Abstract
In a series of articles spanning 8 years, Ed Ellis reviewed the clinical results of the treatment of 478 mandibular angle fractures managed by eight different techniques. During a series of benchtop investigations employing polyurethane synthetic mandible replicas, Rich Haug investigated the biomechanical behavior of approximately 15 different techniques designed to reconstruct mandibular angle fractures. This article reviews these two series of investigations in an attempt to gain insight into the biomechanical and biological factors that affect the successful reconstruction of mandibular angle fractures. It appears that the current techniques used to reconstruct mandibular angle fractures are sound from the standpoint of biomechanics within a range of forces encountered during clinical function. It also appears that an unsuccessful reconstruction is based on a biological result of a behavioral issue such as noncompliance, substance abuse, and/or nutritional or immune compromise.
Keywords: Mandibular angle fractures, yield point, yield load, yield displacement, stiffness, biomechanics, polyurethane synthetic mandible replicas
It is at once unusual and fortunate that two individuals who are well reputed in the field of craniomaxillofacial trauma have pursued the reconstruction of mandibular angle fractures in a thorough and concise manner—one from the clinical perspective and the other from a biomechanical perspective—independently, yet concurrently. Ed Ellis began a series of investigations in 1991 that evaluated eight different methods of reconstructing mandibular angle fractures from the clinical perspective. Although this series of investigations was conducted over an 8-year period, the patient population (and thus demographics of age, sex, socioeconomic status, and ethnicity), geographic location, institution, and responsible senior surgeon and investigator were all the same. Thus, the treatment modality that was the subject of each report was essentially the only meaningful variable in each investigation.1,2,3,4,5,6,7,8 Also fortunate was that the first article in the series reported on management by closed reduction, and therefore could serve a control, or cohort, for comparison.7
Rich Haug began his series of biomechanical investigations using human bone substitutes to eliminate many of the variables associated with natural or live tissue, thereby being able to focus on the single variable of the individual reconstruction modality being evaluated. Eliminating the variables associated with the living, healing human permits a unique opportunity to assess only the reconstruction technique and its mechanical interaction with the substrate being reconstructed. The unique opportunity we have in evaluating and comparing these two series of investigations is that they may give us insight into the advantages of one method of reconstruction over another. Also, we may discern whether a purely biological factor can influence healing and thus the success or failure of the specific reconstruction modality.
This article reviews the clinical series of investigations performed by Ellis and his group, reviews the biomechanical investigations performed by Haug and his group, and then compares and evaluates the findings of both to give the reader insight into the advantages and/or disadvantages of one particular reconstruction modality over another, and to ascertain whether biological influences affect the success or failure of these reconstruction modalities.
ELLIS'S CLINICAL INVESTIGATIONS
Although not first in the chronological sequence of Ellis's investigations, the review by Passeri and co-investigators is presented here initially to act as perhaps a control cohort for comparison with the other investigations in Ellis's series (Table 1).7 In this study, 96 patients with 99 mandibular angle fractures were managed with a closed reduction or nonrigid means of fixation during a 3-year period. Age, sex, ethnicity, number of fractures, etiology, and other systemic injuries were recorded, along with the method of treatment, time between injury and surgery, duration of maxillomandibular fixation, duration of postsurgical follow-up, and complications. The types of complications that were recorded were infection, malocclusion, malunion, and nonunion. The most frequent complication was infection (17%), followed by a combination of infection, nonunion, and malocclusion (4%). The explanations provided by the authors for the complications recorded were that the patients enrolled in this study, who were mostly indigent, were not extremely cooperative, were not healthcare conscious (i.e., were sporadic in making postoperative visits and were noncompliant), and abused drugs. It is convenient to use the cohort reviewed in this investigation as a control for the other studies because the institution, geographic region, and demographics of the patient population were essentially the same. Because maxillomandibular fixation was also used in the other investigations, the only variables were the methods of rigid internal fixation employed during the other investigations.
Table 1.
