Abstract
Objective
To assess the efficacy of peer support for reducing symptoms of depression.
Methods
Medline, PsycINFO, CINAHL, and CENTRAL databases were searched for clinical trials published as of April 2010 using Medical Subject Headings and free text terms related to depression and peer support. Two independent reviewers selected randomized controlled trials (RCTs) which compared a peer support intervention for depression to usual care or a psychotherapy control condition. Meta-analyses were conducted to generate pooled standardized mean differences (SMD) in the change in depressive symptoms between study conditions.
Results
Seven RCTs of peer support versus usual care for depression involving 869 participants were identified. Peer support interventions were superior to usual care in reducing depressive symptoms, with a pooled SMD of -0.59 (95% CI: −0.98, −0.21; p=0.002). Seven RCTs with 301 total participants compared peer support to group cognitive behavioral therapy (CBT). There was not a statistically significant difference between group CBT and peer interventions, with a pooled SMD of 0.10 (95% CI: −0.20, 0.39 p=0.53).
Conclusion
Based on the available evidence, peer support interventions help reduce symptoms of depression. Additional studies are needed to determine effectiveness in primary care and other settings with limited mental health resources.
Keywords: systematic, review, self-help, mutual, depressed, psychotherapy
Introduction
Major depressive disorder is a prevalent psychiatric illness associated with significant disability, mortality, and economic burden[1–4]. Antidepressant medications are an effective treatment for major depressive disorder, but in a large multi-center effectiveness study, two thirds of patients failed to achieve remission after one medication trial, and one third still experienced significant symptoms after four trials[5]. Among patients who achieve remission with antidepressants, more than half relapse within one year. These results suggest that additional services are needed to help patients cope with continued symptoms even while they receive current evidence-based treatments. While depression care management programs can improve outcomes[6], such programs are labor intensive, poorly reimbursed, and are not widely disseminated.
Peer support services, which U.S. government health commissions determine from expert opinion to be essential components of recovery-based mental health care[7, 8], have many attractive features to recommend them as an adjunct to standard depression treatment. Peer support services bring together non-professionals with similar stressors or health problems for the purpose of mutual support or unidirectional support from an experienced peer to a novice peer. Peer support services can be delivered in groups or pairs, and in person, over the telephone, or through the internet. While cost and availability are significant barriers to the utilization of professional mental health services[9–11], peer support services that rely on voluntary efforts of non-professionals have the potential to be widely available at relatively low cost. Other access barriers, such as transportation and scheduling, may also be lower for peer support services, potentially extending the “reach” of these services into community settings[12]. Expanding peer support services for depression is likely to be acceptable based on the popularity of self-help groups for other mental health conditions and life stressors. A 1997 survey estimated 25 million Americans used some form of self-help group outside of the professional mental health community[13].
Several conceptual models exist to explain how peer support might benefit patients with depression[14–16]. Dennis described three overlapping mechanisms for possible salutary effects. According to her analysis, peer support interventions may decrease isolation (direct effect), reduce the impact of stressors (buffering effect), increase sharing of health and self-management information (direct effect), and provide positive role modeling (mediating effect)[15]. Yalom describes peer support groups as having many similar features to group psychotherapy: altruism, cohesiveness, universality, imitative behavior, instillation of hope, and catharsis[16]. Peer support programs may also empower patients to play a more active role in their own self-care[17].
Despite potential economic advantages and the multiple mechanisms through which peer support services could help patients with depression, such programs have been limited in their availability and integration with formal mental health treatment. The lack of integration has historical roots, as some community peer-run programs were formed as alternatives for patients dissatisfied with formal mental health treatment[18, 19]. Beliefs about the efficacy of peer support may also play a role. One survey of psychiatrists found that only a third discussed self-help groups with their mood disorder patients, and beliefs about lack of effectiveness were strong predictors of not supporting self-help groups[20].
The current dearth of systematic evidence regarding the efficacy of peer support may contribute to underutilization of these potentially beneficial services. Prior reviews of peer support for mental health conditions have either not focused on depression specifically, excluded interventions that had some level of professional involvement, or lacked a quantitative assessment of important outcomes such as depressive symptoms[18, 21, 22]. We therefore conducted a meta-analysis of published randomized trials to determine the evidence base for peer support services for depression. Specifically, we assessed whether peer support interventions result in greater reduction of depression symptomscompared to either usual care or psychotherapy.
