Abstract
Objective:
Intensive case management (ICM) is effective for facilitating entry into and retention in outpatient substance use disorder treatment (OSUDT) for low-income substance-dependent women; however, no studies have specifically examined the moderating impact of depressive symptoms on ICM. The purpose of this study was to investigate whether depressive symptoms moderated ICM's effect on OSUDT engagement, attendance, and outcomes for substance-dependent women on Temporary Assistance for Needy Families (TANF). It was hypothesized that highly depressed women would demonstrate worse outcomes on all indicators.
Method:
Logistic regression and generalized estimating equations were used to determine depression's moderating impact on ICM in a secondary analysis of data from a randomized controlled trial comparing the effectiveness of ICM to usual care provided by local public assistance offices in Essex County, NJ. Substance-dependent women (N = 294) were recruited while being screened for TANF eligibility and were followed for 24 months.
Results:
Findings revealed that high levels of depressive symptoms moderated the effectiveness of ICM in unexpected directions for two outcome variables. Subjects with high levels of depressive symptoms in ICM were (a) significantly more likely to engage in at least one treatment program than those in usual care and (b) associated with the fewest mean drinks per drinking day across the 24-month follow-up period. Independent effects for high levels of depressive symptoms and ICM were also found to positively influence engagement, attendance, and percentage days abstinent.
Conclusions:
ICM is effective for substance-dependent women with a broad spectrum of depressive symptoms in enhancing OSUDT utilization and outcomes.
Substance use disorders (SUDs) among low-income mothers remain a major public health concern, particularly given the potential negative impact on future generations (Kost and Smyth, 2002; McGue, 1994). Substance dependence among women is known to be related to poverty, inadequate or unstable housing, and physical abuse (Marcenko et al., 2000), unemployment, and increased medical problems (Shillington et al., 2001). Although research shows that longer stays in treatment predict significantly longer periods until first use of alcohol or other drugs after treatment as well as overall reduced drug and alcohol use for all individuals with SUDs (Acharyya and Zhang, 2003; Green et al., 2004), rates of SUD treatment retention remain lowest for low-income women (Greenfield et al., 1998, 2007; Rosen et al., 2003). Therefore, enhancing treatment engagement and retention for low-income mothers with SUDs remains an important goal for public health.
Among low-income mothers with SUDs, substance-dependent women receiving Temporary Assistance for Needy Families (TANF) are of particular concern. Some estimates indicate that substance dependence is more than twice as likely for TANF recipients than for the general public or nonrecipients with similar sociodemographics (Pollack et al., 2002; Rosen et al., 2003). Barriers to SUD treatment, such as lack of childcare and transportation, persist for women on TANF despite their ability to pay for treatment (Brady and Ashley, 2005; Greenfield et al., 2007; Rosen et al., 2004). In part as a result of these barriers, women with SUDs are more likely to be administratively sanctioned, causing “unstable exits” from welfare (Schmidt et al., 2002, p. 221). These exits increase the likelihood of returning to welfare as a result of factors such as greater economic hardship after sanctioning and continued unemployability (Metsch and Pollack, 2005; Schmidt et al., 2002).
The Personal Responsibility and Work Opportunity Reconciliation Act of 1996 awarded states new privileges that provided unique opportunities for intervention to help women on TANF engage in treatment and eventually exit welfare via employment (Besharov and Germanis, 2004). One such intervention is case management (CM). Various types of CM are used with individuals with SUDs across public and private sectors to increase SUD treatment utilizaion and rates of abstinence (Hesse et al., 2007). Across its different forms and protocols, empirical evaluations of CM demonstrate effectiveness among women on welfare with SUDs in facilitating greater rates of treatment entry and retention, as well as greater rates of abstinence from alcohol and drugs (Brindis and Theidon, 1997; Morgenstern et al., 2006, 2009a; Volpicelli et al., 2000).
In an earlier study, we investigated whether a particular type of CM, intensive CM (ICM), improved SUD treatment utilization and outcomes for substance-dependent women on TANF (Morgenstern et al., 2006). The Substance Abuse Research Demonstration (SARD) study was a field tested, randomized controlled trial implemented in Essex County, NJ (Morgenstern et al., 2003). It examined the effectiveness of ICM in improving SUD treatment engagement, retention, and outcomes for substance-dependent women on TANF who were not currently enrolled in nor actively seeking SUD treatment. ICM was compared with the “screen-and-refer” system (referred to as usual care [UC]) existing in welfare offices at the time. Consistent with previous studies across various types of CM (Brindis and Theidon, 1997; Hesse et al., 2007; Morgenstern et al., 2009a), women assigned to ICM demonstrated greater rates of treatment engagement and attendance, greater rates of abstinence from alcohol and drugs across 24 months, and greater rates of employment than those in UC (Morgenstern et al., 2006, 2009b).
Despite this proven effectiveness, it remains unknown to what extent the presence of co-occurring disorders or their symptomatology may hinder ICM's therapeutic impact on SUD treatment utilization and outcomes. SUDs among women on TANF are directly associated with significantly higher rates of comorbid mental health disorders than in the general population (Rosen et al., 2004), the most common of which are major depressive disorder and dysthymia (Watkins et al., 2004). Depressive symptoms were also of concern among the SARD substance-dependent sample. Consistent with national prevalence rates among mothers on welfare (Lennon et al., 2002), almost half (45%) of the SARD substance-dependent sample reported moderate to severe depressive symptoms at baseline, compared with only 5% of the SARD nondependent comparison sample (Morgenstern et al., 2003). Although simultaneous or integrated mental health and SUD services are recommended as optimal treatment for individuals with co-occurring disorders (Institute of Medicine, 2006; Mueser et al., 2003), the primary goal of the SARD ICM intervention was solely to enhance SUD treatment utilization and subsequent employment. Given this focus, depressive symptoms may have been untreated, potentially complicating the implementation of ICM and affecting participation in SUD treatment. Understanding how depressive symptoms affect SUD treatment utilization and outcomes is crucial to informing policymakers, administrators, and practitioners about which substance-dependent women are best helped by ICM and under what circumstances.