Summary of Ellis's Clinical Investigations of Mandibular Angle Fracture Fixation Techniques
| Investigation | Patient Population | Fixation Technique | Results |
|---|---|---|---|
| Passeri LA, Ellis E, Sinn DP (1993)7 | 96 patients with 99 fractures managed over 3-y | Closed reduction with maxillomandibular fixation, or nonrigid means of fixation | 17% infection only, 4% combination of infection, nonunion, and malocclusion |
| Ellis E 3rd, Ghali G (1991)2 | 30 patients managed over 1-y | Single 2.7-mm lag screw technique | 27% additional fixation, 23% infection/bone exposure, 7% occlusal discrepancies |
| Ellis E 3rd, Karas N (1992)3 | 30 patients with 31 fractures | Two 2-mm four-hole minidynamic compression plates | 30% total complication rate; swelling and low-grade infection requiring plate removal (17%), early infection (10%), nonunion with malocclusion (3%) |
| Ellis E 3rd (1993)1 | 52 patients with 52 fractures over 2-y | 2.7-mm reconstruction plate | 8% postoperative malocclusion and 8% postoperative infection |
| Ellis E 3rd, Sinn DP (1993)4 | 65 consecutive patients | Two 2.4-mm dynamic compression plates | 32% infections, 32% hardware removal, 18% nonunion, 2% nonunion with malocclusion |
| Ellis E 3rd, Walker LR (1994)5 | 67 consecutive patients with 69 fractures | Two 2-mm noncompression miniplates (self-tapping screws) | 28% total complications. 25% infections, 23% hardware removal, 7% delayed union, 1% nonunion. |
| Ellis E 3rd, Walker LR (1996)6 | 81 patients treated over 2-y period | One 2-mm four-hole superior border noncompression miniplate (self-tapping screws) | 16% infection, 1% infection and fibrous union |
| Potter J, Ellis E 3rd (1999)8 | 46 patients with 51 fractures over 2-y | One seven-hole, thin, malleable miniplate secured with six 1.3-mm self-tapping screws | 15% total infections, 6% minor infections,11% plate fracture, 4% requiring additional fixation |
In 1991, Ellis's group began its series that investigated use of different fixation techniques for the reconstruction of mandibular angle fractures.2 In this first study, 30 patients were managed over a 1-year period with a single 2.7-mm lag screw fixation method that has become known as the Niederdellmann technique. Additional fractures, teeth in the line of fracture, duration of maxillofacial fixation, postsurgical occlusal relationship, infection, dehiscence/exposure of bone, and need for further surgery were recorded. Twenty-seven percent of the patients required additional fixation, 7% had minor occlusal discrepancies, and 23% developed soft tissue infections and/or bone exposures. The authors offer that this is a very technique-sensitive procedure, requiring experience. They also suggested that the indigent, noncompliant population of patients may have been the cause of the high infection/dehiscence rate.
Next in the series was a review of the management of 30 consecutive patients with 31 mandibular angle fractures managed by two 2-mm, four-hole minidynamic compression plates.3 Additional fractures, presence of a tooth in the line of the fracture (or its extraction), complications during surgery, postsurgical occlusion, and complications were recorded. The total complication rate was 30% with the most frequent being swelling and low-grade infection requiring plate removal (17%), followed by early infections (10%), and, finally, nonunion with malocclusion (3%). The authors' suggested reasons for complications were failure to use drains (no longer popular in this present era), insufficient stability provided by the fixation that was applied, and failure to tap (again, no longer used in this present era).
In 1993, Ellis published the results of the management of 52 patients with unilateral mandibular angle fractures over a 2-year period with 2.7-mm reconstruction plates.1 The plate lengths appear to have varied in fixation from 6 to 10 screws. The type of fracture, concomitant fractures, presence or extraction of a tooth in the line of fracture, complications during surgery, postsurgical occlusion, and postsurgical complications were all recorded. Eight percent of the patients sustained a postoperative malocclusion, and another 8% suffered postoperative infections. This rate of infection was considered by the author to be commendable in light of the demographics of the patient population, the etiology of the fractures, and the frequent transcutaneous surgical approach. Moreover, the technical difficulty in bending large reconstruction plates was discussed as an explanation for the postoperative malocclusions.