Methods
Eligibility Criteria
In order for studies to be included in the meta-analysis they were required to fulfill the following criteria: 1) randomized design where participants were assigned to either a peer support intervention for depression or a usual care or psychotherapy control condition; 2) the study participants had current symptoms of depression; 3) depression symptoms were measured before and after the intervention and at similar time points in the control condition.
Interventions were considered to be peer support for depression if they placed individuals with current depression in regular contact with at least one other person with either current or prior depression. Peer support groups could be professionally led; however, in order to distinguish these from group psychotherapy (i.e. cognitive behavioral therapy), group interventions needed to either be described as peer support (or mutual support or self-help) or to be organized so that participants determined the majority of the topics and content of discussion. Interventions were included regardless of their format (i.e. groups, pairs, telephone) and could be of any duration or frequency.
Literature Search and Study Selection
Our literature search utilized queries to Medline, PsycINFO, CINAHL, and Cochrane Collaboration’s register of controlled trials (CENTRAL) databases to identify articles published as of April 2010. Searches used the following Medical Subject Headings (MeSH) and free text terms: Depression, Depressive Disorder, Depressive Disorder (Major), Peer Group, Self-Help Groups, “depress*”, “support group*”, “mutual”, “peer support”. Limits, when available, were applied to include only adult populations, any form of clinical trial, and peer-reviewed publications. We manually reviewed the reference lists of articles meeting inclusion criteria to identify additional relevant references.
Titles and abstracts were reviewed by two of the authors (PP and MV) to exclude irrelevant or clearly ineligible papers. Each reviewer then reviewed the full text of the remaining articles to make a final determination of eligibility. Discrepancies in the reviewers’ selection of eligible articles were resolved in a consensus discussion.
Data Extraction and Analysis
We reviewed each eligible study using a data extraction form to obtain the following: inclusion criteria (e.g. the method used to classify participants as depressed), number and demographic characteristics of participants, depression outcome measure(s), pre- and post-intervention or control condition scores on depression measures, and key aspects of study design such as intervention format, length, and frequency. These items were chosen to determine study eligibility, to extract the outcome data necessary for meta-analyses, to identify study population characteristics, and to identify potential sources of heterogeneity. The extraction tool was developed, pilot tested, and refined by one author (PP) and reviewed by a second author (MV).
We assessed the risk of bias for individual studies (i.e. study quality) at the study level using similar criteria to the Jadad scale[23]. Specifically, each study was assessed for the presence and quality of randomization, blinding of raters, and adequate accounting and percentage of participant drop-outs. These items were used to report overall quality of the included studies and as potential sources of heterogeneity.
The pre-to-post differences in mean values on depression measures were calculated for each arm of the trials, as were the standard deviations and number of subjects. Standardized mean differences (mean/SD) between arms were calculated as the primary estimates of effect. Analyses were conducted separately for: (a) studies that compared peer support to usual care and (b) studies that compared peer support to cognitive behavioral therapy. One study, Bright et al. [24], included four study arms using a 2×2 design to evaluate peer support and cognitive behavioral therapy on one dimension and professional group leaders vs. paraprofessional group leaders on another dimension. For purposes of the meta-analysis, this was considered as two separate trials since each arm contained different subjects for each comparison.
A DerSimonian-Laird random effects model was utilized to pool the standardized mean differences and calculate 95% confidence intervals[25]. Heterogeneity was evaluated using Cochran’s Q test of heterogeneity and I2, which measures the proportion of inconsistency among studies that cannot be explained by chance. Between-study variance (τ2) was also calculated. Alpha was set at 0.05, 2-tailed. Stratified analyses were conducted by gender and by the type of measure used to evaluate depression.
An influence analysis was conducted; this reflects the results when individual studies are omitted one at a time. We also conducted an analysis which included all subjects who were randomized to their assignment groups but later dropped out. We assumed baseline measures remained constant for patients who dropped out, a conservative approach which assumed no effect of the treatment for all subjects who did not complete the study.
To assess the possibility of publication bias, contour-enhanced funnels plots were generated[26]. The Begg and Mazumdar adjusted rank correlation test and the Egger regression asymmetry test for publication bias were also used[27, 28].
