Abstract
Background
We determined the genetic diversity of mycobacteria isolated from tuberculosis patients in Mbarara Uganda, using region of difference (RD) analysis and spacer oligonucleotide typing (spoligotyping).
Methods
Sputum samples were cultured on Lowenstein Jensen media. The isolates were characterized using RD analysis and spoligotyping.
Results
The majority (92.8%) of the patients were new cases, 60% were males and 44% were HIV positive with a mean age of 33.7 years. All the 125 isolates were identified as M.tuberculosis sensu stricto. Most (92.8%) of the isolates were modern strains. Spoligotyping revealed 79 spoligotype patterns, with an overall diversity of 63.2%. Sixty (48%) isolates formed 16 clusters each consisting of 2–15 isolates. Mst (59.2 %) of the isolates were Uganda genotype strains. The major shared spoligotypes in our sample were SIT 135 (T2-Uganda) with 12 isolates and SIT 128 (T2) with 5 isolates. Sixty nine (87%) patterns had not yet been defined in the SpolDB4.0.database.
Conclusion
The TB epidemic in Mbarara is caused mainly by modern M.tuberculosis strains of the Uganda genotype. The wide diversity of strains may indicate that the majority of the TB cases are reactivation rather than re-infection. However this needs to be ascertained with more discriminative finger printing techniques.
Keywords: Mycobacteria, spoligotypes, Region of difference
Introduction
In spite of the wide availability of cost effective interventions for its control, tuberculosis (TB) is still a major global health problem and the leading cause of death from a curable infectious disease1. Uganda ranks 16th among the world's 22 countries with the highest tuberculosis burden in the world2. The country had more than 40,000 TB cases in 2007,with an estimated incidence rate of 330 per 100,000 people and a directly observed therapy short course (DOTS) treatment success rate of 70 percent in 2007)2 with greater Mbarara contributing about 26% of all TB cases.
An increasing amount of evidence indicates that M. tuberculosis' ability to spread varies from strain to strain and that different strains have different geographical and/or host specificities3,4. Since the discovery of DNA polymorphisms in M. tuberculosis, molecular typing of strains has become an invaluable tool for the study of epidemiology of TB. Some of the applications include; predicting transmission rates andidentifying dominant strains associated with outbreak8, severe disease9 and drug resistance5
Genotyping of M. tuberculosis using IS6110 restriction fragment length polymorphism has for a long time been the gold standard. However this technique is labor-intensive and requires culturing of the slow-growing mycobacteria and the results are sometimes difficult to compare among laboratories. More recently, spoligotyping based on the variability in the direct repeat locus of M. tuberculosis, is useful for tracking TB epidemics, detecting new outbreaks, and better defining high-risk populations to focus prevention strategies7,8. Important advantages of spoligotyping are that it is cheap, easy to perform and fast. In addition, it has been demonstrated that the results are highly reproducible. Important advantages of spoligotyping are that it is cheap, easy to perform and fast. In addition, it has been demonstrated that the results are highly reproducible9. Comparative-genomics approaches greatly enhanced our understanding of the mechanisms of insertion and deletion of DNA and the resulting distribution of variable regions around the genomes of tubercle bacilli10–12. There are 20 variable regions, of which 14 regions of difference (RD1 to RD14) were found to be absent from Bacillus Calmette-Guérin (BCG) Pasteur relative to M. tuberculosis H37Rv12–14. Six regions, H37Rv-related deletions (RvD1 to RvD5 and M. tuberculosis specific deletion 1 (TbD1), are absent from the M. tuberculosis H37Rv genome relative to other members of the M. tuberculosis complex. Based on the presence or absence of the TbD1 region, M. tuberculosis strains can be divided into “ancestral” and “modern” types. The Beijing, Haarlem, and African strains responsible for major epidemics are modern types9,10
The Beijing and Beijing-like strains are most prevalent in the Far East-Asia. In Europe, the Harlem lineage represents about 25% of the isolates. In South America, about 50% of the strains belong to the LAM family. Three major genotypic families (Haarlem, LAM, and T) are the most frequent in Africa, Central America, Europe and South America. Outside Europe, The Haarlem strains were mainly found in Central America and Caribbean. The “ill-defined genetic family, was found in all continents. The East-African-Indian (EAI) family is also highly prevalent in the Far-East-Asia, in the Middle East and Central Asia. The East-African-Indian (EAI) family is more prevalent in South-East Asia, particularly in the Philippines16, in Myanmar and Malaysia17, in Vietnam and Thailand18 The CAS1-Delhi family is essentially localized in the Middle-East and Central Asia, more specifically in South-Asia, and preferentially in India19,20 Iran, and Pakistan21,22. Lastly, the X family is highly prevalent in North America and Central American regions23. The aim of this study was to evaluate the genotypic diversity of the Mycobacterium tuberculosis complex (MTC) strains using Region of Difference analysis and spoligotyping in this high HIV prevalence community.
