Abstract
Background
Methods used by dental practitioners to diagnose and treat dentin hypersensitivity are not well documented. The authors conducted a survey of dentists in the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT) to ascertain the treatment methods they used.
Methods
Via an Internet survey, the authors collected data regarding methods used for diagnosis and treatment of dentin hypersensitivity from 209 Northwest PRECEDENT dentists.
Results
The PRECEDENT dentists indicated that they most often used fluoride varnishes and gels, advice regarding toothbrushing and diet, bonding agents, restorative materials and glutaraldehyde/2-hydroxyethyl methacrylate (HEMA) to treat dentin hypersensitivity. They reported that the most successful treatments were fluorides, glutaraldehyde/HEMA, bonding agents, potassium nitrates and restorative treatments; they considered observation, advice regarding toothbrushing and diet and laser therapy to be the least successful. Dentists listed fluorides, calcium phosphates, glutaraldehyde/HEMA and bonding agents as the treatments most desirable for inclusion in a future randomized clinical trial of dental hypersensitivity treatments.
Conclusions
Dentists rely on patients to assess the severity of dentin hypersensitivity. Modalities for the diagnosis and treatment of hypersensitivity are diverse. Methods used to diagnose and treat dentin hypersensitivity in practice are challenging to justify.
Clinical Implications
Practitioners should be aware of the diversity of methods available for diagnosing and treating dentin hypersensitivity as they manage the care of their patients with this condition.
Keywords: Dentin hypersensitivity, practice-based research
Dentin hypersensitivity can be defined as a short, sharp pain arising when dentin is exposed to evaporative, thermal, tactile, osmotic or chemical stimuli and the pain cannot be ascribed to any other dental defect or disease.1,2 Dentin hypersensitivity is believed to be activated by fluid flow within dentin tubules resulting from changes in temperature or from physical or osmotic stimuli near an exposed dentin surface. Patients report pain as being triggered principally by cold drinks but also by hot drinks, toothbrushing and sweet foods.3 Fluid flow purportedly excites baroreceptors, leading to neural discharge—the so-called hydrodynamic theory of pain.4 The hydrodynamic theory assumes that tubules are patent between the exposed dentin surface and the pulp. Dentin tubules may become exposed as a result of enamel loss from attrition, abrasion, erosion (acid dissolution) or abfraction (cervical stress lesion)5; however, dentin exposure most often results from gingival recession accompanied by cementum loss from the root surfaces of canines and premolars.6–8
Dentin hypersensitivity is diagnosed by means of a patient’s self-report of pain, the evaluation of the patient’s response to various stimuli, and the exclusion of other dental and periodontal conditions. Conditions that should be ruled out include dental caries, pulpitis, cracked tooth structure, fractured restorations, postrestorative sensitivity, occlusal trauma, marginal leakage, chipped teeth and gingival inflammation.1 Therefore, dentin hypersensitivity is, by definition, a diagnosis of exclusion.9,10 The diagnosis of dentin hypersensitivity also may include a subjective evaluation of its effect on daily life.9
Numerous methods have been used to treat or manage dentin hypersensitivity. The ideal desensitizing agent should not irritate or endanger the pulp, should be relatively painless when applied or shortly afterward, should be easily applied, should act rapidly, should be permanently effective, should be cost effective and should not discolor tooth structure.11 Current treatment approaches attempt to reduce pain by targeting the pulpal nerves directly (typically with potassium nitrate) or by occluding the dentin tubules with a precipitating compound or a sealing agent, with a secondary goal of remineralizing the dentin. Diverse agents or formulations have shown various degrees of effectiveness in reducing the symptoms of dentin hypersensitivity, with some being applied professionally and others being applied as at-home treatments.10,11
The varied array of surface treatments for dentin hypersensitivity suggests that no single treatment meets all of the ideal criteria. Furthermore, the testing of new products is hampered by the lack of a gold standard for comparison. At present, there is no evidence demonstrating the superiority of any one desensitizing agent; treatment choice seems to depend mostly on the practitioner’s experiences and personal preferences.10,11 Therefore, we conducted a study to identify the diagnostic and treatment options for dentin hypersensitivity used by dentists in the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT). Our hypothesis was that accurate data regarding what dentists currently use most successfully will help define prospective studies of effective treatments.
