Abstract
Purpose
Depression and impulsivity have been positively correlated to problem gambling, but no study has focused on the combined effects of both on the onset of problem gambling. This study examined the possible synergistic effect of depressive symptoms and impulsivity in early adolescence on late adolescence gambling behaviors among a longitudinal cohort of 678 students from Baltimore, MD.
Methods
The South Oaks Gambling Screen-Revised for Adolescents (SOGS-RA), Teacher Observation of Classroom Adaptation Revised (TOCA-R), and Baltimore How I Feel-Adolescent Version (BHIF-AY), were used to assess late adolescence gambling behaviors, early adolescence impulsivity and depressive symptoms, respectively. Data analyses were conducted using ANOVA and binary logistic regression models.
Results
Twelve percent of the sample were problem gamblers (includes at-risk and problem gamblers), 87.5% of whom were males and 12.5% were females (p<0.001). Among males, there appeared to be a slight association between early adolescence depressive symptoms and late adolescence problem gambling. Compared to nongambling (NG) and social gambling (SG), depressive symptoms increased the odds of problem gambling by four-fold (PG vs. NG: OR=4.1, 95% CI=0.73–22.47, p=0.11; PG vs. SG: OR=3.9, 95% CI=0.78–19.31, p=0.10). Among those with high depressive symptoms, increases in impulsivity decreased the odds of problem gambling while among those with high impulsivity, increases in depressive symptoms decreased the odds of problem gambling.
Conclusions
Early adolescence depressive symptoms appear to be more positively associated with late adolescence problem gambling than early adolescence impulsivity, there seems to be a divisive interaction between depressive symptoms and impulsivity on problem gambling.
Keywords: Depressive symptoms, Impulsivity, Problem gambling, Early Adolescence, Late Adolescence
Introduction
As gambling venues and opportunities become more accessible and normalized, increasing numbers of underaged youths are participating in these activities. Between 70–90% of adolescents have gambled [1], and 3–8% are problem gamblers with another 10–15% at risk for the development of a gambling problem; considerably higher than the 1–3% of problem gamblers among the general adult population [2]. Adolescents at risk for problem gambling could go on to experience gambling-related consequences that may negatively impact their lives [3].
Adolescence is a vulnerable period marked by increased risk-taking. Studies suggest adolescents to be highly sensitive to environmental influences, and become more socially aware and engage in risk-taking behavior under the influence of social pressure [4]. Another explanation suggests that despite being cognitively aware of the risks involved, adolescents engage in risky behaviors due to their underestimation of the risks and belief that the risks are acceptable [5]. Adolescent gambling is a high-risk behavior believed to be a gateway to other deviant behaviors such as substance use, and is associated with adverse mental health outcomes such as depression and suicide [6].
Studies indicate an association between depression and problem gambling [7–9]. Generally, adolescent problem gamblers report increased depressive symptomatology compared to other adolescents [7]. Beaudoin and Cox [8] suggest that excessive gambling behavior is undertaken as a means to alleviate depressive symptoms. These coping gamblers can develop severe gambling problems because motivations behind coping with negative emotions and life concerns are associated with addictive behaviors [9].
Impulsivity, defined as a predisposition toward rapid, unplanned reactions to stimuli without regard to the negative consequences of these reactions to himself or to others [10], is a normative behavior during childhood development related to the neurobiological changes in both brain organization and function. Adolescents’ inability to refrain from impulsive behaviors is thought to be due to their underdeveloped inhibitory control [11]. Impulsivity is an important aspect of the personality of problem gamblers. Vitaro and colleagues [12] report that disruptiveness and low inhibition during childhood distinguished problem gamblers from social/nonproblem gamblers during adolescence.
While both depression and impulsivity have individually been found to be positively correlated to problem gambling [13], the studies have generally been univariate in that they focused on only one variable at a time in its association with gambling. However, several studies have shown a significant multiplicative interaction between depression and impulsivity on aggressive behaviors and alcohol involvement, both of which have been shown to be positively correlated to problem gambling [14,15]. Therefore this paper hypothesizes that the presence of both depressive symptoms and impulsivity exhibited in early adolescence (age 11) is positively associated with problem gambling during late adolescence (ages 17–20), and the association will be synergistic. This study aims to elucidate the probable relationship between depressive symptoms and impulsivity, and problem gambling.