This study aimed to understand how depressive symptoms affect the ability of ICM to facilitate outpatient SUD treatment (OSUDT) utilization and reduce problematic substance use among substance-dependent women receiving TANF. Because this particular ICM intervention was not designed to address the complexities or symptomatology of co-occurring disorders, it was hypothesized that depressive symptoms would moderate ICM such that women with high levels of depressive symptoms (HDS) would fare worse than women with low levels of depressive symptoms (LDS) on three primary outcomes. Specifically, a secondary analysis was performed using data from the SARD study to explore how depressive symptoms moderated ICM's effect on (a) engagement into at least one OSUDT program, (b) OSUDT attendance, and (c) substance use.
Method
The complete SARD study methods are reported elsewhere (Morgenstern et al., 2003, 2006) and are briefly reviewed here.
Study participants
Screening.
Individuals were approached in welfare offices in Essex County, NJ, while applying for or seeking recerti-fication of TANF benefits. Potential subjects were assessed by welfare workers to screen for problematic substance use, using the CAGE-AID (i.e., the CAGE questionnaire altered to include drugs; Brown and Rounds, 1995), as a part of routine procedures determining TANF eligibility. If a participant screened positively, she was referred for evaluation with an addiction counselor in a location that protected confidentiality.
Eligibility criteria.
Formal selection criteria for participants included being (a) TANF eligible, (b) eligible for New Jersey's welfare-to-work program, and (c) able to speak English well enough to complete an interview (Morgenstern et al., 2001). Eligible individuals also met criteria for a substance-dependence diagnosis (according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV]; American Psychiatric Association, 1994), as measured by the Structured Clinical Interview for DSM-IV (First et al., 1996). Women were excluded if they were (a) actively psychotic or receiving treatment for a psychotic disorder, (b) receiving or seeking methadone treatment, (c) seeking long-term residential treatment, (d) currently engaged in SUD treatment, or (e) medically deferred from work requirements.
Sample description.
Three hundred two substance-dependent women participated in the SARD study.Because depressive symptoms were a primary variable of interest, only those women who completed a baseline Beck Depression Inventory, Second Edition (BDI-II; Beck et al., 1996), were included in this analysis, yielding a final sample size of 294. Participants were between 18 and 54 years of age; 95.7% were non-Hispanic Black, 3.3% were Hispanic, and 1% were White. This was a representative sample of Essex County welfare recipients who satisfied eligibility criteria (Morgenstern et al., 2001). The typical substance-dependent participant was about 36 years old, had not graduated high school, and had two to three children (Morgenstern et al., 2006). Her mean annual income was $10,000, and she had been on welfare an average of 12 years. Of the 294 women, 156 were assigned to ICM and 138 were assigned to UC.
Study interventions
Once they met eligibility requirements, consented, and agreed to participate, women were randomly assigned to one of two conditions: ICM or UC. Clinical staff for both conditions consisted of addiction counselors with master's degrees in social work or psychology.
Intensive case management.
ICM was a manual-guided intervention (Morgenstern et al., 1999). Although it is called ICM, this experimental intervention was a combination of intensive, strengths-based, and clinical CM (as defined in Mueser et al., 1998). The staff-to-client ratio was 1 to 20. During the initial phase of ICM, case managers identified barriers to treatment entry, including childcare, transportation, and housing problems, and provided needed services. There was intensive outreach to clients in the community and 24-hour coverage. In addition, case managers implemented direct clinical services, including motivational interviewing and ongoing supportive counseling, although they were not considered mental health providers. Case managers were also highly involved in each client's SUD treatment and assisted treatment facility staff with coordinating services. Client contacts were frequent, and case managers met with clients weekly. Clients also received vouchers to purchase items (e.g., children's toys) as incentives for attending SUD treatment. Over the course of the 24-month follow-up period, case manager contact with clients increased or decreased on the basis of need and phase of treatment.
Usual care.
Women randomized to UC met with a clinical care coordinator who reviewed their need for SUD treatment and referred them to the appropriate level of care. This screen-and-refer model was the standard of care in New Jersey at the time of data collection (Morgenstern et al., 2008). If clients failed to attend a first session of treatment, outreach was limited to several phone calls and letters. Clients had the option of returning to be reassessed and assigned to treatment if the initial treatment failed or at any time during the 24 months of study participation (Morgenstern et al., 2006).
Case management fidelity and discriminability.
Both the intensive case managers and UC condition coordinators kept daily activity logs for each participant, including noting the type of and time spent performing each task. Using a formal review process, supervisors and researchers independently rated completion of ICM tasks through close clinical supervision and chart review, respectively. In a previous report, the investigators found significant differences in the number of contacts, services, and hours spent with clients for each of the interventions (Morgenstern et al., 2006). Notably, ICM provided more intensive services for clients than UC.
Procedures
Master's-level clinicians conducted baseline assessments and master's- and bachelor's-level research staff conducted all other interviews (Morgenstern et al., 2003). All clinicians/ interviewers had extensive experience assessing clients with SUDs. All received intensive training in administering measures and close supervision by a doctoral-level psychologist. Participants were randomly assigned to ICM or UC after completion of the baseline assessment to ensure assessing clinicians were blind to condition. Participants were recruited between 1999 and 2002 and then followed for 24 months (Morgenstern et al., 2008). At 3, 9, 15, and 24 months after baseline, participants received in-person or telephone follow-up, which were structured interviews with a research staff member. Follow-up retention rates were high at all time points, ranging from 85% to 95% (Morgenstern et al., 2006, 2009b).
Measures
Baseline characteristics.
The Addiction Severity Index-Expanded Female Version (ASI-F; Center for Substance Abuse Treatment, 1997) is the gold standard for structured interviews for evaluating individuals with SUDs in both research and clinical settings and demonstrates high reliability and validity across numerous studies (Makela, 2004). Drug and alcohol composite scores were used as a means to establish baseline substance use severity. The ASI-F was also used to collect participant demographic information at baseline, including age, education, and recent employment history, as well as receipt of mental health services in the first 3 months of the study.
