1. Introduction
Worldwide, over 100 million women rely on intrauterine contraceptive devices for contraception [1]. Removal of intrauterine contraceptive devices (IUC) is typically an uncomplicated procedure, requiring simply grasping the IUC strings and pulling gently [2, 3]. Missing IUC strings, that is IUC strings that are not visible at the external cervical os, are a commonly encountered complication of IUC removal and use. Between 4.5–18.1% of IUC users have missing strings on string checks or at the time of removal [2, 4, 5]. The majority of IUCs with missing strings can be retrieved in the office with the use of proper tools and adequate anesthesia [2,5]. Here we describe a variety of tools and procedures available for retrieval of IUCs with missing strings as well as present an algorithm for their management.
Differential diagnosis
The differential diagnosis of missing IUC strings includes unnoticed expulsion, misplacement outside the uterine cavity, broken or severed IUC strings and string retraction into the cervical canal or endometrial cavity. All of these may occur with or without pregnancy [6]. Unnoticed expulsion may lead to return to normal menstrual cycles in the setting of a progestin IUC or missed periods in pregnancy and is reported in between 5–14% [4, 7] of cases with missing strings. Misplacement outside the intrauterine cavity should be suspected when a patient develops pain in the lower abdomen or pelvis, no change in menstrual cycle pattern with a progestin IUC in place, or signs and symptoms of pregnancy. An IUC may be misplaced into the abdominal or pelvic cavity, broad ligament, uterine tube or uterine wall. Misplacement is a rare finding in women with missing strings, accounting for 0–5% of cases [8]. Retraction of the tail is the most common cause of missing strings. This may be due to short, broken or severed strings, uterine enlargement secondary to a tumor or pregnancy, or rotation of the device.
Management of IUC with missing strings
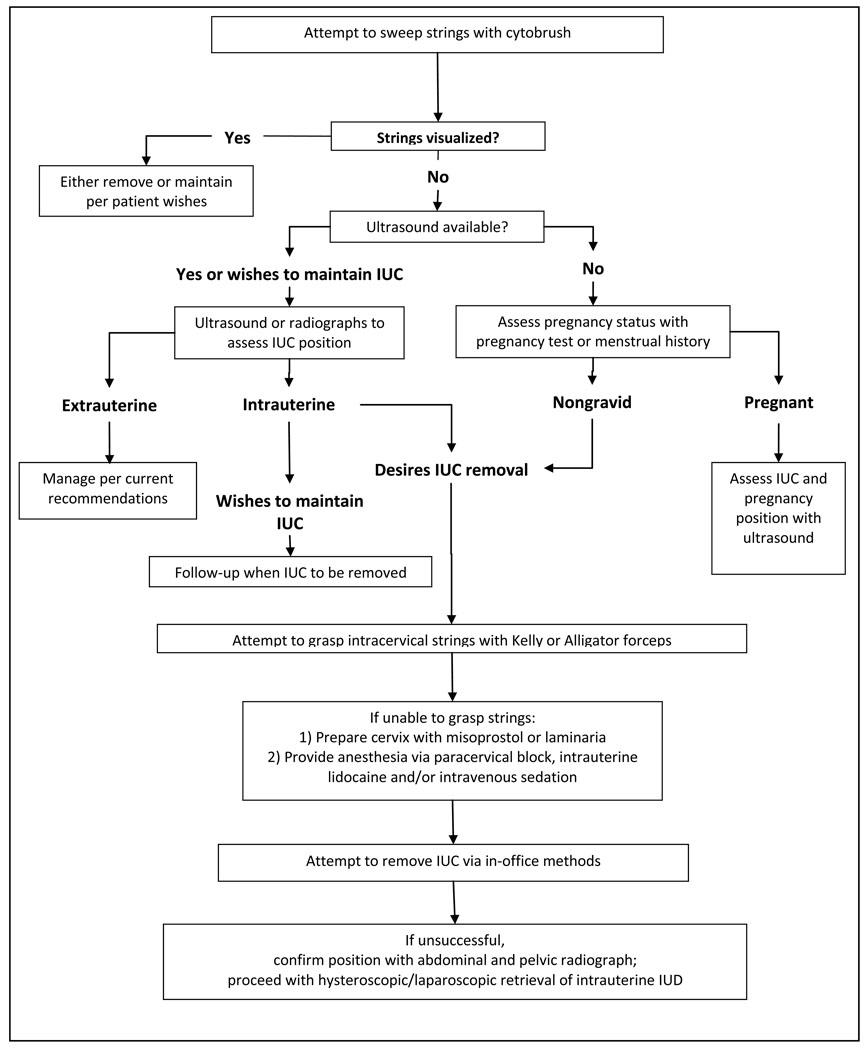
To assist in locating and managing an IUC with missing strings, the clinician should take a menstrual history and pain history as well as investigating possible expulsion. In addition, it should be determined whether the patient would like to have the IUC removed or would like to maintain the IUC (Fig. 1).
