Summary
Co-occurring substance use disorders (SUDs) are common among chronic pain patients. However, limited data are available to guide treatment for chronic pain patients with SUD.
Recent data suggest that comorbid substance use disorders (SUDs) are common among chronic non-cancer pain (CNCP) patients; however, prevalence rates vary across studies and findings are limited regarding treatment options for CNCP patients with comorbid SUD. The purpose of this systematic review is to assess the prevalence, associated demographic and clinical characteristics, and treatment outcomes for CNCP patients with comorbid SUD. We conducted searches from Ovid MEDLINE, PsychINFO, and PubMED from 1950 through February 2010 and retrieved the references. Thirty-eight studies met inclusion criteria and provided data that addressed our key questions. Three to forty-eight percent of CNCP patients have a current SUD. There are no demographic or clinical factors that consistently differentiate CNCP patients with comorbid SUD from patients without SUD, though SUD patients appear to be at greater risk for aberrant medication-related behaviors. CNCP patients with SUD are more likely to be prescribed opioid medications and at higher doses than CNCP patients without a history of SUD. CNCP patients with comorbid SUD do not significantly differ in their responses to treatment compared to CNCP patients without SUD, though the quality of this evidence is low. Limited data are available to identify predictors of treatment outcome. Although clinical experience and research suggests that SUDs are common among CNCP patients, only limited data are available to guide clinicians who treat this population. Research is needed to increase understanding of the prevalence, correlates, and responses to treatment of CNCP patients with comorbid SUDs.
Keywords: Chronic pain, Substance use disorder, Treatment outcomes, Opioids, Systematic review, Quality of life
1. INTRODUCTION
An expanding empirical literature suggests that chronic non-cancer pain (CNCP) is often comorbid with substance use disorders (SUD). Recent studies indicate that CNCP is common among patients being treated for SUD [19,21] and history of SUD occurs frequently among patients who receive treatment for CNCP [38,52]. However, the prevalence rates reported in recent studies have varied substantially, as has methodological rigor.
It is generally not understood how best to treat CNCP among patients with comorbid SUD, as little empirical data are available to guide interventions. Providers may be concerned about prescribing opioid medications to patients with SUD history due to concerns of misuse, addiction, or diversion [5,28]. Additionally, patients with a history of SUD may be more resistant to traditional interventions due to increased tolerance to opioid medications, comorbid psychopathology, or other factors [3,20]. Because prior chronic pain research studies have typically excluded patients with a history of SUD [15,16], there is little information available regarding the effectiveness of interventions to treat chronic pain in this population, a population which may be at risk for poorer pain treatment outcomes.
Recent systematic reviews have examined the prevalence of SUD among patients receiving opioid medications for chronic back pain [54] and the proportion of CNCP patients prescribed opioids who develop abuse or aberrant drug-related behaviors [7]. Although these reviews provide key information regarding the prevalence of SUD among CNCP patients taking opioids and the safety of prescribing opioids; they do not directly compare risk or pain treatment outcomes based on SUD status. Since clinicians may make key treatment decisions based on history of SUD [5], additional information is needed about the safety and efficacy of interventions for patients with pain and comorbid SUD.
The primary purpose of this systematic review is to identify the prevalence of SUDs among patients with CNCP, assess clinical factors that differentiate CNCP patients with SUD from CNCP patients without SUD, describe variation in medical care received based on history of comorbid SUD, and examine differences in treatment outcomes based on SUD status.
1. METHODS
A series of key questions were developed by the research team, which were reviewed and modified by several additional individuals with expertise in the treatment of pain and/or conducting systematic reviews. These key questions assessed (1) the prevalence of comorbid SUD among patients with CNCP, (2) clinical differences that distinguish patients with SUD and CNCP from patients without comorbid SUD, (3) differences in treatment based on SUD status, (4) the efficacy of different treatments for CNCP in patients with comorbid SUD, and (5) factors that predict pain treatment outcomes among patients with CNCP and SUD. The specific key questions are included with the results.
Two research librarians independently designed search strategies based on the key questions, and conducted searches in Ovid Medline, PsychINFO, and PubMed of literature published from 1950 through February 16, 2010. Searches were limited to English-language and human studies. Appendix A provides the search strategies in detail. The results of both searches were combined into a single master reference library. We examined selected literature reviews and bibliographies to identify additional manuscripts published in peer-reviewed journals.