Methods
Sample
The data came from the Johns Hopkins Center for Prevention and Early Intervention Cohort 3 [16], a study initiated as a randomized prevention trial targeting academic achievement and aggression. Recruitment occurred in Fall 1993 at nine urban primary schools, primarily located in western Baltimore, MD. Within each school, there were three 1st grade classrooms, which were randomly divided into two intervention and one control groups. The classroom-centered (CC) intervention, which created opportunities for more positive attention from teachers and peers, consisted of three components: curricular enhancements; improved classroom behavior management practices; and supplementary strategies for children not performing adequately [17]. The family-school partnership (FSP) intervention was designed to improve achievement and reduce early aggression and shy behavior by enhancing parent-school communication and providing parents with effective teaching and child behavior management strategies [17]. There was no prevention program for the control group, only the usual curriculum was provided [17].
At the time of school enrollment, first graders were randomly assigned to each of the three designated classrooms. Across the 27 classrooms, there were 678 children; 86% were African Americans, and 53% were males. Sixty-nine percent of the participants received free or reduced-price lunches, a proxy for family poverty. While the intervention only lasted for one year, the cohort was followed-up annually. Study protocols were approved by institutional review boards (IRB) of Johns Hopkins University.
Measures
Late Adolescent Gambling
The South Oaks Gambling Screen-Revised for Adolescents (S0GS-RA), a 12-item adaptation of the adult orientated SOGS, assesses gambling behavior in the past 12 months using wording of items and response options that reflect adolescence gambling behavior at an age appropriate reading level [18]. The scale correlates with gambling activity (r=0.39), gambling frequency (r=0.54), and the amount of money gambled in the past year (r=0.42). The Cronbach’s alphas are 0.86 for males and 0.76 for females [18]. The suggested scoring criteria set a cutoff score of 4 or more to indicate problem gambling, 2–3 to indicate at-risk problem gambling, and 0–1 to indicate social gambling among those who reported having gambled in the past 12 months [19]. Those who reported not having gambled in the past 12 months are nongamblers. Adolescent at-risk and problem gamblers have similar profiles [3]; therefore they were grouped together in the present study and will be collectively referred to as “problem gamblers” from this point on. The SOGS-RA were only administered in 2004, 2006, and 2007 (when respondents were aged 17, 19, and 20, respectively), and the three waves were combined as a cumulative measure of gambling behavior in this study’s sample.
Early Adolescent Impulsivity
The Teacher Observation of Classroom Adaption-Revised (TOCA-R) assesses childhood behaviors [20]. Trained assessors guide the 6th grade teachers through a structured interview of 36 items pertaining to the child’s adaptation to classroom task demands over the preceding three-week period. For this study, we focused on the subscale of Self regulation/Impulsivity (Cronbach’s alpha=0.79), which consists of three items—waits for turn, interrupts or intrudes on others, and blurts out answer before question is complete. Adaptation is rated on a six-point frequency scale, from 1 = almost never to 6 = almost always. An impulsivity score is created by taking the mean of the total sum, with a higher score indicating higher impulsivity. The four-month test-retest reliability for the subscale is over 0.60. The 6th grade TOCA-R data was used as the early adolescent measure of impulsivity.
Early Adolescent Depressive Symptoms
The Baltimore How I Feel-Adolescent Version (BHIF-AY) is a 45-item self-report scale assessing depressive and anxious symptoms among middle and high school youths [21]. Adolescents report the frequency of symptoms over the last two weeks on a four-point scale, from 1 = never to 4 = always or almost always. Depressive symptom scores are created by taking the means of the total responses to the 14 items, with higher scores indicating higher frequencies of symptoms. The Depression subscale has a two-week test-retest reliability coefficient of 0.83 and Cronbach’s alpha of 0.83 [22]. The 6th grade BHIF-AY data was utilized during analysis.
Statistical Analysis
Chi-square statistics were used to uncover the baseline demographic trends of the cohort. Individuals were divided into 3 gambling categories—nongamblers (NG), social gamblers (SG), and problem gamblers (PG). In an effort to create a cumulative measure of gambling, individuals were categorized based on their highest level of gambling behavior. ANOVA explored differences in the mean scores of the BHIF-AY and TOCA-R subscales across the three gambling categories, and the Pearson correlation coefficient was calculated for the depressive symptom and impulsivity scores.
