Abstract
A system of orderly triage of the injured in World War I and a protocol for early wound management of war injuries were introduced by Antoine De Page in 1914 at the beginning of World War I. The five steps of the De Page protocol (coined by the author as Ordre de Triage) were to be followed in detail by the French and Belgian armies. A younger Belgian colleague, Robert Danis, was recruited to aid in the management of the ambulance corps to transport the injured from dressing (“clearing”) stations to centers of more advanced care, away from the Franco-Belgian front. Danis, also from Brussels, introduced the principles of osteosynthesis of bone a little over a decade later. De Page and Danis, both surgeons, tendered immense carry-forwards for future generations.
Keywords: Triage, wounds of war, De Page, Danis
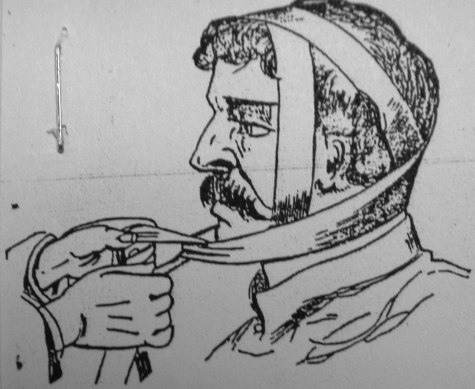
The Napoleonic War and the European wars during the Second French Empire revolutionized armed warfare (1799 to 1815 and 1852 to 1870, respectively), due in part to the introduction of mass conscription and the use of artillery.1,2 The injured soldiers of the day made their way after trauma by walking from the line of confrontation to distant health stations for wound care; rarely was retrieval by horse or horse-and-wagon available. The less able were left to await assistance or suffer an agonizing death. Stabilization of fractures of the mandible was achieved much as it had been for centuries: manipulation, placement of circumdental wires about the teeth at the line of fracture, and the application of a Bertrandi dressing3 (Fig. 1). On occasion, a Chopart-Desault type of oral splint was used in lieu of wire to stabilize the fragments of the lower jaw before applying “the Bertrandi.”
Figure 1.
First designed in 1787, the Bertrandi dressing was popular in Europe for the stabilization of fractures of the lower jaw, and it was still widely used in World War I. Fragments were manipulated by hand, and the chin was placed in the center of the linen dressing that had been split into four tails. One set of sleeves was drawn horizontally, from the nape of neck to the chin. A second set was passed vertically, tied together, and then brought down to engage the horizontal sleeves. (The Barton and Hamilton dressings, popular in North America during World War I, were of similar design.) Application of “the Bertrandi” was preceded by the application of circumdental wires about the teeth adjacent to the fracture, or preceded by the insertion of a Chopart-Desault oral splint.
French Empire surgeons uniquely recommended proactive, incisional debridement of gunshot wounds, but their advice was largely discounted. Doubters dominated, and, until The Great War (World War I [WWI]), the technique of open exploration and debridement of wounds was deemed to be inappropriate and subject to unnecessary risk.4,5
WORLD WAR I
When the German, French, and Belgian armies settled into trench warfare near the Marne River, some 12 miles northeast of Paris, there was no pre-established system of triage along the front, extending some 500 miles, from Ypres and Flanders Fields in the north, to Alsace-Lorraine and the Franco-Swiss border in the south.6,7,8,9 Man-made trenches and underground bunkers (abri) became the norm, as the lines of engagement stabilized (Fig. 2). The trenches and abri were within range of machine-gun fire, heavy rifle shot, and mortar, fired from 150- and 210-mm howitzers. Notably, the trenches (and the men in them) were subject to the weather and flooding.8,9 A poem by Siegfried “Mad Jack” Sassoon well describes the horrors of mud and mortar, and the peril of retrieving the wounded in a 1918 Memorial Tablet10:
Figure 2.

Trenches were dug in the fertile farmland along the length of the front, interrupted only by underground bunkers, called abri, or other fortifications. The injured were carried through, around, or across the trenches to clearing stations. Planks across the trenches were called duckboards. The goal was to deliver the afflicted to clearing stations, some 500 to 1000 yards behind the line of entrenchment.
I died in Hell (they called it Passchendaele); my wound was slight.
And I was hobbling back; and then a shell burst slick upon the duckboards;
So I fell into the bottomless mud, and lost the light.
