Abstract
Airway management in patients with maxillofacial trauma is complicated by injuries to routes of intubation, and the surgeon is frequently asked to secure the airway. Airway obstruction from hemorrhage, tissue prolapse, or edema may require emergent intervention for which multiple intubation techniques exist. Competing needs for both airway and surgical access create intraoperative conflicts during repair of maxillofacial fractures. Postoperatively, edema and maxillomandibular fixation place the patient at risk for further airway compromise.
Keywords: Airway obstruction, facial injuries, intubation, jaw fractures, laryngeal masks, mandibular fractures, maxillary fractures, maxillofacial injuries, tracheostomy
Patients with maxillofacial trauma present unique airway management challenges in the emergent, operative, and postoperative settings. The craniomaxillofacial surgeon is often asked to secure the airway in patients with severe facial injuries, and familiarity with available techniques allows for the most expedient and least morbid means of success. Orotracheal intubation remains the primary method of securing the emergent airway. Fiberoptic-assisted nasotracheal intubation has gained popularity in managing difficult airways despite traditional concern for intracranial penetration in patients with severe skull base injuries. Temporizing measures such as the laryngeal mask airway and esophageal/tracheal combination tube provide ventilation until a definitive airway can be obtained. When other measures fail, cricothyroidotomy is an expedient means of tracheal intubation.
Intraoperative maxillomandibular fixation often necessitates nasotracheal intubation. When nasoorbitoethmoid (NOE) fractures coexist with mandibular fractures, the nasotracheal tube interferes with operative correction. Tracheostomy and intraoperative exchanges between naso- and orotracheal intubation have traditionally been used in this subset of patients, yet surgeons have sought other methods to avoid the associated morbidity of these maneuvers. Submental and retromolar intubation maintain oral and nasal access while simultaneously avoiding tracheostomy.
Postoperative management of patients with maxillofacial trauma focuses on avoiding reintubation of the difficult airway. Maxillomandibular fixation affects respiratory parameters, and close monitoring of these patients is sometimes necessary. Efforts at eliminating difficult airway reintubations have led some anesthesiologists to use pediatric airway exchange catheters after extubation.
EMERGENT MANAGEMENT
Airway maintenance is the first step in the American College of Surgeons Advanced Trauma Life Support protocol.1 In a review of 1025 patients with facial fractures by Tung and colleagues, 17 (1.7%) emergently required establishment of a definitive airway secondary to airway obstruction.2 Thus, the majority of patients with maxillofacial trauma present with a stable airway, and simple monitoring of oxygenation via pulse oximetry is often all that is required. Although infrequent, the life-threatening nature of airway compromise mandates early identification of the patient subset that requires emergent or prophylactic airway control.
Guidelines for tracheal intubation issued by the Eastern Association for the Surgery of Trauma identify cervical spine injury, severe cognitive impairment, severe neck injury, severe maxillofacial injury and smoke inhalation as potential causes for airway obstruction.3 With regards to cognitive impairment, Advanced Trauma Life Support protocol recommends intubation of all patients with a Glasgow Coma Scale score of 8 or less. Airway obstruction directly related to maxillofacial trauma can be caused by tongue base or maxillary prolapse, pharyngeal edema or hematoma, and severe hemorrhage. Patients with bilateral mandibular body fractures are especially at risk for tongue base prolapse; tongue retraction with a heavy suture or towel clamp will allow oxygenation until a definitive airway is secured. Le Fort fractures may cause airway compromise via maxillary prolapse, edema, or hemorrhage. Ng and colleagues reported establishing an emergency airway in 22 (34%) of 64 patients presenting with Le Fort fractures; the severity of the Le Fort fracture also correlated with an increased need for intubation.4
Often the status of the cervical spine is unknown in the acute setting, and care must be taken to prevent inadvertent neurological injury.5 The incidence of cervical spine injury in the entire blunt trauma population is ∼1 to 3%.6,7 The exact relationship between maxillofacial trauma and cervical spine injuries is disputed. Some authors have demonstrated an increased risk of cervical spine injuries in patients with maxillofacial trauma compared with the entire blunt trauma population,8 whereas others have not.9,10 Davidson and Birdsell reviewed 2555 patients presenting with facial fractures and found cervical spine injury in 1.3%.11 When only patients sustaining injury in motor vehicle collisions were examined, however, the rate of concomitant cervical spine injury rose to 5.5%. Regardless, many level 1 trauma centers immobilize the entire spine in all blunt trauma patients until spinal injury can be disproved clinically and/or radiographically. The surgeon called on to emergently secure the airway must be cognizant of the cervical spine during all intubation maneuvers.
No consensus regarding the best means of intubation in patients with cervical spine injuries has been reached.7 Reports of rapid sequence induction, manual inline stabilization of the head, and orotracheal intubation via direct laryngoscopy have shown this to be a safe, successful maneuver.12 To attempt intubation via manual inline stabilization, the patient's head is placed in a neutral position and grasped at the mastoid processes by an assistant (Fig. 1). This serves to limit the natural head movement that occurs during direct laryngoscopy.
Figure 1.
Manual inline stabilization.