Ellis and Sinn then went on to evaluate the reconstruction of mandibular angle fractures with two 2.4-mm dynamic compression plates.4 Sixty-five patients with noncomminuted fractures were enrolled in this investigation. As in the previous investigations, concomitant fractures, presence or extraction of a tooth in the line of fracture, complications during surgery, and postsurgical occlusion and complications were all recorded and analyzed. The first 20 cases were managed without tapping the drill holes, and the last 45 were done with tapping. An overall infection rate of 32% was recorded, with a 40% rate for untapped screws and 29% for those that were tapped. Thirty-two percent of the patients required hardware removal, 18% developed nonunions, and 2% had a nonunion with malocclusion. The technique was described as being “relatively easy, but resulted in an unacceptable rate of infection.”4 The authors offered that two likely factors affecting failure were fracture instability and bone necrosis, and also suggested that not tapping and interfragmental compression caused the devitalization of the bone. Moreover, they went on to comment on the nature of the patient population as being causative due to chronic substance abuse with nutritional and possibly immune deficiencies.
The next in the Ellis series of mandibular angle fracture management investigations addressed the investigators' concerns from their previous article.5 Although compression and nontapping were attributed to failure in that series, this investigation examined noncompression plates that employed self-tapping screws. This study was conducted over a 1-year period and used the same measures and parameters as the previous investigations. Two four-hole noncompression miniplates were secured with 2-mm outer thread diameter, self-tapping screws. The authors identified a 28% total complications rate with 25% infections, 23% of the patients who required hardware removal, 7% with delayed union, and 1% with nonunion. The causes for complications were attributed to the biomechanics of compression and absolute rigid fixation.
In 1996, Ellis and Walker reviewed the management of 81 patients with mandibular angle fractures treated with one four-hole noncompression miniplate that had self-tapping, 2-mm outer thread diameter screws.6 The same parameters for investigation used in pervious studies were recorded. A total of 16% of patients had complications—all being infections—which were classified as minor (14%) or major (2%), with the major complications requiring hospitalization. One patient (1%) developed a fibrous union. Perplexing to the authors was the fact that the patients who developed complications were no different, demographically or socioeconomically, than other patients in the study. The authors suggested that biomechanics, rather than absolute rigid immobilization may be more advantageous for healing.
The last in Ellis's series involved an extension of his thought on biomechanics and nonrigid fixation, along with minimal incision and dissection.8 This study reviewed the management of 46 patients with 51 mandibular angle fractures who were treated by intraoral open reduction and internal fixation using one thin, malleable, seven-hole miniplate secured with six 1.3-mm outer thread diameter, self-tapping screws. The same parameters for investigation as the previous studies were used, and the study was conducted over a 2-year period. In this series, only a 15% complication rate was identified, and all were minor. Six percent suffered minor infections. Although the fixation device fractured in 11% of the patients, only 4% required additional fixation. The authors concluded the discussion of the results of this series of mandibular angle fracture management with the suggestion that nonrigid fixation may be the best modality for management of this specific injury.
