal sinuses (cocaine) |
| Orbital complications—manipulation of inferior division of III nerve, manipulation of the ciliary ganglion, direct injury to the optic nerve |
| Undiagnosed open globe injury with intraoperative rupture |
| Violation of poorly repaired/healed open globe with intraoperative dehiscence |
| 3. Postoperative |
| Orbital complications |
| Unmasking of intraoperative manipulation of inferior division of III nerve or ciliary ganglion or complete III nerve at the posterior orbit/apex |
| Spasm of short posterior ciliary arteries/central artery resulting in vascular occlusion |
| Evolution of intracranial events |
PREOPERATIVE EVALUATION
Intracranial Injuries
Almost 75% of orbital floor fractures result from low impact trauma, such as assault, falls, and sports injuries.12 Intracerebral hemorrhage with impending herniation may present with a unilateral dilated pupil, and diffuse anoxic brain damage can cause midbrain dysfunction and dilated pupils.10 A computed tomography head scan and neurosurgical opinion should be obtained if suspicious symptoms or signs are present, as treatment of closed intracranial injuries usually take precedence. Other systemic injuries such as fractures of the first rib may result in Horner syndrome with consequent mydriasis.13
Traumatic Mydriasis
Direct injury to the globe may occur in up to 19.6% of all orbital fractures.11 This may lead to sphincter muscle rupture with consequent mydriasis. Documentation of the postinjury best-corrected visual acuity is important; slit-lamp examination of the eye and indirect ophthalmoscopy are vital to exclude other more catastrophic globe injuries.
Previous Ocular Surgery and Atonic Pupil
Previous intraocular lens replacement is a common cause of apparent mydriasis and may be unilateral or bilateral. It is thought that mydriasis following cataract surgery results from damage to the sphincter muscle.14 Other reports have also described mydriasis following deep lamellar keratoplasty (due to sphincter ischemia following acute rise in intraocular pressure).15 An uncommon cause of an apparently nonreactive pupil is a prosthetic eye, which has previously been a source of diagnostic anxiety.16
Drugs
Commonly abused recreational drugs such as amphetamines and LSD may cause mydriasis and may also be implicated in the initial injury such as motor vehicle accidents or falls from height. Opiate withdrawal may similarly lead to dilated pupils. Pharmacological agents such as antihistamines, tricyclic antidepressants, and inhaled anticholinergics (such as ipratropium bromide) may all potentially cause mydriasis.
Topical Cycloplegics
It should be remembered that many patients may have undergone assessment by the ophthalmologist prior to consultation with the craniomaxillofacial surgeon and that topical cycloplegics, such as tropicamide and hyoscine eye drops, may have been administered, either as a diagnostic evaluation or treatment for traumatic iritis, and may present as unilateral mydriasis.
Physiological Anisocoria
Physiological anisocoria is common and occurs in 20% of the population.17 However, this is distinguished from other pathological causes of mydriasis by the presence of the direct and consensual light reflexes, usually being less than 1-mm difference between the pupils and maintaining the asymmetry in bright and dark environments.17 In patients with light irides, old photographs are helpful in the diagnosis of this condition.
INTRAOPERATIVE EVALUATION
The pupils should again be briefly assessed just prior to commencement of the operation. The use of narcotics (e.g., morphine) both intraoperatively and in the intensive care context may result in miosis, making them relatively nonreactive, which thus renders assessment for RAPD difficult. Similarly, sympathomimetic agents (e.g., ephedrine, epinephrine, norepinephrine) used for their vasopressive, inotropic, or chronotropic effects may cause mydriasis.
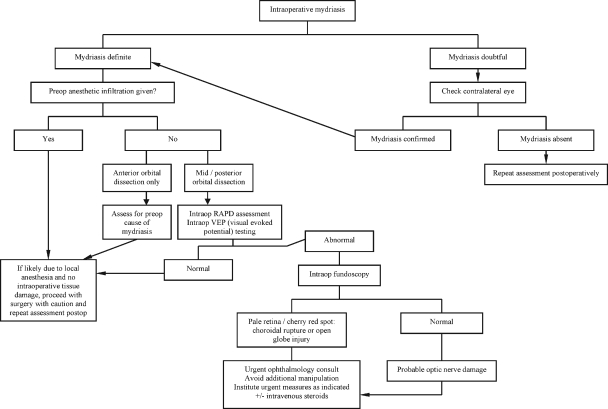
Intraoperatively, should mydriasis of either pupil be present, a repeat assessment of the patient should be done. The presence of mydriasis in one pupil should prompt examination of the contralateral one, hence the importance of proper surgical draping so that both eyes are available for examination intraoperatively. To the authors' knowledge, no algorithm exists for approaching intraoperative papillary mydriasis during orbital floor fracture fixation. Over the years, our unit has developed a novel diagnostic and treatment algorithm in our hospital for intraoperative mydriasis. We have applied this and found it to be useful, and this is detailed in Fig. 5.
