Abstract
Objective
To determine the efficacy of a 2-year obesity prevention intervention in African-American girls.
Design
Memphis GEMS (Girls health Enrichment Multi-site Studies) was a controlled trial in which girls were randomly assigned to an obesity prevention or alternative intervention.
Setting
Local community centers and YMCAs in Memphis, Tennessee.
Participants
Girls ages 8-to-10 years (n=303) who were identified by a parent as African-American and had body mass index (BMI) ≥25th percentile for age or one parent with BMI ≥25 kg/m2.
Interventions
Group behavioral counseling to promote healthy eating and increased physical activity (obesity prevention intervention) or self-esteem and social efficacy (alternative intervention).
Main Outcome Measure
BMI at 2 years.
Results
BMI increased in all girls with no treatment effect (obesity prevention minus alternative) at 2 years (0.09, 95% CI: −0.40, 0.58) kg/m2. Two-year treatment effects in the expected direction were observed for servings/day of sweetened beverages (−0.19, 95% CI=−0.39, 0.09), water (0.21, 95% CI=0.03, 0.40), and vegetables (0.15, 95% CI=−0.02, 0.30), but there were no effects on physical activity. Post-hoc analyses suggested a treatment effect in younger girls (interaction P=.081). BMI difference at 2 years was −2.41 [−4.38, 0.02] in girls initially aged 8 and −1.02 [−2.31, 0.27] kg/m2 in those initially aged 10.
Conclusions
The lack of significant BMI change at 2 years indicates that this intervention alone is insufficient for obesity prevention. Effectiveness may require more explicit behavioral change goals and a stronger physical activity component as well as supportive changes in environmental contexts.
Keywords: children, physical activity, diet, health disparities, randomized controlled trial, GEMS, weight gain
Childhood obesity is a worldwide health concern1 given its high incidence, increasing prevalence, and associated health consequences during childhood and later in adulthood.2, 3 Among U.S. children ages 6–11 years, obesity prevalence has increased almost four-fold over the past three decades, from about 5% to 19%.4, 5
Obesity prevalence in African-American girls has increased more steeply relative to white girls,6 and was 24%-28% in the 2003–2006 National Health and Nutrition Examination Survey.7 The need for effective interventions targeting this high-risk population is, therefore, a particularly high public health priority.8 The Girls health Enrichment Multi-site Studies (GEMS) program sought to address this need through development and evaluation of culturally appropriate obesity prevention approaches in pre-adolescent African-American girls. The GEMS program began in 1999 with a three-year feasibility and pilot studies phase (Phase 1) during which measurements and separate interventions were developed and pilot-tested (but not powered to detect significant effects on BMI) at four research centers.9–13 In Phase 2, two-year efficacy trials were conducted at two centers, Stanford and Memphis, which tested separate interventions, in collaboration with the National Heart, Lung, and Blood Institute.14, 15 This paper reports the results of the Memphis GEMS Phase 2 obesity prevention trial.
Methods
Research Design
Details of the Memphis GEMS trial design have been reported.14 GEMS evaluated an obesity prevention intervention in 303 pre-adolescent African-American girls and their primary caregiver in comparison to an alternative intervention that was not expected to affect diet, physical activity or body weight. The primary outcome was BMI at 2 years. Secondary outcomes were anthropometric and other measures of body composition, diet and physical activity at 1- and 2-years of follow-up.
Recruitment and Eligibility
Recruitment occurred over 5 waves primarily through television and radio ads, and through flyers and presentations in the community. Advertisements described GEMS as a study of healthy growth. To be eligible, girls had to be identified as African-American or black by their parent/caregiver, be age 8–10 years, have BMI ≥25th age-sex specific percentile,16 or have at least one parent with BMI ≥25 kg/m2. Girls were excluded if they had BMI >35 kg/m2 or conditions that would affect their growth or limit participation in the study.
Caregivers gave written informed consent and girls provided assent. The protocol was reviewed by an independent Data and Safety Monitoring Board and approved by the University of Memphis Institutional Review Board and the National Heart, Lung, and Blood Institute.
Interventions
The rationale and development of the GEMS obesity prevention intervention are described elsewhere.14, 17 During the first year, both interventions were offered at 10 community centers or YMCAs, which had adequate facilities for offering health promotion programs (e.g., flexible hours of operation, ample space for physical activity, and areas for basic food preparation).
Interventionists were African-American women with experience teaching and working with children. Participants met in groups of 8 to 15 girls. Both intervention groups had the same number and frequency of sessions. To reduce potential contamination, obesity prevention groups met on weekday evenings and the alternative intervention groups met on Saturday afternoons. Meetings occurred weekly for 14 weeks and then monthly for 20 months (34 sessions over two years). Sessions lasted approximately 90 minutes. During the second year, both interventions transitioned to monthly field trips within the community to provide interactive learning experiences in accordance with the respective intervention goals. The obesity prevention intervention provided practical experience with nutrition and physical activity, and the alternative intervention focused on building social awareness and community responsibility. Both interventions contained techniques outlined by Michie et al.,18 namely, providing information, facilitating goal-setting through demonstration and practical experience, and providing feedback and encouragement. The composition of the groups changed over time, with girls moving from one group to another based on scheduling considerations; however, girls never crossed from obesity prevention to the alternative intervention, or vice versa. Make-up sessions were provided to girls who missed regularly scheduled sessions.