PARTICIPANTS, MATERIALS AND METHODS
We conducted a survey regarding the diagnosis and treatment of dentin hypersensitivity within Northwest PRECEDENT, a practice-based dental research network. The PRECEDENT dental research network is composed of general dentists and orthodontists from five states in the northwestern United States: Idaho, Montana, Oregon, Utah and Washington. In addition, dentists from other specialties or from other states outside the five-state region have been recruited to the network as “Friends of PRECEDENT.” Dentists join the network either as dentist-investigators or Friends of PRECEDENT by completing an online registration at the Northwest PRECEDENT Web site (“www.nwprecedent.net”) after hearing about the network in conferences and journals or receiving a letter of invitation.12 Dentist-investigators participate in clinical studies only after completing training in principles of clinical research, responsible conduct of research for human participants and relevant regulations for research.13 Friends of PRECEDENT do not participate in clinical research involving patients but may participate in surveys. As in most practice-based research networks, dentists who participate in PRECEDENT do not necessarily provide a representative sample of dentists at large.
For our survey, we invited all general dentists from the five-state region and Friends of PRECEDENT (a convenience sample of 301 dentists) to participate, by means of a letter or an e-mail message containing a brief explanation of the study and instructions about how to log on to the data-capture Web site. The Web site used to conduct the survey was open from December 2008 through June 2009, and we made attempts to increase the response rate by contacting the dentists via e-mail, letters and telephone calls during this period. Dentists did not receive training to complete the survey, which required an estimated 20 minutes to complete. Dentists who completed the survey received a monetary token of appreciation. The institutional review board at the University of Washington, Seattle, approved the study protocol and survey.
We collected information regarding types and frequency of use of different methods of diagnosis and treatment of dentin hypersensitivity. As part of the survey, we asked dentists to indicate which treatment methods they used for dentin hypersensitivity from a list of commonly used treatment classifications: oxalates, fluorides, glutaraldehyde/2-hydroxyethyl methacrylate (HEMA), bonding agents or dentin adhesives, potassium nitrates, calcium phosphates, bioactive glass or others. If a dentist placed a response in the wrong category of treatment, we tallied it in the appropriate category during our analysis. In addition, the dentists were asked to indicate their frequency of use of each treatment (occasionally, some of the time, most of the time or all the time). We defined frequent use as use of a treatment most of the time or all the time. Dentists also indicated their opinions regarding which three treatments they considered least and most successful and the three treatments they would most like to see tested in a randomized clinical trial.
We also collected information about the dentists themselves, as well as about their practices. The personal characteristics included age, sex, race, ethnicity, number of years in dental practice and the dental school from which they graduated. The dental practice characteristics included the practice type (private solo or group practice, community clinic, managed care or other), the community setting (rural, urban or suburban), estimated age distribution of patients (average percentage of children, adults and seniors) and estimated payment options accepted (average percentage of patients with private insurance, enrolled in a public assistance program or enrolled in a fee-for-service plan). We estimated prevalences for responses by using sample proportions.
RESULTS
Of the 301 dentists invited to participate in the survey, 209 answered the questionnaire; 10 declined; 20 were not reached by e-mail, telephone, fax or mail; and 62 did not respond. Among the 209 dentists who participated in the survey, 93 percent were general dentists and 28 percent were Friends of PRECEDENT. Among the 92 dentists who did not participate, 80 percent were general dentists and 26 percent were Friends of PRECEDENT. The response rate was 69 percent (209 of 301). On average, dentists completed the survey after 2.4 follow-up attempts (median = 1; interquartile range, 0–5).
The typical dentist participating in the survey was a non-Hispanic white male, 51 to 60 years old, who had been in practice for more than 21 years. Dentists of all age groups were well represented, with 26 percent of respondents in the group aged 20 to 40 years and 16 percent in the group older than 60 years, compared with 33 percent in the most common age group (51–60 years). Dentists with more than 21 years in practice dominated the respondents (51 percent) relative to those in practice one to 10 years (22 percent) and those in practice 11 to 20 years (20 percent). It was common for respondents to have received their dental training in the Northwest, nearly equally in Washington and Oregon (21 percent and 26 percent, respectively), but receipt of training outside these states also was common (applying to 45 percent of respondents). Women and minorities were well represented, with 15 percent of respondents being female and 16 percent of respondents describing themselves as being nonwhite.
The typical dental practice of the responding practitioners was a private solo practice (72 percent) in a suburban setting (43 percent), with a wide age range of patients (20 percent were older than 65 years; 54 percent were aged 18–64 years; 27 percent were aged 0–17 years) who paid for care primarily via private insurance (61 percent). Rural and urban practices were common (27 and 27 percent, respectively). One-quarter of the dental practices were group practices, community clinics or managed-care settings, and 13 percent of the patients paid by means of public assistance programs. (Not all responses total 100 percent because some respondents provided incomplete answers.) Of all the demographic questions, the one regarding dental school was the only variable for which more than 10 percent of respondents did not provide information (12 percent).
