Introduction
Despite increased attention to the problem in recent decades, acute postoperative pain (POP) control remains an ongoing challenge1, 4, 9. Failure to control POP effectively increases cost of care and causes significant suffering. Widespread speculation based on emerging literature holds that inadequately controlled postoperative pain is one of the major risk factors for the development of chronic postoperative pain3, 5.
Progress in POP management depends on quality of POP assessment. Current pain assessment practices hinder progress in pain control because of three limitations. First, postoperative pain, like all pain, is complex and multidimensional10, and reducing it to a single number is a pragmatic over-simplification. Clinicians may sometimes reify the number and treat it rather than the person in pain. Second, the 11- point numerical rating scale (NRS) and the 101-point visual analog scale (VAS), while adequate for epidemiological purposes, are too imprecise to characterize individual patient POP meaningfully Donaldson2. Third, POP assessment methods typically ignore the self-limiting nature of acute pain and fail to determine the rate of POP resolution. Because acute pain is self-limiting, its chronological dimension merits inclusion in pain assessment.
Measurement precision is a function of measurement error. All measurement involves some degree of error, and measures with less error are more precise than those with more error. Rating scale scores include error because they correspond imperfectly to the patient’s true, underlying pain. The standard error of measurement (SEM) gauges a measurement tool’s precision, indicating the typical error of measurement, the give-or-take amount by which a single score is likely to be off. Measurements with small SEMs are quite accurate and therefore reasonably precise, while measurements with large SEMs have poor accuracy and low precision. For a given measurement instrument, the SEM is the standard deviation of the measurement errors across individuals in a population. Improved precision is a fundamental goal of innovation in POP measurement.
Resolution over time is a key feature of POP, and rate of pain resolution is a potentially important clinical outcome. Yet, conventional POP measurement practices focus on static measures of pain that simply gauge POP intensity for a particular time epoch, sometimes averaging multiple pain reports obtained over time to arrive at a single score. This approach provides no information about the rate of pain resolution or POP duration. Simply plotting an individual patient’s pain scores over time reveals a monotonic trend of pain resolution, or a trajectory, that informs the clinician not only about pain intensity but also rate of change in POP. Defining POP as a trajectory rather than as one or more simple point estimates of intensity increases the information yield of pain assessment and improves measurement precision.
The primary purpose of this paper is to demonstrate and evaluate a method for modeling the POP trajectories of individual patients over six days following elective surgery. The trajectory approach to POP measurement permits classification of patients as: 1) Resolving pain over time; 2) Maintaining a constant level of pain over time; or 3) Increasing in pain over time. The secondary purposes of this paper are to: 1) Demonstrate that measurement precision of the pain trajectory is superior to that of conventional NRS point estimation; 2) Demonstrate the application of the POP trajectory to individual cases; and 3) Examine differences in the POP trajectory across age, sex, surgical site, education level and ethnic group.
Materials and Methods
Subjects
A convenience sample of 711 elective surgery patients in the University of Utah Healthcare System gave informed consent to participate in a study of larger scope that included daily reports of postoperative pain intensity. The study had the approval of the University of Utah Institutional Review Board. Of the 711 patients consented, 502 provided complete NRS data over six days following surgery. These patients ranged in age from 18 to 84 years with a median age of 46 years, and 260 were female. The proportion of female gender by surgical sites was as follows: Abdomen 100/154; back 13/32; chest 20/27; head/neck 23/51; hip 22/42; limb 74/174; and shoulder 8/22. Table 1 breaks down the sample by ethnicity and education level.
Table 1.