Girls and caregivers participated in the obesity prevention intervention through a combination of separate and joint sessions. Girls developed behavioral goals to eat a nutritionally balanced diet, reduce consumption of sugar-sweetened beverages and high-fat high caloric foods, increase intake of water, vegetables and fruits, increase moderate-to-vigorous physical activity and decrease sedentary behavior. Behavioral strategies included skill building, self-monitoring, feedback and positive reinforcement, goal-setting, problem-solving and social support. Caregivers were encouraged to make changes in the home food environment such as increasing the availability of healthy foods.
The alternative intervention targeted the girls only and was designed to provide meaningful benefits with the goal of improving self-esteem and social efficacy. There was no focus on changing behaviors at home or activities related to diet, physical activity or body weight.
There were separate interventionists for the obesity prevention and alternative intervention groups, and they were trained only for their assigned intervention. All interventionists were blind to outcome measurements. The Project Director continuously evaluated treatment fidelity through direct observation and monitoring of both intervention groups. Of the 10% randomly videotaped sessions, the Project Director determined whether the objectives were consistently implemented. The range of sessions judged acceptable was 92%–100% (reflects ratings based on 1=strongly agree or 2=agree).
Randomization
Randomization was stratified by recruitment wave, and within wave, by community center. Eligible participants were randomly assigned to either the obesity prevention or self-esteem intervention. Randomization occurred initially in two mirror-image blocks of 15. Later, independent blocks of five at each center were used to ensure better balance between the two intervention groups.
Measurements
Trained staff performed all measurements at baseline and 1- and 2-years follow-up, and were blind to group assignment. Baseline social and demographic information for the girl and her household was collected from the parent/caregiver.
Anthropometric, Bioelectric Impedance, and Sexual Maturation Measurements
Height, weight, and waist circumference were measured twice while girls were barefoot and wore lightweight clothing. A stadiometer (Shorr Productions, Olney, MD) and electronic scale (Scaletronix 5602, White Plains, NY) were used to measure height and weight. Waist circumference was measured at the level of the umbilicus at end-expiration with a Moore Medical Physician’s Tape Measure. BMI percentiles were calculated from the Centers for Disease Control and Prevention (CDC) growth charts.16 Three measurements of triceps skinfold thickness were taken (Harpenden Model C-136, Plymouth, MI). All measurements were averaged. Bioelectric impedance measures (Tanita TBF-300A, Tanita Corp., Arlington Heights, IL) were obtained using manufacturer protocol to estimate body composition. Sexual maturation was assessed by self-report using drawings and descriptions of pubertal stages.19
Dietary Assessment
Trained interviewers collected 24-hour dietary recalls (Nutrition Data System for Research [NDS-R] Version 4.05_33, University of Minnesota) on three nonconsecutive days, (including one weekend day), and analyzed as three-day averages. The first 24-hour recall occurred face-to-face and the subsequent two recalls were conducted by telephone. Standardized methodology was used, and quality control procedures included a multiple pass approach and probes.20, 21
Physical Activity Monitoring
A validated accelerometer22 (Actigraph Version 2.2, Manufacturing Technologies Inc., Fort Walton Beach, FL) was used to assess physical activity for three consecutive days, typically including one weekend day; measurements were averaged. Number of minutes spent in moderate-to-vigorous physical activity was calculated, defined as ≥3000 counts/min.23
Statistical Analysis
Unless otherwise indicated, all analyses and determination of effect size followed the GEMS protocol14 and were evaluated at a two-tailed alpha level of 0.05. Because of the a priori distinction between the primary outcome analysis and all secondary analyses, no adjustment for multiple comparisons was made. Baseline comparisons between the two intervention groups on the primary and secondary outcomes were performed with t-tests and chi-square tests.
The primary analysis used analysis of covariance (ANCOVA) to assess differences between the two intervention groups in BMI at 2 years with adjustment for baseline BMI. Data were analyzed according to intention-to-treat principles.24 In a preliminary step, multiple imputation was used to generate a predicted value to replace missing values in both intervention groups.25 A prediction equation was developed using data for girls in the alternative intervention group who provided both baseline and 2-year follow-up data. That equation was used to predict 2-year BMI values for girls in either intervention group who did not attend the 2-year follow-up visit, adding random error based on the distribution of the 2-year BMI. This procedure was repeated to create five complete data sets which were analyzed separately; the results were combined using SAS PROC MIANALYZE (SAS/STAT 9.1 User's Guide, 2004, SAS Institute Inc.,Cary, NC).