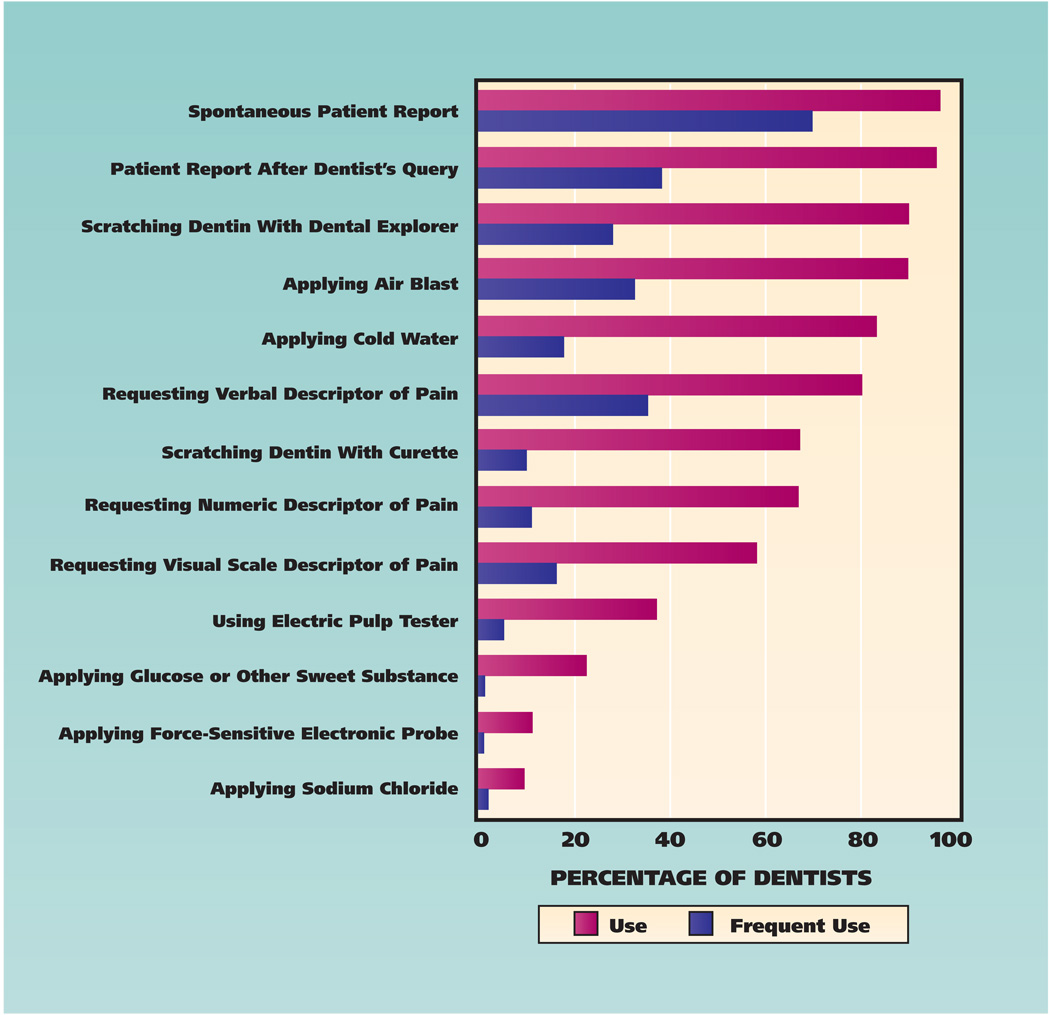
Methods used by responding practitioners to diagnose dentin hypersensitivity were diverse and used inconsistently (Figure 1). The most frequently reported diagnostic method was a spontaneous patient report (97 percent of practitioners), which 70 percent of practitioners indicated they used frequently. Patient reports prompted by a query from the dentist also were common (96 percent) but not used as frequently (38 percent) as spontaneous reports. Practitioners frequently requested verbal (80 percent) or numeric (58 percent) descriptions of the pain or required the patient to rate the pain level on a visual scale of some type (37 percent).
Figure 1.
Methods used by dentists (N = 209) in the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry to diagnose dentin hypersensitivity.
The use of an explorer and air blast (90 percent) was the most common means of assessing dentin hypersensitivity clinically, but the use of cold water (83 percent) and a curette (67 percent) also was common. Less commonly used methods of assessment were the use of an electric pulp tester (37 percent), application of glucose or sodium chloride (22 and 9 percent, respectively) or use of a force-sensitive electronic probe (11 percent). Less than 5 percent of respondents did not answer one or more questions regarding the frequency of use of the different methods to diagnose dentin hypersensitivity.