Methods
Study setting
The study was conducted between May 2007 and April 2008 in the four districts of greater Mbarara namely Ibanda, Isingiro, Kiruhura and Mbarara. This region has been heavily affected by the TB/HIV epidemic. In 2005, the case notification for Mbarara was 175/100,000 people compared to the 147/100,000 people for Uganda24. In 2008 the TB/HIV co-infection rate for Mbarara was 65%25.
Study design
This was a cross sectional study which was conducted between May 2007 and April 2008 and enrolled consecutively all smear-positive newly diagnosed and retreatment TB patients aged e” 18 years. Three consecutive sputum samples (spot, early morning and spot) were taken from each patient according the Uganda National TB and Leprosy guidelines. Only the sample with the highest ZN smear grade was further analyzed for each patient. Samples were stored at 4°C at the recruitment clinics, in any case for not more than 48 hours, until transported in a cold box to the NTRL in Kampala for processing and culture.
Sputum sample processing
Specimens (2.5–10 ml) were processed by the standard N-acetyl L-cystein (NALC)-NaOH method26 and concentrated at 4000 × g for 15 minutes. The sediment was reconstituted to 2.5 ml withphosphate buffer pH 6.8, to make the inoculum for the smears and cultures.
Culture and identification
Two Lowenstein-Jensen slants, one containing 0.75% glycerol and the other containing 0.6% pyruvate, were inoculated with the sediment and incubated at 37°C and examined weekly for growth. Cultures were considered negative when no colonies were seen after 8 weeks incubation.
DNA Extraction
Isolates were harvested and DNA extracted using a standardized protocol27
RD analysis
RD analysis for speciation of the isolates was done at the department of Medical Microbiology, Makerere University College of Health Sciences as previously described28.
Spoligotyping
Standard spoligotyping was performed as previously described29 using a commercially available kit (Isogen Bioscience BV, Maarssen, The Netherlands).
Data analysis
Socio-demographic data was entered into the computer using Microsoft Excel 2000 software and was then exported to SPSS version 10 for analysis. All genotyping data were digitized and analyzed with the BioNumerics software, version 5.0 (Applied Maths, Kortrijk, Belgium). Genotype identification was carried out according to SpolDB430 and by the freely assessable MIRU-VNTRplus web database31. The latter comprises genotyping data of a reference strain collection of validly described mycobacterium tuberculosis complex (MTBC) genotypes. Labels for major phylogenetic clades were assigned according to signatures provided in SpolDB4. Univariate analysis of categorical variables utilized percentages while means and standard deviations were calculated for continuous variables. The median and range was presented whenever continuous data was skewed.
Ethical considerations
This study received ethical clearance from the faculty research and ethics committee of the faculty of medicine of Mbarara University of Science and Technology, the institutional review board of Mbarara University of Science and Technology and the National Council for Science and Technology. Patients were identified and managed according to Uganda NTLP guidelines32. Informed consent to participate in the study as well as permission to use isolates from samples provided were obtained from all enrolled participants.
Results
We enrolled a total of 167 sputum positive tuberculosis patients who were presenting for TB diagnosis at the various TB clinics in the greater Mbarara during the study. Most (92.8%) of the patients were newly diagnosed and nine (7.2%) had a history of previous treatment. Their mean age was 33.7 years and seventy five (60%) of them were males. Fifty five of the 125 patients were HIV seropositive, twenty six were HIV sero-negative and forty four had unknown sero-status because they did not consent to testing.