Education level by ethnicity.
| Ethnicity | College Degree | High School Diploma | Post Graduate Degree | Some College | Some High School |
|---|---|---|---|---|---|
| African American | 6 | 24 | 0 | 6 | 6 |
| Asian/Pacific Islander | 12 | 6 | 0 | 24 | 6 |
| Caucasian | 714 | 636 | 282 | 936 | 138 |
| Hispanic | 12 | 36 | 18 | 78 | 36 |
| Native American or Alaskan Native | 6 | 6 | 0 | 0 | 6 |
| Other | 0 | 0 | 12 | 0 | 6 |
Inclusion criteria for study participation were age equal to or greater than 18 years and elective orthopedic or general surgery at the University of Utah. Exclusion criteria were inability to speak English, physical or psychiatric co-morbidities that could compromise the ability of the patient to comply with study requirements, ongoing treatment for a pre-existing chronic pain condition, and ophthalmic surgery. We also excluded patients who would be unavailable for post-discharge follow-up.
Pain Measurement
Patients provided a pain report daily using an eleven point NRS ranging from zero to 10 with the anchors “no pain” at zero and “worst possible pain” at 10. Participants agreed to provide pain ratings at interview while in hospital and to provide subsequent pain ratings on a daily basis after discharge until they had completed the full six-day record. Using postage-paid return envelopes, they mailed their completed data forms to the study coordinator who entered the ratings into the database and de-identified the records.
Procedures
Data collectors performed initial screening on medical records, contacted potential volunteers prior to surgery on surgical wards, and obtained informed consent. They instructed consented subjects in the use of the booklet to report their pain levels on a daily basis, telling them to record their report at their convenience each day. Patients rated their postoperative pain at rest for the day. Day 1 in the data record was the first full day of recovery following surgery. Participants who completed and returned the full six days of data recording received a coupon worth $30 at a local store. Seventy one percent of consented subjects provided a complete data record.
Design and Statistical Approach
The pain trajectory is a longitudinal characterization of acute pain as a growth curve, normally resolving in intensity over days. The psychometric goal of growth curve modeling is to estimate the true, dynamic course of acute pain resolution in each individual. A basic assumption of this approach is that acute pain is an attribute of the individual patient that follows a dynamic trajectory, with individuals differing in the specific features of their unique pain trajectories. The most parsimonious characterization of an individual trajectory across six measures is a linear fit, and simple linear plots of pain intensity over days provide reasonable approximations of the true, underlying pain trajectories. With this simple linear model, each patient’s trajectory has two key features: 1) the intercept, or initial pain level; and 2) the slope, or rate of pain resolution.
To classify individual patient pain trajectories, we examined trajectory slopes. We formed a 50% confidence interval around each individual’s slope and determined whether it included zero. If the confidence interval contained zero, then we classified the subject as having a flat slope. Subsequently, we classified all cases as decreasing in pain over time, staying about the same, or increasing in pain over time2.
Measurement error for each patient’s intercept and slope derived from the individual least squares fit regression equations. To ascertain the error for each point estimate, we employed a mixed effect analysis8 using SAS Proc Mixed7. The SEM for the point estimates is the standard error of estimation for the mixed effects linear regression equation incorporating random effects for both slopes and intercepts.
Results
The Mean POP Trajectory
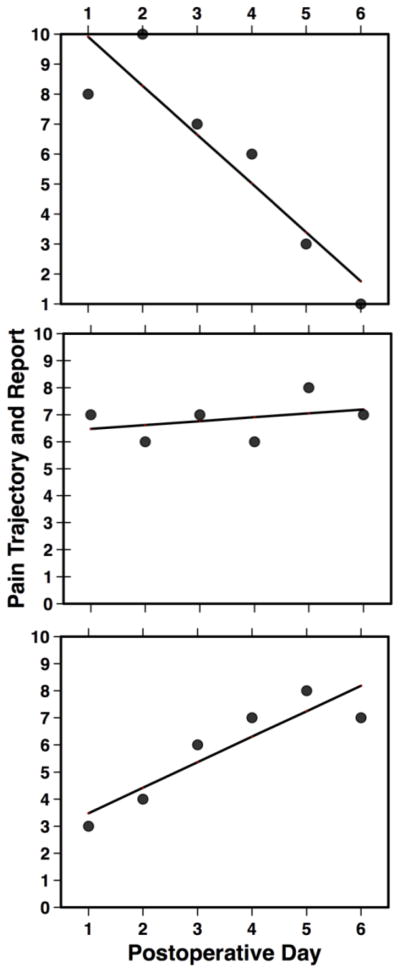
Figure 1 displays the mean POP trajectory for the entire patient sample. Comparisons of the Bayesian Information Criteria for multiple polynomial fits revealed that a linear fit provides the most reasonable approximation of POP resolution across six days. The POP trajectory has two key features: 1) The intercept, or initial pain level; and 2) The slope, or rate of pain resolution over days. The mean POP trajectory intercept was 5.59 with a standard deviation of 2.20.