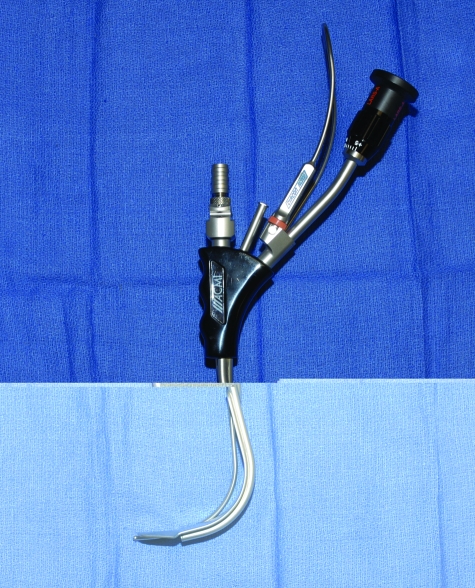
Other intubation tools that limit cervical motion include the Bullard laryngoscope (ACMI Corporation, Southborough, MA) and the flexible fiberoptic endoscope. The Bullard is a rigid laryngoscope (Fig. 2) whose anatomic blade design allows insertion and fiberoptic glottic visualization while maintaining a neutral head position. An attached stylet permits concomitant endotracheal tube insertion while a separate port allows for lidocaine injection or oxygenation. Improved ventilation provided by the larger port of the Bullard laryngoscope has been used during intubation of patients with maxillofacial trauma and immobilized cervical spines.13 Another option to both minimize head movement and avoid unsuccessful oral intubation in the sedated patient is fiberoptic nasotracheal intubation. Reports in patients with maxillofacial trauma, however, are sparse.3
Figure 2.
Bullard laryngoscope.
The conscious patient presenting with severe hemorrhage often presents a treatment dilemma with regards to cervical spine management. These patients will often struggle to sit up with their neck flexed and head down to clear blood and prevent aspiration.14 In these situations, the risk of airway compromise must be carefully balanced against the risk of spinal injury. Efforts to clinically clear the spine and/or place the patient in a semirigid cervical collar may hedge against potential neurological injury in these difficult circumstances.
Gunshot wounds to the face often present unique challenges in airway management due to significant tissue loss and, less frequently, associated hemorrhage. The need for emergent airway control in these patients ranges from 17 to 35% in recent reviews.15,16,17,18 Many authors recommend elective intubation even if the patient is initially stable to prevent delayed airway compromise, especially in patients with mandibular injury, oral bleeding or edema, and close-range shotgun wounds. Despite significant soft tissue loss, direct oral intubation can frequently be accomplished. If unsuccessful, some authors recommend fiberoptic nasotracheal intubation, cricothyroidotomy, and lastly, blind nasal intubation.19
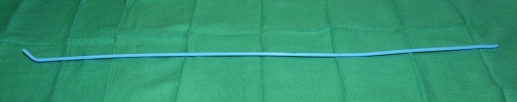
Regardless of the associated injuries, the primary means of securing the airway in the vast majority of acutely desaturating patients with maxillofacial trauma is orotracheal intubation via direct laryngoscopy.3 This has often already been performed by paramedics or emergency department personnel. For patients with severe trauma such as gunshot wounds or in whom attempts at intubation have failed, the surgeon may be called to intervene. Simple maneuvers may improve the success of orotracheal intubation. Suction is often necessary to clear pharyngeal secretions and bleeding. Visualization of the larynx may be improved with cricoid pressure by an assistant. In patients where visualization of the true vocal cords is still difficult, some have described the use of a gum elastic bougie (Fig. 3).20 This long introducer has an angled tip that is inserted beneath the epiglottis and advanced blindly through the glottis. Correct placement is confirmed by the distinctive feel of the tracheal rings; the patient is then intubated over the bougie. Video laryngoscopes, such as the GlideScope (Verathon, Inc., Bothell, WA), are promising new devices that allow visualization from the laryngoscope blade on a separate monitor21,22; their use in trauma patients has not yet been described (Fig. 4).
Figure 3.
Gum elastic bougie.
Figure 4.

GlideScope video laryngoscope. (Reprinted with permission from Verathon, Inc., Bothell, WA.)
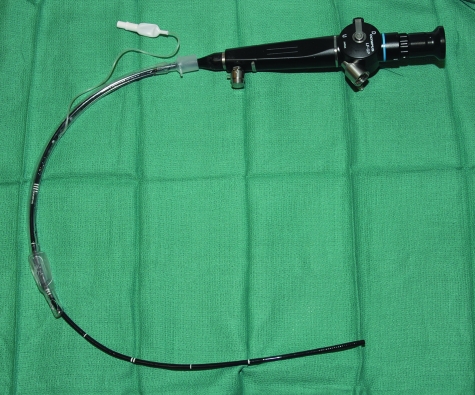
In patients with significant trismus due to associated mandible fractures, laryngoscopy is extremely difficult and other methods are necessary. Current widespread availability and use of fiberoptic endoscopes has made fiberoptic-assisted nasotracheal intubation a valuable asset in airway management. Many prefer this method for patients who are maintaining their oxygen saturation because it allows for awake intubation, thus avoiding potential airway emergencies in the anesthetized patient. An endotracheal tube is placed over a flexible fiberoptic bronchoscope and advanced to the handle (Fig. 5). The bronchoscope, in contrast to the nasolaryngoscope, provides the necessary length, a suction port to clear blood and/or secretions, and a port for injection of topical anesthetic. After the bronchoscope is directed through the vocal cords, the endotracheal tube is advanced into the airway over the scope. The endotracheal tube does not always advance easily secondary to nasal and laryngeal resistance. It is therefore important to maintain constant visualization of the trachea to prevent inadvertent scope displacement and possible esophageal intubation. The presence of an assistant to advance the endotracheal tube while the surgeon maintains tracheal visualization is helpful. Fiberoptic intubation can be accomplished orally or nasally, although the oral route requires greater skill in placement and is less well tolerated by the awake patient. Injection of topical anesthetic onto the true vocal cords is often necessary in the awake patient to prevent laryngospasm. If possible, having the patient sitting will result in less tongue base prolapse and, consequently, better visualization of the larynx.