Of the 167 samples that were cultured 140 (84%) grew, 14 (8%) had no growth and 13 (8%) were contaminated. Of the 140 cultures 15 (10.7%) were no available for DNA extraction.
All the 125 isolates available for RD analysis were identified as M.tuberculosis sensu stricto. Seven isolates were found to have all the RD loci conserved including TbD1 and were therefore ancestral strains (Table 1).
Table 1.
Species identification and PCR results of the M. tuberculosis complex isolates
| Targeted PCR locus | |||||
| M.tuberculosis complex | 16S | RD4 | RD9 | RD12 | TbD1 |
| Ancestral M. tuberculosis* (n=07) |
+ | + | + | + | + |
| Modern M. tuberculosis2‡ (n=118) |
+ | + | + | + | − |
Defined as possessing the TbD1 locus intact
Defined as possessing the TbD1 deletion
+ = Locus intact
− = Locus deleted
The isolates gave 79 different spoligopatterns, with an overall diversity of 63.2%. A total of 62 (49.6%) isolates, were grouped into 16 clusters consisting of 2–15 isolates each, while the remaining 63 (51.4%) of the strains did not cluster.
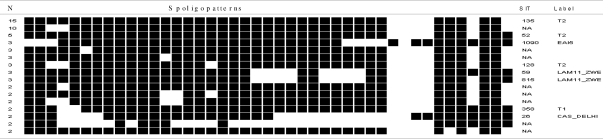
The family assignment showed that 59.2% of the isolates belonged to the Uganda family, 7.2 % to the CAS_DELHI Family, 6.4% to the Latin American Mediterranean (LAM) family, and 5.6 % to the East-African Indian (EAI) family, 4% belonged to the Cameroon family, 2.4% to the Ghana family and 13.6% were not assigned to any family. Among the 16 clusters, three clusters included five or more isolates each and were defined as major spoligotypes, while minor spoligotypes, on the other hand, were defined as spoligotype international types (SITs) that contained less than five isolates per cluster (Figure 1).
Figure 1.
Spoligotype pattern of clustered M. tuberculosis strains in the study.
a As identified in SpolDB4.0; SIT, spoligotype international type; Nb, number of isolates (as a percentage of total M. tuberculosis strains in the study); cfilled boxes represent positive hybridization while empty boxes represent absence of spacers; d label defining the lineage/sub lineage; ND, not yet determined in SpolDB4.0.
Comparison of the spoligotypes in our study with SpolDB4.0 allowed differentiation between ubiquitous types (SIT 26-CAS_DELHI, SIT 52-T2, SIT 53-T1, SIT 54-MANU2, SIT 59-LAM11_ZWE, SIT356- CAS, SIT 358-T1, SIT 420-T2, SIT 815- LAM11_ZWE, SIT 1090 - EAI5 and S PubMedIT 1572-T2) and those believed to be endemic in Uganda (SIT 128- T2 and SIT 135 - T2).
Spoligotypes that did not match any existing pattern in the SpolDB4 database were defined as orphans. Of the 79 patterns observed in this study, 69 were true orphans having no counterpart in the database.
Majority (59.2%) of the isolates lacked hybridization to either spacer 40 alone or to both 40 and 43. These Uganda genotype strains formed 8 clusters (ranging 2 to 15 isolates). Nine strains were Uganda genotype I while seventy seven were Uganda genotype II (Data not shown). Forty eight Uganda genotype strains did not cluster.
Discussion
To have a better knowledge of moving and expanding clones of M. tuberculosis within the Mbarara, we have used RD analysis and spoligotyping to characterize mycobacteria isolated from newly diagnosed and previously treated sputum smear positive TB patients in Mbarara, South Western Uganda, a country in which both HIV infection and TB are endemic.
Deletion analysis using 16s, RD4, RD 9, RD12 and TbD1 revealed that all the strains investigated were M. tuberculosis. Seven of 125 M. tuberculosis strains tested had the TbD1 region intact, indicating these were ancestral strains. Most of the ancestral strains had the following spoligotype signatures: absence of spacers 29 to 32, presence of spacer 33, and absence of spacer34.