Figure 1.
The Mean POP Trajectory for the entire sample (N = 502). The symbols are mean NRS values ± the 99% confidence interval for each. The line indicating the mean POP trajectory is a linear regression fitted to the points.
Patterns in Pain Resolution
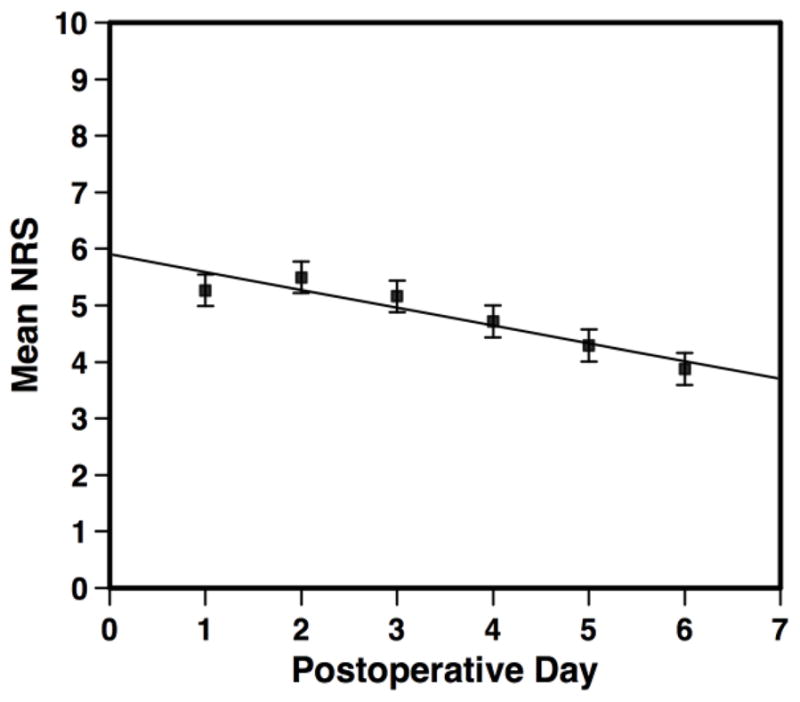
Figure 2 provides a histogram of the slopes for the entire sample. The mean slope was −.31 with a standard deviation of .45. This figure indicates that our patient sample was not homogeneous. Part of the histogram approximates or exceeds zero, indicating that some subjects failed to demonstrate a reduction in pain intensity over time. The remainder of the subjects formed two contrasting groups. Those who partly or fully resolved their pain over six days had negative slopes, and those who demonstrated a pattern of increasing pain over days had positive slopes.
Figure 2.
Histogram of postoperative pain trajectory slopes. For each case, we formed a 50% confidence interval for the slope and determined whether it included zero. We designated as flat those fits with confidence intervals that included zero. Subjects with positive slopes demonstrated increasing POP over days. Those with negative slopes demonstrated varying rates of pain resolution.