Results
Literature Search and Study Selection
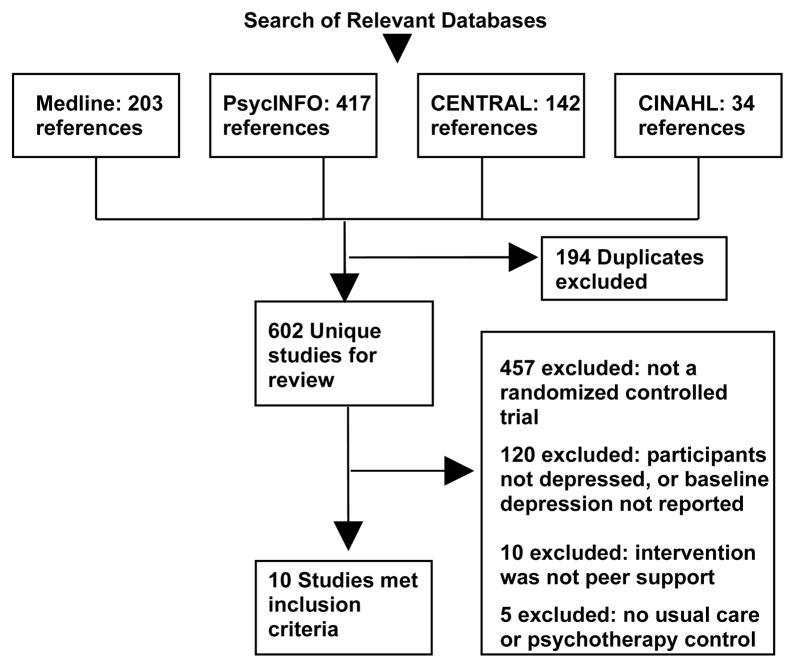
The computerized database search resulted in 602 unique abstracts to be manually reviewed. After reviewing the abstracts and full text of likely eligible studies, 10 studies were determined to meet the criteria for inclusion in the review (Figure 1)[29–38]. Seven studies compared a peer support intervention to usual care, seven compared peer support to psychotherapy, and four studies contained both comparison conditions.
Figure 1.
Selection of Studies
In each case the psychotherapy condition was group cognitive behavioral therapy. Summary characteristics of the eligible studies are provided in Table 1.
Table 1.
Characteristics of Randomized Trials of Peer Support Interventions for Depression
| Study | N | % Female | Mean Age | Primary Study Inclusion criteria | Depression Outcome Measure | Peer Support Intervention | Control Condition(s) |
|---|---|---|---|---|---|---|---|
| Ayen I. et al, 2004 | 51 | 100 | 46–56 (range) | BDI > 13, no menstrual period in last 12 months | BDI | 12 session weekly PSG | CBT, Usual care |
| Bright JI. et al, 1999 | 98 | 71 | 46 | HSRD > 10 | BDI, HRSD | 10 session weekly PSG | CBT |
| Chen CH.et al, 2000 | 60 | 100 | 29 | BDI > 9/10, post-partum | BDI | 4–5 session weekly PSG | Usual care |
| Dennis CL., 2009 | 701 | 100 | 20–34 (median) | EPDS > 9, post-partum | EPDS | ~10 weeks telephone peer mentor | Usual care |
| Evans RL. et al, 1995 | 78 | 32 | 54 | CES-D > 15, stage II cancer with planned XRT | CES-D | 8 session weekly PSG | CBT, Usual care |
| Kelly JA. et al, 1993 | 68 | 0 | 34 | CES-D > 15, HIV positive | CES-D | 8 session weekly PSG | CBT, Usual care |
| Maynard CK. et al, 1993 | 34 | 100 | 45 | Depressed women (self-identified) | BDI | 12 session weekly PSG | CBT, Usual care* |
| Michielin P. et al, 2007 | 40 | Not reported | 56–59 | BDI > 9, caregiver for someone with serious mental illness | BDI | 10 session PSG over 15 weeks | CBT |
| Ong Y. et al, 1987 | 20 | 85 | 74 | Depressed elderly patients (Feighner research criteria) following inpatient stay | Zung depression scale | 9 months weekly PSG | Usual care |
| Verduyn C. et al, 2003 | 119 | 100 | 30 | BDI > 14, mother of pre-school aged child | BDI, HRSD | 16 session weekly PSG | CBT, Usual care |
PSG = Peer support group, CBT = group cognitive behavioral therapy, BDI = Beck Depression Inventory, CES-D = Center for Epidemiological Studies Depression scale
EPDS = Edinborough Postpartum Depression Scale, HRSD = Hamilton Rating Scale for Depression, HRSD = Hamilton Rating Scale for Depression
Patients were not randomized to this condition and therefore it was excluded from the meta-analyses
There were several notable studies excluded from the analyses. Two randomized controlled trials were excluded because peer interventions were studied only as add-ons to depression care management, an effective intervention that is not part of usual care in most settings[39, 40]. Attempts to isolate the effects of peer support by comparing the combined interventions to depression care management alone would not have been consistent with our other comparisons of peer support to a usual care or to a psychotherapy control condition. If additional studies of the “add on” effect of peer support combined with depression care management become available, these studies may be important to include in separate future meta-analyses. Three randomized trials were excluded because the active comparison conditions were novel interventions (e.g. walking group, infant massage group) that as a consequence could not be pooled with either usual care or psychotherapy[41–43]. Finally two studies of peer support for depression in post-partum women were excluded because results for the pre and post depression measures were not provided and one was not a randomized trial[31, 44].