The same ANCOVA approach was used to evaluate treatment effects on primary and secondary outcomes at 1 year and on secondary outcomes at 2 years. The ANCOVAs for BMI were repeated separately with stratification on median baseline BMI (≤20.8 and >20.8 kg/m2), age tertiles (7.98 to <8.73, 8.73 to 9.77, and >9.77 to11.0 years), and household income (<$40,000 and ≥$40,000) to evaluate treatment effects in these strata. In each case, the stratification factor was tested for interaction between the stratification factor and treatment group. Post hoc, repeated measures ANCOVA was used to evaluate treatment effects on BMI at 1- and 2-years follow-up, with adjustment for baseline BMI; separate models evaluated the main effect for treatment group and the visit-by-treatment group interaction. Also post hoc, the repeated measures ANCOVAs for BMI were done separately with stratification on baseline age; in this model, age was modeled continuously and all 2- and 3-way interactions involving visit, treatment group, and age were included. The subgroups pertaining to baseline BMI, age, and household income were pre-specified, based on the extant literature. To gauge the impact of multiple imputation procedures, analyses were repeated for BMI separately for those girls who completed the study, with no imputation for missing data. Results from these secondary analyses were generally similar to the results for the primary and secondary analyses with imputation.
Results
Recruitment, Baseline Characteristics and Follow-up Rates
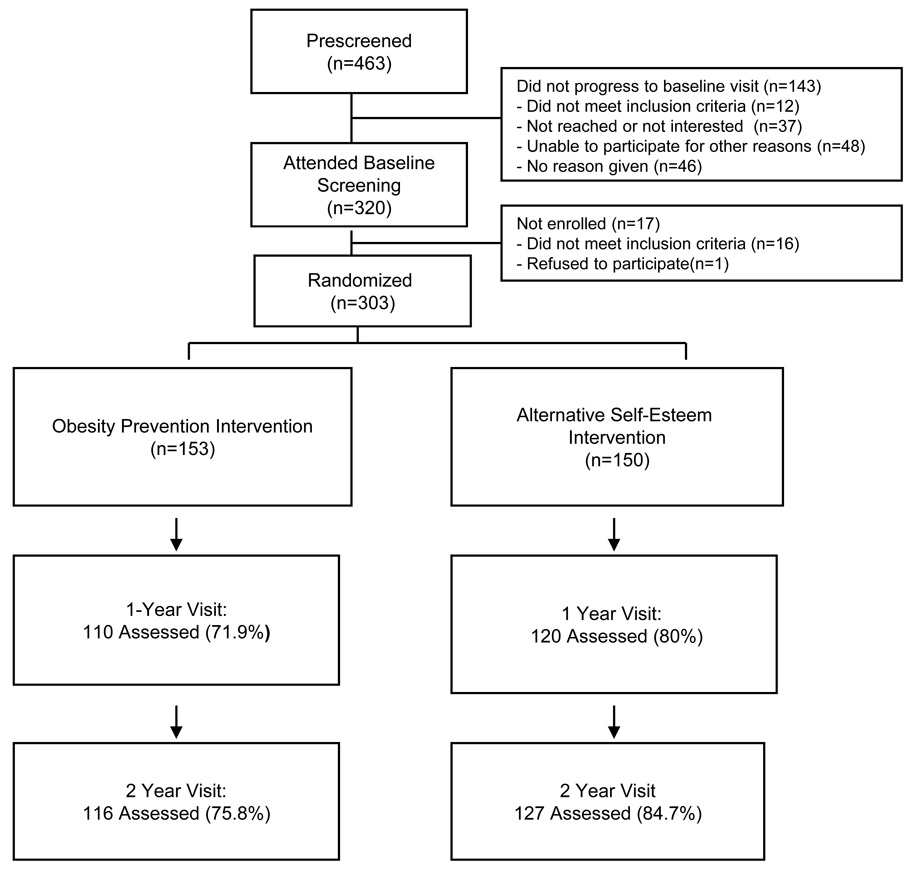
Of 463 respondents, almost three-fourths (n = 338, 73%) were eligible and scheduled for baseline assessment (Figure 1). A total of 303 enrolled in the trial. Mean values and distributions for the major demographic, anthropometric, dietary, and physical activity baseline measures were not significantly different between the two intervention groups (Table 1) .14
Figure 1.
GEMS participant recruitment, randomization, and follow-up
Table 1.