Depression.
Depressive symptoms were measured using the BDI-II. The BDI-II is a self-report, 21-item questionnaire that yields a continuous score, ranging from 0 to 63, indicating level of experienced distress (Beck et al., 1996). Scores from 0 to 19 indicate no to mild depressive symptoms; 20 and above indicates moderate to severe depressive symptoms. The reliability and validity of the BDI-II with populations with SUDs has been well established (e.g., Dum et al., 2008; Greenfield et al., 1998). For this sample, the BDI-II demonstrated a high degree of reliability (i.e., Cronbach's coefficient α = .908). BDI-II scores were normally distributed (range: 0-61, M= 20, SD = 11.5, Mdn = 19).
Previous studies demonstrate that scores of 20 and above on the BDI-II are sensitive and specific in indicating the presence of major depressive disorder (Beck et al., 1996), and 20 is a widely used threshold to indicate the presence of clinically significant depressive symptoms (Greenfield et al., 1998). For ease of interpretation in the present analyses, scores were dichotomized by this clinically relevant split: (a) LDS (scores ranging from 0 to 19) and (b) HDS (scores ≥ 20). Approximately 52% of 294 substance-dependent women reported HDS. Women with HDS were evenly distributed across condition: 46.5% in ICM and 50.4% in UC. Differences in the rates of depression between the two conditions were not statistically significant (p > .50).
Outpatient substance use disorder treatment utilization.
OSUDT, defined here as a hospital- or community-based program specializing in treatment of SUDs (excluding methadone maintenance), has demonstrated more effectiveness with women in reducing substance use than other types of formal treatment (Hser et al., 2003). It also tends to be the treatment of choice for both substance using mothers on welfare (as a result of the continued ability to care for their children in the community; Corcoran, 2001) and individuals with co-occurring drug dependence and major depressive disorder (Grant, 1997). For these reasons, this study focuses only on OSUDT utilization.
Administrative data were collected from OSUDT programs to obtain accurate records of engagement and attendance. OSUDT programs completed a weekly attendance log for each participant in both UC and ICM. For those clients for whom such data could not be collected, subjects answered detailed questions about their involvement in OSUDT at each assessment that was then corroborated by case managers. Client self-reported utilization accounted for less than 5% of the data. To eliminate potential biases, analyses were conducted both with and without client self-report data. Equivalent results were found.
Engagement.
The National Commission for Quality Assurance's Health Plan Employer Data and Information Set's definition of treatment engagement was used for this study, as suggested by clinical and research experts in the field of substance misuse for use across studies (Washington Circle, 2004). Consistent with these standards, engagement was defined as admission to an OSUDT program with three additional visits within 30 days. A dichotomous, dependent variable was created to indicate that a participant engaged in at least one program if the above criteria were satisfied for any of the programs to which a participant was assigned.
Attendance.
Based on the same administrative data, SUD treatment attendance was measured by counting the number of days a participant attended OSUDT. The frequency of days attended was summed in quarterly periods across the 24 months for a total of eight time points. This was the primary dependent variable for treatment attendance.
Substance use outcomes.
The Timeline Followback (TLFB; Sobell et al., 1980) was used to collect data on alcohol and other drug use during the 24-month study period. The TLFB is an interviewer-assisted, calendar-based method that uses specific techniques (e.g., memory cues) for participants to recall daily drinking (in standard drink equivalents) and types and frequency of other drug use. The TLFB has demonstrated reliability and validity for recall periods of up to 1 year (Fals-Stewart et al., 2000), with high temporal stability and reliability when used with psychiatric outpatients (Carey et al., 2004). For the present study, alcohol and drug use data were collected for each day from the date of baseline to obtain a continuous record of use across 24 months (Morgenstern et al., 2006). At each assessment, daily data were collected from the date of the previous assessment. Self-reported substance use was confirmed via collateral interviews and urine drug screens, with 87.2% to 95.5% agreement (Morgenstern et al., 2006). Participants reported greater or equivalent use in comparison to corroborative measures.
To investigate both the intensity and frequency of substance use, two variables were created from the TLFB data to provide dependent variables for substance use outcomes: percentage days abstinent (PDA) and mean drinks per drinking day (DDD). Both of these summary variables were calculated for each participant for each month across the 24-month follow-up period for a total of 24 time points each. Intensity of drug use was not collected.
Readiness to change.
Readiness to change was measured at baseline using the University of Rhode Island Change Assessment (URICA; McConnaughy et al., 1983). A single composite score was constructed by summing scores on three subscales—contemplation, action, and maintenance— and then subtracting the precontemplation subscale score from the total (DiClemente et al., 2001). A higher score indicates greater readiness to change. The URICA demonstrates good reliability and validity across studies and study populations (Field et al., 2009).
Analytic plan
Two statistical methods were used to test the impact of depressive symptoms on the effectiveness of ICM on OSUDT utilization and outcomes. First, logistic regression was used to examine the likelihood that a participant engaged in at least one OSUDT program. Second, generalized estimating equations (GEE; Liang and Zeger, 1986) were used to analyze the nonnormal, longitudinal data for the three dependent variables: days attended OSUDT, PDA, and mean DDD. GEE is a data analytic technique appropriate for a longitudinal panel design because it is a powerful test that corrects for correlated observations (Stokes et al., 2000). Although GEE is also useful in adjusting for random missing data, only 1.7% of the data were missing.
The first step in building each of the four models was to explore for baseline group differences. Four groups were created across condition and HDS/LDS. Demographic characteristics (i.e., age, race, education, income, number of children, and employment) were compared across groups using chi square tests, t tests, and one-way analyses of variance, where appropriate. In addition, rates of baseline substance use frequency and severity were examined.
The next step in model building was to enter demographic and baseline substance use variables into each model to examine their relationships to the dependent variables before examining main effects. Those attributes found to be marginally significant contributors (p < .10) were kept (age, drug and alcohol use severity, and recent employment) and entered into each of the four models as covariates. After examining the relationships between each covariate and dependent variable, main effects for depression and condition were entered into the model. For all the GEE models, time and a Time × Condition interaction term were added to test for effects over time. Lastly, a Depression × Condition interaction term was added to each of the models to test for a moderating effect of depression on ICM.