Measures used to evaluate depression
All studies included self-reported measures of depression. Six studies used the Beck Depression Inventory (BDI), two studies used the Center for Epidemiological Studies Depression Scale (CES-D), one study used the Zung Self-Rating Depression Scale, and one study used the Edinburgh Postnatal Depression Scale (EPDS). Two studies assessed depression with the Hamilton Rating Scale for Depression (HRSD) in addition to the BDI. When studies included both BDI and HSRD measures, we used the BDI results for our main meta-analyses but performed sensitivity analyses using the HRSD results, finding no differences in the reported conclusions.
Quality
Two of the three primary quality measures as described by Jadad were satisfied by all studies. In addition to all being randomized trials, all studies described participant drop-outs and reported study completion rates between 59.1% to 98.0% (mean 82.2%); outcomes were not available for subjects who dropped out. While double-blinding of psychosocial interventions was not feasible, only a three studies described single-blinding of outcomes assessments. Also, only three studies described the method of randomization, a secondary indicator of study quality.
Meta-analysis: Peer Support versus Usual Care
Seven randomized trials compared a peer support intervention for depression to usual care[30–33, 35, 36, 38]. There were a total of 849 participants among these trials. Four of the trials enrolled exclusively depressed women: two studies were of post-partum women, one was of mothers of school-aged children, and one studied menopausal women. Of the remaining studies, one was of depressed HIV positive men, another was of depressed patients with stage II cancer, and the last was of elderly patients recently discharged from an inpatient psychiatric setting.
The pooled standardized mean difference comparing peer support with usual care was −0.59 (95% CI, −0.98, −0.21; p=0.002). There was a significantly greater reduction in mean depression scores with peer support than with usual care. Heterogeneity was observed among studies, with Cochran’s Q of 20.52 (p=0.002), I2 of 70.8%, and τ2 of 0.167. Therefore, we investigated sources of the heterogeneity such as the gender of the subjects, the type of measure used to evaluate depression, and whether the study conducted blinded assessments (a quality measure). Stratification by gender and depression measure resulted in continued heterogeneity across some subgroups. When we stratified by blinding of raters, there was no longer significant heterogeneity within each subgroup. Figure 2 shows the forest plot of the results.
Figure 2.
Forest Plot Comparing Changes in Depressive Symptoms for Peer Support versus Usual Care
The intent-to-treat analysis yielded a significant reduction in depressive symptoms, with a pooled standardized mean difference of −0.65 (95% CI, −1.08, −0.21; p=0.004). According to the results of the influence analysis, the significance of our findings did not change with the removal of any one study. No evidence of publication bias was identified. Neither the Egger nor the Begg test yielded significant results (p=0.106 and p=0.548, respectively). Visual inspection of the contour-enhanced funnel plot did not show obvious asymmetry across the levels of significance.