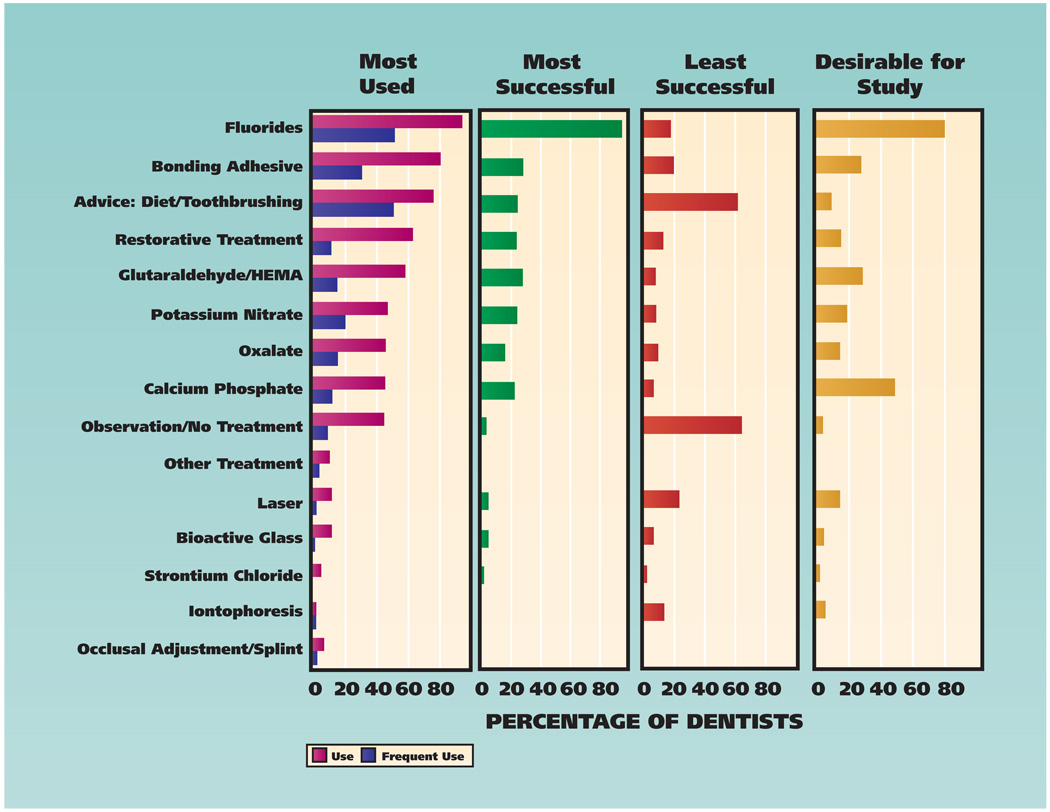
Respondents used a wide variety of methods to treat dentin hypersensitivity (Table 1), and they appeared to have notably different opinions as to which methods were most (Table 2, page 1102) and least (Table 3, page 1103) successful. Practitioners used a mean of 8.2 (standard deviation [SD] = 3.3) different products or techniques to treat dentin hypersensitivity and a mean of 2.7 (SD = 2.1) techniques frequently. When we grouped the results from Tables 1 through 3 (Figure 2, page 1104), several patterns emerged. Fluoride use was, by far, the most common treatment modality (94 percent) and was the only treatment for dentin hypersensitivity used frequently by more than 50 percent of the respondents. Practitioners commonly rated fluoride use as their most successful treatment modality (96 percent) and only occasionally indicated that fluorides were least successful (18 percent). Other commonly used treatments for dentin hypersensitivity were application of bonding agents (81 percent), restorative treatments (63 percent) and application of glutaraldehyde/HEMA (58 percent). Yet, respondents did not commonly rate these latter three treatments as most successful (< 35 percent). Other treatment types that respondents used relatively frequently were application of potassium nitrates (47 percent), application of oxalates (46 percent) and application of calcium phosphates (46 percent); respondents only occasionally rated these treatment methods as most successful.
TABLE 1.
Products or techniques most used and used frequently (most or all of the time) by Northwest PRECEDENT* dentists (N = 209) to treat dentin hypersensitivity.