ANTOINE DE PAGE (1862 TO 1925)
Antoine De Page was born on November 28, 1862, to Elisabeth and Fredric De Page in the village of Boitsfort, near Brussels, Belgium, the seventh of nine children. De Page (pronounced de paj) earned his doctorate in medicine at the age of 25 from the University of Brussels and then studied anatomy and physiology for 3 years, in Prague.4 The follow-on training in Prague allowed De Page to visit the clinics of such giants as Thierch, Gusenbauer, and Billroth in Vienna, Austria.
On his return to Belgium in 1890, De Page joined the faculty at the University of Brussels. Within two decades, he had served as Chief of Surgical Services at University Hopital Saint-Jean and Hopital Saint-Pierre,4 culminating in his election to the Brussels Academie de Medicine in 1907.
Five years later, Queen Elisabeth of Belgium asked De Page to establish three Belgian hospitals in Constantinople, on the Gallipoli Peninsula, to receive the “walking wounded” from the Balkans War, a prelude to WWI. De Page carefully noted “the tendency for suppuration [in the wounds of war],11,12,13,14 especially when hurried surgeons intervene on the battlefield.” In April 1914, he offered instruction regarding the surgery of war to members of the International Society of Surgery in New York.15 De Page was unaware that his experience with Gallipoli wound care would be used in 3 to 4 months during WWI. Indeed, it was on August 14, 1914, that the invasion of Belgium was initiated; the loss of more than 250,000 German soldiers and 350,000 French, British, Australian, and Canadian soldiers at the Franco-Belgian front would follow.
On learning of the German invasion, De Page escaped from Brussels across the Franco-Belgian border into northeastern France.4 Several days later, he reached the coast and the town of Calais, overlooking the Strait of Dover (the narrowest point in the English Channel).
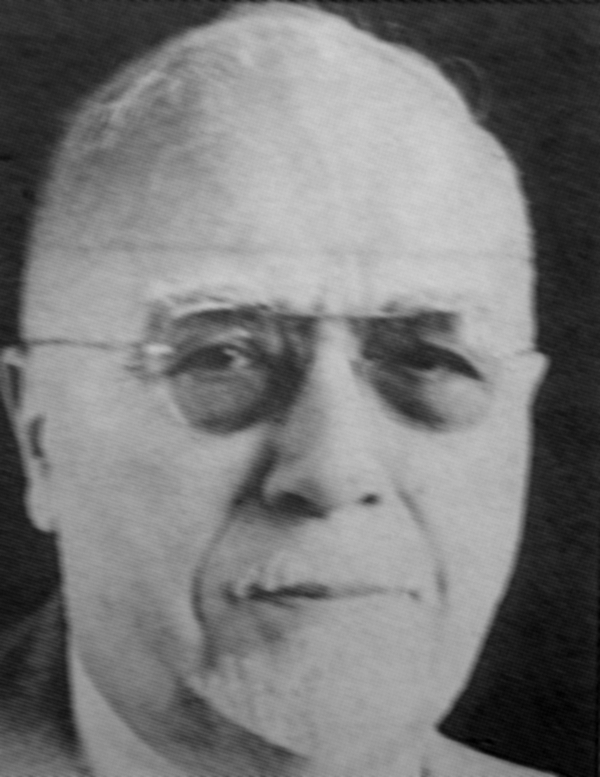
In due course, at the request of the Queen, De Page (then a colonel) (Fig. 3) created a military hospital at La Panne, Belgium, just north of the border with France. Tissue response to wounding by gunshot, the debridement and repair of insulted tissues, the differentiation of gangrene into four varieties, and an analysis of host defenses following infection4,11 were among the many disciplines studied at La Panne. De Page suggested the exploration of all war wounds, much like the French Empire surgeons before him. “Simple debridement,” he said, “was simply not enough”; “contaminated and contused tissue,” he indicated, “require excision, followed by open irrigation, using a Carrel reservoir16 and Dakin's solution.”
Figure 3.

Antoine De Page (1862–1925) is pictured in uniform, as a Colonel of the Belgian Army. His five-step, systematic evacuation of the injured (referred to as the “Ordre de Triage” by the author) was a noble feat, saving a multitude of lives. (Courtesy of the College of Physicians of Philadelphia.)
Most critically, De Page established a defined, orderly sequence to be followed in the evacuation of the injured.9,10,11,15 He recommended five steps of planned evacuation, which the author has coined “Ordre de Triage” [pronounced Order of Tree-uz] (Order of Triage).