Baseline Characteristics of the GEMS Participants (mean, SD, or n, %)
| Characteristic | Obesity Prevention Intervention |
Alternative Intervention |
All |
|---|---|---|---|
| N | 153 | 150 | 303 |
| Age, y | 9.3 (0.9) | 9.3 (0.9) | 9.3 (0.9) |
| Anthropometry | |||
| Height, cm | 139.8 (8.7) | 140.0 (9.4) | 139.9 (9.1) |
| Weight, kg | 43.1 (15.5) | 44.0 (15.0) | 43.5 (15.2) |
| Body mass index (kg/m2) | 21.7 (6.0) | 22.0 (5.7) | 21.8 (5.8) |
| Body mass index percentile [n, %] | |||
| BMI <85th percentile | 69 (45.1) | 61 (46.7) | 130 (42.9) |
| BMI 85th to <95th percentile | 28 (18.3) | 22 (14.7) | 50 (16.5) |
| BMI ≥ 95th percentile | 56 (36.6) | 67 (44.7) | 123 (40.6) |
| Waist circumference, cm | 71.1 (15.4) | 71.8 (15.3) | 71.5 (15.3) |
| Body fat, percent | 28.0 (11.5) | 28.5 (13.2) | 28.2 (12.3) |
| Fat-free mass, kg | 29.2 (6.5) | 29.8 (6.1) | 29.4 (6.3) |
| Triceps skinfold thickness, mm | 18.2 (8.5) | 18.9 (9.8) | 18.5 (9.1) |
| Dietary Intake per day | |||
| Sweetened beverage servings | 1.08 (0.83) | 1.00 (0.71) | 1.04 (0.77) |
| Water servings | 0.69 (0.60) | 0.71 (1.63) | 0.70 (1.23) |
| Vegetable servings | 0.98 (0.70) | 0.90 (1.40) | 0.94 (1.10) |
| Fruit servings | 0.40 (0.70) | 0.30 (1.46) | 0.35 (0.60) |
| Total fat, percent kcal | 35.9 (5.7) | 35.9 (5.8) | 35.9 (5.7) |
| Total energy, kcal | 1475 (452) | 1379 (452) | 1427 (454) |
| Physical Activity per day | |||
| Activity, total counts | 527 (172) | 526 (159) | 526 (165) |
| Moderate-to-Vigorous, min | 21.1 (17.6) | 20.2 (14.6) | 20.6 (16.1) |
At 1-year follow-up, 76% (230/303) of the baseline sample was available for assessment and 80% (243/303) at the 2-year follow-up (Figure 1). At the end of the study, 84% (253/303) had at least a 1- or 2-year assessment and 71% (216/303) completed both follow-ups. Those who did not complete follow-up visits were similar to those who did in terms of age (P=.43), BMI (P=.49), and pubertal maturation (P=.16 and P=.30 for breast development and pubic hair, respectively). The only significant group difference was baseline vegetable intake among girls who did not complete the year 1 assessment. Average daily vegetable intake among girls in the active intervention was higher than that of girls in the alternative intervention (1.16 [SD=0.86] vs. 0.76 [SD=0.51] servings/d, P=.03).
Intervention Attendance
Session attendance over the two years averaged 27.8 (SD=8.05) for the obesity prevention intervention and 27.9 (SD=8.10) for the alternative intervention, including make-up sessions, which comprised about 50% of all attendance (P=.94).
Body Mass Index
Table 2 presents BMI and anthropometric findings from the a priori ANCOVAs. Mean BMI and other anthropometric measures increased in both intervention groups each year. There were no significant differences between the two intervention groups in mean BMI or any other anthropometric measures at the 1- and 2-year follow-ups.
Table 2.
Adjusted Means (SE) and Treatment Effects (Differences) for Body Mass Index (BMI) and Anthropometric Measurements at 1- and 2-Years Follow-upa
| Measure | Obesity Prevention Intervention |
Alternative Intervention |
Difference (95% C.I.) |
|
|---|---|---|---|---|
| BMI, kg/m2 | 1-Year | 23.6 (0.14) |
23.5 (0.14) |
0.09 (−0.40, 0.58) |
| 2-Years | 24.7 (0.18) |
24.8 (0.19) |
−0.06 (−0.87, 0.75) |
|
| Waist circumference, cm |
1-Year | 76.2 (0.49) |
76.0 (0.49) |
0.20 (−1.24, 1.63) |
| 2-Years | 79.6 (0.60) |
79.7 (0.61) |
−0.10 (−1.97, 1.78) |
|
| Body fat, percent | 1-Year | 30.3 (0.38) |
30.7 (0.39) |
−0.40 (−1.82, 1.01) |
| 2-Years | 32.2 (0.41) |
32.3 (0.42) |
−0.10 (−1.32, 1.16) |
|
| Fat-free mass, kg | 1-Year | 34.1 (0.25) |
33.9 (0.29) |
0.15 (−0.61, 0.91) |
| 2-Years | 37.6 (0.28) |
37.2 (0.29) |
0.32 (−0.79, 1.43) |
|
| Triceps skinfold thickness, mm |
1-Year | 22.4 (0.76) |
22.5 (0.77) |
−0.13 (−2.90, 2.64) |
| 2-Years | 26.0 (0.91) |
27.0 (0.92) |
−0.10 (−4.75, 2.79) |
|
| Weight, kg | 1-Year | 52.1 (0.36) |
52.0 (0.36) |
0.10 (−1.023, 1.22) |
| 2-Years | 58.4 (0.55) |
58.3 (0.56) |
0.02 (−1.74, 1.77) |
|
| Height, cm | 1-Year | 147.2 (0.44) |
147.6 (0.77) |
−0.36 (−2.23, 1.51) |
| 2-Years | 152.4 (0.37) |
152.5 (0.37) |
−0.02 (−1.37,1.33) |
From a priori ANCOVAs.
Dietary Intake and Physical Activity
Table 3 displays dietary and physical activity findings. Relative to baseline, all girls reported increases in mean intake of sweetened beverages, but at the 2-year visit, the obesity prevention group had 0.19 fewer servings/day than the alternative intervention group (P=.075). The obesity prevention group reported increased water consumption from baseline, and at 2-years had 0.21 more servings/day than the alternative intervention group (P=.022). Vegetable intake decreased from baseline in both intervention groups, but at 2 years, the obesity prevention group reported 0.15 servings/day higher vegetable intake than the alternative intervention group (P=.069). At 2 years, energy intake was reported to be 78 kcal/day less for the obesity prevention intervention group compared to the alternative intervention group, although this difference was not statistically significant (P=.16).