Within each of the GEE analyses, for each dependent variable (i.e., treatment attendance days, PDA, and mean DDD), a negative binomial distribution with log link function was specified, which provided good model fit. In addition, an exchangeable working correlation matrix was specified (Stokes et al., 2000). All analyses were conducted using the SAS statistical software program (SAS Institute Inc. Cary, NC). To further explore the findings of the primary analyses, post hoc analyses were performed.
Because depressive symptoms were the primary focus, two methodological decisions should be noted. First, the potential influence of a participant's involvement in mental health treatment on OSUDT utilization and substance use outcomes was considered. When mental health treatment utilization was examined, however, only 3% and 6% of the entire substance-dependent sample attended any inpatient or outpatient mental health treatment, respectively, during the first 3 months of the study when CM services were most intensive. Mental health treatment utilization was therefore excluded from the analyses.
Second, recognizing that the use of a continuous rather than dichotomous variable for depressive symptoms increases the power of analyses, all analyses were initially performed with a continuous form of the BDI-II score. These initial analyses yielded equivalent findings to the dichotomous variable. The dichotomous variable was chosen to facilitate ease of presentation and interpretation of the main and interaction effect findings.
Results
Baseline group equivalence
Demographics.
All four groups, defined by depression and condition, demonstrated equivalence on all demographic variables, including age, race, education, income, number of children, number of years on welfare, and recent employment (Table 1).
Table 1.
Baseline characteristics of substance-dependent women on TANF by depressive symptoms and condition, Essex County, NJ
| Low depressive symptoms |
High depressive symptoms |
||||
| Variable | ICM (n = 84) M (SD) or % | UC (n = 69) M (SD) or % | ICM (n = 72) M (SD) or % | UC (n = 69) M (SD) or % | Total (N=294) M (SD) or % |
| Age, in years | 36.8 (5.8) | 35.9 (7.7) | 37.2 (6.9) | 35.0 (6.3) | 36.2 (6.7) |
| Race | |||||
| Black, non-Hispanic | 95.3% | 97.1% | 95.9% | 95.7% | 96.3% |
| Hispanic, any race | 4.7% | 1.4% | 2.7% | 2.9% | 2.7% |
| Other | 1.4% | 0.0% | 1.4% | 1.4% | 1.0% |
| Graduated from high school | 48.2% | 50.7% | 47.3% | 45.7% | 48.0% |
| Annual income: $5,000-$9,000 | 59.0% | 50.7% | 58.3% | 47.8% | 54.3% |
| No. of children younger than 18 years old | 2.5(1.8) | 2.5(1.6) | 2.2(1.3) | 2.7 (2.0) | 2.5(1.7) |
| No. of years on welfare | 13.1 (7.9) | 10.6 (7.0) | 12.5 (8.1) | 11.9(7.9) | 11.8(7.3) |
| Recent part-time or full-time employment | 21.4% | 18.8% | 13.9% | 20.6% | 18.8% |
| Primary substance dependence diagnosis | |||||
| Alcohol | 17.6% | 26.1% | 17.6% | 25.7% | 21.8% |
| Cannabis | 4.7% | 10.1% | 4.1% | 5.7% | 6.3% |
| Cocaine | 41.2% | 29.0% | 37.8% | 31.4% | 35.7% |
| Opiate | 35.3% | 31.9% | 39.2% | 37.1% | 36.0% |
| ASI-F alcohol severity composite score | .21 (.26) | .29 (.31) | .35 (.32) | .36 (.36) | .30 (.32) |
| ASI-F drug severity composite score | .20 (.13) | .20 (.14) | .26 (.14) | .27 (.15) | .23 (.14) |
Notes: TANF = Temporary Assistance for Needy Families; ICM = intensive case management; UC = usual care; ASI-F = Addiction Severity Index—Expanded Female Version.
Substance use.
ASI-F composite scores for drug and alcohol use severity were significantly different across depression groups (Table 1). Both drug use, t(288) = -3.95, p < .001, and alcohol use, t(271.1) = -2.97, p < .01, severity scores were higher for participants with HDS than for those with LDS.
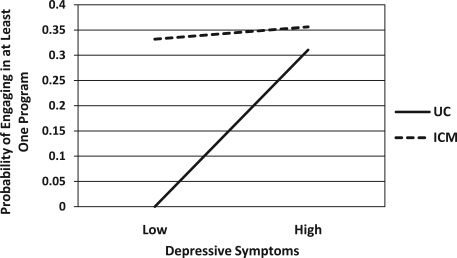
Engagement in OSUDT
Results of the logistic regression yielded two significant covariates: baseline drug use severity (B = 2.187, SE = 1.0373, p < .05) and age (B = 0.0706, SE = 0.0217, p < .01). Results also indicated that being in ICM (B = 0.3317, SE = 0.1438, p < .03) and having HDS (B = 0.3105, SE = 0.1476, p < .04) were independently significant in predicting the likelihood that a participant engaged in at least one program. The interaction term was also significant (B = -0.2858, SE = 0.1443, p < .05), indicating that there was a moderation effect of depression on condition, as demonstrated by Figure 1. ICM performed equally well in the presence of either LDS or HDS, whereas UC did not. A post hoc descriptive examination of the data revealed that women with HDS in ICM demonstrated the highest rate of OSUDT engagement and individuals with LDS assigned to UC demonstrated the lowest rate (Table 2).
Figure 1.
Probability of substance-dependent women on TANF (Temporary Assistance for Needy Families) in Essex County, NJ, engaging in at least one treatment program, by depressive symptoms and condition
Table 2.