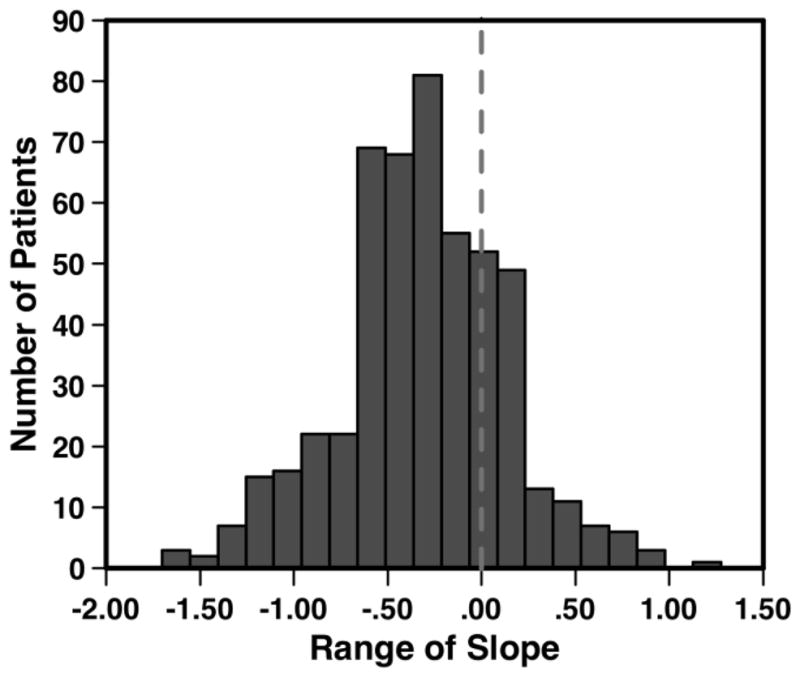
Decomposing the sample into three subgroups reveals strikingly different POP trajectory patterns. Figure 3 illustrates decomposition of the mean trajectory into three subgroups of patients classified according to the groupings that emerged from Figure 2. It displays the mean POP trajectories for: Panel A – the entire sample; Panel B – the subset with negative slopes; Panel C – the subset with flat slopes; and Panel D – the subset with positive slopes. In Panel A, 100% of the sample, the average subject resolved his or her pain at a rate less than one third rating scale unit per day. Subjects in Panel B, 63% of the sample, resolved their POP at a mean rate exceeding half a pain-rating unit per day. Panel C displays the mean POP trajectory for the 25% of the sample who did not reduce their pain at all over the six days. The 12% of the sample whose pain worsened over the six days (Panel D), on the average, reported pain increasing at the rate of about 0.4 units per day. Only 63% of the sample had the expected negative slope for POP resolution over six days while 37% had flat or positive slopes. Table 2 provides further details about the POP trajectories of the three subgroups.
Figure 3.
Contrasting patterns of postoperative pain. Panel A depicts the mean POP trajectory for all patients. Panel B shows the mean trajectory for those patients classified as having a negative pain resolution. Panel C displays the mean trajectory for those patients who had a flat slope over six days. Panel D demonstrates the mean trajectory for those patients who had increasing POP over six days.
Table 2.
Mean pain trajectories with standard deviations (SDs).
| Group | N | Sample Percentage | Mean Intercept | SD Intercept | Mean Slope | SD Slope |
|---|---|---|---|---|---|---|
| Whole Sample | 502 | 100% | 5.59 | −0.31 | ||
| Negative Slope | 314 | 63% | 6.05 | −0.58 | ||
| Flat Slope | 127 | 25% | 5.20 | −0.04 | ||
| Positive Slope | 61 | 12% | 4.02 | 0.41 |
The slope and intercept of the pain trajectories correlated inversely, r = −.47. The negative slope patients whose pain was highest at the outset tended to resolve their pain at a faster rate, about a half unit per day, than those whose pain was low or moderate at the outset. Within the group classified as positive, patients whose pain was lower initially tended to increase in pain at a slightly faster rate than patients whose pain was initially higher. On the basis of these three patterns of postoperative pain resolution, we classified all of the study patients into three groups: negative slopes, flat slopes and positive slopes.