Figure 5.
Fiberoptic bronchoscope with attached endotracheal tube.
Much controversy exists regarding nasotracheal intubation in the presence of skull base fractures. Multiple reports of intracranial placement of nasogastric,23,24 nasopharyngeal,25,26 and nasotracheal tubes27 with subsequent severe neurological sequelae or death have led many to condemn nasotracheal intubation in patients with extensive cribriform plate or sphenoid sinus fractures. Intracranial penetration from attempted nasotracheal intubation has also been reported after trans-sphenoidal pituitary surgery.28 All cases involved blind insertion of the nasotracheal tube; no intracranial placement during fiberoptic intubation has been reported. Despite these rare case reports, some authors continue to advocate blind nasotracheal intubation in patients with skull base fractures.29 For the surgeon attempting to secure the airway in patients with maxillofacial trauma, it would seem the risk, albeit small, of catastrophic, blind intracranial tube insertion is unnecessary when other options are available. However, if blind nasotracheal intubation is attempted, it is essential to direct the tube posteriorly along the nasal floor to avoid superior displacement. Placing a gloved finger through the mouth into the nasopharynx allows palpation of the advancing tube and facilitates proper pharyngeal positioning.
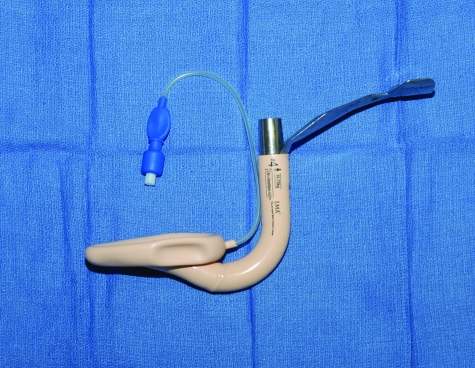
Additional choices for managing the emergent airway include the intubating laryngeal mask airway (LMA Fastrach, LMA North America, San Diego, CA), esophageal/tracheal double lumen airway (Combitube, Tyco Healthcare Group LP, Pleasanton, CA), lighted stylet, and retrograde intubation. The laryngeal mask airway is placed blindly through the mouth and seals off the hypopharynx via a circumferential inflatable cuff; this design may prevent aspiration of cephalad bleeding but not of gastric contents.30 Ventilation is accomplished without actually intubating the trachea. The related intubating laryngeal mask airway (ILMA) (Fig. 6) is designed to allow subsequent passage of an endotracheal tube with detachable anesthesia circuit connector (LMA ET Tube, LMA North America, San Diego, CA). Successful emergent use of the ILMA has been described in a patient with maxillofacial trauma.31 Its ease of insertion and subsequent ability to blindly intubate the trachea may be advantageous when direct laryngoscopic intubation fails.
Figure 6.
Intubating laryngeal mask airway.
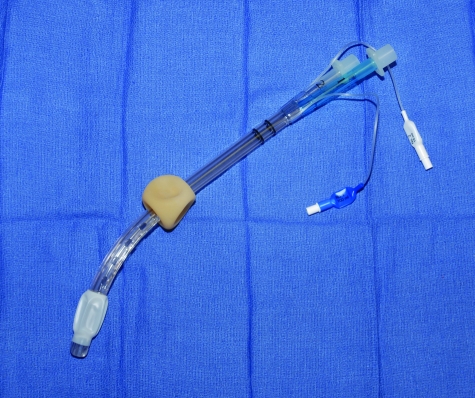
The esophageal/tracheal combination (ETC) tube is a dual lumen, dual cuff tube that is blindly inserted into the esophagus (Fig. 7). The distal, smaller balloon is inflated within the esophagus and may prevent reflux of gastric contents. The proximal, larger balloon seals off the oropharynx and allows ventilation via perforations between the two cuffs. Similar to the ILMA, ventilation is accomplished without direct tracheal intubation. However, if the ETC is inadvertently placed into the trachea, ventilation can still be performed via the second lumen. Successful use of this device by paramedics has been described in patients with maxillofacial trauma after unsuccessful attempts at endotracheal intubation.32,33 Rare complications include piriform sinus and esophageal perforations.34 Disadvantages of the ETC compared with the ILMA include an inability to perform definitive tracheal intubation without removal. Nevertheless, it may provide a facile means of ventilation in patients with maxillofacial trauma.