| PRODUCT† OR TECHNIQUE | DENTISTS WHO USE IT (%) |
DENTISTS WHO USE IT FREQUENTLY (%) |
|---|---|---|
| Advice Regarding Toothbrushing | 73 | 47 |
| PreviDent Gel | 53 | 18 |
| Advice Regarding Diet | 48 | 28 |
| Resin-Based Composite | 46 | 6 |
| Gluma Desensitizer | 45 | 10 |
| Glass Ionomers | 42 | 7 |
| Over-the-Counter Potassium Nitrate Toothpaste | 37 | 16 |
| Duraflor | 37 | 14 |
| Watchful Waiting | 37 | 7 |
| MI Paste | 31 | 7 |
| Clearfil SE Bond | 30 | 10 |
| Protect Desensitizing Solution | 22 | 5 |
| Omni Vanish 5% NaF White Varnish | 22 | 12 |
| Prime & Bond NT | 21 | 7 |
| No Treatment | 19 | 2 |
| Optibond | 19 | 9 |
| MI Paste Plus | 17 | 6 |
| Duraphat | 14 | 3 |
| Gel-Kam Gel | 14 | 4 |
| Sensodyne Sealant | 14 | 6 |
| Lasers | 11 | 1 |
| Omni Cavity Shield Varnish | 10 | 2 |
| Scotchbond | 10 | 2 |
| SootheRx | 9 | 1 |
| D/Sense Crystal Dual-Action Crystal Precipitate Desensitizer | 8 | 1 |
| Other Fluoride-Based Product | 23 | 11 |
| Other Glutaraldehyde/HEMA ‡–Based Product | 21 | 5 |
| Other Bonding Agent or Dentin Adhesive | 20 | 5 |
| Other Potassium Nitrate–Based Product | 14 | 4 |
| Other Oxalate-Based Product | 12 | 4 |
| Other Products or Techniques | 30 | 11 |
PRECEDENT: Practice-based REsearch Collaborative in Evidence-based DENTistry.
Manufacturers are as follows (products listed in alphabetical order): Clearfil SE Bond (Kuraray America, New York City); D/Sense Crystal Dual-Action Crystal Precipitate Desensitizer (Centrix, Shelton, Conn.); Duraflor (Medicom, Atlanta); Duraphat (Colgate, New York City); Gel-Kam Gel (Colgate); Gluma Desensitizer (Heraeus Kulzer, South Bend, Ind.); MI Paste (Ortho Technology, Tampa, Fla.); MI Paste Plus (Ortho Technology); Omni Cavity Shield Varnish (Omni Preventive Care, West Palm Beach, Fla.); Omni Vanish 5% NaF White Varnish (Omni Preventive Care); Optibond (Kerr Sybron, Orange, Calif.); PreviDent Gel (Colgate); Prime & Bond NT (Dentsply, Milford, Del.); Protect Desensitizing Solution (Sunstar Butler, Chicago); Scotchbond (3M ESPE, St. Paul, Minn.); Sensodyne Sealant (GlaxoSmithKline, Philadelphia); SootheRx (3M ESPE).
HEMA: 2-Hydroxyethyl methacrylate.
TABLE 2.
Products or techniques considered by Northwest PRECEDENT* dentists (N = 209) to be most successful in treating dentin hypersensitivity.
| PRODUCT† OR TECHNIQUE | DENTISTS RATING IT MOST SUCCESSFUL (%) |
|---|---|
| Gluma Desensitizer | 23 |
| Duraflor | 19 |
| PreviDent Gel | 17 |
| Advice Regarding Toothbrushing | 16 |
| MI Paste | 14 |
| Over-the-Counter Potassium Nitrate Toothpaste | 14 |
| Glass Ionomers | 13 |
| Omni Vanish 5% NaF White Varnish | 11 |
| Resin-Based Composite | 11 |
| Clearfil SE Bond | 9 |
| Duraphat | 8 |
| Advice Regarding Diet | 7 |
| MI Paste Plus | 7 |
| Gel-Kam Gel | 6 |
| Protect Desensitizing Solution | 6 |
| Other Bonding Agent or Dentin Adhesive | 24 |
| Other Fluoride Varnish Product | 18 |
| Other Fluoride–Based Product | 14 |
| Other Potassium Nitrate–Based Product | 10 |
| Other Products or Techniques | 24 |
PRECEDENT: Practice-based REsearch Collaborative in Evidence-based DENTistry.
Manufacturers are as follows (products listed in alphabetical order): Clearfil SE Bond (Kuraray America, New York City); Duraflor (Medicom, Atlanta); Duraphat (Colgate, New York City); Gel-Kam Gel (Colgate); Gluma Desensitizer (Heraeus Kulzer, South Bend, Ind.); MI Paste (Ortho Technology, Tampa, Fla.); MI Paste Plus (Ortho Technology); Omni Vanish 5% NaF White Varnish (Omni Preventive Care, West Palm Beach, Fla.); PreviDent Gel (Colgate); Protect Desensitizing Solution (Sunstar Butler, Chicago).
TABLE 3.