Meta-analysis: Peer Support versus Cognitive Behavioral Therapy
A total of 301 participants were included in the seven randomized trials which compared a peer support intervention to group cognitive behavioral therapy[29, 32–37]. These studies overlap with the studies that included a usual care control condition. Three of the seven studies included only women (none were of post-partum women) and one included only men (all of whom were HIV positive). Additional studies in this analysis included a study of depressed caregivers responsible for someone with a serious mental illness and a study that sought to compare both the efficacy of professional versus para-professional group leaders and peer support versus group CBT.
The pooled standardized mean difference was 0.10 (95% CI:−0.20, 0.39; p=0.53) indicating that there was no significant difference in depression outcomes between those randomized to a peer support intervention versus group cognitive behavioral therapy. Overall, there was some heterogeneity among studies, although it did not reach significance (Cochran’s Q=11.69, p=0.11; I2=40.1%; τ2=0.071). The forest plot, stratified by use of blinded assessments to be consistent with the usual care analysis, is shown in Figure 3. According to an influence analysis, the significance of our findings did not change with the removal of any one study. The contour-enhanced funnel plot did not suggest publication bias; neither did the Egger test (p=0.487) nor the Begg test (p=0.902).
Figure 3.
Forest Plot Comparing Changes in Depressive Symptoms for Peer Support versus Group Cognitive Behavioral Therapy (CBT)
Discussion
The pooled results from randomized controlled trials indicate that peer support interventions improve depression symptoms more than usual care alone and that the effects may be comparable to those of group cognitive behavioral therapy. The estimated effect size of peer support vs. usual care for symptoms of depression (0.59) is similar to those recently reported in meta-analyses of psychotherapy trials for depression (0.67, or 0.42 after correcting for publication bias) and of published antidepressant medication trials (0.41) [45, 46]. These findings suggest that peer support interventions have the potential to be effective components of depression care, and they provide evidence in support of expert opinion advocating for peer support to be included in recovery-oriented mental health treatment[7, 8].
We found significant heterogeneity across studies comparing peer support to usual care and we were able to account for this heterogeneity by stratifying based on whether depression was assessed under conditions blinded to treatment assignment. The pooled effect size was much smaller for blinded studies than for unblinded studies (−0.21 vs. −0.95, respectively), suggesting internal bias amongst the unblinded studies. Based on this more conservative estimate of effect size, peer support may be less efficacious than some established evidence-based treatments for depression (i.e. antidepressant medications). Interestingly, a recent meta-analysis of psychotherapy for depression found the effect size to also be much lower among high quality studies (0.22 for high-quality studies vs. 0.68 for all studies) and comparable to the effect size for peer support when blinded assessments were used[47]. The observed positive effect of peer support, coupled with its potential low cost and scalability, may therefore make it an attractive alternative when other depression care interventions (including those with modestly larger effects) are unavailable, unaffordable, or unacceptable.
Our generally positive results should be viewed in the context of a mixed literature on peer support for general medical conditions and health behaviors, alcohol dependence (i.e. Alcoholics Anonymous), and serious mental illness[18, 21, 48–51]. Collectively, meta-analyses and reviews in these other areas indicate that peer support may be an effective intervention for patients with a variety of health concerns; however, much of the evidence is limited by the use of observational data or by the heterogeneous methods used to deliver and assess peer support in controlled trials.
The results of our meta-analysis are also limited in that many of the included studies drew from several distinct subpopulations of depressed individuals (i.e., post-partum women, men with HIV). While this may improve the generalizability of our findings to depressed patients with co-morbid general medical conditions, our findings may actually be less generalizable to depressed patients that have no other co-occuring condition in common. The paucity of available studies also limited our ability to conduct stratified analyses or meta-regression analyses to explore potentially important determinants of depression outcomes associated with peer support interventions, such as comorbidity, initial depression severity, or length of intervention. Our study is also limited in that the fidelity of the group cognitive behavioral therapy and the treatment that “usual care” participants received were not available to be included in the meta-analysis. It is also possible that our search strategy, which included only peer-reviewed publications, may have missed some eligible and influential studies. Our analyses, however, did not show evidence of publication bias or that any one study influenced the results. Ongoing and future studies of peer support may influence the results in subsequent meta-analyses.