Figure 7.
Esophageal/tracheal Combitube.
The lighted stylet represents another option for difficult intubations in patients with maxillofacial trauma. The stylet is bent 90 to 120 degrees ∼3 to 6 cm from the distal end and is then blindly introduced into the hypopharynx.35 Correct positioning produces an ambient glow in the midline at about the level of the hyoid bone; transillumination off the midline signifies malposition within the piriform sinus. The endotracheal tube is then advanced, sometimes employing a rocking motion to direct the tube beneath the epiglottis. A continuous glow accompanies tracheal intubation, whereas a brief interruption and subsequent recovery indicates esophageal intubation. Although most often accomplished with the patient's head extended, lighted stylet intubation can be performed in cervically immobilized patients. The lighted stylet can also be used for nasotracheal intubation, and successful application in patients with maxillofacial trauma has been reported.36
Yet another method of intubation that has been successfully employed in patients with maxillofacial trauma is retrograde intubation.37,38 A large bore Angiocath (14 to 18 gauge) is inserted at an ∼45-degree angle through the cricothyroid membrane or the proximal trachea; aspiration of air confirms placement. The catheter is advanced and the needle removed. A long guidewire is then inserted through the catheter and advanced out the nose or retrieved from the mouth with Magill forceps. The endotracheal tube is advanced over the wire via the side port, or Murphy's eye, or pulled by tying the tube to the wire's end. Decreased resistance to intubation may be accomplished by first advancing a tube exchanger, removing the wire, and then intubating over the exchanger.
When attempts at intubation or ventilation have failed, cricothyroidotomy is considered the procedure of choice.3 The relative ease in locating the cricothyroid membrane and its proximity to the skin allow more expedient dissection compared with emergent tracheostomy. In a review of 8320 trauma admissions, Salvino and colleagues reported performing 30 (0.4%) cricothyroidotomies for emergent airway control.39 Studies requiring emergent cricothyroidotomy or tracheostomy for patients specifically with maxillofacial trauma report rates from 0.1 to 3.3%.2,40 Often the decision to perform a cricothyroidotomy is made after failure of previous attempts at oro- or nasotracheal intubation, although it may also be the initial maneuver used to secure the airway. Studies reveal 15 to 23% of emergent cricothyroidotomies as the first and only means of airway control.39,41 Reported indications include excessive emesis or hemorrhage, known cervical spine fracture, and inability to visualize the vocal cords. Cricothyroidotomy is contraindicated in pediatric patients due to anatomic constraints and in patients with suspected laryngotracheal separation.
OPERATIVE MANAGEMENT
Intraoperative airway management of patients with maxillofacial trauma is complicated by competing needs for airway and surgical access. Often, the preferred route for endotracheal tube placement prevents or interferes with surgical intervention. For patients with severe panfacial injuries, intraoperative endotracheal tube changes and tracheostomy remain common means of managing the airway. However, techniques such as submental and retromolar intubation have recently been espoused to eliminate the morbidity associated with tracheostomy as well as the risk of intraoperative tube repositioning.
Maxillomandibular fixation is often employed intraoperatively when correcting both mandibular and maxillary fractures, and, therefore, nasotracheal intubation remains the preferred technique in these patients. Preformed curved nasotracheal tubes may be used to minimize operative field interference but vary in their degree of protrusion from the nose depending on the patient's anatomy. More precise methods of tube placement use curved, metal anesthesia circuit connectors. After successful nasotracheal intubation, the plastic connector is removed and the endotracheal tube grasped with hemostats at the naris. The tube is then cut ∼1 cm above the hemostats and a curved 60- to 90-degree connector is attached (Fig. 8). The airway circuit is then supported on the forehead and fixed with tape and/or a circumferential head dressing. This results in minimal intrusion of the tube into the operative field.
Figure 8.
Curved endotracheal tube connector.
Patients with coexisting jaw and NOE fractures present additional challenges, and, consequently, various airway management techniques have been employed. A nasotracheal tube interferes with correction of septal and NOE fractures and may be breeched during surgery on the midface.42 One solution is to simply switch from nasal to oral intubation intraoperatively. After completion of internal fixation of jaw fractures and release of maxillomandibular fixation, the patient is nasally extubated and reintubated orally. Multiple creative methods of switching from naso- to orotracheal intubation without actual extubation have also been described.43,44,45 None of these maneuvers is ideal because they all interrupt the surgical procedure and risk the loss of a previously secure airway. As a result, many surgeons advocate tracheostomy before correcting extensive panfacial fractures.
Before the widespread application of rigid plating techniques, postoperative maxillomandibular fixation was frequently necessary to ensure proper occlusion. Maxillomandibular fixation combined with severe edema in patients with extensive panfacial injuries necessitated tracheostomy to protect against postoperative airway compromise. The advent of rigid internal fixation often allowed the release of maxillomandibular fixation before extubation and, consequently, avoidance of tracheostomy in more patients.46 Nevertheless, a standard tracheostomy before surgery provides a safe, stable airway that does not interfere with the operative field and protects against postoperative airway obstruction secondary to surgical manipulation. Possible intraoperative airway compromise during endotracheal tube exchanges is avoided. In the presence of severe neurological and/or cardiopulmonary injury, which will result in the need for continued ventilatory support after surgery, elective tracheostomy certainly provides the safest means of airway maintenance with the least morbidity. Yet for patients with maxillofacial trauma who do not require long-term ventilation, many surgeons continued to search for methods of avoiding tracheostomy.