An interaction term was created for the depressive symptoms and impulsivity scores. To eliminate any potential confounding that gender could introduce, ANOVA and logistic regressions were conducted separately for males and females. Several logistic regression models both with and without the interaction term, compared SG to NG (reference group=NG), PG to NG (reference group=NG), and PG to SG (reference group=SG). Depressive symptoms and impulsivity scores were further centered for better interpretation of the interaction effects [23]. Logistic regressions with the centered covariates, their interaction, adjusted for demographic variables, modeled the associations among early adolescence depressive symptoms and impulsivity and late adolescence gambling behavior.
Due to the initial study design, students were clustered within schools. Individuals belonging to the same cluster were likely to resemble one another due to their shared environment; and if the resemblances in outcomes among those in each cluster were ignored, the standard errors would be underestimated, inflating the Type I error [24]. As a result, using STATA 11.0 [25], a variant of the Huber-White sandwich estimator of variance was used to obtain robust standard errors and variance estimates.
Results
Demographics
Approximately 92% (n=618) of the original cohort of 678 were available for at least one of the 2004, 2006, and 2007 follow-ups. With the exception of race, those lost to follow-up did not differ from those who were available in terms of demographics, early adolescence depressive symptom and impulsivity. African-Americans were underrepresented (80.0% vs 86.9%) while Caucasians (18.3% vs 13.1%) were overrepresented among those lost to follow-up compared to those who were followed up (p=0.003). After gender stratification, the race disparity became insignificant among males but remained so among females (p=0.003).
Of the 618 participants, 45.2% (n=279) were NG, 43.2% (n=267) were SG, and 11.6% (n=72) were PG. There were no significant differences among the three gambling categories in terms of race, group assignment, and lunch status (Table 1). However, great disparity was found for gender (p<0.001) across the gambling groups. Females were more likely to be NG (59.1% vs 40.9%) while males were more likely to be SG (56.2% vs 43.8%) and PG (87.5% vs 12.5%).
TABLE 1.
Characteristics of Nongamblers, Social Gamblers, and Problem Gamblers
| NG | SG | PG | p value* | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Total | 279 (45.2) | 267 (43.2) | 72 (11.6) | -- |
| Gender | ||||
| Male | 114 (40.9) | 150 (56.2) | 63 (87.5) | <0.001 |
| Female | 165 (59.1) | 117 (43.8) | 9 (12.5) | |
| Race | ||||
| African-American | 245 (87.8) | 228 (85.4) | 64 (88.9) | 0.61 |
| Caucasian | 34 (12.2) | 39 (14.6) | 8 (11.1) | |
| Group Assignment | ||||
| Control | 97 (34.8) | 85 (31.8) | 18 (25.0) | 0.40 |
| CC | 94 (33.7) | 92 (34.5) | 23 (31.9) | |
| FSP | 88 (31.5) | 90 (33.7) | 31 (43.1) | |
| Lunch | ||||
| Free/reduced | 188 (68.1) | 183 (68.8) | 53 (75.7) | 0.46 |
| Paid | 88 (31.9) | 83 (31.2) | 17 (24.3) | |
Note. NG=Nongambler; SG=Social gambler; PG=Problem gambler (includes at-risk and problem gamblers); CC=Classroom-centered intervention; FSP=Family-school partnership intervention.
produced from Chi-square statistics
Impulsivity and Depressive Symptom Effects
Early adolescence depressive symptoms and impulsivity did not appear to be correlated to each other in the overall sample (r=−0.03, p=0.54), nor among males (r=−0.02, p=0.87) and females (r=−0.03, p=0.70). Little differences were found in the mean scores of depressive symptoms (NG=0.72, SG=0.72, PG=0.74, p=0.75) and impulsivity (NG=2.27, SG=2.32, PG=2.70, p=0.67) across the gambling categories. Females were 33% and 87% less likely than males to become SG and PG, respectively, in late adolescence (p<0.001).
Due to the gender disparity across the gambling categories (p<0.001), gender stratification was employed to eliminate any potential confounding gender might introduce. The small sample size of female PG (n=9) compromised the power of the analysis among females, therefore the presented results would be limited to only the males.
Prior to accounting for the interaction between depressive symptoms and impulsivity, the logistic regression model, adjusted for race, group assignment, and lunch status, showed that neither covariate differ significantly between male NG and SG (depressive symptoms: OR=1.31, 95% CI=0.29–5.05, p=0.73; impulsivity: OR=1.00, 95% CI=0.70,1.43; p=1.00). A similarly adjusted model without the interaction, comparing PG to NG, showed that while PG was not associated with impulsivity (OR=1.52, 95% CI=0.76–3.05, p=0.23), depressive symptoms reached borderline significance (OR=7.01, 95% CI=0.77–63.80, p=0.08). A third model comparing PG to SG found both covariates to be slightly associated with PG (depressive symptoms: OR=7.74, 95% CI=0.83–72.32, p=0.07; impulsivity: OR=1.80, 95% CI=0.87–3.69; p=0.11).