Outpatient substance use disorder treatment utilization and outcomes among substance-dependent women on TANF by depressive symptoms and condition, Essex County, NJ
| Low depressive symptoms |
High depressive symptoms |
||||
| Variable | ICM (n = 84) M (SD) or % | UC (n = 69) M (SD) or % | ICM (n = 72) M (SD) or % | UC (n = 69) M (SD) or % | Total (N=294) M (SD) or % |
| Engaged in at least one program | 74.1% | 47.8% | 79.7% | 71.4% . | 71.1% |
| Attended at least 30 days of treatment | 41.7% | 24.6% | 61.1% | 23.2% | 38.1% |
| No. days attended treatment over 24 months | 33.9 (47.3) | 27.7 (56.7) | 61.5(61.3) | 43.8 (58.0) | 37.3(55.1) |
| Drinks per drinking day over 24 months | 6.1 (10.1) | 5.7 (5.5) | 5.1 (5.7) | 5.5 (4.6) | 5.7 (7.0) |
Notes: TANF = Temporary Assistance for Needy Families; ICM = intensive case management; UC = usual care.
Outpatient substance use disorder treatment attendance across 24 months
GEE analyses for OSUDT attendance revealed two significant parameter estimates in addition to time when controlling for baseline drug use severity and recent employment: depression (B = 0.5240, SE = 0.2033, p = .01) and condition (B = 0.5002, SE = 0.2453, p < .05). The Depression x Condition interaction term was not significant (B = 0.6524, SE = 0.5018, p = .19). Although having HDS and receiving ICM independently contributed to higher attendance in OSUDT, there was no moderation effect of depression on condition. The additive nature of the main effects of depression and ICM was observed in a post hoc analysis of attendance. For each group, proportions of whom attended at least 30 days of OSUDT and the mean number of days attended over 24 months were examined (Table 2). Those with HDS in ICM had both the largest proportion who had attended at least 30 days of treatment and the highest mean number of days attended.
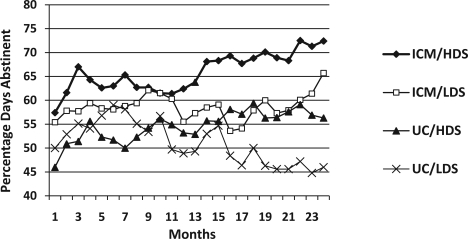
Substance use frequency across 24 months: Percentage days abstinent
Analysis of PDA yielded several significant baseline covariates: baseline drug use severity (B = -0.9026, SE = 0.2375, p < .001), baseline alcohol severity (B = -0.3349, SE = 0.1039, p < .01), age (B = 0.0163, SE = 0.0045, p < .001), and recent employment (B = 0.1705, SE = 0.0719, p < .02). A main effect for depression (B = 0.1839, SE = 0.0659, p < .01) was also revealed. Both condition (B = 0.1282, SE = 0.0662, p = .053) and the Depression × Condition interaction term (B = 0.0854, SE = 0.1335, p = .052) were trending toward significance. Women with HDS and those in ICM were associated with the highest rates of abstinence across 24 months, as seen in Figure 2.
Figure 2.
Percentage days abstinent for substance-dependent women on TANF (Temporary Assistance for Needy Families), by depressive symptoms and condition across 24 months, Essex County, NJ
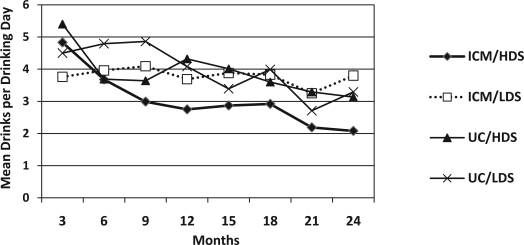
Alcohol use intensity across 24 months: Mean drinks per drinking day
GEE analysis of mean DDD yielded three significant baseline covariates in addition to time: baseline alcohol use severity (B = 1.9572, SE = 0.1772, p < .001), age (B = -0.0280, SE = 0.0095, p < .01), and recent employment (B = -0.4609, SE = 0.1939, p < .02). There were no main effects for depression or condition. The Depression × Condition term (B = -0.6161, SE = 0.2649, p < .03) was significant. Examination of the interaction term revealed, as shown in Figure 3, that women with HDS assigned to ICM had fewer mean DDD across follow-up in comparison with the other three groups, establishing the fewest mean DDD by Month 9 and sustaining that change over 24 months.
Figure 3.
Mean drinks per drinking day for substance-dependent women on TANF (Temporary Assistance for Needy Families), by depressive symptoms and condition across 24 months, Essex County, NJ
Additional post hoc analysis
The above findings revealed that HDS independently led to greater treatment initiation, retention, and more positive outcomes. One possible explanation for this is that women on TANF with HDS had greater readiness to change at treatment entry than those with LDS. Women with co-occurring depression and substance dependence are known to experience greater levels of physical and financial distress than their nondepressed counterparts (Chandler et al., 2004; Poleshuck et al., 2006; Schmidt et al., 2002), which may enhance their motivation to initiate treatment. In an effort to explore this possibility, we correlated readiness to change with the continuous BDI-II score and found a weak, but highly significant, positive relationship (r = .200, p < .001).
Discussion
Because of the absence of a specialized focus on co-occurring disorders, it was hypothesized that ICM would be less effective for substance-dependent women on TANF with HDS than those with LDS in facilitating OSUDT utilization and substance use outcomes. It was expected that depression would moderate ICM such that women with HDS would fare worse on all four dependent variables than those with LDS: OSUDT engagement, OSUDT attendance, PDA, and mean DDD. Our hypotheses were not supported. Moderation effects for depression were found for two dependent variables but in unexpected directions. Women in ICM with HDS demonstrated higher rates of engagement and lower mean DDD than those with LDS as a result of the moderated relationship. For the remaining dependent variables, women with HDS in ICM demonstrated equivalent or higher rates of attendance and PDA compared to their LDS counterparts; however, this was the result of independent effects of ICM and HDS rather than moderation. Findings demonstrated that ICM remains an effective intervention in the context of HDS and, in some cases, performs better than in the context of LDS. Potential explanations for both the moderation effects and the independent effects of depression are explored further below.