The diversity of the M. tuberculosis found in the present study (63.2%) is high compared to 17.8% described from a study in central Uganda33, which may indicate geographical differences in the epidemiology of TB (reactivation versus reinfections) in Uganda. This is not easily determined using spoligotyping alone and would therefore require more discriminative techniques to confirm this. Similar studies in Tanzania have shown genetic diversity that ranges from 36%–52 %34,35. The effect of this diversity on transmission is not clear and need to be studied further.
In this study 69 (87%) of the spoligopatterns could not be typed on the basis of the existing SpolBD4 database. These strains warrant further characterization to better understand them and to add our knowledge to the molecular epidemiology of TB in this area of Uganda. Majority (59.2%) of the strains in our sample were of the Uganda genotype, a finding which is in keeping those of earlier studies in Uganda36–39 as opposed to the surrounding East African countries40.
For example a study in Kenya40 found only eight (11%) of 73 isolates to be of the Uganda family while in northern Tanzania34 only four (3%) of 130 strains were T2-Uganda. Collectively these findings are in keeping with those of other studies showing a tendency for local genotypes to form a greater proportion of the circulating strains. For example in Guinea Bissau, 51% of the isolates belonged to the Guinea Bissau family41; Cameroon where 46.7% of the isolates belonged to the Cameroon family, LAM10-CAM42; Harare, Zimbabwe where 31.8%–47.2% of the isolates were LAM-ZWE variants43,44 and in Zambia where 65% of the isolates were also of the LAM-ZWE family44. It is thus tempting to speculate that local strains are more likely to transmit in a given local setting compared to others4,39.
Conclusions
We have shown that the majority of the Mycobacteria in Mbarara are modern M. tuberculosis with a wide diversity of spoligotypes and a predominance of the Uganda family. Fingerprinting of these isolates with more discriminative techniques will give a better insight of the molecular epidemiology of TB in Mbarara.
Acknowledgements
This study received funding from DAAD and WHO/Tropical disease research. We thank Mr. Charles Ndaula of the TB laboratory at Mbarara University and the staff at National reference tuberculosis laboratory at Wandegeya and the molecular biology laboratory staff at Makerere University Medical School for technical assistance.
References
- 1.Dye C. Global epidemiology of tuberculosis. Lancet. 2006;367:938–940. doi: 10.1016/S0140-6736(06)68384-0. [DOI] [PubMed] [Google Scholar]
- 2.Global tuberculosis control - epidemiology, strategy, financing. World Health Organisation Report. WHO/HTM/TB/2009.411. [Google Scholar]
- 3.Filliol I, Motiwala A S, Cavatore M, Qi W, Hazbon M H, Bobadilla del Valle M, Fyfe J, et al. “Global phylogeny of Mycobacterium tuberculosis based on single nucleotide polymorphism (SNP) analysis: insights into tuberculosis evolution, phylogenetic accuracy of other DNA fingerprinting systems, and recommendations for a minimal standard SNP set”. J Bacteriol. 2006;188(2):759–772. doi: 10.1128/JB.188.2.759-772.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gagneux S, DeRiemer K Van, Kato-Maeda T, de Jong MBC, Narayanan S, Nicol M, Niemann S, et al. Variable host-pathogen compatibility in Mycobacterium tuberculosis. Proc Natl Acad Sci U S A. 2006;103(8):2869–2873. doi: 10.1073/pnas.0511240103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Umubyeyi AN, Gasana M, Basinga P, Zawadi JP, Gatabazi J, Pauwels P, Nzabintwali F, Nyiramasarabwe L, Fissette K, Rigouts L, Struelens MJ, Portaels F. Results of a national survey on drug resistance among pulmonary tuberculosis patients in Rwanda. Int J Tuberc Lung Dis. 2007;11(2):189–194. [PubMed] [Google Scholar]