HAUG'S BIOMECHANICAL INVESTIGATIONS
Rich Haug initially began his biomechanical research using natural animal bone as a human substitute.9,10,11 The decision not to use human cadaveric mandibles was because biomechanical, ethical, practical, and monetary issues made their use less than ideal. The biomechanical issues were the normal variation in geometry, proportion, and material properties that occurs through natural variation.12,13 Ethical concerns existed in the lay and medical communities regarding the use of human tissues for research.14,15 Practical issues included storage, preservation, and disease transmission.16,17 Monetary considerations included not only the costs incurred by addressing the practical issues but also the cost of purchasing the cadaver tissue. For these reasons, animal tissue and other materials have been used for research.9,10,11,18 Unfortunately, most of these same issues exist with the use of animal tissues, although purchase cost may be significantly lower. For such reasons, Haug's group first sought to explore different human bone substitutes and to identify an appropriate substrate for use in biomechanical investigations.19
In 2000, Bredbenner and Haug compared human cadaver mandibular bone, bovine rib, porcine rib, photoelastic epoxy, and two types of polyurethane synthetic mandibles, each of which had been used previously in maxillofacial biomechanical research.19 It is interesting to note that bovine rib actually has the geometry and proportions of an edentulous human hemimandible, being broader at the base and thinner at what would be the alveolus, with a cancellous core and cortical outer layer.10 Photoelastic epoxy is an interesting material in that it can provide insight into the stress and strain encountered within the substrate when in function.20 Red oak actually has the identical modulus of elasticity as natural bone.21 The two polyurethane synthetic mandible replicas were created from impressions of actual human cadavers and thus were uniform in geometry and proportion. Because each was fabricated from the same impression, the variations that routinely occur in nature were eliminated. One was created without a simulated cortex (Sawbones, Pacific Research Laboratories, Vashon Island, WA), and the other had a simulated cancellous core and simulated outer cortex (Synbones, Landquart, Switzerland). Each of these replicas has been used to simulate craniomaxillofacial surgery for educational purposes. The mechanical standards for comparison were pullout strength and insertional torque, the gold standards in the industry.22 Both 1-mm and 2.4-mm outer thread diameter screws were used in the analysis. The results of this investigation indicated that no statistically significant differences existed between either of the synthetic mandible types and the human cadaver mandible for the parameters tested. Thus, the use of these human bone substitutes was validated for this type of research, and both provide a near ideal alternative to human mandibular tissue.
After this validation of using polyurethane synthetic mandible replicas as human bone substitutes for research, Haug's group went on to evaluate different reconstruction modalities for mandibular angle fractures (the focus of this review), mandibular condyle fractures, mandibular symphysis/parasymphysis fractures, and edentulous mandible fractures. Each of the investigations in this series identified the endpoints for the experimentation as either (1) catastrophic failure (the plate/screw system broke) or (2) the yield point (that point at which permanent deformation of the system began). Yield load (the load at which permanent deformation began), yield displacement (the distance at which the yield point was reached), and stiffness (the slope of the yield-displacement curve) were the measures used for comparison. In addition, rather than consider loads that exceeded normal human function, postsurgery or post-trauma loads were only considered within parameters for chewing, speaking, and swallowing.
The first in this series was performed during the era of controversy between two camps of surgeons who differed in fixation philosophy—the “big plate” group (the AO — Arbeitgemeinschaft für osteosynthesis fragen) and the “small plate” group (the Champy followers).23 During this first investigation, Haug's group compared a two, two-hole, 2.4-mm miniplate to the conventional technique that used a 2.4-mm two-hole tension band, two-hole stabilization plate (Table 2). In addition, a third system was evaluated and compared that essentially reversed the placement of the conventional system, based on the anatomy of the angle of the mandible. The larger, thicker stabilization plate was placed at the larger, thicker superior border and alveolus, and the thinner tension band was placed at the thinner inferior border. At the end of the investigation, absolutely no statistically significant differences between any of the three groups were found. This was a rather remarkable finding, as well as validation for both the big plate and small plate philosophical camps.
Table 2.
Summary of Haug's Biomechanical Investigations of Mandibular Angle Fracture Fixation Techniques
| Investigation | Results |
|---|---|
| Haug RH, Barber JE, Reifeis R (1996)23 | No statistically significant differences seen between the three different plating techniques. |
| Haug RH, Fattahi TT, Goltz M (2001)24 | No statistically significant differences seen in yield load within any of the categories for both incisal edge loading and contralateral molar loading. |
| No statistically significant differences seen among the best performing representatives of each category for yield point during incisal edge loading. Statistically significant difference noted between reconstruction plate and single monocortical superior border plate for yield load under torsionally deforming forces, but not between any of the other groupings. | |
| Haug RH, Street CC, Goltz M (2002)25 | Degree of adaptation affected mechanical behavior. All systems performed favorably with 0-mm offset. Locking systems all performed favorably at 1- and 2-mm offset. Nonlocking single monocortical superior border fixation system continued to perform favorably, even at 1-mm offset. |
The next in Haug's series that evaluated mandibular angle fracture fixation techniques was an investigation that was much more comprehensive: 14 different plating philosophies or techniques were compared, using 150 polyurethane synthetic mandible replicas and 190 plates secured with 1180 screws. The study evaluated vertically deforming forces (incisal edge loading) and torsional forces (contralateral molar loading).24 The different philosophies and techniques (Table 3) can generally be categorized as single screw or single monocortical superior border plate techniques, monocortical two-plate techniques, monocortical tension band/bicortical stabilization plate techniques, and reconstruction plate techniques. Because of the magnitude of the project, the statistical analysis was first conducted within the philosophical technique groups, and then between the best performers of each group. To do a comparison between each individual technique would have required three to four times the number of samples and would have required approximately another $250,000.00 in funding.