Investigators reviewed all of the abstracts identified from the searches. Full-text articles of potentially relevant abstracts were obtained for comprehensive review. Eligible study designs included controlled clinical trials, open-label treatment studies, systematic reviews, cohort (prospective or retrospective) studies, or cross-sectional assessments. Case reports were not included. Studies were excluded if they were not in English; addressed only acute pain; involved only animals; did not address an alcohol use disorder or illicit SUD (e.g., studies about nicotine dependence or caffeine were excluded); addressed pain due to cancer, gout, or pancreatitis; or specifically related to the use of tramadol or buprenorphine. We also excluded studies that solely examined the prevalence of aberrant medication-related behaviors, as this issue has recently been studied in depth [7].
To document chronic pain and SUD status, we relied on investigators’ operational definitions for categorization. Designation of substance misuse or SUD included positive urine drug screens for illicit substances, self-reported history of SUD, medical record documentation of SUD status, responses on validated self-report measures, as well as structured clinical interviews or diagnostic interviews.
Criteria developed by the United States Preventive Services Task Force were used to rate the quality of studies for providing data to our specific key questions [10]. In some instances, we abstracted data from studies that were not specifically designed a priori to address our specific key questions. In these instances, we rated the quality of the study to address our key questions, which may not necessarily be representative of the overall quality of the study. Individual studies were initially rated as “good”, “fair”, or “poor” by two investigators who were blinded to one another’s ratings, (see Appendix B for criteria used). A third reviewer arbitrated when there were disagreements. We assessed the overall quality of evidence addressing each key question using a method developed by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) Working Group [2], which rates the evidence from “Very Low” to “High” (see Appendix C).
2. RESULTS
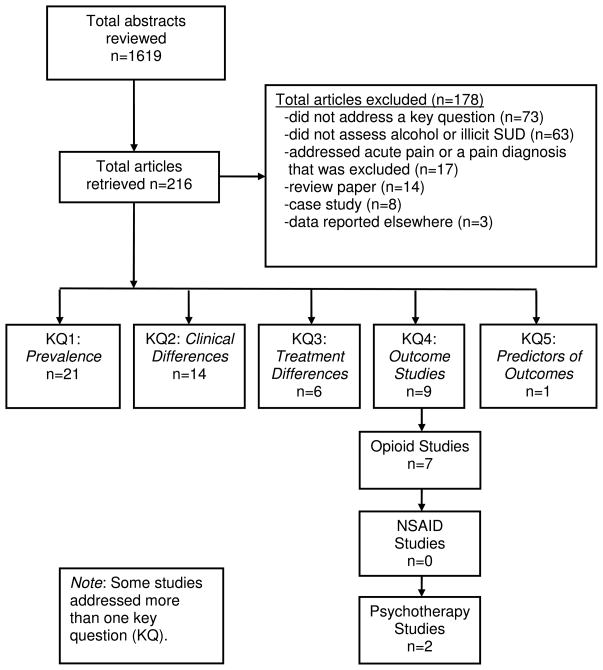
The combined library contained 1,552 unique citations, 216 were reviewed at the full-text level as they initially appeared to relate to a key question. Additional articles were excluded if they did not answer a key question (n=73), did not assess CNCP or SUD (n=63), con0sisted solely of a case study (n=8), related to pain diagnoses that were excluded (n=17), was a narrative or non-systematic review paper (n=14), or the article was a summary of results reported in another manuscript (n=3). Figure 1 shows a flow diagram for the results of the literature search and articles that were included or excluded. A total of 38 articles were identified that provided data on at least one key question.
Figure 1.
Chronic Non-Cancer Pain and Substance Use Disorder (SUD) Literature Review.
3.1. Key Question 1: What is the prevalence of comorbid substance use disorder (SUD) in patients with chronic non-cancer pain?