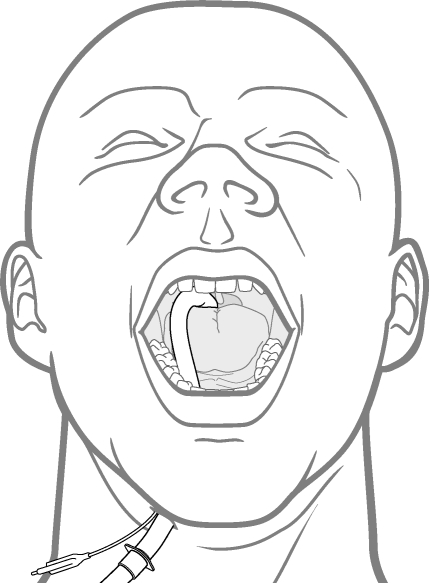
Submental intubation was first described by Hernández in 1986 and was designed to eliminate the morbidity of tracheostomy in patients undergoing maxillofacial surgery.47 The patient is first intubated orally with a reinforced endotracheal tube. The original description places an incision within the submandibular triangle (contrary to the name, submental intubation), parallel to and one finger's breadth below the mandibular border (Fig. 9). The side opposite any body or angle fractures is chosen if possible. Incisions below the mandibular angle48 and within the midline49,50 have also been described. Dissection is then carried bluntly through the mylohyoid and along the inner mandibular cortex; subperiosteal versus extraperiosteal dissection is debated. The floor of mouth mucosa is then incised over the dissecting instrument. The pilot balloon and endotracheal tube without connector are pulled through the incision while the tube is stabilized to prevent inadvertent extubation. Some authors have advocated using endotracheal tubes with detachable connectors such as that designed for the intubating laryngeal mask airway.51,52 After reattaching the connector and hooking up the anesthesia circuit, the tube is sutured to the skin. The endotracheal tube can be brought back into the mouth before extubation, although extubation directly through the submental incision has been described.49,52
Figure 9.
Submental intubation.
Proponents of submental intubation cite more aesthetic scars, avoidance of morbidity associated with tracheostomies, and minimal complications. In a review by Caron and colleagues of 25 patients with maxillofacial trauma treated with submental intubation, 1 (4%) patient developed cellulitis at the incision site.53 Meyer and colleagues reported 1 (4%) patient with hypertrophic scarring and 2 (8%) patients with floor of mouth abscesses in their series of 25 patients with maxillofacial trauma.54 Anwer and colleagues reported 2 of 14 (14%) patients with postoperative superficial skin infections.48 Other possible disadvantages include submandibular gland, Wharton's duct, lingual nerve injury, and orocutaneous fistula formation. Additionally, increased sedation may be necessary due to the oral route of tube placement in patients who require long-term ventilation.
Perhaps the simplest and least morbid technique of avoiding tracheostomy in patients with panfacial fractures is retromolar intubation. After oral intubation in patients with missing or impacted third molars, a reinforced endotracheal tube can be passed through the retromolar space and secured to an adjacent tooth with dental wire.55 Patients who can close their jaws after introducing an index finger into the retromolar space likely have adequate room for this maneuver. Some authors have described concurrent third molar extraction56 and bone removal57 to enable retromolar intubation, although the latter method seems to add further morbidity to a technique designed to avoid it. Children are well suited for this method; Arora and colleagues reported 79 of 80 (99%) pediatric patients could accommodate a retromolar endotracheal tube while maintaining centric occlusion.58 No reports using retromolar intubation indicate difficulty with placement of maxillomandibular fixation.
POSTOPERATIVE MANAGEMENT
Patients with extensive maxillofacial trauma who are maintained in maxillomandibular fixation after surgery should be carefully monitored while in the hospital. Studies have predictably demonstrated increased respiratory obstruction in patients with maxillomandibular fixation59,60 and, therefore, they should be placed on continuous pulse oximetry. Steroids may be considered to decrease postoperative edema and improve respiratory status. Wire cutters or scissors must be placed at the bedside and, more important, ancillary staff should be taught which wires to cut if significant dyspnea or severe nausea/vomiting develops.
A unique means of avoiding difficult postoperative reintubations is via placement of a pediatric airway exchange catheter. Before extubation, this catheter is inserted through the oro- or nasotracheal tube with care taken to ensure placement above the carina. Extubation is then performed over the catheter, leaving it within the airway. It is then secured to the head and used for oxygen delivery if necessary. Surprisingly, tolerance of the catheter is quite high with reports ranging from 94 to 97%.61,62 Reintubation is performed over the catheter and has been uniformly successful in published accounts.