Table 3.
Summary of the Fixation Techniques Used
| Category | Fixation Technique |
|---|---|
| Control | No fixation |
| Single screw or monocortical superior border plate techniques | One 2.4 OTD, 40-mm long lag screw |
| One seven-hole, 1.3-mm adaptation plate secured with six 1.3-mm OTD, 6-mm long monocortical screws | |
| One six-hole 2-mm superior border plate secured with six 2-mm OTD, 6-mm long monocortical screws | |
| One six-hole, 2-mm locking superior border plate secured with six 2-mm OTD, 6-mm long monocortical locking screws | |
| Monocortical two-plate techniques | Two 2-mm plates secured with six 2 OTD, 6-mm long monocortical screws each |
| Two 2-mm locking plates secured with six 2 OTD, 6-mm long monocortical locking screws each | |
| One eight-hole strut plate secured with eight 2-mm OTD, 6-mm long monocortical screws | |
| Monocortical tension band/bicortical stabilization plate techniques | One six-hole 2-mm tension band secured with six 2-mm OTD, 6-mm long monocortical screws and; one eight-hole curved 2-mm bicortical stabilization plate secured with six 2-mm OTD, 16-mm long bicortical screws |
| One six-hole 2-mm tension band secured with six 2 OTD, 6-mm long monocortical screws and; one 2.4-mm limited contact dynamic compression plate secured with six 2.4-mm OTD, 16-mm long bicortical screws | |
| One six-hole 2-mm tension band secured with six 2 OTD, 6-mm long monocortical screws and; one 2.4-mm six-hole angled universal fracture plate secured with six 2.4-mm OTD 16-mm long bicortical screws | |
| One 2-mm locking tension band secured with six 2-mm OTD, 6-mm long monocortical locking screws and; one 2-mm locking stabilization plate secured with six 2-mm OTD, 16-mm long bicortical locking screws | |
| Reconstruction plate techniques | One seven-hole titanium hollow reconstruction plate secured with six 3-mm OTD, 16-mm long bicortical titanium hollow reconstruction screws, after pretapping and then locked with six locking screws |
| One six-hole 2.7-mm reconstruction plate secured with six 2.7-mm OTD, 16-mm long bicortical screws after pretapping | |
| One 2.4-mm locking reconstruction plate secured with six 2.4-mm OTD, 16-mm long bicortical locking screws |
OTD, outer thread diameter.
From Haug RH, Fattahi TT, Goltz M. A biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg 2001;59(10):1199–1210.
This broad investigation found no statistically significant differences in yield load (the most important measure of failure) within any of the categories for both incisal edge loading (vertical deformation) and contralateral molar loading (torsional deformation) (Table 2). That means that despite hardware differences, within categories each of the different plating techniques performed the same. Even more dramatic was the statistical comparison among the best performing representative from each group. Again, no statistical differences for the yield point during incisal edge loading were found. This amazing observation means that a single monocortical superior border plate performed as well as a monocortical two-plate system, a monocortical tension band/bicortical stabilization plate system, and a reconstruction plate. However, a statistically significant difference was noted between the reconstruction plate and the single monocortical superior border plate for yield load under torsionally deforming forces, but not between any of the other groupings. This means that no differences were found between the reconstruction plate and either of the other two-plate systems, or between the single monocortical superior border plate and any of the other two-plate systems for yield load under torsionally deforming forces. Again, this was a very intriguing finding. Essentially, all of the systems could potentially perform similarly within functional parameters.