Future research should employ larger randomized controlled trials, particularly among a more broadly representative population of patients with depression in primary care settings, in order to better characterize those patients for whom peer support would be most efficacious. In addition, the optimal approach to providing peer support needs clarification. Although most existing trials’ interventions used in-person peer groups, the largest trial used a telephone-based intervention with pairs. Identifying whether one or the other method, or a combination of the methods, is more effective for certain patients is an important goal for future research. Other important research questions include whether there are differences in response between patients experiencing acute versus chronic depression, the optimal duration and frequency of peer interactions, the amount and type of prior training peers should receive, and whether there are specific patient characteristics that could be used in matching patients to peers in order to improve outcomes. While peer support has the potential to be delivered at low cost, the actual costs of delivering peer support (including training of peers and coordination of services) should be formally evaluated. Finally, future trials should seek to characterize the mechanisms by which peer support may provide therapeutic benefit.
Conclusion
Based on the pooled results from published RCTs, peer support interventions for depression result in greater improvement in depression symptoms than usual care and may have similar efficacy to group cognitive behavioral therapy. There was wide variability in the patient populations and peer interventions studied, and therefore clinical trials capable of determining the optimal dose and type of peer relationships, and likely responders to peer support are needed. Given the high level of functional burden imposed by depression world-wide, peer support for depression should also be studied as a potentially low-cost intervention in primary care or other settings where more established but costly depression services are unavailable.
Acknowledgments
Funding Support: This research was supported by the VA Health Services Research & Development Service (IIR 04-104-2), Michigan Diabetes Research and Training Center (NIH DK020572) and the Michigan Institute for Clinical and Health Research (NIH UL1RR024986).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.BlairWest GW, Mellsop GW, EyesonAnnan ML. Down-rating lifetime suicide risk in major depression. Acta Psychiatr Scand. 1997;95:259–263. doi: 10.1111/j.1600-0447.1997.tb09629.x. [DOI] [PubMed] [Google Scholar]
- 2.Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: How did it change between 1990 and 2000? J Clin Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder - Results from the National Comorbidity Survey Replication (NCS-R) JAMA-J Am Med Assoc. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Global Burden of Disease (The 2004 Update) Geneva, Switzerland: 2008. pp. 44–51. [Google Scholar]
- 5.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiat. 2006;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 6.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression - A cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 7.President’s New Freedom Commission. Achieving the Promise: Transforming Mental Health Care in America (New Freedom Commission Final Report) Rockville, MD: Freedom Committee; 2003. [Google Scholar]
- 8.U.S. Department of Health and Human Services. National Consensus Statement on Mental Health Recovery. US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2004. [Google Scholar]
- 9.McCarthy JF, Blow FC, Valenstein M, Fischer EP, Owen RR, Barry KL, Hudson TJ, Ignacio RV. Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: Evaluating accessibility and availability barriers. Health Services Research. 2007;42:1042–1060. doi: 10.1111/j.1475-6773.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simon GE, Grothaus L, Durham ML, VonKorff M, Pabiniak C. Impact of visit copayments on outpatient mental health utilization by members of a health maintenance organization. Am J Psychiat. 1996;153:331–338. doi: 10.1176/ajp.153.3.331. [DOI] [PubMed] [Google Scholar]