Gender, Age, Surgical Site, Ethnicity, and Education Level
Women had a significantly higher mean intercept (X̄ = 5.77) than men (X̄ = 5.39), P <.0001), but they resolved their pain more quickly. The mean slope for women was −.347 while for men it was significantly less steep, −.287, P = .0005. For older patients, intercepts were significantly lower (P < .0001) and slopes were significantly higher (P = <.0001), indicating a slower rate of pain resolution after surgery with increasing age. Younger patients reported more pain immediately after surgery but they resolved it more rapidly.
Table 3 lists the mean intercepts and slopes for the different surgical sites. The sites differed significantly on the means for both measures (P < .0001), with mean initial pain being highest and resolving at the fastest rate for the chest surgeries. Patients undergoing hip surgeries had the lowest mean initial pain levels and the slowest rate of pain resolution.
Table 3.
Mean pain trajectories with standard deviations (SDs).
| Group | N | Sample Percentage | Mean Intercept | SD Intercept | Mean Slope | SD Slope |
|---|---|---|---|---|---|---|
| Whole Sample | 502 | 100% | 5.59 | 2.20 | −0.31 | .45 |
| Negative Slope | 314 | 63% | 6.05 | 2.11 | −0.57 | .32 |
| Flat Slope | 127 | 25% | 5.20 | 2.06 | −0.04 | .14 |
| Positive Slope | 61 | 12% | 4.02 | 2.07 | 0.41 | .24 |
Characterizing Individual Pain Trajectories
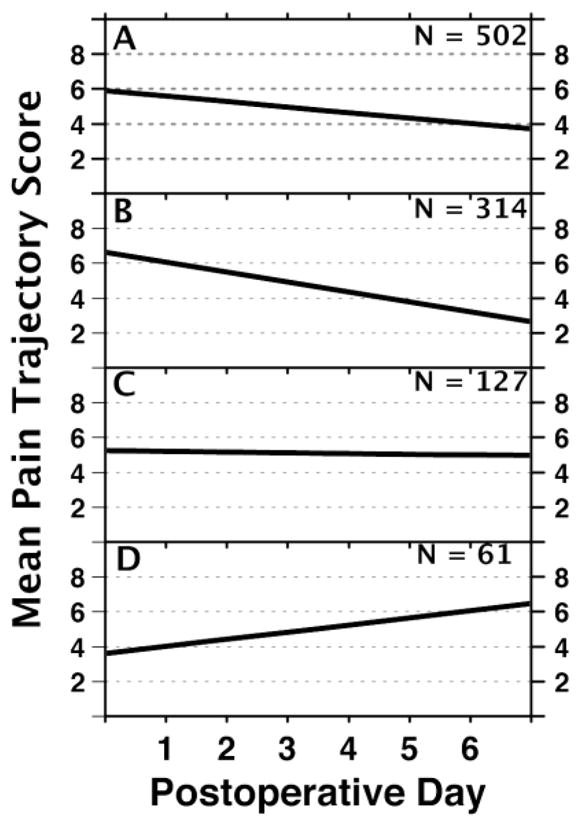
Pain trajectories provide a clinically useful way of characterizing the individual patient’s POP. Figure 4 illustrates three individual cases drawn from each of the three classifications. Patient A has a high level of pain initially but resolves it rapidly at the rate of 1.6 pain-rating units per day. Patient B has no meaningful change in POP over the six-day time window. Patient C demonstrates low initial pain intensity followed by a steady exacerbation at the rate of nearly one pain rating unit per day.
Figure 4.
Three representative patients illustrating the pain trajectory categories. Each panel displays an individual patient’s daily pain ratings (dots) and the pain trajectory (line). Panel A depicts the POP Trajectory for a 21-year old female African American patient with a negative slope following abdominal surgery. Her trajectory has an intercept of 9.91 with a slope of 1.63. Panel B depicts the trajectory of a patient who had essentially invariant pain intensity over the six days of study. This 49-year old White female patient underwent limb surgery. Her intercept is 6.48 with a slope of .14. Panel C displays an individual patient with a positive pain trajectory following surgery. This 67-year old White female patient underwent shoulder surgery. Her pain trajectory has an intercept of 3.48 and a slope of .94.