Products or techniques considered by Northwest PRECEDENT* dentists (N = 209) to be least successful in treating dentin hypersensitivity.
| PRODUCT† OR TECHNIQUE | DENTISTS RATING IT LEAST SUCCESSFUL (%) |
|---|---|
| Advice Regarding Diet | 43 |
| Watchful Waiting | 39 |
| No Treatment | 25 |
| Lasers | 22 |
| Advice Regarding Toothbrushing | 19 |
| Iontophoresis | 13 |
| Resin-Based Composite | 7 |
| Glass Ionomers | 6 |
| Den-Mat Desensitize! | 3 |
| Gel-Kam Rinse | 3 |
| Strontium Chloride | 3 |
| Gel-Kam Gel | 3 |
| Other Bonding Agent or Dentin Adhesive | 22 |
| Other Glutaraldehyde/HEMA ‡–Based Product | 8 |
| Other Fluoride Varnish Product | 7 |
| Other Bioactive Glass Product | 5 |
| Other Products or Techniques | 28 |
PRECEDENT: Practice-based REsearch Collaborative in Evidence-based DENTistry.
Manufacturers are as follows (products listed in alphabetical order): Den-Mat Desensitize! (DenMat, Santa Maria, Calif.); Gel-Kam Gel (Colgate, New York City); Gel-Kam Rinse (Colgate).
HEMA: 2-Hydroxyethyl methacrylate.
Figure 2.
Treatments for dentin hypersensitivity considered by dentists (N = 209) in the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry to be most frequently used, most and least successful, and most desirable for future study. HEMA: 2-hydroxyethyl methacrylate.
Several treatments for dentin hypersensitivity were used relatively rarely, including iontophoresis (1 percent), application of strontium chloride (4 percent) or bioactive glasses (10 percent), and use of lasers (11 percent) (Figure 2). Respondents rarely, if ever, rated these treatment methods as most successful. Giving advice regarding diet or toothbrushing techniques (76 percent) and observation (45 percent) were relatively common, but these often were rated as the least successful means of treatment (51 and 64 percent, respectively). Less than 10 percent of the respondents failed to answer one or more questions about use of treatments for dentin hypersensitivity.
When queried about aspects of treatment of dentin hypersensitivity for which they would like further investigation, respondents suggested a wide variety of treatments (Figure 2) but most commonly suggested fluorides (79 percent), calcium phosphates (48 percent), glutaraldehyde/HEMA (29 percent) and bonding agents (28 percent). Respondents did not demonstrate as much interest in further study of other treatment methods, including potassium nitrates, restorative treatments, oxalates and lasers.
DISCUSSION
The primary goal of our study was to assess the methods of diagnosis and treatment of dentin hypersensitivity used by practicing dentists. The data we obtained were limited to the northwestern United States; these results should be extended to a broader geographic region only with caution. The survey results suggest that practitioners commonly rely on the patient to report and assess the presence and severity of dentin hypersensitivity and use a wide variety of products and techniques to treat the condition. Fluoride was a common treatment and the one respondents most often viewed as successful, whereas they most often viewed observation, lasers, and dietary and toothbrushing advice as least successful. Understanding the state of current practice with regard to dentin hypersensitivity may aid clinicians in considering their treatment options and may provide researchers with a baseline from which to design clinical studies that test relevant treatment and diagnostic strategies.
Our survey results indicated that the responding dentists relied primarily on patients’ reports, either spontaneous or generated via the dentist’s query, to identify dentin hypersensitivity. The respondents also commonly relied on patients to describe the severity of their sensitivity via comparison with other sources of pain. Beyond patients’ reports, practitioners used various means to confirm and assess dentin hypersensitivity clinically. Although these methods were diverse, most relied on mechanical, thermal or osmotic stimulation, suggesting that practitioners are aware of and subscribe to the current state of knowledge on hydrodynamic mechanisms.14 An exception was the use of the electric pulp tester, which nearly 40 percent of respondents used but which less than 5 percent of respondents used frequently. Practitioners’ reliance on patients’ complaints for diagnosis of dentin hypersensitivity suggested that they were not convinced of a reliable alternative clinical method of diagnosing dentin hypersensitivity in patients. The fact that few of the methods identified were used frequently supports this hypothesis. Given most of our respondents’ reliance on the patient’s spontaneous report to identify dentin hypersensitivity, the true prevalence of this condition may be underestimated.15–17
In our study, treatment choices were highly dependent on the practitioner and were split between at-home and in-office strategies. In a survey among Dutch general practitioners, 18 the treatments most often prescribed were at-home treatments: brushing with therapeutic toothpastes, advice regarding oral hygiene and application of therapeutic toothpastes or fluoride preparations at bedtime. In-office treatments were performed occasionally by 50 percent of the dentists and included the use of bonding agents or varnishes and, less frequently, cervical restoration. Another survey of general practitioners in the United Kingdom reported a wide range of treatments that included both in-office and at-home products; the most frequently used were desensitizing pastes and gels; fluoride varnishes, toothpastes, rinses or gels; advice regarding toothbrushing; bonding agents; and glass ionomer restorations.19 The results of our study are in agreement with the findings of these surveys.