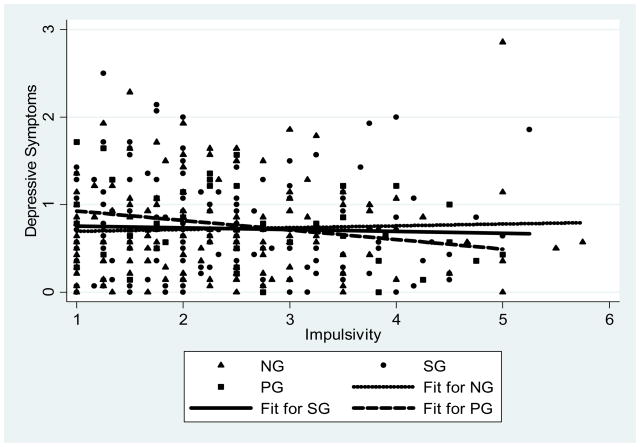
With the depressive symptoms × impulsivity interaction term (p=0.67) added to the logistic model comparing SG to NG, depressive symptoms and impulsivity remained to have little association (data not shown, available upon request). The interaction term reached borderline significance (p=0.06) in the model comparing PG to NG (Table 2). While depressive symptoms was slightly associated by increasing the odds of PG by 4.1-fold (95% CI=0.73–22.47, p=0.11), impulsivity did not appear to be associated (OR=0.54, 95% CI=0.59–1.31, p=0.54). Additionally, assignment into the FSP intervention group during grade 1 increased the odds of PG by more than 2-fold (OR=2.59, 95% CI=1.15–5.87, p=0.02). In a similar model with the interaction term (p=0.05), comparing PG to SG (Table 2), depressive symptoms reached borderline significance by increasing the odds of PG by 3.9-fold (95%CI=0.78–19.31, p=0.10) while impulsivity had little effect (OR=0.90, 95% CI=0.63–1.30, p=0.57). FSP group assignment was slightly associated with PG (OR=2.56, 95% CI=0.90–7.30, p=0.08). Figure 1 displays the relationship between depressive symptoms and impulsivity among the three gambling groups. The divisive interaction between depressive symptoms and impulsivity among PG is particularly apparent as its slope is the steepest and most negative, indicating that the higher the PG’s score in one variable, the lower his score in the other.
TABLE 2.
Adjusted Odds Ratios of the Interaction Effects of Early Adolescence Depressive Symptoms and Impulsivity on Late Adolescence Gambling Behaviors among Males
| PG vs. NG* | PG vs. SG+ | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Depressive Symptoms | 4.06 | 0.73,22.47 | 0.11 | 3.88 | 0.78,19.31 | 0.10 |
| Impulsivity | 0.54 | 0.59,1.31 | 0.54 | 0.90 | 0.63,1.30 | 0.57 |
| African-American | 1.23 | 0.37,4.06 | 0.74 | 0.42 | 0.11,1.52 | 0.19 |
| Group Assignment | ||||||
| Control | 1.00 | 1.00 | ||||
| CC | 1.77 | 0.59,5.35 | 0.31 | 1.04 | 0.34,3.17 | 0.95 |
| FSP | 2.59 | 1.15,5.87 | 0.02 | 2.56 | 0.90,7.30 | 0.08 |
| Lunch | ||||||
| Free/reduced | 1.00 | 1.00 | ||||
| Paid | 0.83 | 0.34,2.05 | 0.69 | 0.60 | 00.26,1.39 | 0.24 |
Note. NG=Nongambler; SG=Social gambler; PG=Problem gambler (includes at-risk and problem gamblers); CC=Classroom-centered intervention; FSP=Family-school partnership intervention.
NG=reference group
SG=reference group
FIGURE 1. Depressive Symptoms and Impulsivity Scores of NG vs. SG vs. PG.