The POP Trajectory and Measurement Precision
To evaluate the measurement precision of the POP trajectory, we compared the SEMs of: a) The Standard point estimate measure of pain; b) The intercept for the POP trajectory; and c) The slope for the POP trajectory. The SEM for conventional POP measurement of a single point (point estimate), such as the first of six days, is 1.28. A Z-score range of −1.96 to +1.96 defines 95% of the area under the normal curve. Therefore, the 95% confidence interval for a patient NRS pain report of 6 would extend from 6 - (1.96 × 1.28) to 6 + (1.96 × 1.28), or from 3.5 to 8.5. An NRS report of 6 has poor precision because the rating the subject produced could just as well be any number in the 3.5 to 8.5 range. In contrast, the POP trajectory estimate of the intercept (the first day) has an SEM of .71. A patient reporting a 6 would have a 95% confidence interval ranging from 4.6 to 7.4. Thus, the pain trajectory improves precision in POP measurement.
A greater benefit occurs with estimates of change in pain across days. The SEM associated with the change across any two days for conventional measurement is 1.67 but with the pain trajectory, the SEM for such a change is a linear function of the time separation and the SEM of the slope, .22. The relative advantage of the trajectory measure is greatest for adjacent time points. With conventional measures, a patient reporting a change on the NRS from 8 to 3 on any two days would have a 95% confidence interval for change ranging from 5 – (1.96 × 1.67) to 5 + (1.96 × 1.67), which means that the true magnitude of change could be anywhere from 1.73 to 8.27. With the pain trajectory estimate based on the slope, the 95% confidence interval would extend from 5 – (1.96 × (1).22) to 5 + (1.96 × (1).22), or 4.57 to 5.43 between any two adjacent days, and from 5-(1.96 × (5).22) to 5 + (1.96 × 5(.22), or 2.84 to 7.16, between Days 1 and 6. The pain trajectory characterization of POP resolution is always more reliable and valid than obtained by simply examining the change scores, with the advantage becoming extreme with smaller time separations.
To compare the precision of the pain trajectory to that of the average over six days, we calculated the standard error of the average pain under the assumption of linear change. The expected average pain occurs at day 3.5 for each patient, and the standard error of this estimate is the square root of the linear contrast [1 3.5] Σest [1 3.5]′, where Σest is the sampling covariance matrix of the individual’s intercept and slope parameter estimates. Unlike the computation of the simple average, this provides the correct uncertainty level because it conditions on time, yielding plausible independence of the conditional responses. This trajectory-based value of the standard error of an individual’s mean response, averaged across patients, is .491, which compares favorably with the underestimate of .623 for the SE of an individual’s simple average. The SE of an individual’s predicted mean value is lower than the SE of an individual’s intercept (.71) because it lies in the middle of the bow-shaped prediction interval surrounding the regression line. Clinically, the average is of little or no utility because the hallmark feature of POP is systematic change over time.
Discussion
The main findings of this study are these: 1) Acute pain is a self-limiting condition and its measurement needs to gauge rate of resolution; 2) Obtaining and modeling repeated measures of pain over six days following surgery, the POP trajectory, yields better measurement precision and also new information about the rate of pain resolution; 3) Pain trajectory assessment makes the data of the individual patient sufficiently precise to be meaningful for interpretation; 4) The rate of pain resolution, a new variable derived from the POP trajectory, is potentially valuable for both patient management and outcomes research; and 5) The POP trajectory allows patient classification based on the direction of change, or lack thereof, following surgery. For clinical investigators pursuing the hypothesis that poorly managed POP increases the risk of chronic postoperative pain4, 5, this classification and the related slope and intercept measures open new opportunities for future research. We suggest that the slow rate of progress in POP management stems in part from: a) Imprecise pain measurement; and b) Failure to assess the chronology of acute pain, particularly its rate of resolution. Our data reveal that the POP trajectory provides better precision than conventional pain measurement approaches as well as an index of the rate of pain resolution.