- 6.van Embden J D, van Gorkom T, Kremer K, Jansen R, van Der Zeijst B A, Schouls L M. Genetic variation and evolutionary origin of the direct repeat locus of Mycobacterium tuberculosis complex bacteria. J Bacteriol. 2000;182(9):2393–2401. doi: 10.1128/jb.182.9.2393-2401.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sola C, Filliol I, Guttierez C, Mokrousov I, Vincent V, Rastogi N. Spoligotype database of Mycobacterium tuberculosis: biogeographical distribution of shared types and epidemiological and phylogenetic perspectives. Emerg Infect Dis. 2001;7:390–396. doi: 10.3201/eid0703.010304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quitugua T, Seaworth BJ, Weis SE, Taylor JP, Gillette JS, Rosas II, et al. Transmission of drug-resistant tuberculosis in Texas and Mexico. J Clin Microbiol. 2002;40:2716–2724. doi: 10.1128/JCM.40.8.2716-2724.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kremer K, van Soolingen D, Frothingham R, Haas WH, Hermans PW, Martin C, Palittapongarnpim P, Plikaytis BB, et al. Comparison of methods based on different molecular epidemiological markers for typing of Mycobacterium tuberculosis complex strains: interlaboratory study of discriminatory power and reproducibility. J Clin Microbio. 1999;37(8):2607–2618. doi: 10.1128/jcm.37.8.2607-2618.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brosch R, Gordon SV, Marmiesse M, Brodin P, Buchrieser C, Eiglmeier K, Garnier T, Gutierrez C, Hewinson, Kremer K, Parsons LM, Pym AS, Samper S, van Soolingen D, Cole ST. A new evolutionary scenario for the Mycobacterium tuberculosis complex. Proc Natl Acad Sci U S A. 2002;99(6):3684–3689. doi: 10.1073/pnas.052548299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brosch R, Pym AS, Gordon SV, Cole ST. The evolution of mycobacterial pathogenicity: clues from comparative genomics. Trends Microbiol. 2001;9(9):452–458. doi: 10.1016/s0966-842x(01)02131-x. [DOI] [PubMed] [Google Scholar]
- 12.Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, Gordon S V, Eiglmeier K, Gas S, et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature. 1998;393(6685):537–544. doi: 10.1038/31159. [DOI] [PubMed] [Google Scholar]
- 13.Behr MA, Wilson M A, Gill WP, Salamon H, Schoolnik G K, Rane, Small PM. Comparative genomics of BCG vaccines by whole-genome DNA microarray. Science. 1999;284(5419):1520–1523. doi: 10.1126/science.284.5419.1520. [DOI] [PubMed] [Google Scholar]
- 14.Gordon SV, Brosch R, Billault A, Garnier T, Eiglmeier K, Cole ST. Identification of variable regions in the genomes of tubercle bacilli using bacterial artificial chromosome arrays. Mol Microbiol. 1999;32(3):643–655. doi: 10.1046/j.1365-2958.1999.01383.x. [DOI] [PubMed] [Google Scholar]
- 15.Namwat W, Luangsuk P, Palittapongarnpim P. The genetic diversity of Mycobacterium tuberculosis strains in Thailand studied by amplification of DNA segments containing direct repetitive sequences. Int J Tuberc Lung Dis. 1998;2(2):153–159. [PubMed] [Google Scholar]
- 17.Phyu S, Jureen R, Ti T, Dahle UR, Grewal HM. Heterogeneity of Mycobacterium tuberculosis isolates in Yangon, Myanmar. J Clin Microbiol. 2003;41(10):4907–4908. doi: 10.1128/JCM.41.10.4907-4908.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sola C, Rastogi N. Genetic description and frequency maps of some major families of Mycobacterium tuberculosis. In: Ngeow YF, Yap SF, editors. Molecular Epidemiology and Population Genetics of Tuberculosis. Kuala Lumpur: Academy of Sciences of Malaysia; 2006. pp. 23–68. [Google Scholar]