First Order of Triage
The injured were to first be evacuated by stretcher to the nearest clearing station, by brancardiers (stretcher-bearers) under the cover of darkness (Fig. 4). Transit by day invited unfriendly fire from the German trenches and mortar from German-held higher ground, often only some 500 yards away.
Figure 4.
The injured were maneuvered through the archipelago of trenches by stretcher. Both bearers and the patient were potentially exposed above ground level to gun fire and mortar.
Second Order of Triage
On reaching the clearing stations at key locations along the front, dressings were to be applied to wounds, and a priority of evacuation was to be established before transport (Fig. 5). Major, even minor, surgery according to De Page was to be avoided at these early stages of engagement. In the presence of major bleeding or wounds of the thorax or abdomen, the soldier was immediately placed in a cart and wheeled to the nearest safe area that would allow the approach of an ambulance. The moderately injured were offered transport at night.
Figure 5.
At clearing stations wounds were dressed, and the priority of evacuation of the injured was determined. Most evacuations were achieved at night. The critically wounded were relayed along in the daylight, despite the increased exposure to unfriendly fire.
Third Order of Triage
Existing ambulances in Paris were under the purview of the Sanitary Service of Paris and were distinctly overwhelmed by the press of casualties. A Mr. Harjes of Morgan & Harjes Company, Bankers answered De Page's call for assistance by offering his private estate at Sandricourt, some 20 miles outside of Paris, as a cantonment for the ambulance corps (Fig. 6). There, the American Red Cross and Young Men's Christian Association (YMCA) provided driver training, classes in the Belgian and French languages, military drills, and lectures on the maintenance of ambulance vehicles. Ambulances were dispatched to “whisk” the injured away, taking them over shelled, pot-holed, dirt roads from the clearing stations to centers of more definitive care.17
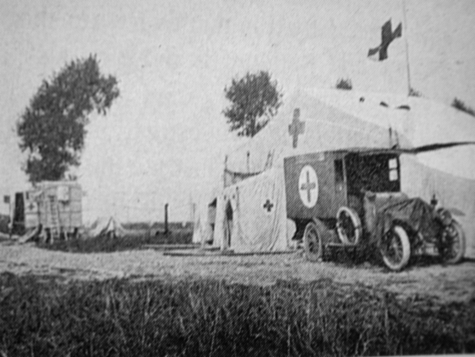
Figure 6.
The typical ambulance is pictured, awaiting dispatch to staging areas near the front line.
Fourth Order of Triage
As the fourth order, in a sequence of five, De Page established mobile centers for surgical urgent care, the postes avances des hospitaux du front. Each post consisted of four ambulances and an outfitted trailer17 and was the first stop for patients with acute hemorrhage and equally critical wounds of the thorax and the abdomen. Tents were provided for postoperative recovery (Fig. 7).
Figure 7.
A mobile surgical unit offered a fourth step in the triage of the injured. Acute hemorrhage was an indication for early intervention, as were open thoracic and abdominal wounds. The adjacent tents were used for initial recovery from surgery.
Fifth Order of Triage
Patients were evacuated to Paris, Versailles, Compiegne, La Panne, or other hospitals along the coast (Fig. 8), collectively considered the final level of triage. Some patients underwent reconstructive procedures at centers in metro Paris, such as Neuilly (Lycee Pasteur), and in metro London, such as Saint Hughes College, under the care of Morestin, Gillies, or Cushing, to name a few.18,19,20
Figure 8.
De Page assembled a military hospital at La Panne, along the Belgian Coast near the border with France. As was then typical, the hospital was established at a preexisting resort, in this case the Hotel de L'Ocean. The resort, seen in the background along the shoreline, was used to house surgeons, staff, and military units. The hospital complex, some 12 km behind the trenches, was U-shaped, with pavillons (wings) to favor the segregation of the wounded according to the complexity of their wounds. A building used for research of war-inflicted pathology is noted in the foreground, at the apex of the U-shaped hospital aggregate.