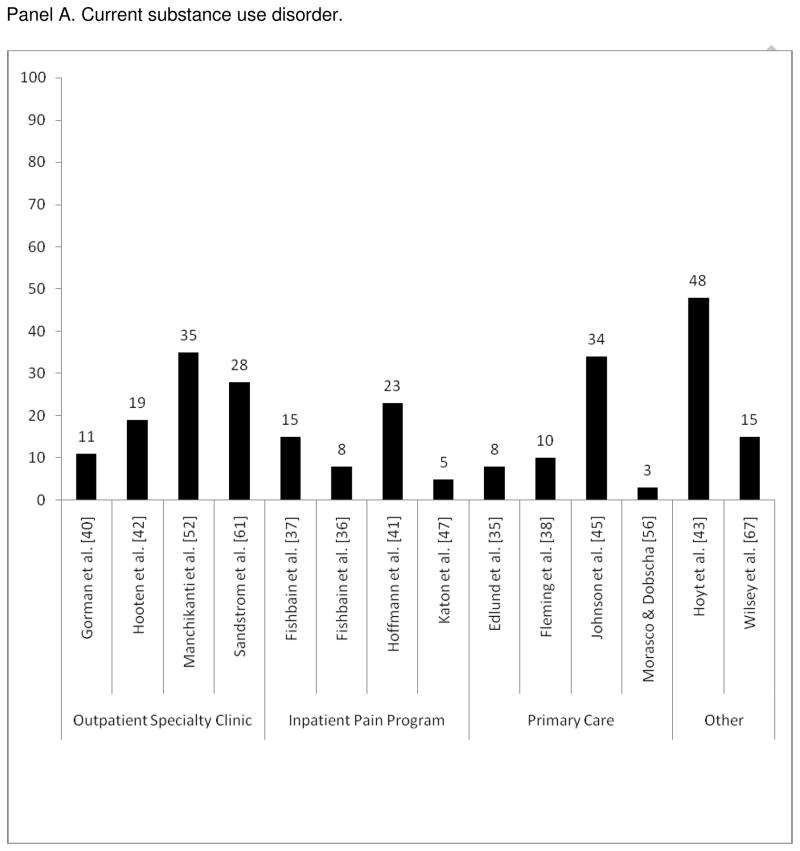
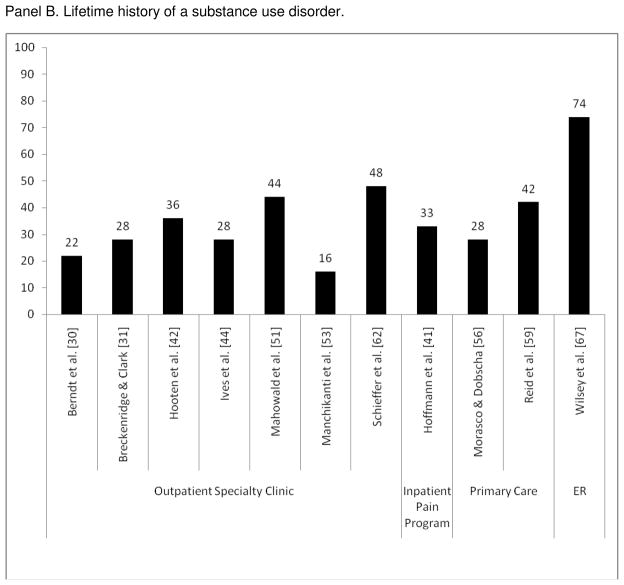
We identified a total of 21 studies that provided data on the prevalence of comorbid SUD among chronic pain patients (Figure 2). These included one systematic review, 14 cross-sectional studies, four prospective cohort studies, and two retrospective cohort studies.
Figure 2.
Proportion of chronic non-cancer pain patients with a current or lifetime substance use disorder.
Panel A. Current substance use disorder.
Panel B. Lifetime history of a substance use disorder.
One good quality systematic review examined the prevalence and efficacy of opioid prescribing for chronic back pain among empirical studies published from 1966–2005 [54]. This included studies on the prevalence of SUD in patients prescribed opioids for chronic back pain. Studies were included if they focused on chronic back pain, adults, non-obstetric, had no pre-existing diagnosis of opioid dependence, and included use of opioids. Of the four studies reviewed that examined the prevalence of SUD among chronic back pain patients who were prescribed opioids, the reported prevalence of current SUD ranged from 3% to 43%, with a lifetime prevalence as high as 54%. Studies varied with respect to methods used to assess SUD, patient heterogeneity, and type of clinical practice. These studies were rated as generally being of poor quality.