We have classified patients according to their pattern of pain resolution, demonstrating that in our sample more than one third of the patients are still living with unresolved POP at six days with trajectories that predict no immediate improvement and perhaps further exacerbation. Perkins and Kehlet5 asserted that poor acute pain control is a primary cause of POP progression to chronic pain. Peters et al.6 reported that postoperative patients reporting high levels of pain four days post-surgery were at risk for chronic pain at a six-month follow-up. In our sample, 60% of patients reported a pain level greater than 4 on Day 4. The identification and additional management of patients with non-resolving pain trajectories clearly merits further study. Although tracking patients and obtaining pain scores after discharge may increase cost of care, the savings to the health care system in prevention of chronic pain should justify the expenditure.
We have characterized the acute pain trajectory in POP patients with a simple linear fit. In principle, it should be possible to apply this model within an electronic medical record, at a nursing station, or in a simple hand-carried device. Our POP trajectory derives from measures obtained daily across six days. For clinical application, it is feasible to construct and continuously revise pain ratings from every nursing shift, automatically flagging patients whose trajectories reveal increasing or non-resolving pain following surgery. As few as three measures could provide a rough idea of the direction of the trajectory. Telephone contact with patients after hospital discharge or in day surgery cases, could efficiently extend the trajectory and allow identification of those patients who need additional pain management.
Randomized controlled trials directed at improving POP can employ the POP trajectory as an outcome measure. The improved precision of measurement will allow smaller study samples than conventional acute pain measures. More importantly, the rate of pain resolution (the slope of the linear pain trajectory) provides new outcome information. With the trajectory approach to POP measurement, it is possible to develop interventions that target rapid pain resolution rather than, or in addition to, reduced pain intensity. For research purposes, the mixed effect models8 that are now available in most major statistical software packages can generate acute pain trajectories with a somewhat higher precision than simple linear fits provide. This approach to growth curve modeling combines information from the central tendencies of the sample with information unique to the individual case to optimize the estimate of the individual pain trajectory. Moreover, mixed effects models optimize testing and statistical inference to a greater degree than older statistical models. Although this methodology is not practical for everyday clinical application, it is feasible and desirable for clinical trials.
Acknowledgments
Support for this work came from a grant to the first author from the National Institutes of Health, R01 NR009542.
Footnotes
The authors have no financial or other relationships that constitute a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–540. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 2.Donaldson G. Patient-reported outcomes and the mandate of measurement. Qual Life Res. 2008;17:1303–1313. doi: 10.1007/s11136-008-9408-4. [DOI] [PubMed] [Google Scholar]
- 3.Hinrichs-Rocker A, Schulz K, Jarvinen I, Lefering R, Simanski C, Neugebauer EA. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) - a systematic review. European journal of pain (London, England) 2009;13:719–730. doi: 10.1016/j.ejpain.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101:77–86. doi: 10.1093/bja/aen099. [DOI] [PubMed] [Google Scholar]
- 5.Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology. 2000;93:1123–1133. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 6.Peters ML, Sommer M, de Rijke JM, Kessels F, Heineman E, Patijn J, Marcus MA, Vlaeyen JW, van Kleef M. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg. 2007;245:487–494. doi: 10.1097/01.sla.0000245495.79781.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singer JD. Using SAS PROC MIXED to fir multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23:323. [Google Scholar]
- 8.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press, Inc; 2003. [Google Scholar]
- 9.Sommer M, de Rijke JM, van Kleef M, Kessels AG, Peters ML, Geurts JW, Gramke HF, Marcus MA. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. European journal of anaesthesiology. 2008;25:267–274. doi: 10.1017/S0265021507003031. [DOI] [PubMed] [Google Scholar]
- 10.White PF. Multimodal analgesia: its role in preventing postoperative pain. Curr Opin Investig Drugs. 2008;9:76–82. [PubMed] [Google Scholar]