Fig. 1.
Flowchart for removal of IUC with missing strings.
Locating the intrauterine device
When IUC strings are noted to be missing, the first step in management is use of a cervical cytology brush to sweep strings from the endocervix. This procedure alone is frequently effective and can be performed regardless of intentions for the IUC or pregnancy status [9]. In addition a colposcope may be used to improve visualization of intracervical IUC strings [10]. If the strings cannot be swept easily with the cytobrush, an ultrasound examination, if readily available, should be performed to assure intrauterine location [11]. A pregnancy test should also be performed. When an appropriately located IUC is confirmed on ultrasound examination and the patient wishes to maintain the IUC, no further follow up is required until the IUC is to be removed. If the patient is pregnant or wishes to maintain the IUC, an ultrasound to assess pregnancy and IUC location should be obtained. In nonpregnant patients who desire IUC removal, further exploration of the endocervix is performed with Kelly, Patterson alligator or Spencer Wells forceps [11, 12]. If intracervical exploration is not successful, then intrauterine exploration is the next step.
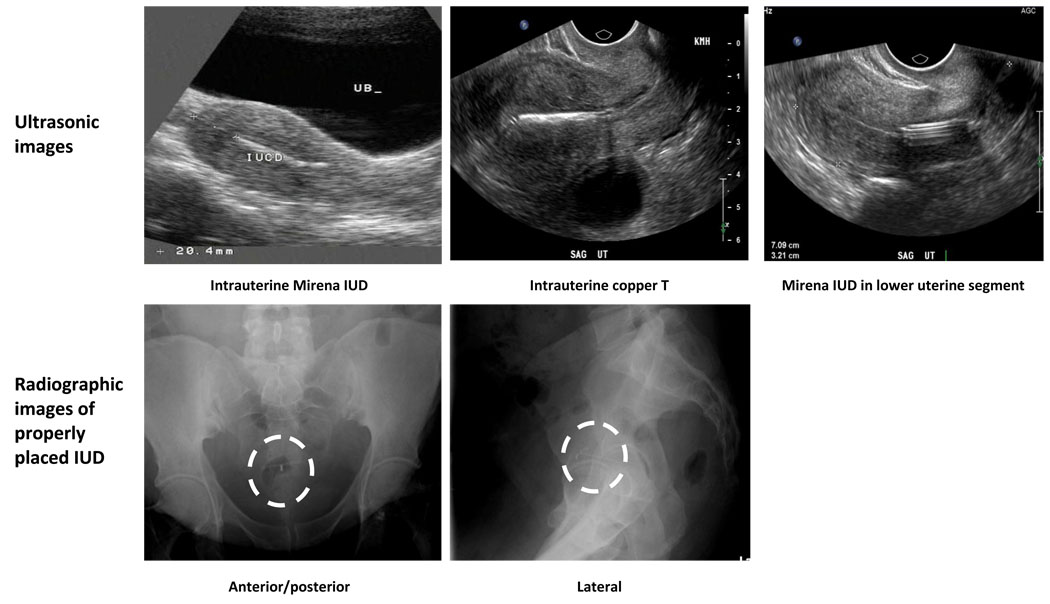
While ultrasound is currently the optimal method for determining intrauterine position, if specific signs of intrauterine IUC placement are not noted, further imaging to establish IUC position should be performed (Fig. 2) [13]. On ultrasound, the IUC should have a double bar sign and create shadowing. If these signs are not seen unequivocally, further imaging via radiography should be performed to confirm intrauterine position. An ultrasound examination performed immediately after attempting IUC removal may be misleading, as focal hemorrhage can be highly echogenic and give a false impression of an IUC in the uterus. In a patient with probable appropriate IUC placement obtaining an abdominal flat plate and a lateral pelvic radiograph may provide additional information regarding the location of the IUC [14,15]. Abdominal plain films should include the entire abdominal cavity including the most dependent portion of the pelvis and most superior aspects of the upper quadrants to prevent mistaking an intraabdominal IUC in the extremes of the abdominal cavity for an expeled IUC. An intraabdominal IUC can travel through the abdominal cavity often mimicking the pattern of bowel peristalsis [16].