In our review of studies, which included CNCP patients regardless of whether they were prescribed opioids, we found the overall prevalence of current SUD among CNCP patients was broad, ranging from 3% to 48% [35–38,40–43,45,47,52,56,61,67]. The lifetime prevalence of any SUD ranged from 16% to 74% [30,31,41,42,44,51,53,56,59,62,67]. The highest rates of SUD were in samples of CNCP patients visiting emergency rooms seeking opioid refills (e.g., 74% met criteria for lifetime SUD) [67], patients who were medically compromised (e.g., 48% of inpatients with severe pain in a tertiary care facility or residential program for AIDS met criteria for current SUD) [43], or when urine toxicology was used to identify substance use (e.g., 35% of patients seeking care at an interventional pain management practice had a positive urine drug screen for an illicit substance or non-prescribed substance) [52].
3.2. Key Question 2: How do patients with chronic non-cancer pain and comorbid SUD differ from chronic non-cancer pain patients without a history of SUD on demographic and clinical factors?
We found 14 studies that directly compared patients with CNCP and SUD versus CNCP alone on demographic and clinical factors; these included nine cross-sectional and five cohort studies. Based on the literature, the results are categorized into one of four groups (described below): demographic variables, pain outcome variables, psychiatric variables, and prescription medication misuse.
3.2.1. Demographic Variables
Six studies compared differences among CNCP patients on demographic variables based on SUD status. In a poor quality cohort study of 50 patients referred to an orthopedic clinic for low back pain, male patients with high alcohol use had higher rates of unemployment than male patients with low alcohol use (specific numbers not provided) [61]. In another poor quality study of 500 patients in a rural private practice prescribed opioids for pain management, women had higher rates of past marijuana use than men (13% versus 7%, no p-value reported), but there were no difference in the rate of overall past drug use based on gender (19% among women and 12% among men; no p-value reported) [53]. In contrast, a good quality study of 283 patients at a hospital-based pain center found higher rates of current SUD among men compared to women (20.4% versus 7.9%, p < 0.01) [37]. Additional studies reported no differences among CNCP patients based on SUD status on the variables age, gender, race/ethnicity, marital status, years of education [56], or employment status [39]. A fair quality retrospective cohort study analyzing data from two health plans, which represented approximately four million total patients, found that men with CNCP were over-represented among those with illicit SUD history or alcohol use disorders [64]. However, a higher proportion of women with CNCP had prior opioid use disorders. Individuals with CNCP and a history of SUD were younger than those without a history of SUD.
In summary, data are mixed regarding whether women or men with chronic pain were more likely to have a prior SUD. Inconsistent results were also found on age and employment status. Other reports suggest that there were no significant differences among chronic pain patients based on SUD status on the variables gender, race/ethnicity, marital status, or years of education (Grade = Very Low).
3.2.2. Pain Variables
Five studies were available that compared differences on pain-related variables between pain patients with and without comorbid SUD. A poor quality and good quality study did not detect any differences on measures of pain intensity or pain functioning based on SUD status [43,62]. A fair quality study that included only veterans who were diagnosed with hepatitis C found that patients with a history of SUD were more likely to have a current pain diagnosis than patients without a history of SUD, although the absolute percent differences was small (69% versus 63%, p < 0.001) [65]. The remaining two studies had conflicting results. In a poor quality cross-sectional study with 142 patients at an outpatient clinic for low back pain, patients with low alcohol use reported more impairment in functioning due to pain than patients with higher current alcohol use [40]. A fair quality cross-sectional study of 127 patients recruited from VA primary care clinics who were taking opioids for musculoskeletal pain found that patients with a history of SUD had lower scores of pain intensity than patients without a history of SUD, but no other differences were detected in regards to pain diagnoses, duration of pain, or scores on measures of pain functioning [56].
In summary, the data regarding the relationship between SUD status and pain variables among patients with CNCP are contradictory. Several studies suggest that CNCP patients with comorbid SUD do not differ from pain patients without comorbid SUD on measures of pain intensity or functioning while other studies do not find this relationship (Grade = Very Low).
3.2.3. Psychiatric Variables
Four studies included information comparing differences on psychiatric and mental health variables among CNCP patients based on SUD status. One good quality study of 288 VA multidisciplinary pain clinic patients found that SUD patients had higher scores of anxiety, but not depression [62]. In a separate fair quality study on 127 VA primary care patients taking opioids for chronic musculoskeletal pain, no differences were detected on measures of current depression, PTSD, quality of life, or current alcohol or substance use [56]. In a poor quality study with 48 CNCP patients admitted to a hospital for treatment of chronic infections or AIDS, SUD patients were more likely to endorse tobacco abuse, but no differences existed in history of emotional of physical abuse (p < 0.05) [39]. In a separate poor quality study with 500 CNCP patients prescribed opioids and recruited from a rural private practice, patients with depression were more likely to have current substance abuse (12% versus 5%, no p-value reported) [53].