The latest in the Haug et al series evaluating mandibular angle fracture fixation techniques explored the relationship between locking and nonlocking fixation systems.25 Using the same measures for evaluation, as well as the same functional parameters, the effects of locking and nonlocking hardware were evaluated for a 2-mm single monocortical superior border plate and a 2.4-mm reconstruction plate. These were reconstructed with a 0-mm offset (intimate adaptation of the plate to the mandible), a 1-mm offset (the equivalent of “sloppy” plate bending), and a 2-mm offset (totally inappropriate plate bending). As one would expect, at 2 mm both of the nonlocking systems immediately failed, whereas the locking systems performed favorably. At a 0-mm offset, all systems performed favorably. Of interest is that at 1 mm the nonlocking reconstruction plate failed to perform, whereas the nonlocking single monocortical superior border fixation continued to perform favorably. Even with technical difficulties, such as sloppy plate contouring, the single monocortical superior border fixation system was more forgiving.
DISCUSSION
When reviewing the observations and conclusions common to Ed Ellis's investigations, two general themes become apparent. First, biological factors play a role, such as the nutritional and perhaps immune deficiencies associated with the indigent population that was enrolled in the study and the noncompliant and substance abusing behavior associated with that population. Second, certain techniques may be problematic. This includes compression techniques and self-tapping techniques.
When reviewing the results of Haug's series, it becomes clear that within the functional parameters established for postsurgical, post-trauma patients (certainly below 30 kg, most likely below 20 kg, and probably approaching 10 kg bite force) that all systems currently in use are biomechanically effective reconstructive alternatives for mandibular angle fractures.9,10,18,22,23,25 Most dramatic was the statistical similarity even between the very large reconstruction plates and very thin superior border monocortical plates in their ability to resist vertical deformation, differing only in their ability to resist torsionally deforming forces. No biomechanical differences were noted between the compression systems compared with the noncompression systems, as implied by Ellis. Moreover, all of the systems in Haug's series employed self-tapping screws except for the titanium hollow reconstruction plates (which used screw receptacles that were tapped).
If we were to use the results of the patients assessed in Passeri et al7 as a control cohort, then we would have the beginning of a standard for comparison of the other techniques in Ellis's series. Because the patients managed in that study received, for the most part, closed reduction and maxillomandibular fixation, their complication rate of 17% could be assumed to be the standard for comparison. With that in mind, the absolute rigid techniques (stainless steel reconstruction plate) and noncompression techniques were as minimally problematic (15 to 16% complications) as the closed reduction group in Passeri's article (17%), whereas the other techniques fared much more poorly (27 to 32%). Because this differs from Haug's observations, it suggests some form of biological rather than mechanical difference.
Ellis concludes that the best results (although not statistically different than other methods in his series) came from a single, thin, malleable monocortical noncompression plate, using 1.3-mm outer thread diameter, self-tapping screws placed through an intraoral incision with minimal dissection and soft tissue stripping.8 He goes on to ask, “If less stability across an angle fracture meets with better clinical success, how much instability can be tolerated.”8 Restated, how thin and malleable can a plate be and still provide resistance to deforming forces when in function? We tried to answer that question using the same synthetic mandible replicas and same functional parameters as were used in the investigations in Haug's series. We used the smallest plate/screw system currently available, the Synthes (Synthes Maxillofacial, Paoli, PA) 1-mm system (Fig. 1).
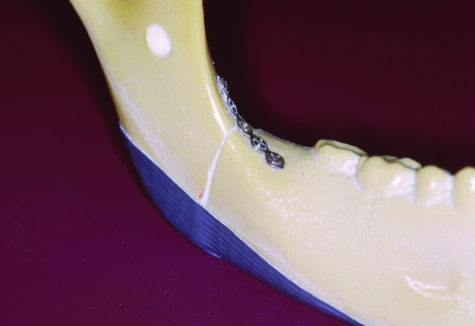
Figure 1.
The polyurethane synthetic mandible replica reconstructed with a five-hole microplate and monocortical self-tapping, 1-mm outer thread diameter screws. Note the simulated pterygomandibular sling (using duct tape), intended to mimic minimal soft tissue stripping.