Note. NG=Nongambler; SG=Social gambler; PG= problem gambler (includes at-risk gamblers)
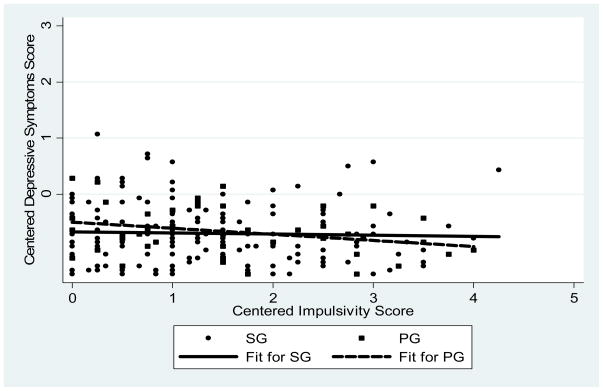
Depressive symptoms and impulsivity scores were further centered to emphasize their divisive interaction on PG [23]. Depressive symptoms scores were centered at the 90th percentile and impulsivity scores at the 10th percentile, and an interaction term for the two centered covariates was created. A model comparing PG to NG, adjusted for demographics, showed that while an increase in depressive symptoms among those at the 10th percentile of impulsivity yielded little change in the odds of PG (OR=2.35, 95% CI=0.66–8.39, p=0.19), an increase in impulsivity among those at the 90th percentile of depressive symptoms decreased the odds of PG (OR=0.40, 95% CI=0.17–0.99, p=0.05). A similar model comparing PG to SG showed that while an increase in depressive symptoms among those at the 10th percentile of impulsivity had little effect on PG (OR=1.95, 95% CI=0.69–5.49, p=0.21), an increase in impulsivity for those at the 90th percentile of depressive symptoms decreased the odds of PG (OR=0.34, 95% CI=0.11–0.99, p=0.05). Figure 2 displays the divisive interaction between the two centered scores on PG compared to SG.
FIGURE 2. Depressive symptoms centered on 90th percentile and Impulsivity centered on 10th percentile of SG vs. PG.
Note. SG=Social gambler; PG= problem gambler (includes at-risk gamblers)
Logistic models with centered depressive symptoms scores at the 10th percentile and impulsivity scores at the 90th percentile, their interaction term, and adjusted for demographics, were used next. Compared to NG, an increase in depressive symptoms among those at the 90th percentile of impulsivity, decreased the odds of PG (OR=0.50, 95% CI=0.15–1.01, p=0.05) while impulsivity appeared to have little effect among those at the 10th percentile of depressive symptoms (OR=0.82, 95% CI=0.54–1.22, p=0.33). A similarly adjusted model comparing PG to SG showed that an increase in depressive symptoms among those at the 90th percentile of impulsivity decreased the odds of PG (OR=0.28, 95% CI=0.07–1.06, p=0.06) while an increase in impulsivity among those at the 10th percentile of depressive symptoms had little effect on PG (OR=0.82, 95% CI=0.55–1.21, p=0.31).
Discussion
While there appeared to be a slight association between early adolescence depressive symptoms and late adolescence problem gambling among boys, it only appeared after adjusting for impulsivity, the interaction between depressive symptoms and impulsivity, race, intervention group assignment, and lunch status. Additionally, the combined effects of both depressive symptoms and impulsivity appeared to have a divisive effect on problem gambling, instead of the hypothesized synergistic effect.
Unlike impulsivity, which has been shown to decrease over time, childhood depressive symptoms have been shown to have lasting effects [26,27]. The recurrence of episodes was common among youths with major depression, with 18%–26% report a new episode within 1 year of recovery, 40%–45% within 2 years, and 75% within 5 years [28]. Childhood depressive symptoms are also strongly associated with poor adaptive functioning and various personality disorders in young adulthood [26]. Therefore, our finding that early adolescence depressive symptoms, both individually and upon interaction with impulsivity, had a borderline significant association with late adolescence problem gambling seems consistent with previous studies that have shown the enduring consequences of depressive symptoms.
While the divisive effect of the presence of both seemed surprising, it was found that most literature regarding individuals with comorbid depression and high impulsivity/impulse-related personality disorders focused on suicidality [29]. For example, a study sampling inpatients with major depression found that those admitted for suicide attempts scored significantly higher in impulsivity than their non-attempt counterparts [29]. Such studies could imply that individuals with comorbid depression and high impulsivity direct their disinhibitions inward in the form of self-destructive ideations, which could explain the divisive effect of the interaction of depressive symptoms and impulsivity on problem gambling as gambling tends to be a more outward form of escapism.