Table 3.
Adjusted Means (SE) and Treatment Effects (Differences) for Dietary and Physical Activity Measures at 1- and 2-Years Follow-upa
| Per Day | Obesity Prevention Intervention |
Alternative Intervention |
Difference (95% C.I.) |
|
|---|---|---|---|---|
| Sweetened beverages, servings |
1-Year | 1.11 (0.07) |
1.24 (0.07) |
−0.13 (−0.36, 0.09) |
| 2-Years | 1.27 (0.07) |
1.45 (0.07) |
−0.19 (−0.39, 0.09) |
|
| Water, servings | 1-Year | 0.79 (0.06) |
0.61 (0.06) |
0.18 (−0.21, 0.38) |
| 2-Years | 0.81 (0.06) |
0.59 (0.06) |
0.21 (0.03, .40) |
|
| Vegetable, servings | 1-Year | 0.87 (0.05) |
0.86 (0.05) |
0.02 (−0.14, 0.19) |
| 2-Years | 0.87 (0.05) |
0.72 (0.05) |
0.15 (−0.02, 0.30) |
|
| Fruit, servings | 1-Year | 0.32 (0.03) |
0.30 (0.03) |
0.02 (−0.07, 0.11) |
| 2-Years | 0.29 (0.04) |
0.29 (0.05) |
−0.01 (−0.17, 0.16) |
|
| Total fat, percent energy |
1-Year | 35.9 (0.50) |
35.4 (0.52) |
0.5 (−1.26, 2.28) |
| 2-Years | 35.7 (0.47) |
35.5 (0.47) |
0.1 (−1.71, 1.94) |
|
| Total energy, kcal | 1-Year | 1373 (35.5) |
1426 (35.6) |
−54 (−188.3, 80.6) |
| 2-Years | 1347 (32.8) |
1425 (32.9) |
−78 (−186.3, 31.1) |
|
| Physical activity counts |
1-Year | 496 (8.7) |
482 (8.8) |
14 (−10, 38) |
| 2-Years | 447 (7.7) |
440 (7.8) |
7.5 (−14, 21) |
|
| Moderate-to- vigorous activity, min |
1-Year | 21.1 (0.8) |
20.1 (0.8) |
1.0 (−1.2, 3.2) |
| 2-Years | 16.8 (0.6) |
16.2 (0.7) |
0.6 (−1.3,2.4) |
From a priori ANCOVAs.
Girls in both groups decreased their physical activity over time. Physical activity did not differ significantly between the two groups at either the 1- or 2-year follow-up visit.
Post-hoc BMI analyses
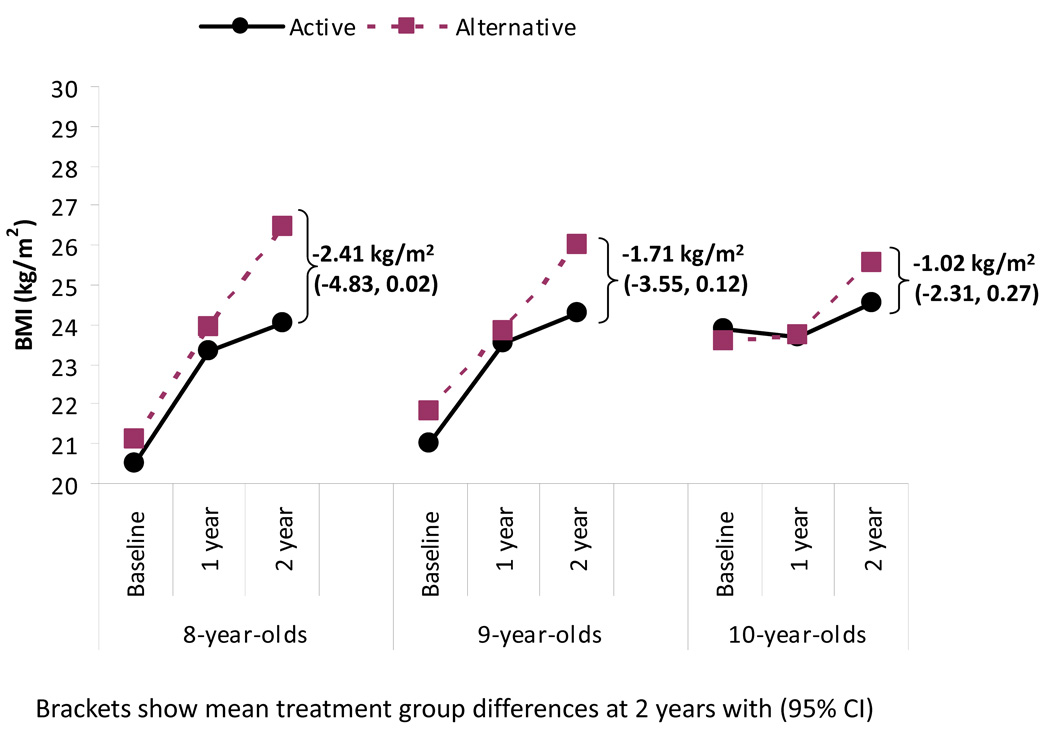
Pre-specified secondary analyses did not identify significant interactions for subgroups defined by baseline BMI, age and household income. However, in the post hoc repeated measures ANCOVA that included treatment group, age, visit, and all interactions, with adjustment for baseline BMI, the average F-test across five imputed data sets for the age-by-treatment-by-visit interaction term had a P value of .081. The pattern of the predicted means was suggestive of an intervention effect among younger girls at the 2-year follow-up visit (Figure 2).