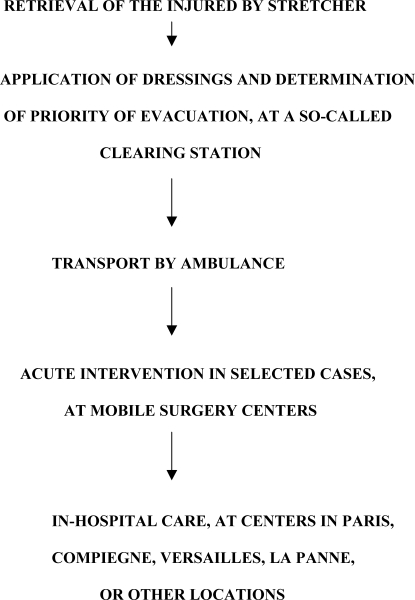
Approximately 40% of injured soldiers that reached this final level of triage had suffered artillery wounds, and another 40% had incurred wounds at the muzzle of small arms, according to tabulations published by Chalier and Glenard in 1916.21 Ten of 12 clothing samples taken from wounded soldiers revealed beta aerogenes, beta tetani, streptococcus, or staphylococcus; the cultures reflected the farmland of the area that had been cultivated and fertilized with manure for centuries.22 The Ordre De Page favored staged assessment and orderly intervention, in the care of the injured soldier, as depicted in the algorithm (Fig. 12) at the end of this article.
Figure 12.
Five steps, an Ordre de Triage (Order of Triage) as perceived by the author, were recommended by Antoine De Page, transferring soldier-care from the line of confrontation, to interim stations and eventually hospital care. De Page was aided by Robert Danis, a fellow countryman, in the third step (ambulance transport) of the orderly triage of the injured.
ROBERT DANIS (1880 TO 1962)
Recognizing the need for improved ambulance retrieval in the Belgian sector, De Page called on a fellow countryman and younger colleague, Robert Danis, for assistance.
Also born in Brussels, in 1880, Danis received his degree in medicine from the University of Brussels. He then became a general surgeon, working in the fields of thoracic and vascular surgery, and argued in his doctoral thesis (Anastomoses et Ligatures Vasculaires) that most secondary hemorrhage is caused by faulty operative technique and delayed infection.23,24
Like De Page, Danis had been displaced from Brussels by the invading German Army, and De Page called on him to organize the ambulance service (the Third Order of Triage) along the Franco-Belgian front. Purportedly, he visited the cantonment outside Paris at Sandricourt. Twenty ambulances with two men to a car constituted an Ambulance Section, under the leadership of an army Lieutenant. A chef, sous chef, several cooks, clerks, and a few mechanics were assigned to each section.
The ambulances were allocated in groups to one of several field bases at the rear of the front line. Because transport of the injured was to be achieved at night and because no lights were permitted on the vehicles, it was customary for one of the team to precede the ambulance and guide the vehicle around ubiquitous pot holes and other irregularities in the dirt roads. The member on foot, in front of the ambulance, wore a handkerchief on his back to guide the slow transit from the clearing station and back.17
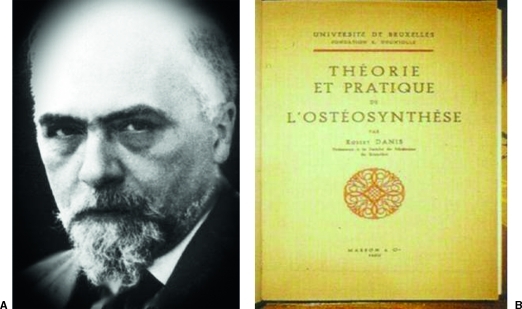
Danis (Fig. 9A) resumed his role as a general surgeon immediately after the war and was elected to the positions of Professor of Operative Surgery and Director of Gynecology at the University Hopital Saint-Pierre in metropolitan Brussels. There, he refined his approach to breast cancer and radical mastectomy.23,24
Figure 9.
(A) Robert Danis (1880–1962) is pictured during the postwar period, at which time his interest in osteosynthesis was paramount. (B) The 1932 text on osteosynthesis, best provided by axial compression, is pictured.
Danis (pronounced da-Nees) became interested in the process of bone healing. In two major published works—Technique de l'Osteosynthese, in 1932 (Fig. 9B) and Theorie et Pratique de l'Osteosynthese, in 1949—he stressed the need for interfragmentary compression if one is to achieve normal (callus-free) healing.25,26 He quite often quoted details of the turn-of-the-century publications of Alvin Lambotte to support his position.27 Danis listed four major principles of osteosynthesis:
Anatomical reduction is to be exact to allow implants used in the repair to exert long-lasting interfragmentary compression.
Compression is to be such that the postoperative movement of muscles and joints is unencumbered.
Immobilization with a cast is to be avoided because of the tendency to produce dystrophic (neuroligamentous) dysfunction.