Depression's moderation of ICM on engagement was found in conjunction with independent effects of both HDS and ICM. One potential explanation for the increased likelihood of engagement, as the post hoc analysis supported, is that highly depressed women may demonstrate greater readiness to change. Although this does not represent treatment seeking per se, it may indicate a greater willingness to engage in treatment seeking behaviors. Generally, individuals with co-occurring substance dependence and depression are known to initiate treatment more than their nondepressed counterparts (Grant, 1997; Rosen et al., 2004, 2006); however, those reports focused on treatment utilization outside the context of CM. Greater readiness to change coupled with an intervention responsive to mental health vulnerabilities, in this case ICM, may capitalize on this readiness and enhance the likelihood of engagement by addressing practical barriers to treatment initiation. Further research is needed to expand our understanding about readiness to change in the context of depression and other co-occurring disorders.
The presence of a moderation effect for mean DDD was both interesting and puzzling. Contrary to hypotheses, findings were in line with the few studies that have found more positive substance use outcomes for those with depressive disorders (e.g., Charney et al., 1998; Kranzler et al., 1996); however, existing literature provides few explanations for why this might be, particularly in the context of a preponderance of research that demonstrates the opposite (e.g., Hasin et al., 2002, 2004; McKay et al., 2002). In this study, the moderation effect was unique in reducing the intensity of alcohol use rather than frequency. It remains unclear what may be contributing to this relationship, particularly given the lack of moderation for PDA and the absence of a measure of drug use intensity. Previous research on ICM found that greater rates of abstinence were attributable directly to ICM rather than treatment (Morgenstern et al., 2006), and case manager contact was the most robust mediator of ICM (Morgenstern et al., 2008). Thus, it may be that women in ICM with HDS had more cause to have ongoing contact with case managers over the 24 months, subsequently influencing the intensity of alcohol use beyond PDA. Research exploring this dynamic and the differing effects for frequency and intensity is needed.
An explanation for why ICM maintains effectiveness in the context of HDS is that its therapeutic effects may be mimicking therapeutic interventions known to successfully treat depression, such as behavioral activation treatment (Jacobson et al., 2001). Although there were no repeated measures of depressive symptoms to indicate that such symptoms were resolved, ICM may have supported individuals in identifying new behaviors that helped them to function better in spite of mood (i.e., focused activation), such as engaging in OSUDT; addressed environmental triggers for depression, such as reducing social isolation through direct case manager contact or organizing transportation; or addressed fears related to treatment entry (e.g., fear of losing custody of children), which are often cited by substance-dependent women on welfare as reasons they avoid beginning and remaining in treatment (Rosen et al., 2004).
In addition to its moderation effects, the direct impact of depressive symptoms in the context of co-occurring substance dependence on OSUDT attendance and PDA is particularly notable. To the best of our knowledge, this is the first study to report rates of OSUDT utilization and outcomes specifically for non-treatment-seeking, substance-dependent women on TANF with depressive symptoms. Inconsistent findings in the literature on related populations provide little to elucidate depression's independent influence on either attendance or PDA. Historically, women with co-occurring SUDs and mental health disorders on TANF are difficult to retain in OSUDT (Curran et al., 2002; Dunlap et al., 2003), with barriers to treatment, such as lack of transportation, causing high rates of attrition (Rosen et al., 2004). As mentioned above, a majority of studies also point to poor prognoses after treatment for substance-dependent individuals with depression (Hasin et al., 2004); however, these findings are limited to clinical samples already in treatment. For this non-treatment-seeking sample, this study may mark the first time participants were overtly encouraged to attend and remain in treatment (by UC or ICM). Furthermore, research suggests OSDUT may be a viable alternative in low-income communities, where there is a general absence of mental health services (Allard et al., 2003). Greater access to treatment coupled with a higher readiness to change may increase engagement and spur treatment retention, ultimately affecting outcomes.
There were several limitations to this study. To eliminate potential confounders, strict eligibility criteria excluded large segments of both the welfare and substance using populations, thus limiting the generalizability of findings to only work-eligible, substance-dependent populations. Although this provided strength to analyses by focusing on only the most vulnerable, extreme cases, it prevented extrapolating findings to other substance using populations, such as individuals with a DSM-IV substance-abuse diagnosis and those drug users on or seeking methadone maintenance treatment at the time of study entry. In addition, the unique attributes of this particular ICM—such as the use of master's-level case managers, motivational interviewing, and contingency management—limit the generalizability of the findings to other versions of CM (Morgenstern et al., 2006). These components of ICM may have affected its success, and it is unknown to what extent they may be the mechanisms of action within this particular intervention.
Despite these limitations, these findings underscore the importance and effectiveness of a tailored social service intervention, such as ICM, for helping substance-dependent women on TANF with co-occurring disorders. Although this ICM intervention was not designed to address the needs of women with co-occurring disorders, it proved to be an effective intervention across a broad range of depressive symptoms. Early and thorough assessment of co-occurring mental health disorders is important for helping to determine who may be best helped by limited and coveted services to facilitate entry and tenure in an OSUDT program and ultimately affect substance use outcomes.
Further examination of the impact of high levels of depressive symptoms on the variety of forms of CM is needed. Only with more intensive, focused investigations that include both qualitative and quantitative methods implemented across populations will we begin to understand the breadth and quality of the impact of depressive symptoms on CM and discover potential causal explanations. Further understanding of the therapeutic relationship, motivations of participants, and the specific active ingredients of CM will be vital to honing its use in the mental and public health fields. In addition, studies of the impact of other mental health disorders on SUD treatment utilization and outcomes are vital to expanding our understanding of the most effective implementation of ICM specifically and CM at large.
Acknowledgements
We acknowledge the support of the Division of Family Development at the New Jersey Department of Human Services and the staff at the National Council on Alcohol and Drug Dependence. The authors thank Brett Hagman for his invaluable contributions and the reviewers for their astute suggestions.
Footnotes
This study was supported by National Institute on Drug Abuse grant 5 R01 DA 12256, the Administration for Children and Families, Assistant Secretary for Planning and Evaluation grant 90XP0002, and the New Jersey Department of Human Services.