Figure 2.
Predicted mean body mass index (BMI) from post-hoc repeated measures analysis of 3-way interaction for age, visit, and treatment group
Discussion
The primary BMI analysis indicates that the obesity prevention intervention did not significantly reduce weight gain relative to the alternative intervention. In secondary analyses there were also no significant effects on other anthropometric measures. Statistically significant or marginally-significant treatment effects were observed on reported intakes of sweetened beverages, water and vegetables, but there were no effects on measured physical activity. Post hoc secondary analyses also suggested an age difference in effects on BMI such that treatment-related differences in BMI in the youngest girls were more than twice as large as those in the oldest girls: −2.41 vs. −1.02 kg/m2. While not a significant difference, as we were not powered to detect a 3-way interaction, the magnitude of this difference suggests clinical relevance.
Findings of no effect are common in obesity prevention trials and a recent commentary estimated that 42% to 50% of trials were effective, depending on the study inclusion criteria and definitions of effectiveness used in systematic reviews.26 The lack of a significant effect on BMI is particularly disappointing when considering the need for interventions in this high-risk population and in light of the theoretical and empirical support for the cultural appropriateness and potential efficacy of the Memphis GEMS obesity prevention program.10, 17 It may be particularly difficult to identify effective obesity prevention strategies in high-risk populations such as African-American girls because the difficulty of avoiding weight gain may be greater in the social and environmental contexts in which they live. GEMS targeted behaviors that are also strongly influenced by school, neighborhood, and media context related to eating and physical activity,17, 27, 28 and these influences are more adverse for African-Americans.
The types of food stores and restaurants available in predominantly African-American neighborhoods are relatively less conducive to the purchase and consumption of healthful foods (e.g., fewer supermarkets, more fast food restaurants) compared to predominantly white neighborhoods.29 Promotion of high-calorie foods and beverages to African-Americans through television, outdoor advertising, and other media is high relative to the intensity of such promotions to whites or the general population29–32 and may have greater salience due to ways in which ethnically distinctive populations respond to targeted advertising.33 A similarly adverse picture applies to physical activity options, i.e., lower access to safe and attractive options for outdoor physical activity in neighborhoods where African-American children live.34, 35 Some of these environmental challenges are especially applicable to children in lower income communities, in which the majority of Memphis GEMS participants reside. Multi-level interventions in which both contextual and individual behaviors are targeted may be needed,29 although the evidence for the effectiveness of such interventions is currently also lacking.
Our findings suggest ways to strengthen the potential effectiveness of the GEMS intervention in directly facilitating behavior changes. Obesity prevention programs tend to differ from obesity treatment programs in that they promote healthful eating and activity patterns without specific goal levels for caloric intake and expenditure. Consistent with a prevention approach, the GEMS obesity prevention intervention emphasized behaviors such as reducing sweetened beverage intake and increasing water intake. The intervention had an impact on these behaviors but not on total caloric intake, which was not directly emphasized. A more explicit emphasis on the need for caloric moderation may be warranted, even in elementary-age children, in order to influence mean BMI, with appropriate precautions to avoid triggering inappropriate caloric restriction. Even more striking is the potential to improve intervention effectiveness with respect to physical activity and inactivity. Girls in both intervention groups became less physically active as they grew older, such that their highest level of physical activity was at baseline. This observation reflects the well-known pattern of decreasing physical activity in adolescent girls, particularly among African-American girls.36 The potential for physical activity to moderate weight gain over time is substantial. Findings from the National Heart, Lung, and Blood Institute Growth and Health Study (NGHS) showed that African-American girls who were consistently physically active throughout adolescence (ages 9 through 19) had 3 kg/m2 lower mean BMI than girls who were consistently inactive.37 However, attempts to increase physical activity, or even reduce the decline in physical activity that occurs during adolescence, continue to pose a challenge.38, 39
Our findings may have implications for the developmental timing of preventive interventions. Stice et al.40 noted that intervention effectiveness to reduce mean BMI was lowest among 9- to 11-year-old participants, an age range in which fat accumulation in girls occurs and continues relatively linearly through age 14.41, 42 Instituting measures to prevent excess weight gain concurrent with pubertal growth will be difficult if hormonal processes overshadow potential intervention effects. Intervening on girls well before puberty to better moderate the trajectory of adiposity gain may be preferable and is consistent with our finding of a larger effect in girls who were youngest at enrollment, i.e., age 8 years. There may also be behavioral explanations for differential treatment effects in younger girls such as family environmental influences that can be explored through analysis of mediators of effects reported here.