On the other hand, because one of the appeals of gambling is its alleviation of current stress, engaging in this behavior could be problematic for youths who have not yet developed healthy, adaptive coping skills. When gambling no longer fulfills their need to escape from their painful realities and instead adds to their stress through problems such as debt, many problem gamblers turn to suicide [30]. Within a sample of 500 problem gamblers, 48% reported suicide ideation and 13% reported suicide attempts [30]. Furthermore, major depressive disorder is positively associated with suicide [31]. Therefore the high prevalence of suicidality among problem gamblers further demonstrates the long-term adverse outcomes of those with major depressive disorder in that not only can early adolescence depressive symptoms place one at risk for late adolescence problem gambling, symptoms exhibited by problem gamblers can also place them at risk for suicide.
While the current findings may not be generalizable beyond inner-city African-American male adolescents, their clinical implications are significant. Urban African-American male youths’ high rates of incarceration, unemployment, death, and high school drop-out have been attributed to environmental factors such as poverty, lack of neighborhood social organization, and deviant peer associations [32,33]. Such factors have also been associated with depression [34]. The present study found evidence to suggest that depressive symptoms exhibited as early as middle school to be associated with late adolescence problem gambling. Furthermore, those who received the one-year FSP intervention during 1st grade had increased odds of problem gambling in late adolescence. An evaluation of the intervention shows that FSP decreased problem behaviors, such as fighting and breaking rules, among boys a year after its implementation [35]. The success could indicate strong parent-child relationships where parents were attending to the well-being of their children. However urban families experience high rates of marital disruptions, and single-parent households tend to have lower parental-monitoring [36]. The attenuation in parental attention following marital disruption could cause children to feel rejected, and parental rejection has been positively associated with depression [37]. Therefore, early adolescence could be a point of entry for interventions in that youths observed to be depressed by teachers or counselors, receive referrals to cognitive behavioral therapy where they can learn adaptive coping strategies to deal with their environmental and familial stressors. Such therapy could lower their depressive symptom, odds of gambling initiation, and other adverse outcomes such as suicide as previously discussed.
There are several limitations to the study. While the original cohort was prospectively followed-up annually, the method with which the depressive symptoms and impulsivity data were collected was cross-sectional. As a result, it was difficult to discern which preceded the other. Furthermore, because the gambling data was not collected until the subjects were around age 17 in 2004, age of gambling initiation was unknown for those who responded as having ever gambled in that first wave. Therefore, while the current study shed light on the association between early adolescence depressive symptoms and impulsivity and late adolescence problem gambling, the true temporal sequencing of depressive symptoms, impulsivity, and problem gambling was not established. Such temporality would be vital toward effective intervention methods aiming to prevent and treat problem gambling in that different approaches would be necessary if problem gambling were a precursor for depressive symptoms and impulsivity, a mediator between depressive symptoms and impulsivity, or an outcome of depressive symptoms and impulsivity.
Due to the low prevalence of problem gambling, at-risk and problem gamblers were combined into one group for the present study. While the two groups were found to be similar in terms of their levels of sensation seeking, anxiety, self-discipline, self-esteem, and maladaptive coping skills, not all at-risk gamblers progress into problem gamblers [1,23]. As a result, the current findings could be biased due to some unmeasured difference between the two groups. Future studies could aim to uncover the protective factors that may differentiate at-risk gamblers from problem gamblers.
The female sample’s lack of statistical power limited the findings to only males. The small number of female problem gamblers could be due to the time point at which data was collected. Studies found females to initiate gambling later than males [38], a phenomenon reflected in our study with the higher number of female nongamblers and the lower numbers of female social and problem gamblers at late adolescence. Because it is during adulthood that most females initiate gambling, the timeframe of the current study’s data may not adequately depict the issue of problem gambling among females.
Major strengths of the study include the sample, selected from an epidemiologically defined population representative of African-American students in schools in urban neighborhoods, and the 92% response rate. Therefore even though the sample size of the primary outcome of late adolescence problem gambling was small, its associations with early adolescence depressive symptoms and impulsivity, though somewhat imprecise, should be representative of the sample.
Conclusion
Early adolescence depressive symptoms appear to be more positively associated to late adolescence problem gambling than early adolescence impulsivity, and there seems to be a divisive interaction between depressive symptoms and impulsivity on problem gambling. In recent years, the prevalence of problem gambling among adolescents has exceeded that of adults [1–2]. Adolescent problem gamblers are not only more likely to become adult problem gamblers but are also at risk of substance abuse and other psychiatric disorders [6]. More research is necessary in this area to uncover further risk and protective factors so that effective intervention methods could be proposed.