- 19.Vijaya-Bhanu N, van Soolingen D, van Embden JDA, Dar L, Pandey RM, Seth P. “Predominance of a novel Mycobacterium tuberculosis genotype in the Delhi region of India”. Tuberculosis. 2002;82(2\3):105–112. doi: 10.1054/tube.2002.0332. [DOI] [PubMed] [Google Scholar]
- 20.Kulkarni SSC, Filliol I, Rastogi N, Kadival G. Spoligotyping of Mycobacterium tuberculosis isolates from patients with pulmonary tuberculosis in Mumbai, India. Res Microbiol. 2005;156(4):588–596. doi: 10.1016/j.resmic.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Gascoyne-Binzi D, Barlow RE, Essex A, Gelletlie R, Khan MA, Hafiz S F R, Collyns TA, Hawkey PM. Predominant VNTR family of strains of Mycobacterium tuberculosis isolated from South Asian patients. Int J Tuberc Lung Dis. 2002;6(6):492–496. doi: 10.5588/09640569512995. [DOI] [PubMed] [Google Scholar]
- 22.Farnia P, Mohammadi F, Masjedi MR, Varnerot A, Zarifi AZ, Tabatabee J, Douraghei M, Ghazisaeedi K, Mansorri D, Bahadori M, et al. Evaluation of tuberculosis transmission in Tehran: using RFLP and spoligotyping methods. J Infect. 2004;49(2):94–101. doi: 10.1016/j.jinf.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Sebban M, Mokrousov I, Rastogi N, Sola C. A Datamining approach to Spacer Oligonucleotide Typing of Mycobacterium tuberculosis. Bioinformatics. 2002;18:235–243. doi: 10.1093/bioinformatics/18.2.235. [DOI] [PubMed] [Google Scholar]
- 24.Republic of Uganda, Ministry of Health, author. National tuberculosis and Leprosy programme, South Western Uganda Annual report. 2005
- 25.Republic of Uganda, Ministry of Health, author. National tuberculosis and Leprosy programme, South Western Uganda Annual report. 2008
- 26.Kent P, Kubica G. Public health mycobacteriology: A guide for the level III laboratory. Atlanta, Ga: U. S. department of Health and Human Services. Centers for Disease Control, Atlanta, Ga. Centres for Disease Control; 1985. [Google Scholar]
- 27.van Embden JD, Cave MD, Crawford JT, Dale JW, Eisenach KD, Gicquel B, Hermans P, Martin C, McAdam R, Shinnick TM, et al. Strain identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J Clin Microbiol. 1993;31(2):406–409. doi: 10.1128/jcm.31.2.406-409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asiimwe BB, Koivula T, Kallenius G, Huard RC, Ghebremichael S, Asiimwe J, Joloba ML. Mycobacterium tuberculosis Uganda genotype is the predominant cause of TB in Kampala, Uganda. Int J Tuberc Lung Dis. 2008;12(4):386–391. [PubMed] [Google Scholar]
- 29.Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, Bunschoten A, Molhuizen H, et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997;35(4):907–914. doi: 10.1128/jcm.35.4.907-914.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brudey K, Driscoll JR, Rigouts L, Prodinger WM, Gori A, Al-Hajoj SA, Allix C, Aristimuno L, Arora J, Baumanis V, Binder L, Cafrune P, Cataldi A, et al. Mycobacterium tuberculosis complex genetic diversity: mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol. 2006;6:23. doi: 10.1186/1471-2180-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allix-Béguec C, Harmsen D, Weniger T, Supply P, Niemann S. Evaluation and user-strategy of MIRU-VNTRplus, a multifunctional database for online analysis of genotyping data and phylogenetic identification of Mycobacterium tuberculosis complex isolates. J Clin Microbiol. 2008;46(8):2692–2699. doi: 10.1128/JCM.00540-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Republic of Uganda, Ministry of Health, author. Manual of the National Tuberculosis and Leprosy programme in Uganda for district TB /Leprosy supervisors: First edition. 1992 Jun