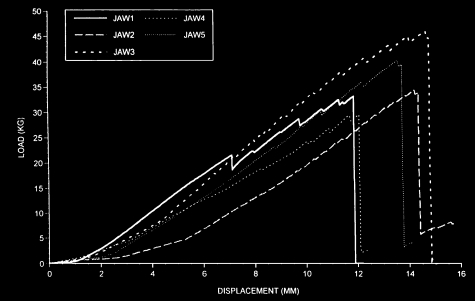
Five polyurethane mandible replicas were uniformly sectioned at the angle of the mandible using a jig. Each was reconstructed with a Synthes five-hole microplate and four 1-mm outer thread diameter screws. To represent the pterygomandibular sling that remained undissected during this simulated surgery, duct tape was used (Fig. 1). These reconstructed replicas were then secured in a jig and tested as in Haug and co-investigators' previous investigations. The results of the load displacement data were recorded (Fig. 2). It is interesting to note that the yield point (i.e., the point at which permanent deformation of the system began) occurred at 27 to 45 kg. Remembering that functional parameters for postsurgical, post-trauma patients are certainly below 30 kg, most likely below 20 kg, and probably approaching 10 kg, even this very small system meets the functional requirements under the conditions tested.
Figure 2.
The load/displacement data for the five samples tested.
Although benchtop investigations using synthetic replicas help to identify trends in behavior, these trends need to be verified with clinical investigations. The differences noted in the Ellis series, despite similarities observed in Haug's series, suggest that biological factors may be the most important factors in the success or failure of a reconstructive technique. It appears that the current techniques used to reconstruct mandibular angle fractures are sound from the standpoint of biomechanics within a range of forces encountered during clinical function. It also appears that an unsuccessful reconstruction is based on biological results of behavioral issues such as noncompliance, substance abuse, and/or nutritional or immune compromise.
References
- Ellis E., 3rd Treatment of mandibular angle fractures using the AO reconstruction plate. J Oral Maxillofac Surg. 1993;51(3):250–254. doi: 10.1016/s0278-2391(10)80166-1. [DOI] [PubMed] [Google Scholar]
- Ellis E, 3rd, Ghali G. Lag screw fixation of mandibular angle fractures. J Oral Maxillofac Surg. 1991;49(3):234–243. doi: 10.1016/0278-2391(91)90212-5. [DOI] [PubMed] [Google Scholar]
- Ellis E, 3rd, Karas N. Treatment of mandibular angle fractures using two mini dynamic compression plates. J Oral Maxillofac Surg. 1992;50(9):958–963. doi: 10.1016/0278-2391(92)90055-5. [DOI] [PubMed] [Google Scholar]
- Ellis E, 3rd, Sinn D P. Treatment of mandibular angle fractures using two 2.4-mm dynamic compression plates. J Oral Maxillofac Surg. 1993;51(9):969–973. doi: 10.1016/s0278-2391(10)80036-9. [DOI] [PubMed] [Google Scholar]
- Ellis E, 3rd, Walker L R. Treatment of mandibular angle fractures using two non-compression miniplates. J Oral Maxillofac Surg. 1994;52(10):1032–1036. doi: 10.1016/0278-2391(94)90169-4. [DOI] [PubMed] [Google Scholar]
- Ellis E, 3rd, Walker L R. Treatment of mandibular angle fractures using one non-compression miniplate. J Oral Maxillofac Surg. 1996;54(7):864–871. doi: 10.1016/s0278-2391(96)90538-8. [DOI] [PubMed] [Google Scholar]
- Passeri L A, Ellis E, 3rd, Sinn D P. Complications of nonrigid fixation of mandibular angle fractures. J Oral Maxillofac Surg. 1993;51(4):382–384. doi: 10.1016/s0278-2391(10)80350-7. [DOI] [PubMed] [Google Scholar]
- Potter J, Ellis E., 3rd Treatment of mandibular angle fractures with a malleable noncompression miniplate. J Oral Maxillofac Surg. 1999;57(3):288–292. doi: 10.1016/s0278-2391(99)90674-2. [DOI] [PubMed] [Google Scholar]