CONCLUSIONS
Management of patients with maxillofacial trauma presents difficulties specific to injuries of the upper airway. Multiple options exist for securing the emergent airway, and specific interventions will depend on the availability of instruments and experience of practitioners in each setting. Each technique has certain advantages and limitations; when properly applied, the airway can be secured with minimal morbidity. The decision to perform cricothyroidotomy must be made on an individual basis, and some patients may still require it as the initial intervention. Intraoperatively, fracture patterns will dictate routes of intubation. Newer options such as submental and retromolar intubation are gaining popularity. Postoperative vigilance must be high for patients who are still in maxillomandibular fixation. Difficult airways may benefit from placement of airway exchange catheters before extubation.
References
- American College of Surgeons. Committee on Trauma Advanced Trauma Life Support Program for Doctors. 7th ed. Chicago: American College of Surgeons; 2004.
- Tung T C, Tseng W S, Chen C T, et al. Acute life-threatening injuries in facial fracture patients: a review of 1,025 patients. J Trauma. 2000;49:420–424. doi: 10.1097/00005373-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Dunham C M, Barraco R D, Clark D E, et al. Guidelines for emergency tracheal intubation immediately after traumatic injury. J Trauma. 2003;55:162–179. doi: 10.1097/01.ta.0000083335.93868.2c. [DOI] [PubMed] [Google Scholar]
- Ng M, Saadat D, Sinha U K. Managing the emergency airway in Le Fort fractures. J Craniomaxillofac Trauma. 1998;4:38–43. [PubMed] [Google Scholar]
- Kellman R. The cervical spine in maxillofacial trauma: assessment and airway management. Otolaryngol Clin North Am. 1991;24:1–13. [PubMed] [Google Scholar]
- Goldberg W, Mueller C, Panacek E, et al. Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. 2001;38:17–21. doi: 10.1067/mem.2001.116150. [DOI] [PubMed] [Google Scholar]
- Crosby E T. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104:1293–1318. doi: 10.1097/00000542-200606000-00026. [DOI] [PubMed] [Google Scholar]
- Hackl W, Hausberger K, Sailer R, et al. Prevalence of cervical spine injuries in patients with facial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:370–376. doi: 10.1067/moe.2001.116894. [DOI] [PubMed] [Google Scholar]
- Hills M W, Deane S A. Head injury and facial injury: is there an increased risk of cervical spine injury? J Trauma. 1993;34:549–553. [PubMed] [Google Scholar]
- Beirne J C, Butler P E, Brady F A. Cervical spine injuries in patients with facial fractures: a 1-year prospective study. Int J Oral Maxillofac Surg. 1995;24:26–29. doi: 10.1016/s0901-5027(05)80852-5. [DOI] [PubMed] [Google Scholar]
- Davidson J S, Birdsell D C. Cervical spine injury in patients with facial skeletal trauma. J Trauma. 1989;29:1276–1278. doi: 10.1097/00005373-198909000-00016. [DOI] [PubMed] [Google Scholar]
- Criswell J C, Parr M JA, Nolan J C. Emergency airway management in patients with cervical spine injuries. Anaesthesia. 1994;49:900–903. doi: 10.1111/j.1365-2044.1994.tb04271.x. [DOI] [PubMed] [Google Scholar]
- Ghouri A F, Bernstein C A. Use of the Bullard laryngoscope blade in patients with maxillofacial injuries. Anesthesiology. 1996;84:490. doi: 10.1097/00000542-199602000-00054. [DOI] [PubMed] [Google Scholar]
- Perry M, Dancey A, Mireskandari K, et al. Emergency care in facial trauma: a maxillofacial and ophthalmic perspective. Injury. 2005;36:875–896. doi: 10.1016/j.injury.2004.09.018. [DOI] [PubMed] [Google Scholar]
- Dolin J, Scalea T, Mannor L, et al. The management of gunshot wounds to the face. J Trauma. 1992;33:508–514. doi: 10.1097/00005373-199210000-00004. [DOI] [PubMed] [Google Scholar]
- Kihtir T, Ivatury R R, Simon R J, et al. Early management of civilian gunshot wounds to the face. J Trauma. 1993;35:569–575. doi: 10.1097/00005373-199310000-00012. [DOI] [PubMed] [Google Scholar]
- Chen A Y, Stewart M G, Raup G. Penetrating injuries of the face. Otolaryngol Head Neck Surg. 1996;115:464–470. doi: 10.1177/019459989611500519. [DOI] [PubMed] [Google Scholar]
- Demetriades D, Chahwan S, Gomez H, et al. Initial evaluation and management of gunshot wounds to the face. J Trauma. 1998;45:39–41. doi: 10.1097/00005373-199807000-00007. [DOI] [PubMed] [Google Scholar]
- McLean J N, Moore C E, Yellin S A. Gunshot wounds to the face: acute management. Facial Plast Surg. 2005;21:191–198. doi: 10.1055/s-2005-922859. [DOI] [PubMed] [Google Scholar]