The dentists in our survey used myriad products to treat dentin hypersensitivity, but the diversity of responses strongly suggested that the respondents were not convinced of the clinical efficacy of any of the treatments. On average, the same practitioner had tried eight different products or techniques to treat dentin hypersensitivity and had used three products or techniques frequently. One practitioner reported having used as many as 16 different products or techniques. The only exception was fluoride treatments, which a large majority of practitioners used and which nearly one-half used frequently. Most practitioners considered fluoride use a successful clinical strategy, but at least one-fifth did not. Yet, even within the group of those who used fluoride, the diversity of responses regarding the various fluoride products was substantial and suggests practitioners’ lack of confidence in the treatments. The indication that a large majority of practitioners in our study would like to see more studies about the efficacy of fluorides supports this view.
Beyond fluorides, few products or strategies to treat dentin hypersensitivity were used frequently by the respondents, and few were deemed among the most successful. The relative prevalence of the use of restorative materials such as resin-based composites, glutaraldehyde/HEMA or bonding agents is not surprising, given the prevalence of these materials in the arsenal of most dental practices and practitioners’ familiarity with them. The use of these restorative materials perhaps is understandable intuitively, but our respondents did not commonly consider these approaches most successful and nearly as often viewed them as least successful.
Although providing advice about diet or toothbrushing was a common approach to management of dentin hypersensitivity, most respondents did not consider it a successful clinical strategy. Only one-fourth of practitioners viewed this approach as among the most successful, whereas nearly two-thirds viewed it as among the least successful. Observation and waiting, although not as commonly used, also ranked among the least successful strategies. The message from the respondents in this survey was that, more often than not, doing nothing or attempting to change the patient’s hygiene or dietary practices were not promising approaches. The few practitioners who desired further research into the observation technique or who thought more study about diet and toothbrushing was advisable strongly emphasized this point. The use of less accepted treatments such as lasers, bioactive glasses or iontophoresis may suggest that dentists are not satisfied with the more common treatment methods available and are willing to try other methods even if they are not used commonly or proven clinically.
Queries of respondents about their wish for further studies yielded two curious findings. First, respondents had a surprising desire for further study of calcium phosphates, even though relatively few dentists used them frequently or considered the treatment to be among the most successful. This interest may stem in part from a combination of the influence of advertising and dissatisfaction with other, more established treatment modalities. Second, dentists did not express interest in further study of oxalates and nitrates despite the relatively common use of these treatments.
CONCLUSIONS
In our survey, we found that among dentists in the Northwest PRECEDENT network, treatment of dentin hypersensitivity with fluorides was the modality most used, most frequently used and most often viewed as successful. Observation or advice about diet and toothbrushing were most often viewed as least successful.
Products and techniques used for treatment of dentin hypersensitivity were diverse, suggesting uncertainty among dentists about the best way to treat patients, as well as dissatisfaction with outcomes of available treatments. Practitioners commonly relied on the patient to report and assess the presence and severity of dentin hypersensitivity.
Acknowledgments
This article was submitted on behalf of the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT) network with support from grants DE016750 and DE016752 from National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, Md.
ABBREVIATION KEY
- HEMA
2-Hydroxyethyl methacrylate.
- PRECEDENT
Practice-based Research Collaborative in Evidence-based DENTistry.
Footnotes
Disclosure. None of the authors reported any disclosures.
The authors appreciate the invaluable contributions of the dentist-investigator members of the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry and their staff members.
Information about obtaining reprints of this article or about permission to reproduce this article in whole or in part can be found at: http://www.ada.org/prof/resources/pubs/jada/permissions.asp
Contributor Information
Joana Cunha-Cruz, Department of Dental Public Health Sciences, School of Dentistry, University of Washington, 1959 N.E. Pacific St., Box 357475, Seattle, Wash. 98195-7475, “silvajcc@u.washington.edu”..
John C. Wataha, Department of Restorative Dentistry, School of Dentistry, University of Washington, Seattle..
Lingmei Zhou, Department of Dental Public Health Sciences, School of Dentistry, University of Washington, Seattle..
Walter Manning, maintains a private practice in dentistry in Albany, Ore., and is a dentist-investigator for the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry..
Michael Trantow, maintains a private practice in dentistry in Spokane Valley, Wash., and is a dentist-investigator for the Northwest Practice-based Research Collaborative in Evidence-based DENTistry..
Meishan M. Bettendorf, Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry, University of Washington, Seattle..
Lisa J. Heaton, Department of Dental Public Health Sciences, School of Dentistry, University of Washington, Seattle..
Joel Berg, Department of Pediatric Dentistry, School of Dentistry, University of Washington, Seattle..