- Haug R H. The effects of screw number and length on two methods of tension band plating. J Oral Maxillofac Surg. 1993;51(2):159–162. doi: 10.1016/s0278-2391(10)80015-1. [DOI] [PubMed] [Google Scholar]
- Haug R H. The effect of screw number on reconstruction plating. Oral Surg Oral Med Oral Pathol. 1993;75(6):664–668. doi: 10.1016/0030-4220(93)90418-4. [DOI] [PubMed] [Google Scholar]
- Murphy M T, Haug R H, Barber J E. A comparison of the mechanical characteristics of three sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg. 1997;55(5):489–494. doi: 10.1016/s0278-2391(97)90699-6. [DOI] [PubMed] [Google Scholar]
- Dechow P C, Nail G A, Schwartz-Dabney C L, Ashman R B. Elastic properties of human supraorbital and mandibular bone. Am J Phys Anthropol. 1993;90(3):291–306. doi: 10.1002/ajpa.1330900304. [DOI] [PubMed] [Google Scholar]
- Kohn D H, Richmond E M, Dootz E R, et al. In vitro comparison of parameters affecting the fixation strength of sagittal split osteotomies. J Oral Maxillofac Surg. 1995;53(12):1374–1383. doi: 10.1016/0278-2391(95)90658-4. [DOI] [PubMed] [Google Scholar]
- King A I, Viano D C, Mizeres N, et al. Humanitarian benefits of cadaver research on injury prevention. J Trauma. 1995;38(4):564–569. doi: 10.1097/00005373-199504000-00016. [DOI] [PubMed] [Google Scholar]
- O'Neill O. Medical and scientific uses of human tissue [editorial] J Med Ethics. 1996;22(1):5–7. doi: 10.1136/jme.22.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh J M, King A I. Control of transmission of HIV and other bloodborne pathogens in biomechanical cadaveric testing. J Orthop Res. 1990;8(2):159–166. doi: 10.1002/jor.1100080202. [DOI] [PubMed] [Google Scholar]
- Gorup J M, Merola A A, Bono C M, et al. Technique for the harvesting of human cadaveric spines. Spine. 1998;23(20):2222–2225. doi: 10.1097/00007632-199810150-00016. [DOI] [PubMed] [Google Scholar]
- Haug R H, Barber E, Punjabi A P. An in vitro comparison of the effect of number and pattern of positional screws on load resistance. J Oral Maxillofac Surg. 1999;57(3):300–308. doi: 10.1016/s0278-2391(99)90677-8. [DOI] [PubMed] [Google Scholar]
- Bredbenner T L, Haug R H. Substitutes for human cadaveric bone in maxillofacial rigid fixation research. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(5):574–580. doi: 10.1067/moe.2000.111025. [DOI] [PubMed] [Google Scholar]
- Rudman R A, Rosenthal S C, Shen C, et al. Photoelastic analysis of miniplate osteosynthesis for mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(2):129–136. doi: 10.1016/s1079-2104(97)90057-3. [DOI] [PubMed] [Google Scholar]
- Avallone E A, Baumeister T. Mark's Standards Handbook for Mechanical Engineers. 9th ed. Philadelphia: McGraw; 1987.
- American Society for Testing and Materials Annual Book of ASTM Standards. Vol. 13.01. Philadelphia: The American Society for Testing and Materials; 1998.
- Haug R H, Barber J E, Reifeis R. A comparison of mandibular angle fracture plating techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(3):257–263. doi: 10.1016/s1079-2104(96)80349-0. [DOI] [PubMed] [Google Scholar]
- Haug R H, Fattahi T T, Goltz M. A biomechanical evaluation of mandibular angle fracture plating techniques. J Oral Maxillofac Surg. 2001;59(10):1199–1210. doi: 10.1053/joms.2001.26726. [DOI] [PubMed] [Google Scholar]
- Haug R H, Street C C, Goltz M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg. 2002;60(11):1319–1326. doi: 10.1053/joms.2002.35732. [DOI] [PubMed] [Google Scholar]