- Jabre P, Combes X, Leroux B, et al. Use of gum elastic bougie for prehospital difficult intubation. Am J Emerg Med. 2005;23:552–555. doi: 10.1016/j.ajem.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Sun D A, Warriner B, Parsons D G, et al. The GlideScope video laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384. doi: 10.1093/bja/aei041. [DOI] [PubMed] [Google Scholar]
- Cooper R M, Pacey J A, Bishop M J, McCluskey S A. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198. doi: 10.1007/BF03027728. [DOI] [PubMed] [Google Scholar]
- Ferreras J, Junquera L M, Garcia-Consuegra L. Intracranial placement of a nasogastric tube after severe craniofacial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:564–566. doi: 10.1067/moe.2000.110032. [DOI] [PubMed] [Google Scholar]
- Genu P R, de Oliveira D M, Vasconcellos R J, et al. Inadvertent intracranial placement of a nasogastric tube in a patient with severe craniofacial trauma: a case report. J Oral Maxillofac Surg. 2004;62:1435–1438. doi: 10.1016/j.joms.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Schade K, Borzotta A, Michaels A. Intracranial malposition of nasopharyngeal airway. J Trauma. 2000;49:967–968. doi: 10.1097/00005373-200011000-00032. [DOI] [PubMed] [Google Scholar]
- Martin J E, Mehta R, Aarabi B, et al. Intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma. Mil Med. 2004;169:496–497. doi: 10.7205/milmed.169.6.496. [DOI] [PubMed] [Google Scholar]
- Marlow T J, Goltra D D, Jr, Schabel S I. Intracranial placement of a nasotracheal tube after facial fracture: a rare complication. J Emerg Med. 1997;15:187–191. doi: 10.1016/s0736-4679(96)00356-3. [DOI] [PubMed] [Google Scholar]
- Paul M, Dueck M, Kampe S, Petzke F, Ladra A. Intracranial placement of a nasotracheal tube after transnasal trans-sphenoidal surgery. Br J Anaesth. 2003;91:601–604. doi: 10.1093/bja/aeg203. [DOI] [PubMed] [Google Scholar]
- Rosen C L, Wolfe R E, Chew S E, et al. Blind nasotracheal intubation in the presence of facial trauma. J Emerg Med. 1997;15:141–145. doi: 10.1016/s0736-4679(96)00355-1. [DOI] [PubMed] [Google Scholar]
- Rollert M K. The case against the laryngeal mask airway for anesthesia in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2004;62:739–741. doi: 10.1016/j.joms.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Mason A M. Use of the intubation laryngeal mask airway in pre-hospital care: a case report. Resuscitation. 2001;51:91–95. doi: 10.1016/s0300-9572(01)00376-8. [DOI] [PubMed] [Google Scholar]
- Blostein P A, Koestner A J, Hoak S. Failed rapid sequence intubation in trauma patients: esophageal tracheal Combitube is a useful adjunct. J Trauma. 1998;44:534–537. doi: 10.1097/00005373-199803000-00021. [DOI] [PubMed] [Google Scholar]
- Davis D P, Valentine C, Ochs M, Vilke G M, Hoyt D B. The Combitube as a salvage airway device for paramedic rapid sequence intubation. Ann Emerg Med. 2003;42:697–704. doi: 10.1016/s0196-0644(03)00396-2. [DOI] [PubMed] [Google Scholar]
- Smith C E, DeJoy S J. New equipment and techniques for airway management in trauma. Curr Opin Anaesthesiol. 2001;14:197–209. doi: 10.1097/00001503-200104000-00012. [DOI] [PubMed] [Google Scholar]
- Davis L, Cook-Sather S D, Schreiner M S. Lighted stylet tracheal intubation: a review. Anesth Analg. 2000;90:745–756. doi: 10.1097/00000539-200003000-00044. [DOI] [PubMed] [Google Scholar]
- Verdile V P, Heller M B, Paris P M, Stewart R D. Nasotracheal intubation in traumatic craniofacial dislocation: use of the lighted stylet. Am J Emerg Med. 1988;6:39–41. doi: 10.1016/0735-6757(88)90203-3. [DOI] [PubMed] [Google Scholar]
- King H K, Huntington C, Wooten D J. Translaryngeal guided intubation in an uncooperative patient with maxillofacial injury: case report. J Trauma. 1994;36:885–886. doi: 10.1097/00005373-199406000-00022. [DOI] [PubMed] [Google Scholar]
- Weksler N, Klein M, Weksler D, et al. Retrograde tracheal intubation: beyond fibreoptic endotracheal intubation. Acta Anaesthesiol Scand. 2004;48:412–416. doi: 10.1111/j.0001-5172.2004.00347.x. [DOI] [PubMed] [Google Scholar]
- Salvino C K, Dries D, Gamelli R, et al. Emergency cricothyroidotomy in trauma victims. J Trauma. 1993;34:503–505. doi: 10.1097/00005373-199304000-00006. [DOI] [PubMed] [Google Scholar]
- Taicher S, Givol N, Peleg M, Ardekian L. Changing indications for tracheostomy in maxillofacial trauma. J Oral Maxillofac Surg. 1996;54:292–295. doi: 10.1016/s0278-2391(96)90744-2. [DOI] [PubMed] [Google Scholar]