References
- 1.Canadian Advisory Board on Dentin Hypersensitivity. Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. J Can Dent Assoc. 2003;69(4):221–226. [PubMed] [Google Scholar]
- 2.Chabanski MB, Gillam DG. Aetiology, prevalence and clinical features of cervical dentine sensitivity. J Oral Rehabil. 1997;24(1):15–19. doi: 10.1046/j.1365-2842.1997.00471.x. [DOI] [PubMed] [Google Scholar]
- 3.Rees JS, Addy M. A cross-sectional study of dentine hypersensitivity. J Clin Periodontol. 2002;29(11):997–1003. doi: 10.1034/j.1600-051x.2002.291104.x. [DOI] [PubMed] [Google Scholar]
- 4.Brannstrom M, Astrom A. The hydrodynamics of the dentine: its possible relationship to dentinal pain. Int Dent J. 1972;22(2):219–227. [PubMed] [Google Scholar]
- 5.Smith BG, Knight JK. A comparison of patterns of tooth wear with aetiological factors. Br Dent J. 1984;157(1):16–19. doi: 10.1038/sj.bdj.4805401. [DOI] [PubMed] [Google Scholar]
- 6.Orchardson R, Collins WJ. Clinical features of hypersensitive teeth. Br Dent J. 1987;162(7):253–256. doi: 10.1038/sj.bdj.4806096. [DOI] [PubMed] [Google Scholar]
- 7.Chabanski MB, Gillam DG, Bulman JS, Newman HN. Prevalence of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department. J Clin Periodontol. 1996;23(11):989–992. doi: 10.1111/j.1600-051x.1996.tb00525.x. [DOI] [PubMed] [Google Scholar]
- 8.Chabanski MB, Gillam DG, Bulman JS, Newman HN. Clinical evaluation of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department: a pilot study. J Oral Rehabil. 1997;24(9):666–672. doi: 10.1046/j.1365-2842.1997.00552.x. [DOI] [PubMed] [Google Scholar]
- 9.Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol. 1997;24(11):808–813. doi: 10.1111/j.1600-051x.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 10.Dababneh RH, Khouri AT, Addy M. Dentine hypersensitivity: an enigma? A review of terminology, mechanisms, aetiology and management. Br Dent J. 1999;187(11):606–611. doi: 10.1038/sj.bdj.4800345. [DOI] [PubMed] [Google Scholar]
- 11.Grossman L. A systematic method for the treatment of hypersensitive dentin. JADA. 1935;22(3):592–598. [Google Scholar]
- 12.DeRouen T, Cunha-Cruz J, Hilton T, et al. What’s in a dental practice-based research network? Characteristics of Northwest PRECEDENT dentists, their patients and office visits. JADA. 2010;141(7):889–899. doi: 10.14219/jada.archive.2010.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeRouen TA, Hujoel P, Leroux B, et al. Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry: preparing practicing dentists to engage in practice-based research. JADA. 2008;139(3):339–345. doi: 10.14219/jada.archive.2008.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dowell P, Addy M. Dentin hypersensitivity: a review—1. Etiology, symptoms and theories of pain production. J Clin Perio. 1983;10(4):341–350. doi: 10.1111/j.1600-051x.1983.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 15.Gillam DG, Seo HS, Bulman JS, Newman HN. Perceptions of dentine hypersensitivity in a general practice population. J Oral Rehabil. 1999;26(9):710–714. doi: 10.1046/j.1365-2842.1999.00436.x. [DOI] [PubMed] [Google Scholar]
- 16.Gillam DG, Seo HS, Newman HN, Bulman JS. Comparison of dentine hypersensitivity in selected occidental and oriental populations. J Oral Rehabil. 2001;28(1):20–25. doi: 10.1046/j.1365-2842.2001.00631.x. [DOI] [PubMed] [Google Scholar]
- 17.Irwin CR, McCusker P. Prevalence of dentine hypersensitivity in a general dental population. J Ir Dent Assoc. 1997;43(1):7–9. [PubMed] [Google Scholar]
- 18.Schuurs AH, Wesselink PR, Eijkman MA, Duivenvoorden HJ. Dentists’ views on cervical hypersensitivity and their knowledge of its treatment. Endod Dent Traumatol. 1995;11(5):240–244. doi: 10.1111/j.1600-9657.1995.tb00496.x. [DOI] [PubMed] [Google Scholar]
- 19.Gillam DG, Bulman JS, Eijkman MA, Newman HN. Dentists’ perceptions of dentine hypersensitivity and knowledge of its treatment. J Oral Rehabil. 2002;29(3):219–225. doi: 10.1046/j.1365-2842.2002.00812.x. [DOI] [PubMed] [Google Scholar]