The many strengths of Memphis GEMS include the randomized controlled trial design, the high degree of quality control built into intervention delivery and data collection, the large sample size, the relatively long (2-year) period of intervention and follow-up, the high-risk ethnic group and primarily low-income study population that is typically under-served, and the 80% follow-up rates at the 2-year visit. Sensitivity analyses indicated that imputation for missing data did not alter conclusions. Also, the intervention materials can be readily disseminated to and adapted by community organizations.17 Limitations of the study include the narrow age range and the single race and gender; although appropriate to the development of a culturally targeted approach, this reduces generalizability of the results. Another potential limitation, discussed elsewhere,17 was the somewhat high percentage of participants who required make-up sessions, which may have reduced the impact of the intervention as originally designed. Also, as is common with many obesity interventions,27, 28, 40, 43 our significant effects were observed primarily on subjective (e.g., diet) and not objective (e.g., BMI) measures, suggesting the possibility of response bias. Finally, while the alternative intervention stressed self-esteem and never mentioned diet, exercise or BMI, its intensity may have generated attention effects that may have affected our results.
In summary, the Memphis GEMS obesity prevention intervention that promoted healthy eating behaviors and increased physical activity targeted to low-income African-American girls and their caregivers did not reduce mean BMI relative to an alternative intervention after 2 years. A relatively large effect was suggested in the youngest girls, indicating that preventive interventions may need to start well before puberty. The obesity prevention intervention was associated with relative improvements in several dietary behaviors—sweetened beverage consumption, water and vegetable intake—but had no impact on physical activity levels, which showed a marked decline among girls in both groups. This aspect of the program requires strengthening. More fundamentally, success with individually-oriented preventive interventions, especially those targeted to African-Americans or low-income populations, may require concurrent environmental and policy changes to improve contexts for eating and physical activity behavior change.
Acknowledgements
We would like to thank the Memphis GEMS participants and their families, the Memphis GEMS field staff, and the City of Memphis Division of Park Services and the Memphis YMCAs for the use of their community centers. We also are grateful for the helpful collaboration of the Stanford GEMS investigators and the National Heart, Lung, and Blood Institute Project Office, and for the valuable comments of the GEMS Data and Safety Monitoring Board.
Footnotes
Research was supported by cooperative agreements HL62662 and HL62663 from the National Heart, Lung, and Blood Institute, National Institutes of Health.
Trial Registration: Trial registry: Clinicaltrials.gov; Registration No.: NCT00000615 (http://clinicaltrials.gov/ct/show/NCT00000615?order=1).
References
- 1.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 2.Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007 Dec 6;357(23):2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005 Apr 19;111(15):1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006 Apr 5;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995 Oct;149(10):1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006 Feb;14(2):301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008 May 28;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 8.Obarzanek E, Pratt CA. Girls health Enrichment Multi-site Studies (GEMS): new approaches to obesity prevention among young African-American girls. Ethn Dis. 2003 Winter;13(1 Suppl 1):S1–S5. [PubMed] [Google Scholar]
- 9.Baranowski T, Baranowski JC, Cullen KW, et al. The Fun, Food, and Fitness Project (FFFP): the Baylor GEMS pilot study. Ethn Dis. 2003 Winter;13(1 Suppl 1):S30–S39. [PubMed] [Google Scholar]
- 10.Beech BM, Klesges RC, Kumanyika SK, et al. Child- and parent-targeted interventions: the Memphis GEMS pilot study. Ethn Dis. 2003 Winter;13(1 Suppl 1):S40–S53. [PubMed] [Google Scholar]
- 11.Robinson TN, Killen JD, Kraemer HC, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003 Winter;13(1 Suppl 1):S65–S77. [PubMed] [Google Scholar]
- 12.Rochon J, Klesges RC, Story M, et al. Common design elements of the Girls health Enrichment Multi-site Studies (GEMS) Ethn Dis. 2003 Winter;13(1 Suppl 1):S6–S14. [PubMed] [Google Scholar]
- 13.Story M, Sherwood NE, Himes JH, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis. 2003 Winter;13(1 Suppl 1):S54–S64. [PubMed] [Google Scholar]
- 14.Klesges RC, Obarzanek E, Klesges LM, et al. Memphis Girls health Enrichment Multi-site Studies (GEMS): Phase 2: design and baseline. Contemp Clin Trials. 2008 Jan;29(1):42–55. doi: 10.1016/j.cct.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Robinson TN, Kraemer HC, Matheson DM, et al. Stanford GEMS phase 2 obesity prevention trial for low-income African-American girls: design and sample baseline characteristics. Contemp Clin Trials. 2008 Jan;29(1):56–69. doi: 10.1016/j.cct.2007.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000 Jun 8;(314):1–27. [PubMed] [Google Scholar]