Acknowledgments
This study was funded by a research grant from the National Institute of Child and Human Development, National Institutes of Health (NICHD-NIH, RO1HD060072- P.I. Dr. Martins). The JHU PIRC Second Generation Intervention Trial is funded by National Institute on Drug Abuse grant RO1 DA11796 (P.I. Dr. Ialongo). We thank Scott Hubbard for data management.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Derevensky J, Gupta R. Adolescent gambling: Current knowledge, myths, assessment strategies and public policy implications. In: Smith G, Hodgins D, Williams R, editors. Research and measurement issues in gambling studies. New York: Academic Press; 2007. pp. 437–63. [Google Scholar]
- 2.National Research Council. Pathological gambling: A critical review. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 3.Hardoon KK, Derevensky JL. Child and adolescent gambling behavior: Current knowledge. Clin Child Psychol Psychiatry. 2002;7:263–81. [Google Scholar]
- 4.Choudhury S, Blakemore SJ, Charman T. Social cognitive development during adolescence. Soc Cogn Affect Neurosci. 2006 Dec;1(3):165–74. doi: 10.1093/scan/nsl024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerrard M, Gibbons FX, Benthin AC, et al. A longitudinal study of the reciprocal nature of risk behaviors and cognitions in adolescents: What you do shapes what you think, and vice versa. Health Psychol. 1996;15(5):344–54. doi: 10.1037//0278-6133.15.5.344. [DOI] [PubMed] [Google Scholar]
- 6.Messerlian C, Gillespie M, Derevensky JL. Beyond drugs and alcohol: Including gambling in a high-risk behavioural framework. Paediatr Child Health. 2007 Mar;12(3):199–204. doi: 10.1093/pch/12.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta R, Derevensky JL. Adolescent gambling behavior: A prevalence study and examination of the correlates associated with problem gambling. J Gambl Stud. 1998 Winter;14(4):319–45. doi: 10.1023/a:1023068925328. [DOI] [PubMed] [Google Scholar]
- 8.Beaudoin CM, Cox BJ. Characteristics of problem gambling in a Canadian context: A preliminary study using a DSM-IV-based questionnaire. Can J Psychiatry. 1999 Jun;44(5):483–7. doi: 10.1177/070674379904400509. [DOI] [PubMed] [Google Scholar]
- 9.Stewart SH, Zack M, Collins P, et al. Subtyping pathological gamblers on the basis of affective motivations for gambling: Relations to gambling problems, drinking problems, and affective motivations for drinking. Psychol Addict Behav. 2008 Jun;22(2):257–68. doi: 10.1037/0893-164X.22.2.257. [DOI] [PubMed] [Google Scholar]
- 10.Moeller FG, Barratt ES, Dougherty DM, et al. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001 Nov;158(11):1783–93. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- 11.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: A critical period of addiction vulnerability. Am J Psychiatry. 2003 Jun;160(6):1041–52. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vitaro F, Ladouceur R, Bujold A. Prediction and concurrent correlates of gambling in early adolescent boys. J Early Adolesence. 1996;16(2):211–28. [Google Scholar]
- 13.Turner N, Jain U, Spence W, et al. Pathways to pathological gambling: Component analysis of variables related to pathological gambling. International Gambling Studies. 2008;8(3):281–98. [Google Scholar]
- 14.Colder CR, Chassin L. Affectivity and impulsivity: temperament risk for adolescent alcohol involvement. Psychol Addict Behav. 1997 Jun;11(2):83–97. [Google Scholar]
- 15.Hynan D, Grush J. Effects of impulsivity, depression, provocation, and time on aggressive behavior. J Res Pers. 1986 Jun;20(2):158–171. [Google Scholar]
- 16.Ialongo NS, Kellam SG, Poduska J. Manual for the Baltimore How I Feel. Baltimore, MD: Johns Hopkins University; 1999. [Google Scholar]
- 17.Dolan L, Kellam S, Brown C, et al. The short-term impact of two classroom-based preventive interventions on aggressive and shy behaviors and poor achievement. J Appl Dev Psychol. 1993 Sep;14(3):317–345. [Google Scholar]
- 18.Winters KC, Stinchfield RD, Fulkerson J. Toward the development of an adolescent gambling problem severity scale. J Gamb Stud. 1993;9:63–84. [Google Scholar]
- 19.Winters KC, Stinchfield RD, Kim L. Monitoring adolescent gambling in Minnesota. J Gamb Stud. 1995;11:165–83. doi: 10.1007/BF02107113. [DOI] [PubMed] [Google Scholar]
- 20.Werthamer-Larsson L, Kellam S, Wheeler L. Effect of first-grade classroom environment on shy behavior, aggressive behavior, and concentration problems. Am J Community Psychol. 1991 Aug;19(4):585–602. doi: 10.1007/BF00937993. [DOI] [PubMed] [Google Scholar]
- 21.Ialongo N, Poduska J, Werthamer L, et al. The distal impact of two first grade preventive interventions on conduct problems and disorder and mental health service need and utilization in early adolescence. J Em Behav Disorders. 2001;9:146–60. [Google Scholar]
- 22.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV):620 Description, differences from previous versions, and reliability of some common diagnoses. J AmAcadChild Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 23.William R. Interpreting interaction effects; Interaction effects and centering. Retrieved May 25, 2010 from http://www.nd.edu/~rwilliam/stats2/l53.pdf.