Figure 2.
Radiographic and ultrasonic images of intrauterine contraceptive devices
Pain control
Intrauterine exploration for the IUC may be painful, therefore administration of analgesia and possibly cervical dilation should be performed prior to exploration. In a trial of IUC removal after Lamicel insertion, about half of women experienced substantial pain, 10% equated the intensity to that of labor pains. The remaining half of women reported they did not have significant pain [17]. Cervical dilation may be achieved by intravaginal placement of misoprostol one to two h prior to retrieval or intracervical placement of laminaria 24 h prior to the IUC retrieval attempt. Options for analgesia include a paracervical block alone or with conscious sedation. Additionally, intrauterine instillation of lidocaine has been used as a successful adjunct to paracervical block in IUC retrievals [18]. After adequate anesthesia has been administered, one may proceed with intrauterine exploration and IUC removal with one or more of the tools described below.
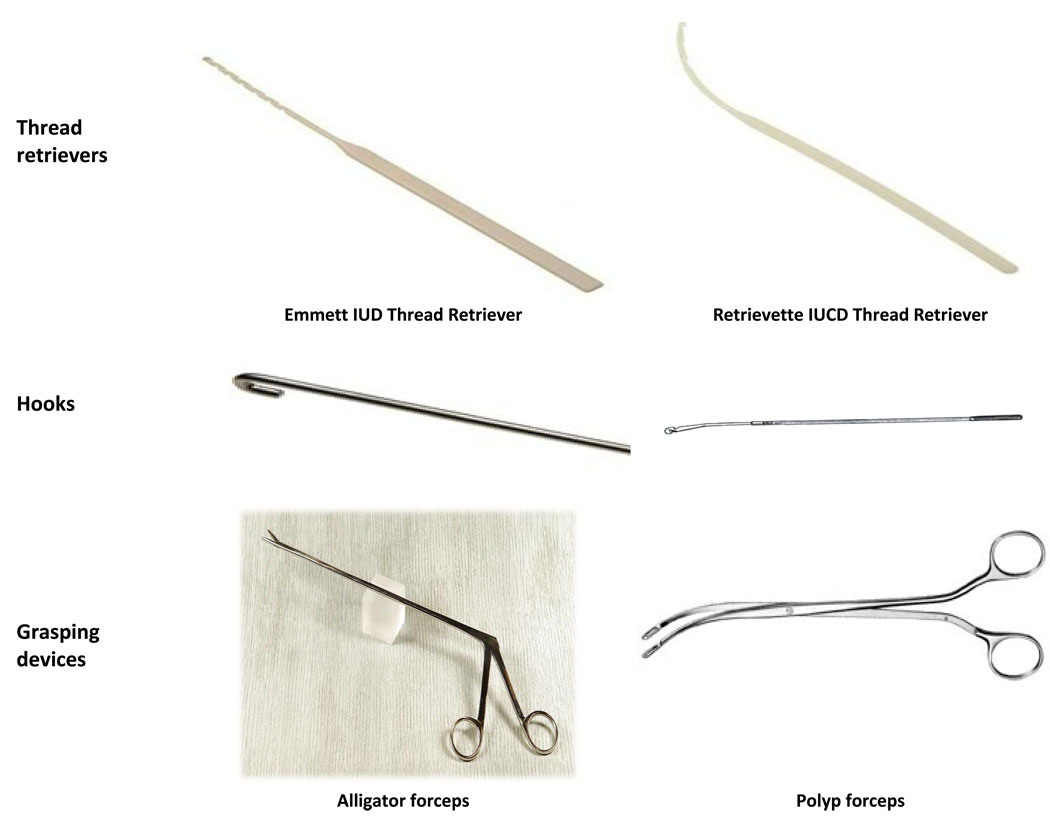
Procedures and tools for removal
Although different shapes of IUCs are available world wide [19], ring or loop shapes and T shaped IUCs are predominant. Hook devices and suction curettes are more often successful in retrieving rings or loops, while grasping devices are more useful for T shaped devices. Thread retrieval devices may be used with any shape device (Fig. 3). Following removal, particularly difficult removals, the IUC should be inspected to assure that the entire device was retrieved, fragmentation of an IUC [20] or retention of the hormone release capsule [21], although rare, has been reported.