Figure 5.
Algorithm for intraoperative evaluation of mydriasis. RAPD, relative afferent pupillary defect.
In general, bilateral mydriasis is much less sinister than unilateral mydriasis. One should again screen for possible precipitating causes of mydriasis as described below. In cases where orbital dissection has proceeded to the mid- or posterior orbit, the presence of a unilateral mydriasis should prompt an intraoperative ophthalmologic assessment before continuing with surgery. Visual evoked potentials and fundoscopy may be warranted in its further evaluation. The commonest causes of mydriasis are that of local anesthetic diffusion (solutions containing adrenaline) and traction of inferior rectus and oblique muscles causing temporary neuropraxia of the inferior branch of the oculomotor nerve.
Pharmacological Agents
Sympathomimetic or anticholinergic medications used during anesthesia can produce mydriatic effect on both pupils. Atropine causes muscarinic acetylcholine receptor blockade and is commonly used at the time of anesthetic induction as a chronotrope and reduction of secretions. Ephedrine and related sympathomimetic compounds are sometimes used for augmentation of blood pressure in multiple trauma patients. These patients generally present with bilateral mydriasis that reverses upon discontinuation of the offending agent. Other pharmacological agents such as phenylephrine/lignocaine spray for topical airway anesthesia,18 nebulized ipratropium,19 and topical epinephrine nasal spray20 have all been reported to cause unilateral mydriasis intraoperatively.
Local Anesthetic Infiltration
Preoperative injection of anesthetic mixture containing lignocaine and adrenaline and bupivacaine into conjunctiva or eyelids can lead to its diffusion into the iris muscular complex, leading to cycloplegia and consequent mydriasis. Based on data previously published by Lim et al, this phenomenon appears to be more common with the transconjunctival approach (2.1%, anesthetic injected into lower conjunctiva) than the subciliary approach (0.8%, anesthetic injected into lower eyelid skin).1 In such cases, patients present with unilateral mydriasis that wears out toward the end of the surgery and usually requires no intervention, provided that other more important causes of unilateral mydriasis have been excluded.
Iatrogenic Globe Injury
Violation of a previously undiagnosed open globe injury may result in intraoperative rupture during its manipulation for exposure of the orbital fracture. This is best prevented rather than treated; a preoperative assessment by the ophthalmologist is paramount in diagnosis of such potential injuries. Intraoperatively, this is recognized by the presence of a tear-drop shaped pupil, loss of the red reflex secondary to vitreous hemorrhage, subconjunctival bleeding, or loss of globe turgor. If present, the surgery should be stopped and an urgent ophthalmologic consult should be obtained on table. Intravenous high-dose steroids (60 mg/d) may be warranted. Fortunately, globe injury is an unlikely event if mydriasis is the sole clinical sign.
Injury to the Inferior Branch of the Oculomotor Nerve and Ciliary Ganglion
The neuroanatomy of the pupillary reflex has been discussed in detail previously. As the inferior oblique and inferior rectus muscles share the capsulopalpebral fascia, overzealous manipulation of the muscles during exposure of the orbital floor fracture may consequently lead to injury to the ciliary ganglion or the inferior branch of the oculomotor nerve, hence, although rare, resulting in mydriasis,21 which may be irreversible. One should refrain from placing a retractor too posteriorly along the lateral aspect of the orbit to avoid injury to the ciliary ganglion22; gentle subperiosteal dissection and elevation of the globe and prolapsed orbital fat during surgery is essential in its prevention. Apart from comminuted inferior/medial rim fractures that may require manipulation of the inferior oblique origin, extensive comminuted floor fractures with periosteal dehiscence and prolapse of orbital fat into the maxillary sinus are often accompanied by excessive manipulation of the inferior orbit, which may result in ciliary ganglion dysfunction.
Vascular occlusion of the ophthalmic/central retinal artery is often a devastating intraoperative complication and can be ruled out by excluding pale ischemic edematous retina or cherry red spot in the macula on fundoscopy.