Callus is to be considered a pathological structure (une formation pathologique) that can be readily avoided by osteosynthesis (don't l'osteosynthese permet souvent deja d eviter l'aparition).24
For rigid fixation, Danis typically applied double or crossed transosseous wire or chose screws with a wide thread to grasp the cancellous bone (vis helicoidale) of limb fractures. A myriad of other implants, such as special hip screws, bolts, and short nails with a V profile, were saved for special occasions.25
In a quest for even more refined implants, Danis turned to his workshop, as Lambotte had done before him, at the turn of the century,27 and two major achievements quickly surfaced. First, Danis developed and demonstrated techniques that would allow precise cortical screw-fixation after pretapping of the thread. Second, in 1938, he “constructed a plate (known as the coapteur) with which axial compression could be exerted.25 Its screws were anchored in both cortices.” In his 1949 text, Theorie et Pratique de l'Osteosynthese, Danis describes these newer implants and techniques, reporting their use in some 1500 cases.26
The concepts espoused by Danis regarding applied compression and bone healing were basic to subsequent research and clinical applications, particularly in regard to appliances for rigid fixation:
By Eggers (1948)28 when he demonstrated purposeful osteogenesis following the use of a so-called compressive “internal contact splint”;
By Charnley (Compression Arthrodesis, 1953)29; his observation that the majority of pseudoarthroses could be healed just by compression was revolutionary;
By Bagby and Janes30 (1958) when they developed their various bone compression plating systems; and
By the founders of the Association for the Study of Internal Fixation (ASIF)/AO (Arbeitsgemeinschaft für Osteosynthesefragen [in Swedish]), especially Muller and Allgower (1958), when new plating systems were taken through clinical testing and brought to market.31
Danis (Fig. 10) became President of the International Society of Surgery as his contributions became recognized worldwide and as the principles he espoused were increasingly accepted as applicable to operative intervention in surgery.
Figure 10.
Danis traveled extensively in his later years as the major contributions of callus-free healing achieved recognition. He is considered to be one of four forerunners of AO techniques perfected by the Association for the Study of Internal Fixation (ASIF) Swiss research group. The other three recognized forerunners were Lambotte, Kuntscher, and Bohler.24 (Picture courtesy of AO Foundation.)
Danis shared his innovations through speeches, publications, and film. During lectures, he frequently drew on the blackboard with both hands simultaneously. Painting, playing musical instruments, and cooking gourmet foods consumed his spare time. And, away from the operating theater, Robert Danis was seldom without a trusted tobacco pipe (Fig. 11).
Figure 11.
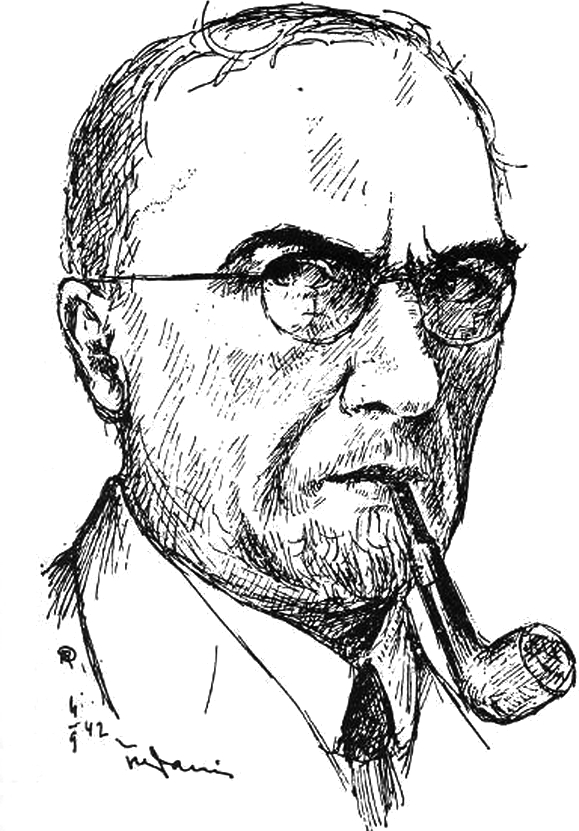
Danis, with an ever-present tobacco pipe, is depicted in this drawing. Innovations by Lambotte at the turn of the century and by Danis after World War I presaged the later strides in the stabilization and successful healing of fractures of the skeleton, supplemented by the works of Luhr, Spiessel, Champy, Muller, Allgower, Prein, and many others. (Picture courtesy of AO Foundation.)