References
- Acharyya S, Zhang H. Assessing sex differences on treatment effectiveness from the Drug Abuse Treatment Outcome Study (DATOS) American Journal of Drug and Alcohol Abuse. 2003;29:415–444. doi: 10.1081/ada-120020524. [DOI] [PubMed] [Google Scholar]
- Allard SW, Rosen D, Tolman RM. Access to mental health and substance abuse services among women receiving welfare in Detroit. Urban Affairs Review. 2003;38:787–807. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory, Second Edition Manual. San Diego, CA: Harcourt Brace; 1996. [Google Scholar]
- Besharov D, Germanis P. Full-engagement welfare in New York City: Lessons for TANF s participation requirements. Washington, DC: American Enterprise Institute, Welfare Reform Academy; 2004. [Google Scholar]
- Brady TM, Ashley OS, editors. Women in substance abuse treatment: Results from the Alcohol and Drug Services Study (ADSS) (DHHS Publication No. SMA 04-3968, Analytic Series A-26 ed.) Rock-ville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005. [Google Scholar]
- Brindis C, Theidon KS. The role of case management in substance abuse treatment services for women and their children. Journal of Psychoactive Drugs. 1997;29:79–88. doi: 10.1080/02791072.1997.10400172. [DOI] [PubMed] [Google Scholar]
- Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse. Wisconsin Medical Journal. 1995;94:135–140. [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Temporal stability of the Timeline Followback Interview for alcohol and drug use with psychiatric outpatients. Journal of Studies on Alcohol. 2004;65:774–781. doi: 10.15288/jsa.2004.65.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Supplementary administration manual for the expanded female version of the Addiction Severity Index (ASI) instrument: The ASI-F (DHHS Publication No. SMA 96-8056) Washington, DC: Government Printing Office; 1997. [Google Scholar]
- Chandler D, Meisel J, Jordan P, Rienzi BM, Goodwin SN. Substance abuse, employment, and welfare tenure. Social Service Review. 2004;78:628–651. [Google Scholar]
- Charney DA, Paraherakis AM, Negrete JC, Gill KJ. The impact of depression on the outcome of addictions treatment. Journal of Substance Abuse Treatment. 1998;15:123–130. doi: 10.1016/s0740-5472(97)00183-9. [DOI] [PubMed] [Google Scholar]
- Corcoran J. Treatment approaches for child welfare mothers with addiction problems: An empirical review to guide practice. Journal of Social Work Practice in the Addictions. 2001;1:5–24. [Google Scholar]
- Curran GM, Kirchner JE, Worley M, Rookey C, Booth BM. Depressive symptomatology and early attrition from intensive outpatient substance use treatment. Journal of Behavioral Health Services and Research. 2002;29:138–143. doi: 10.1007/BF02287700. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari J, Zweben A, Morrel T, Lee RE. Motivation hypothesis causal chain analysis. In: Longabaugh R, Wirtz PW, editors. Project MATCH: a Priori Matching Hypotheses, Results, and Mediating Mechanisms. vol. 8. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 206–222. National Institute on Alcohol Abuse and Alcoholism Project MATCH Monograph Series. [Google Scholar]
- Dum M, Pickren J, Sobell LC, Sobell MB. Comparing the BDI-II and the PHQ-9 with outpatient substance abusers. Addictive Behaviors. 2008;33:381–387. doi: 10.1016/j.addbeh.2007.09.017. [DOI] [PubMed] [Google Scholar]
- Dunlap E, Golub A, Johnson BD. The lived experience of welfare reform in drug-using welfare-needy households in inner city New York. Journal of Sociology and Social Welfare. 2003;30:39–58. [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell T, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Field CA, Adinoff B, Harris TR, Ball SA, Carroll KM. Construct, concurrent and predictive validity of the URICA: Data from two multi-site clinical trials. Drug and Alcohol Dependence. 2009;101:115–123. doi: 10.1016/j.drugalcdep.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for DSM-IV. New York, NY: Biometric Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Grant BF. The influence of comorbid major depression and substance use disorders on alcohol and drug treatment: Results of a national survey. National Institute on Drug Abuse Research Monograph. 1997;172:4–15. [PubMed] [Google Scholar]
- Green CA, Polen MR, Lynch FL, Dickinson DM, Bennett MD. Gender differences in outcomes in an HMO-based substance abuse treatment program. Journal of Addictive Diseases. 2004;23:47–70. doi: 10.1300/J069v23n02_04. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh K, Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Archives of General Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Nunes E, Meydan J. Comorbidity of alcohol, drug, and psychiatric disorders: Epidemiology. In: Kranzler HR, Tinsley JA, editors. Dual diagnosis and psychiatric treatment: Substance abuse and comorbid disorders. 2nd ed. New York, NY: Marcel Dekker; 2004. pp. 1–34. [Google Scholar]
- Hesse M, Vanderplasschen W, Rapp RC, Broekaert E, Fridell M. Case management for persons with substance use disorders. Cochrane Database of Systematic Reviews 2007, Issue 4. 2007 doi: 10.1002/14651858.CD006265.pub2. Art. No.: CD006265. [DOI] [PubMed] [Google Scholar]
- Hser Y, Huang D, Teruya C, Anglin DM. Gender comparisons of drug abuse treatment outcomes and predictors. Journal of Drug and Alcohol Dependence. 2003;72:255–264. doi: 10.1016/j.drugalcdep.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Improving the quality of health care for mental and substance-use conditions. Washington, DC: National Academy Press; 2006. [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice. 2001;8:255–270. [Google Scholar]
- Kost KA, Smyth NJ. Two strikes against them? Exploring the influence of a history of poverty and growing up in an alcoholic family on alcohol problems and income. Journal of Social Service Research. 2002;28:23–52. [Google Scholar]
- Krazler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: A posttreatment natural history study. Journal of Studies on Alcohol. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Lennon MC, Blome J, English K. Depression among women on welfare: A review of the literature. Journal of American Medical Women's Association. 2002;57:27–31. [PubMed] [Google Scholar]