Direct iatrogenic injury to the optic nerve is less likely to occur. The optic canal is located ∼45 mm posterior to the infraorbital rim,23,24 and iatrogenic damage to the optic nerve is an uncommon occurrence in experienced hands. Should this occur, it may be detected by the presence of intraoperative relative afferent papillary defect and confirmed on visual evoked potential testing.
POSTOPERATIVE EVALUATION
After orbital floor reconstruction is completed, the pupils should be assessed again. It is a common misperception that anisocoria is a sign of visual loss. The pupil, being an efferent organelle, is independent of the visual input provided both eyes are open and exposed to the same amount of light in ambient light conditions. Thus, each eye should be examined independently with the contralateral eye closed such that the incident light stimulus of the eyes is variable, and a difference in papillary diameter may be seen. Therefore, in the postoperative situation, eliciting an RAPD is more useful than looking for a dilated pupil, unless the patient is “one-eyed.” Forced duction test should also be performed to ensure that the full range of motion of the globe is possible.
Finally, it is worthwhile to note that unexplained iatrogenic visual loss has resulted from other surgical operations involving the face, such as high LeFort I osteotomies25 and fixation of zygomatic complex and Le Fort III fractures.26 In the majority of these cases, the final common mechanism appears to be optic nerve neuropathy, and administration of high-dose intravenous steroids does not appear to result in meaningful recovery of function.25 Although no preventive measures have been specifically identified, the principle of practicing gentle, meticulous surgical techniques is a dictum that still holds true in all cases.
CONCLUSION
The importance of thorough preoperative assessment of signs of ocular injuries in cases of orbital floor fractures cannot be overemphasized. In the authors' institution, early involvement of both the craniomaxillofacial surgeon and oculoplasty service is part of a comprehensive multidisciplinary approach to the management of orbital floor fractures. Ocular injuries often manifest with subtle eye signs and are hence best assessed by an ophthalmologist. Should a mydriatic pupil be detected intraoperatively, much anxiety on the part of the surgeon may be allayed if the mydriasis and its causes were determined preoperatively. Familiarity of the neuroanatomy of the orbit is essential during reconstruction of the orbital floor so as to minimize the incidence of complications related to surgery. Often, the surgery may proceed and be completed without much anxiety with assurance of good visual outcome.
References
- Lim T C, Tan W TL, Lim J, Cheng L C. Where's the point? Plast Reconstr Surg. 1998;101:861–862. doi: 10.1097/00006534-199803000-00052. [DOI] [PubMed] [Google Scholar]
- Kawasaki A. Physiology, assessment, and disorders of the pupil. Curr Opin Ophthalmol. 1999;10:394–400. doi: 10.1097/00055735-199912000-00005. [DOI] [PubMed] [Google Scholar]
- Miller N R, Newman N J. In: Walsh & Hoyt's Clinical Neuro-Ophthalmology. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. Anatomy and physiology of the autonomic nervous system; p. 670. [Google Scholar]
- Izci Y, Gonul E. The microsurgical anatomy of the ciliary ganglion and its clinical importance in orbital traumas: an anatomic study. Minim Invasive Neurosurg. 2006;49:156–160. doi: 10.1055/s-2006-944241. [DOI] [PubMed] [Google Scholar]
- Hawes M J, Dortzbach R K. The microscopic anatomy of the lower eyelid retractors. Arch Ophthalmol. 1982;100:1313–1318. doi: 10.1001/archopht.1982.01030040291018. [DOI] [PubMed] [Google Scholar]
- Lim W K, Rajendran K, Choo C T. Microscopic anatomy of the lower eyelid in Asians. Ophthal Plast Reconstr Surg. 2004;20:207–211. doi: 10.1097/01.iop.0000129013.86760.92. [DOI] [PubMed] [Google Scholar]