FINANCIAL DISCLOSURE
The author is the Chairman of an AO Visiting Professorship each year at the University of Kentucky, which is partially funded by the AO Foundation.
References
- Wetzel D. A Duel of Giants: Bismarck, Napoleon III, and the Origins of the Franco-Prussian War. Madison, WI: University of Wisconsin Press; 2001.
- Wawro J. The Franco-Prussian War in 1870–1871. Cambridge: Cambridge University Press; 2003.
- Dorrance G M, (with collaboration of Bransfield JW) History of Treatment of Fractured Jaws. Philadelphia: 1941.
- Helling T S, Daon E. In Flanders Fields: the Great War, Antoine De Page, and the resurgence of debridement. Ann Surg. 1998;228:173–181. doi: 10.1097/00000658-199808000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruitt B A. Centennial changes in surgical care and research. Ann Surg. 2000;232:287–301. doi: 10.1097/00000658-200009000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falls C. The Great War. London: Longmans Green & Company; 1960.
- Morton D, Granatstein J L. Marching to Armageddon: Canadians and the Great War, 1914–1919. Toronto: Lester & Orpen Dennys Ltd; 1989.
- Winter J M. The Experience of World War I. London: Oxford University Press; 1989.
- Ellis J, Cox M. The World War I Databook: The Essential Facts and Figures for all the Combatants. London: Aurum Press; 1993.
- Sassoon S. War Poems. London: Heinemann; 1919.
- Depage A. War surgery. Ann Surg. 1914;40:137–142. doi: 10.1097/00000658-191408000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depage A. Des principes generaux du traitment des plaies suivant les formations sanitaires. Arch de Med et Pharm Mil. 1917;68:49–52. [Google Scholar]
- Depage A. Apercu clinique sur les effets compares de divers traitments de plaies de guerre: sommaire des recueils des travaus scientifiques de l'ambulance Ocean a La Panne, Fascicule II. Decembre 1917.
- Depage A. General considerations as to the treatment of war wounds. Ann Surg. 1919;69:575–588. doi: 10.1097/00000658-191906000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depage A. Les Ensignments de la Chirguries de Guerre (Instructions in the Surgery of War) New York: International Society of Surgery; 1914.
- Carrel A, Dehelly G. The Treatment of Infected Wounds. Child H, trans. New York: Paul B. Hoeber; 1917.
- Coyle E R. Ambulancing on the French Front. New York: Britton Publishing Company; 1918.
- Rogers B O. Hippolyte Morrestin (1869–1919). Part 1: a brief biography. Aesthetic Plast Surg. 1982;6:141. doi: 10.1007/BF01570633. [DOI] [PubMed] [Google Scholar]
- Gillies H D. Plastic Surgery of the Face, based on Selected Cases of War Injuries of the Face, including Burns. London: Oxford University Press; 1920.
- Cushing H. A study of a series of wounds involving the brain and its enveloping structures. Br J Surg. 1918;5:558–684. [Google Scholar]
- Chalier A, Glenard R. Les grandes blessures de guerre. Rev Chir. 1916;51:210. [Google Scholar]
- Fleming A. On the bacteriology of septic wounds. Lancet. 1915;2:638–643. [Google Scholar]
- Goverts J. Robert Danis: 1880–1962. Bruxelles Med. 1962;42:1001–1005. [Google Scholar]
- Heim U FA. The AO Phenomenon. Berlin: Hans Huber; 2001.
- Danis R. Technique de l'Osteosynthese. Paris: Masson et Cie; 1932.
- Danis R. Technique de l'Osteosynthese. 2nd ed. Paris: Masson et Cie; 1949.
- Lambotte A. L'Intervention Operatoire dans led Fractures. Paris: Masson et Cie; 1907.
- Eggers G WN. Internal contact splint. J Bone Joint Surg. 1948;30-A:40–52. [PubMed] [Google Scholar]
- Charnley J. Compression Arthrodesis. Edinburgh: Livingstone; 1953.
- Bagby G W, Janes J M. The effect of compression on the rate of fracture healing using a special plate. Am J Surg. 1958;95:761–771. doi: 10.1016/0002-9610(58)90625-1. [DOI] [PubMed] [Google Scholar]
- Muller M E, Allgower M. Zur behandlung der pseudoarthrose. Helv Chir Acta. 1958;25:253–262. [PubMed] [Google Scholar]