- 24.Jo B, Asparouhov T, Muthen BO, Ialongo NS, et al. Cluster randomized trials with treatment noncompliance. Psychol Methods. 2008 Mar;13(1):1–18. doi: 10.1037/1082-989X.13.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.StataCorp. Stata statistical software: Release 11.0. 2009. [Google Scholar]
- 26.Aronen ET, Soininen M. Childhood depressive symptoms predict psychiatric problems in young adults. Can J Psychiatry. 2000 Jun;45(5):465–70. doi: 10.1177/070674370004500507. [DOI] [PubMed] [Google Scholar]
- 27.Kasen S, Cohen P, Skodol AE, Johnson JG, Smailes E, Brook JS. Childhood depression and adult personality disorder: Alternative pathways of continuity. Arch Gen Psychiatry. 2001 Mar;58(3):231–6. doi: 10.1001/archpsyc.58.3.231. [DOI] [PubMed] [Google Scholar]
- 28.Strober M, Lampert C, Schmidt S, Morrell W. The course of major depressive disorder in adolescents: I. recovery and risk of manic switching in a follow-up of psychotic and nonpsychotic subtypes. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):34–42. doi: 10.1097/00004583-199301000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Corruble E, Damy C, Guelfi JD. Impulsivity. A relevant dimension in depression regarding suicide attempts? J Affect Disord. 1999 Jun;53(3):211–5. doi: 10.1016/s0165-0327(98)00130-x. [DOI] [PubMed] [Google Scholar]
- 30.Frank ML, Lester D, Wexler A. Suicidal behavior among members of Gamblers Anonymous. J Gambl Stud. 1991 Sep;7(3):249–254. doi: 10.1007/BF01019876. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998 Dec;7(1):3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 32.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Dev. 1994 Apr;65(2):296–318. [PubMed] [Google Scholar]
- 33.Elliott DS, Wilson WJ, Huizinga D, et al. The effects of neighborhood disadvantage on adolescent development. J Res Crime & Del. 1996 Nov;33:389–426. [Google Scholar]
- 34.Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003 Mar;44(1):34–44. [PubMed] [Google Scholar]
- 35.Ialongo NS, Werthamer L, Kellam SG, et al. Proximal impact of two first-grade preventive interventions on the early risk behaviors for later substance abuse, depression, and antisocial behavior. Am J Community Psychol. 1999;27:599–641. doi: 10.1023/A:1022137920532. [DOI] [PubMed] [Google Scholar]
- 36.Shihadeh ES, Steffensmeier DJ. Economic inequality, family disruption, and urban black violence: cities as units of stratification and social control. Social Forces. 1994;73:683–97. [Google Scholar]
- 37.Armsden GC, McCauley E, Greenberg MT, et al. Parent and peer attachment in early adolescent depression. J Abnorm Child Psychol. 1990;18:683–97. doi: 10.1007/BF01342754. [DOI] [PubMed] [Google Scholar]
- 38.Blanco C, Hasin DS, Petry N, et al. Sex differences in subclinical and DSM-IV pathological gambling: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006 Jul;36(7):943–53. doi: 10.1017/S0033291706007410. [DOI] [PubMed] [Google Scholar]