- Jabaley M E, Lerman M, Sanders H J. Ocular injuries in orbital fractures. A review of 119 cases. Plast Reconstr Surg. 1975;56:410–418. doi: 10.1097/00006534-197510000-00007. [DOI] [PubMed] [Google Scholar]
- Binder P S. Evaluation of the eye following periorbital trauma. Head Neck Surg. 1978;1:139–147. doi: 10.1002/hed.2890010207. [DOI] [PubMed] [Google Scholar]
- Wilhelm H. Neuro-ophthalmology of pupillary function—practical guidelines. J Neurol. 1998;245:573–583. doi: 10.1007/s004150050248. [DOI] [PubMed] [Google Scholar]
- Liu G T, Galetta S L. The neuro-ophthalmologic examination (including coma) Ophthalmol Clin North Am. 2001;14:23–39, vii. [PubMed] [Google Scholar]
- Tong L, Bauer R J, Buchman S R. A current 10-year retrospective survey of 199 surgically treated orbital floor fractures in a nonurban tertiary care center. Plast Reconstr Surg. 2001;108:612–621. doi: 10.1097/00006534-200109010-00003. [DOI] [PubMed] [Google Scholar]
- Chi M J, Ku M, Shin K H, Baek S. An analysis of 733 surgically treated blowout fractures. Ophthalmologica. 2010;224:167–175. doi: 10.1159/000238932. [DOI] [PubMed] [Google Scholar]
- Ozel S K, Kazez A. Horner syndrome due to first rib fracture after major thoracic trauma. J Pediatr Surg. 2005;40:e17–e19. doi: 10.1016/j.jpedsurg.2005.06.020. [DOI] [PubMed] [Google Scholar]
- Lam S, Beck R W, Hall D, Creighton J B. Atonic pupil after cataract surgery. Ophthalmology. 1989;96:589–590. doi: 10.1016/s0161-6420(89)32844-2. [DOI] [PubMed] [Google Scholar]
- Maurino V, Allan B DS, Stevens J D, Tuft S J. Fixed dilated pupil (Urrets-Zavalia syndrome) after air/gas injection after deep lamellar keratoplasty for keratoconus. Am J Ophthalmol. 2002;133:266–268. doi: 10.1016/s0002-9394(01)01308-3. [DOI] [PubMed] [Google Scholar]
- Lentschener C, Benhamou D. A mydriasis unnoticed preoperatively. Anesthesiology. 1998;88:284. doi: 10.1097/00000542-199801000-00057. [DOI] [PubMed] [Google Scholar]
- Thompson H S, Newsome D A, Loewenfeld I E. The fixed dilated pupil. Sudden iridoplegia or mydriatic drops? A simple diagnostic test. Arch Ophthalmol. 1971;86:21–27. doi: 10.1001/archopht.1971.01000010023006. [DOI] [PubMed] [Google Scholar]
- Prielipp R C. Unilateral mydriasis after induction of anaesthesia. Can J Anaesth. 1994;41:140–143. doi: 10.1007/BF03009808. [DOI] [PubMed] [Google Scholar]
- Eustace N, Gardiner C, Eustace P, Marsh B. Nebulised ipratropium causing a unilateral fixed dilated pupil in the critically ill patient: a report of two cases. Crit Care Resusc. 2004;6:268–270. [PubMed] [Google Scholar]
- Wu S H, Huang S H, Lu I C, Lee S S, Chang Y L, Chu K S. Unilateral fixed dilated pupil during plastic surgery—a case report. Acta Anaesthesiol Taiwan. 2007;45:175–179. [PubMed] [Google Scholar]
- Bodker F S, Cytryn A S, Putterman A M, Marschall M A. Postoperative mydriasis after repair of orbital floor fracture. Am J Ophthalmol. 1993;115:372–375. doi: 10.1016/s0002-9394(14)73591-3. [DOI] [PubMed] [Google Scholar]
- Gönül E, Timurkaynak E. Lateral approach to the orbit: an anatomical study. Neurosurg Rev. 1998;21:111–116. doi: 10.1007/BF02389315. [DOI] [PubMed] [Google Scholar]
- Lemke B N, Lucarelli M J. Anatomy of ocular adnexa and orbit. In: In: Smith BC, editor. Ophthalmic Plastic and Reconstructive Surgery. 2nd ed. St. Louis, MO: CV Mosby; 1997. pp. 3–78. [Google Scholar]
- Whitnall S E. The Anatomy of the Human Orbit and Accessory Organs of Vision. New York: Oxford University Press; 1932. pp. 1–252.
- Lo L J, Hung K F, Chen Y R. Blindness as a complication of Le Fort I osteotomy for maxillary distraction. Plast Reconstr Surg. 2002;109:688–698. discussion 699–700. doi: 10.1097/00006534-200202000-00041. [DOI] [PubMed] [Google Scholar]
- Bun R J, Vissink A, Bos R R. Traumatic superior orbital fissure syndrome: report of two cases. J Oral Maxillofac Surg. 1996;54:758–761. doi: 10.1016/s0278-2391(96)90698-9. [DOI] [PubMed] [Google Scholar]