- 11.Steele L, Dewa C, Lee K. Socioeconomic status and self-reported barriers to mental health service use. Can J Psychiat-Rev Can Psychiat. 2007;52:201–206. doi: 10.1177/070674370705200312. [DOI] [PubMed] [Google Scholar]
- 12.Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44:119–127. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Mickelson KD, Zhao S. Patterns and correlates of self-help group membership in the United States. Social Policy. 1997;27:20. [Google Scholar]
- 14.Bracke P, Christiaens W, Verhaeghe M. Self-esteem, self-efficacy, and the balance of peer support among persons with chronic mental health problems. J Appl Soc Psychol. 2008;38:436–459. [Google Scholar]
- 15.Dennis CL. Peer support within a health care context: a concept analysis. International Journal of Nursing Studies. 2003;40:321–332. doi: 10.1016/s0020-7489(02)00092-5. [DOI] [PubMed] [Google Scholar]
- 16.Yalom ID. Theory and Practice of Group Psychotherapy. 5. 2005. [Google Scholar]
- 17.Rogers ES, Teague GB, Lichenstein C, Campbell J, Lyass A, Chen R, Banks S. Effects of participation in consumer-operated service programs on both personal and organizationally mediated empowerment: Results of multisite study. J Rehabil Res Dev. 2007;47:785–799. doi: 10.1682/jrrd.2006.10.0125. [DOI] [PubMed] [Google Scholar]
- 18.Davidson L, Chinman M, Kloos B, Weingarten R, Stayner D, Tebes JK. Peer support among individuals with severe mental illness: A review of the evidence. Clin Psychol-Sci Pract. 1999;6:165–187. [Google Scholar]
- 19.Den Boer P, Wiersnia D, Van den Bosch RJ. Why is self-help neglected in the treatment of emotional disorders? A meta-analysis. Psychol Med. 2004;34:959–971. doi: 10.1017/s003329170300179x. [DOI] [PubMed] [Google Scholar]
- 20.Powell TJ, Silk KR, Albeck JH. Psychiatrists’ referrals to self-help groups for people with mood disorders. Psychiatric Services. 2000;51:809–811. doi: 10.1176/appi.ps.51.6.809. [DOI] [PubMed] [Google Scholar]
- 21.Barlow SH, Burlingame GM, Nebeker RS, Anderson E. Meta-analysis of medical self-help groups. Int J Group Psychother. 2000;50:53–69. doi: 10.1080/00207284.2000.11490981. [DOI] [PubMed] [Google Scholar]
- 22.Pistrang N, Barker C, Humphreys K. Mutual help groups for mental health problems: A review of effectiveness studies. American Journal of Community Psychology. 2008;42:110–121. doi: 10.1007/s10464-008-9181-0. [DOI] [PubMed] [Google Scholar]
- 23.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 24.Bright JI, Baker KD, Neimeyer RA. Professional and paraprofessional group treatments for depression: a comparison of cognitive-behavioral and mutual support interventions. Journal of Consulting & Clinical Psychology. 1999;67:491–501. doi: 10.1037//0022-006x.67.4.491. [DOI] [PubMed] [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 26.Sterne J, Newton H, Cox N. Meta-Analysis in Stata: An Updated Collection from the Stata Journal. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 27.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 28.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bright JI, Baker KD, Neimeyer RA. Professional and paraprofessional group treatments for depression: a comparison of cognitive-behavioral and mutual support interventions. Journal of Consulting & Clinical Psychology. 1999;67:491. doi: 10.1037//0022-006x.67.4.491. [DOI] [PubMed] [Google Scholar]
- 30.Chen CH, Tseng YF, Chou FH, Wang SY. Effects of support group intervention in postnatally distressed women. A controlled study in Taiwan. JPsychosomRes. 2000;49:395. doi: 10.1016/s0022-3999(00)00180-x. [DOI] [PubMed] [Google Scholar]
- 31.Dennis CL. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Canadian Journal of Psychiatry - Revue Canadienne de Psychiatrie. 2003;48:115. doi: 10.1177/070674370304800209. [DOI] [PubMed] [Google Scholar]
- 32.Evans RL, Connis RT. Comparison of brief group therapies for depressed cancer patients receiving radiation treatment. Public Health Rep. 1995;110:306. [PMC free article] [PubMed] [Google Scholar]
- 33.Kelly JA, Murphy DA, Bahr GR, Kalichman SC, Morgan MG, Stevenson LY, Koob JJ, Brasfield TL, Bernstein BM. OUTCOME OF COGNITIVE-BEHAVIORAL AND SUPPORT GROUP BRIEF THERAPIES FOR DEPRESSED, HIV-INFECTED PERSONS. Am J Psychiat. 1993;150:1679–1686. doi: 10.1176/ajp.150.11.1679. [DOI] [PubMed] [Google Scholar]