- Isaacs J H, Jr, Pedersen A D. Emergency cricothyroidotomy. Am Surg. 1997;63:346–349. [PubMed] [Google Scholar]
- Gentili M E, Calves Y, Bedhet N. Breeches in a nasotracheal tube: hazard of maxillofacial surgery. Eur J Anaesthesiol. 1999;16:207–208. [PubMed] [Google Scholar]
- Werther J R, Richardson G, McIlwain M R. Nasal tube switch: converting from a nasal to an oral endotracheal tube without extubation. J Oral Maxillofac Surg. 1994;52:994–996. doi: 10.1016/s0278-2391(10)80090-4. [DOI] [PubMed] [Google Scholar]
- Patteson S K, Epps J L, Hall J. Simultaneous oral and nasal tracheal intubation utilizing a fiberoptic scope in a patient with facial trauma. J Clin Anesth. 1996;8:258–259. doi: 10.1016/0952-8180(96)00022-0. [DOI] [PubMed] [Google Scholar]
- Salibian H, Jain S, Gabriel D, Azocar R J. Conversion of an oral to nasal orotracheal intubation using an endotracheal tube exchanger. Anesth Analg. 2002;95:1822. doi: 10.1097/00000539-200212000-00077. [DOI] [PubMed] [Google Scholar]
- Kellman R M, Schilli W. Plate fixation of fractures of the mid and upper face. Otolaryngol Clin North Am. 1987;20:559–572. [PubMed] [Google Scholar]
- Hernández Altemir F. The submental route for endotracheal intubation: a new technique. J Maxillofac Surg. 1986;14:64–65. doi: 10.1016/s0301-0503(86)80261-2. [DOI] [PubMed] [Google Scholar]
- Anwer H MF, Zeitoun I M, Shehata E AA. Submandibular approach for tracheal intubation in patients with panfacial fractures. Br J Anaesth. 2007;98:835–840. doi: 10.1093/bja/aem094. [DOI] [PubMed] [Google Scholar]
- MacInnis E, Baig M. A modified submental approach for oral endotracheal intubation. Int J Oral Maxillofac Surg. 1999;28:344–346. [PubMed] [Google Scholar]
- Davis C. Submental intubation in complex craniomaxillofacial trauma. ANZ J Surg. 2004;74:379–381. doi: 10.1111/j.1445-1433.2004.02995.x. [DOI] [PubMed] [Google Scholar]
- Ball D R, Clark M, Jefferson P, Stewart T. Improved submental intubation. Anaesthesia. 2003;58:189. [PubMed] [Google Scholar]
- Kim K J, Lee J S, Kim H J, et al. Submental intubation with reinforced tube for intubating laryngeal mask airway. Yonsei Med J. 2005;46:571–574. doi: 10.3349/ymj.2005.46.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron G, Paquin R, Lessard M R, et al. Submental endotracheal intubation: an alternative to tracheotomy in patients with midfacial and panfacial fractures. J Trauma. 2000;48:235–240. doi: 10.1097/00005373-200002000-00007. [DOI] [PubMed] [Google Scholar]
- Meyer C, Valfrey J, Kjartansdottir T, et al. Indication for and technical refinements of submental intubation in oral and maxillofacial surgery. J Craniomaxillofac Surg. 2003;31:383–388. doi: 10.1016/j.jcms.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Malhotra N. Retromolar intubation: a simple alternative to submental intubation. Anaesthesia. 2006;61:515–516. doi: 10.1111/j.1365-2044.2006.04635.x. [DOI] [PubMed] [Google Scholar]
- Gibbons A J, Hope D A, Silvester K C. Oral endotracheal intubation in the management of midfacial fractures. Br J Oral Maxillofac Surg. 2003;41:259–260. doi: 10.1016/s0266-4356(03)00114-1. [DOI] [PubMed] [Google Scholar]
- Martinez-Lage J L, Eslava J M, Cebrecos A I, Marcos O. Retromolar intubation. J Oral Maxillofac Surg. 1998;56:302–306. doi: 10.1016/s0278-2391(98)90103-3. [DOI] [PubMed] [Google Scholar]
- Arora S, Rattan V, Bhardwaj N. An evaluation of the retromolar space for oral tracheal tube placement for maxillofacial surgery in children. Anesth Analg. 2006;103:1122–1126. doi: 10.1213/01.ane.0000247852.09732.ec. [DOI] [PubMed] [Google Scholar]
- Kohno M, Nakajima T, Someya G. Effects of maxillomandibular fixation on respiration. J Oral Maxillofac Surg. 1993;51:992–996. doi: 10.1016/s0278-2391(10)80042-4. [DOI] [PubMed] [Google Scholar]
- Yamaguchi H. Effects of intermaxillary fixation during orthognathic surgery on respiratory function after general anesthesia. Anesth Prog. 2001;48:125–129. [PMC free article] [PubMed] [Google Scholar]
- Loudermilk E P, Hartmannsgruber M, Stoltzfus D P, Langevin P B. A prospective study of the safety of tracheal extubation using a pediatric airway exchange catheter for patients with a known difficult airway. Chest. 1997;111:1660–1665. doi: 10.1378/chest.111.6.1660. [DOI] [PubMed] [Google Scholar]
- Dosemeci L, Yilmaz M, Yegin A, et al. The routine use of pediatric airway exchange catheter after extubation of adult patients who have undergone maxillofacial or major neck surgery: a clinical observational study. Crit Care. 2004;8:R385–R390. doi: 10.1186/cc2956. [DOI] [PMC free article] [PubMed] [Google Scholar]