Fig. 3.
Intrauterine contraceptive retrieval devices.
Thread retrievers
Thread retrievers are inserted into the cervix using a clockwise twisting motion both during entrance into the uterine cavity and exit out the cervix. Three types of thread retrievers are described, the Mi-Mark helix [22], the Emmett IUC retrieval device, and the Retrievette IUCD retrieval device. In a randomized controlled trial comparing the three devices, Emmett IUC retrieval device and the Retrievette users were more frequently successful than the Mi-Mark helix users at retrieving an IUC [4]. In a trial comparing the Emmett thread retriever with IUC removing forceps, the forceps were more frequently successful and were able to retrieve devices not retrievable by the thread retrievers [23].
Grasping forceps
Grasping forceps are passed through the cervix and used to grasp the IUC or strings [11, 12. The main difference in the types of forceps is fulcrum location. Patterson alligator forceps have a fulcrum approximately one centimeter from the end of the device, which allows them to be opened completely within the uterine cavity and requires no cervical dilation prior to placement. Patterson alligator forceps are available indifferent lengths; for retrieval of an intrauterine IUC a length of at least 20 cm is required. Stone or polyp forceps can also be used, however, their fulcrum is located at the midpoint of the device. The tips of these forceps may only be opened a small proportion of the entire available angle, thus limiting ability to grasp the IUC.
Hooks
Hook devices are useful for ring or loop IUC, which can be grasped with the hook and brought down to the cervix. Crochet hooks, probes bent into hook shape, as well as hooks specifically designed for IUC retrieval may be used [7, 24, 25]. No formal study has compared their efficacy.
Suction curettes
Ring and loop devices may be retrieved with a suction device such as a three to five millimeter Karman cannula [6] or a Novak curette [26]. The cannula or curette is inserted into the uterus, suction is then applied and either the string or the IUC itself is retrieved from the uterine cavity.
Ultrasound guidance
Ultrasound guidance during IUC removal is likely to improve office retrieval rates particularly among inexperienced clinicians. The quality of ultrasound equipment can influence ability to visualize the IUC and the success of the removal procedure [27].
Conclusions
Missing IUC strings are a common complication of IUC use and removal. The majority of cases may be managed in the in office setting. Cases not manageable in the office may be sent for hysteroscopy once intrauterine location is verified; however, management in the office is more convenient and less costly for the patient and the health care system. Use of proper tools, adequate analgesia, and ultrasound guidance optimize the chances for success.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Salem RM. New attention to the IUD: expanding women's contraceptive options to meet their needs. Popul Rep B. 2006:1–26. [PubMed] [Google Scholar]
- 2.Roke CM. A comparative study of the ease of removal of intrauterine contraceptive devices. Contraception. 1988;37:555–563. doi: 10.1016/0010-7824(88)90002-9. [DOI] [PubMed] [Google Scholar]
- 3.Waldron K. Intrauterine devices: insertion and removal: practical procedures. Aust Fam Physician. 1982;11:40–44. [PubMed] [Google Scholar]
- 4.Bounds W, Hutt S, Kubba A, Cooper K, Guillebaud J, Newman GB. Randomised comparative study in 217 women of three disposable plastic IUCD thread retrievers. Br J Obstet Gynaecol. 1992;99:915–919. doi: 10.1111/j.1471-0528.1992.tb14442.x. [DOI] [PubMed] [Google Scholar]
- 5.Tugrul S, Yavuzer B, Yildirim G, Kayahan A. The duration of use, causes of discontinuation, and problems during removal in women admitted for removal of IUD. Contraception. 2005;71:149–152. doi: 10.1016/j.contraception.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 6.Guillebaud J, Kasonde J. A simple scheme for managing the problem of 'lost threads' with intrauterine devices. Fertility and Contraception. 1979;3:24–32. [PubMed] [Google Scholar]