- Liang K, Zeger SL. Longitudinal analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Makela K. Studies of reliability and validity of the Addiction Severity Index. Addiction. 2004;99:398–410. doi: 10.1111/j.1360-0443.2003.00665.x. [DOI] [PubMed] [Google Scholar]
- Marcenko MO, Kemp SP, Larson NC. Childhood experiences of abuse, later substance use, and parenting outcomes among low income mothers. American Journal of Orthopsychiatry. 2000;70:316–326. doi: 10.1037/h0087853. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, Prochaska JO, Velicer WF. Stages of change in psychotherapy: Measurement and sample profiles. Psychotherapy: Theory, Research, and Practice. 1983;20:368–375. [Google Scholar]
- McGue M. Genes, environment, and the etiology of alcoholism. In: Zucker R, Boyd G, Howard J, editors. The development of alcohol problems: Exploring the biopsychological matrix of risk. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1994. pp. 1–40. [Google Scholar]
- McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD. Relation of depression diagnoses to 2-year outcomes in cocaine dependent patients in a randomized continuing care study. Psychology of Addictive Behaviors. 2002;16:225–235. [PubMed] [Google Scholar]
- Metsch LR, Pollack HA. Welfare reform and substance abuse. The Milbank Quarterly. 2005;83:65–99. doi: 10.1111/j.0887-378X.2005.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Blanchard KA, Kahler C, Barbosa KM, McCrady BS, McVeigh KH. Testing mechanisms of action for intensive case management. Addiction. 2008;103:469–477. doi: 10.1111/j.1360-0443.2007.02100.x. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Blanchard KA, McCrady BS, McVeigh KH, Morgan TJ, Pandina RJ. Effectiveness of intensive case management for substance dependent women receiving Temporary Aid to Needy Families (TANF) American Journal of Public Health. 2006;96:2016–2023. doi: 10.2105/AJPH.2005.076380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Hogue A, Dauber S, Dasaro C, McKay JR. A practical clinical trial of coordinated care management to treat substance use disorders among public assistance beneficiaries. Journal of Consulting and Clinical Psychology. 2009;77:257–269. doi: 10.1037/a0014489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Keller D, Riordan A. Intensive case management for substance abusers treatment manual. 1999. Unpublished manual. [Google Scholar]
- Morgenstern J, McCrady BS, Blanchard KA, McVeigh KH, Riordan A, Irwin TW. Barriers to employability among substance dependent and nonsubstance-affected women on federal welfare: Implications for program design. Journal of Studies on Alcohol. 2003;64:239–246. doi: 10.15288/jsa.2003.64.239. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Neighbors CJ, Kuerbis A, Riordan A, Blanchard K, McVeigh KH, McCrady B. Improving 24-month abstinence and employment outcomes for substance-dependent women receiving Temporary Assistance for Needy Families with intensive case management. American Journal of Public Health. 2009;99:328–333. doi: 10.2105/AJPH.2007.133553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Riordan A, McCrady BS, Blanchard K, McVeigh KH, Irwin TW. Barriers to employability among women on TANF with a substance abuse problem. Washington, DC: Administration for Children and Families; 2001. [Google Scholar]
- Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: A review of research on case management. Schizophrenia Bulletin. 1998;24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated treatment for dual disorders. New York, NY: The Guilford Press; 2003. [Google Scholar]
- Poleshuck EL, Giles DE, Tu X. Pain and depressive symptoms among financially disadvantaged women's health patients. Journal of Women's Health. 2006;15:182–193. doi: 10.1089/jwh.2006.15.182. [DOI] [PubMed] [Google Scholar]
- Pollack HA, Danziger S, Seefeldt KS, Jayakody R. Substance use among welfare recipients: Trends and policy responses. Social Service Review. 2002;76:256–274. [Google Scholar]
- Rosen D, Spencer MS, Tolman RM, Williams DR, Jackson JS. Psychiatric disorders and substance dependence among unmarried low-income mothers. Health & Social Work. 2003;28:157–165. doi: 10.1093/hsw/28.2.157. [DOI] [PubMed] [Google Scholar]
- Rosen D, Tolman RM, Warner LA. Low-income women's use of substance abuse and mental health services. Journal of Health Care for the Poor and Underserved. 2004;15:206–219. doi: 10.1353/hpu.2004.0028. [DOI] [PubMed] [Google Scholar]
- Rosen D, Warner LA, Tolman RM. Comparing psychiatric service use among low-income women and women in a general household population. Social Work Research. 2006;30:223–232. [Google Scholar]
- Schmidt L, Dohan D, Wiley J, Zabkiewicz D. Addiction and welfare dependency: Interpreting the connection. Social Problems. 2002;49:221–241. [Google Scholar]
- Shillington AM, Hohman M, Jones L. Women in substance use treatment: Are those also involved in the child welfare system different? Journal of Social Work Practice in the Addictions. 2001;1:25–46. [Google Scholar]
- Sobell MB, Maisto SA, Sobell LC, Cooper AM, Cooper T, Saunders B. Developing a prototype for evaluating alcohol treatment effectiveness. In: Sobell LC, Ward E, editors. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. New York, NY: Pergamon; 1980. pp. 129–150. [Google Scholar]
- Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. 2nd ed. Cary, NC: SAS Institute Inc; 2000. [Google Scholar]
- The Washington Circle. A brief overview of the Forum on Performance Measures in Behavioral Healthcare [Electronic Version] 2004. Retrieved from http://www.washingtoncircle.org/pdfs/perfMeasures.pdf.
- Volpicelli JR, Markman I, Monterosso J, Filing J, O'Brien CP. Psychosocially enhanced treatment for cocaine-dependent mothers: Evidence of efficacy. Journal of Substance Abuse Treatment. 2000;18:41–49. doi: 10.1016/s0740-5472(99)00024-0. [DOI] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Wenzel SL, Tu W, Paddock SM, Griffin A, Ebener P. Prevalence and characteristics of clients with co-occurring disorders in outpatient substance abuse treatment. American Journal of Drug and Alcohol Abuse. 2004;30:749–764. doi: 10.1081/ada-200037538. [DOI] [PubMed] [Google Scholar]