- 34.Maynard CK. Comparison of effectiveness of group interventions for depression in women. ArchPsychiatrNurs. 1993;7:277. doi: 10.1016/0883-9417(93)90005-h. [DOI] [PubMed] [Google Scholar]
- 35.Verduyn C, Barrowclough C, Roberts J, Tarrier T, Harrington R. Maternal depression and child behaviour problems. Randomised placebo-controlled trial of a cognitive-behavioural group intervention. British Journal of Psychiatry. 2003;183:342. doi: 10.1192/bjp.183.4.342. [DOI] [PubMed] [Google Scholar]
- 36.Ayen I, Hautzinger M. [Cognitive behavior therapy for depression in menopausal women: a controlled, randomized treatment study] Zeitschrift fur Klinische Psychologie und Psychotherapie. 2004;33:290–299. [Google Scholar]
- 37.Michielin P, Cenedese C, Cristofoli M, Zaros N. Usefulness and effectiveness of group cognitive-behavioral psychotherapy and mutual support group therapy for depressed caregivers of psychiatric patients. Giornale italiano di medicina del lavoro ed ergonomia. 2007;29:B18–25. [PubMed] [Google Scholar]
- 38.Ong Y-l, Martineau F, Lloyd C, Robbins I. A support group for the depressed elderly. International Journal of Geriatric Psychiatry. 1987;2:119–123. [Google Scholar]
- 39.Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, Groebe J, Hurt SW, Braden P, Getzell M, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. ArchFamMed. 2000;9:700. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- 40.Ludman EJ, Simon GE, Grothaus LC, Luce C, Markley DK, Schaefer J. A pilot study of telephone care management and structured disease self-management groups for chronic depression. Psychiatric Services. 2007;58:1065. doi: 10.1176/ps.2007.58.8.1065. [DOI] [PubMed] [Google Scholar]
- 41.Armstrong K, Edwards H. The effectiveness of a pram-walking exercise programme in reducing depressive symptomatology for postnatal women. Int J Nurs Pract. 2004;10:177–194. doi: 10.1111/j.1440-172X.2004.00478.x. [DOI] [PubMed] [Google Scholar]
- 42.O’Higgins M, Roberts ISJ, Glover V. Postnatal depression and mother and infant outcomes after infant massage. JAffectDisord. 2008;109:189–192. doi: 10.1016/j.jad.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 43.Onozawa K, Glover V, Adams D, Modi N, Kumar RC. Infant massage improves mother-infant interaction for mothers with postnatal depression. JAffectDisord. 2001;63:201. doi: 10.1016/s0165-0327(00)00198-1. [DOI] [PubMed] [Google Scholar]
- 44.Fleming AS, Klein E, Corter C. The effects of a social support group on depression, maternal attitudes and behavior in new mothers. Journal of Child Psychology and Psychiatry. 1992;33:685. doi: 10.1111/j.1469-7610.1992.tb00905.x. [DOI] [PubMed] [Google Scholar]
- 45.Cuijpers P, Smit F, Bohlmeijer E, Hollon SD, Andersson G. Efficacy of cognitive-behavioural therapy and other psychological treatments for adult depression: meta-analytic study of publication bias. Br J Psychiatry. 196:173–178. doi: 10.1192/bjp.bp.109.066001. [DOI] [PubMed] [Google Scholar]
- 46.Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–260. doi: 10.1056/NEJMsa065779. [DOI] [PubMed] [Google Scholar]
- 47.Cuijpers P, van Straten A, Bohlmeijer E, Hollon SD, Andersson G. The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychol Med. 40:211–223. doi: 10.1017/S0033291709006114. [DOI] [PubMed] [Google Scholar]
- 48.Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on alcoholics anonymou: Sample and study characteristics moderate findings. J Stud Alcohol. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- 49.Groh DR, Jason LA, Keys CB. Social network variables in alcoholics anonymous: A literature review. Clin Psychol Rev. 2008;28:430–450. doi: 10.1016/j.cpr.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ferri M, Amato L, Davoli M. Alcoholics Anonymous and other 12-step programmes for alcohol dependence. Cochrane Database Syst Rev. 2006:24. doi: 10.1002/14651858.CD005032.pub2. [DOI] [PubMed] [Google Scholar]
- 51.Webel AR, Okonsky J, Trompeta J, Holzemer WL. A Systematic Review of the Effectiveness of Peer-Based Interventions on Health-Related Behaviors in Adults. Am J Public Health. 100:247–253. doi: 10.2105/AJPH.2008.149419. [DOI] [PMC free article] [PubMed] [Google Scholar]