- 7.Shapiro AG. Management of the lost intrauterine contraceptive device. Obstet Gynecol. 1977;49:238–240. [PubMed] [Google Scholar]
- 8.Guillebaud J. Scheme for management of lost IUD threads. IPPF Medical Bulletin. 1980;15:1–3. [PubMed] [Google Scholar]
- 9.Ben-Rafael Z, Bider D. A new procedure for removal of a "lost" intrauterine device. Obstet Gynecol. 1996;87:785–786. doi: 10.1016/0029-7844(96)00009-9. [DOI] [PubMed] [Google Scholar]
- 10.Anteby SO, Birkenfeld A. Colposcopy in the localization of missing intrauterine devices. Endoscopy. 1984;16:146–148. doi: 10.1055/s-2007-1018561. [DOI] [PubMed] [Google Scholar]
- 11.Paragard [package insert] Pomona, NY: Duramed Pharmaceuticals; 2006. [Google Scholar]
- 12.Mirena [package insert] Wayne, NJ: Bayer Healthcare Phamaceuticals; 2009. [Google Scholar]
- 13.de Kroon CD, van Houwelingen JC, Trimbos JB, Jansen FW. The value of transvaginal ultrasound to monitor the position of an intrauterine device after insertion. A technology assessment study. Hum Reprod. 2003;18:2323–2327. doi: 10.1093/humrep/deg433. [DOI] [PubMed] [Google Scholar]
- 14.Peri N, Graham D, Levine D. Imaging of intrauterine contraceptive devices. J Ultrasound Med. 2007;26:1389–1401. doi: 10.7863/jum.2007.26.10.1389. [DOI] [PubMed] [Google Scholar]
- 15.Bonilla-Musoles F, Pardo G, Simon C. How accurate is ultrasonography in monitoring IUD placement? J Clin Ultrasound. 2005;18:395–399. doi: 10.1002/jcu.1870180505. [DOI] [PubMed] [Google Scholar]
- 16.Nitke S, Rabinerson D, Dekel A, Sheiner E, Kaplan B, Hackmon R. Lost levonorgestrel IUD: diagnosis and therapy. Contraception. 2004;69:289–293. doi: 10.1016/j.contraception.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Johnson N, Moodley J. Retrieval of intrauterine contraceptive devices with missing tails, using Lamicel. Br J Obstet Gynaecol. 1988;95:97–100. doi: 10.1111/j.1471-0528.1988.tb06487.x. [DOI] [PubMed] [Google Scholar]
- 18.Guney M, Oral B, Mungan T. Efficacy of intrauterine lidocaine for removal of a "lost" intrauterine device: a randomized, controlled trial. Obstet Gynecol. 2006;108:119–123. doi: 10.1097/01.AOG.0000223201.42144.80. [DOI] [PubMed] [Google Scholar]
- 19.Mishell DR., Jr Intrauterine devices. Clin Obstet Gynaecol. 1984;11:679–700. [PubMed] [Google Scholar]
- 20.Nadgir A, Beere D, Barker K. Intrauterine fragmentation of Gyne T380: an uncommon complication. J Fam Plann Reprod Health Care. 2004;30:175–176. doi: 10.1783/1471189041261410. [DOI] [PubMed] [Google Scholar]
- 21.Forrest A, Amarakone I, Lord J. Retained hormone release capsule following removal of Mirena intrauterine system. Bjog. 2008;115:130–131. doi: 10.1111/j.1471-0528.2007.01578.x. [DOI] [PubMed] [Google Scholar]
- 22.Ansari AH, Hoffman D. Retrieval of intrauterine contraceptive device with missing tail by means of a plastic spiral curette (Mi-Mark) Am J Obstet Gynecol. 1982;142:1061–1062. doi: 10.1016/0002-9378(82)90799-2. [DOI] [PubMed] [Google Scholar]
- 23.Johnson N, Dalton M, Bronham D. A randomised cross over trial comparing a thread retriever with IUD removing forceps. British Journal of Family Planning. 1990;16:71–73. [Google Scholar]
- 24.Diaconis JN, Weiner CI. Intrauterine device extraction: a safe method utilizing fluoroscopy. Radiology. 1974;111:479–480. doi: 10.1148/111.2.479. [DOI] [PubMed] [Google Scholar]
- 25.Landesman R. An intrauterine device extractor. Obstet Gynecol. 1971;37:618–619. [PubMed] [Google Scholar]
- 26.Abramovici H, Brandes JM. A simple ambulatory method for removal of occult IUDs. Int J Fertil. 1978;23:79–80. [PubMed] [Google Scholar]
- 27.Ismail H, Mansour D. The 'tail' of a missing intrauterine contraceptive device. J Fam Plann Reprod Health Care. 2002;28:96–97. doi: 10.1783/147118902101196045. [DOI] [PubMed] [Google Scholar]