- 33.Asiimwe BB, Ghebremichael S, Kallenius G, Koivula T, Joloba ML. Mycobacterium tuberculosis spoligotypes and drug susceptibility pattern of isolates from tuberculosis patients in peri-urban Kampala, Uganda. BMC Infect Dis. 2008;8:101. doi: 10.1186/1471-2334-8-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kibiki G, Mulder B, Dolmans WM, de Beer JL, Boeree M, Sam N, van Soolingen D, Sola C, Zanden AG. M. tuberculosis genotypic diversity and drug susceptibility pattern in HIV-infected and non-HIV-infected patients in northern Tanzania. BMC Microbiol. 2007;7(51) doi: 10.1186/1471-2180-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eldholm V, Matee M, Mfinanga SGM, Heun M, Dahle UR. A first insight into the genetic diversity of Mycobacterium tuberculosis in Dar es Salaam, Tanzania, assessed by spoligotyping. BMC Microbiol. 2006;6:76. doi: 10.1186/1471-2180-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Niemann S, Rusch Gerdes S, Joloba ML, Whalen CC, Guwatudde D, Ellner JJ, Eisenach K, Fumokong N, Johnson LJ, Aisu T, et al. Mycobacterium africanum subtype II is associated with two distinct genotypes and is a major cause of human tuberculosis in Kampala, Uganda. J Clin Microbiol. 2002;40:3398–3405. doi: 10.1128/JCM.40.9.3398-3405.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Niemann S, Kubica T, Bange F C, Adjei O, Browne EN, Chinbuah MA, Diel R, Gyapong J, Horstmann RD, Joloba ML, Meyer CG, Mugerwa RD, Okwera A, Osei I, Owusu-Darbo E, Schwander SK, Rusch-Gerdes S. The species Mycobacterium africanum in the light of new molecular markers. J Clin Microbiol. 2004;42:3958–3962. doi: 10.1128/JCM.42.9.3958-3962.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brudey KDJ, Rigouts L, Prodinger WM, Gori A, Al Hajoj SA, Allix C, Arora J, Baumanis V, Binder L, Cafrune P, et al. Mycobacterium tuberculosis complex genetic diversity: mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol. 2006;6(23) doi: 10.1186/1471-2180-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gagneux S, Small PM. Global phylogeography of Mycobacterium tuberculosis and implications for tuberculosis product development. Lancet Infect Dis. 2007;7(5):328–337. doi: 10.1016/S1473-3099(07)70108-1. [DOI] [PubMed] [Google Scholar]
- 40.Githui W, Jordaan AM, Juma ES, Kinyanjui P, Karimi FG, Kimwomi J, Meme H, Streicher EM, Warren R, Mumbi P, van Helden PD, Victor TC. Identification of MDR-TB Beijing/W and other Mycobacterium tuberculosis genotypes in Nairobi, Kenya. Int J Tuberc Lung Dis. 2004;8(3):352–360. [PubMed] [Google Scholar]
- 41.Kallenius G, Koivula T, Ghebremichael S, Hoffner SE, Norberg R, Svensson E, Dias F, Marklund BI, Svenson SB. Evolution and clonal traits of Mycobacterium tuberculosis complex in Guinea-Bissau. J Clin Microbiol. 1999;37(12):3872–3878. doi: 10.1128/jcm.37.12.3872-3878.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Niobe-Eyangoh SN, Kuaban C, Sorlin P, Thonnon J, Vincent V, Gutierrez MC. Molecular characteristics of strains of the cameroon family, the major group of Mycobacterium tuberculosis in a country with a high prevalence of tuberculosis. J Clin Microbiol. 2004;42(11):5029–5035. doi: 10.1128/JCM.42.11.5029-5035.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Easterbrook PJ, Murad S, Lamprecht D, Ives N, Ferguson A, Lowe O, Mason P, Ndudzo A, Taziwa A, Makombe R, Mbengeranwa L, Sola C, Rostogi N, Drobniewski F. High Rates of Clustering of Strains Causing Tuberculosis in Harare, Zimbabwe: a Molecular Epidemiological Study. J Clin Microbiol. 2004;42(10):4536–4544. doi: 10.1128/JCM.42.10.4536-4544.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chihota V, Apers L, Mungofa S, Kasongo W, Nyoni IM, Tembwe R, Mbulo G, Tembo M, Streicher EM, van der Spuy GD, Victor TC, van Helden P, Warren RM. Predominance of a single genotype of Mycobacterium tuberculosis in regions of Southern Africa. Int J Tuberc Lung Dis. 2007;11(3):311–318. [PubMed] [Google Scholar]