- 17.Kumanyika S, Beech B, McClanahan B, et al. Development Of The Family-Based Obesity Prevention Program For Pre-Adolescent African-American Girls In The Memphis Girls health Enrichment Multisite Studies (GEMS). Paper presented at: 7th annual meeting of the International Society for Behavioral Nutrition and Physical Activity; Banff, Alberta, Canada. May 21–24.2008. [Google Scholar]
- 18.Michie S, Jochelson K, Markham WA, Bridle C. Low-income groups and behaviour change interventions: a review of intervention content, effectiveness and theoretical frameworks. J Epidemiol Community Health. 2009;63:610–622. doi: 10.1136/jech.2008.078725. [DOI] [PubMed] [Google Scholar]
- 19.Morris MN, Udry JR. Validation of a self-administered instrument to assess stage of adolescent development. J Youth Adolesc. 1980;9:271–280. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- 20.Cullen KW, Himes JH, Baranowski T, et al. Validity and reliability of a behavior-based food coding system for measuring fruit, 100% fruit juice, vegetable, and sweetened beverage consumption: results from the Girls Health Enrichment Multisite Studies. Prev Med. 2004 May;38 Suppl:S24–S33. doi: 10.1016/j.ypmed.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Cullen KW, Watson K, Himes JH, et al. Evaluation of quality control procedures for 24-h dietary recalls: results from the Girls Health Enrichment Multisite Studies. Prev Med. 2004 May;38 Suppl:S14–S23. doi: 10.1016/j.ypmed.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 22.Janz KF. Validation of the CSA accelerometer for assessing children's physical activity. Med Sci Sports Exerc. 1994 Mar;26(3):369–375. [PubMed] [Google Scholar]
- 23.Treuth MS, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004 Jul;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 24.Lachin JL. Statistical considerations in the intent-to-treat principle. Control Clin Trials. 2000 Oct;21(5):526. doi: 10.1016/s0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- 25.Little RJ, Rubin D. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- 26.Doak C, Heitmann BL, Summerbell C, Lissner L. Prevention of childhood obesity - what type of evidence should we consider relevant? Obes Rev. 2009 May;10(3):350–356. doi: 10.1111/j.1467-789X.2008.00550.x. [DOI] [PubMed] [Google Scholar]
- 27.Koplan JP, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance. Washington, D.C: National Academies Press; 2005. [PubMed] [Google Scholar]
- 28.Maziak W, Ward KD, Stockton MB. Childhood obesity: are we missing the big picture? Obes Rev. 2008 Jan;9(1):35–42. doi: 10.1111/j.1467-789X.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 29.Grier SA, Kumanyika SK. The context for choice: health implications of targeted food and beverage marketing to African Americans. Am J Public Health. 2008 Sep;98(9):1616–1629. doi: 10.2105/AJPH.2007.115626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grier SA. African American & Hispanic Youth Vulnerability to Tarket Marketing: Implications for Understanding the Effects of Digital Marketing. The Second NPLAN/BMSG Meeting on Digital Media and Marketing to Children. 2009 June 29–30; [Google Scholar]
- 31.Hillier A, Cole BL, Smith TE, et al. Clustering of unhealthy outdoor advertisements around child-serving institutions: a comparison of three cities. Health Place. 2009 Dec;15(4):935–945. doi: 10.1016/j.healthplace.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Yancey AK, Cole BL, Brown R, et al. A cross-sectional prevalence study of ethnically targeted and general audience outdoor obesity-related advertising. Milbank Q. 2009 Mar;87(1):155–184. doi: 10.1111/j.1468-0009.2009.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grier S, Kumanyika S. Targeted marketing and public health. Annu Rev Public Health. 2010;31:349–369. doi: 10.1146/annurev.publhealth.012809.103607. [DOI] [PubMed] [Google Scholar]
- 34.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006 Feb;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 35.Taylor WC, Poston WSC, Jones L, Kraft MK. Environmental justice: obesity, physical activity, and healthy eating. J Phys Act Health. 2006 February;3 supp 1 doi: 10.1123/jpah.3.s1.s30. [DOI] [PubMed] [Google Scholar]
- 36.Kimm SY, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002 Sep 5;347(10):709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 37.Kimm SY, Glynn NW, Obarzanek E, et al. Relation between the changes in physical activity and body-mass index during adolescence: a multicentre longitudinal study. Lancet. 2005 Jul 23–29;366(9482):301–307. doi: 10.1016/S0140-6736(05)66837-7. [DOI] [PubMed] [Google Scholar]
- 38.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009 Mar 31;180(7):719–726. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Webber LS, Catellier DJ, Lytle LA, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008 Mar;34(3):173–184. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006 Sep;132(5):667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kimm SY, Barton BA, Obarzanek E, et al. Racial divergence in adiposity during adolescence: The NHLBI Growth and Health Study. Pediatrics. 2001 Mar;107(3):E34. doi: 10.1542/peds.107.3.e34. [DOI] [PubMed] [Google Scholar]
- 42.Malina RM, Bouchard C, Bar-Or O. Growth, Maturation, and Physical Activity. 2nd ed. Champaign, IL: Human Kinetics Books; 2004. Adipose tissue changes during growth. [Google Scholar]
- 43.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008 Jul 22;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]