In summary, the data regarding the relationship between SUD status and psychiatric variables among CNCP patients are generally mixed or non-significant. Some prior reports indicate that pain patients with a history of SUD reported more depression, anxiety, and tobacco use. However, other studies indicated no differences based on SUD status on these and other variables measuring quality of life (Grade = Very Low).
3.2.4. Prescription Medication Misuse
Seven available studies specifically compared CNCP patients on measures of aberrant medication-related behavior based on SUD status. In four separate fair to good quality studies, patients with a history of SUD were significantly more likely to exhibit or report prescription medication misuse [38,56,59.62]. However, three other poor to fair quality studies found no statistically significant difference in rates of prescription medication misuse among CNCP patients with SUD versus those without SUD [48,51,65].
Four of the above studies utilized more sophisticated statistical analyses (e.g., controlled for important covariates, used validated measures, had adequate statistical power) to examine the relationships between SUD status and prescription medication misuse. In three separate studies with primary care patients taking opioids for CNCP, SUD status independently predicted greater likelihood of prescription medication misuse, even after controlling for potentially confounding variables [38,56,59]. An additional good quality report with 288 patients recruited from a VA outpatient pain clinic found that, after controlling for demographic, pain, and psychological factors, medication beliefs (such as thoughts about expected relief from medication) mediated the relationship between SUD status and prescription medication misuse [62].
In summary, the relationship between prescription medication misuse and SUD status is mixed when reviewing the results from studies that simply compare frequencies. However, results from more methodologically rigorous studies suggest that history of SUD is associated with current prescription medication misuse (Grade = Moderate). One additional study indicated that medication beliefs could mediate the relationship, but further work is needed to replicate this finding.
3.3. Key Question 3: In what ways does pain treatment differ when comparing patients who have comorbid chronic non-cancer pain and SUD to chronic non-cancer pain patients who do not have SUD?
A total of six studies, four retrospective cohort and two open-label treatment studies, specifically addressed treatment received for CNCP between SUD and non-SUD patients (Table 1). The data are mixed regarding the ways in which pain treatment differs based on SUD status. Three reports suggest that SUD patients with CNCP were more likely to receive opioids [31,55,64], while another study indicates that CNCP patients with the hepatitis C virus and a history of SUD were less likely to receive opioids [65]. Additionally, there are conflicting data regarding medication dose, as one prior study reported that SUD patients with CNCP and AIDS require higher doses of morphine [46], a second report indicates that CNCP patients with SUDs had lower doses of fentanyl [57]. The most recent study available, summarizing data from two large health plans, suggests that CNCP patients with comorbid SUD are more likely than CNCP patients without a history of SUD to be prescribed opioids, and to receive a higher dose [64].
Table 1.
Key Question 3: Differences in Clinical Treatment for Chronic Non-Cancer Pain Based on Substance Use Disorder (SUD) Status.
| Reference | Study Design | Setting | Number enrolled | Results | Quality Rating |
|---|---|---|---|---|---|
| Kaplan et al. [46] | Open-label treatment study | Inpatients and outpatients with AIDS at 1 of 5 specialty pain service teaching programs | N = 44 | More SUD patients were in the high dose opioid group (47%) than low dose opioid group (16%). No difference between groups in the proportion reporting acceptable analgesia (72% non-SUD vs. 67% SUD). SUD patients required higher doses of sustained-release morphine initially and at the final dose (p=.0004). | Poor |
| Newshan & Lefkowitz [57] | Open-label treatment study | Outpatients with AIDS | N = 35 | Patients with SUD history of had lower doses of fentanyl than patients without SUD history (36.1 +/− 19.6 mg/h vs. 62.5 +/− 28.9 mg/h, p<.003) | Poor |
| Breckenridge & Clark [31] | Retrospective Cohort | A VA Medical Center and an outpatient general medical clinic | N = 200 | Patients with SUD were more likely to be prescribed an opioid rather than NSAID (OR=4.7). | Fair |
| Massey et al. [55] | Retrospective Cohort | Level 1 trauma center. All patients had admission to hospital for high-energy fracture and treated by orthopedics | N = 50 | Patients with positive toxicology screens at baseline were more likely to be prescribed opioids 3–6 months after discharge. At 6 months, rate was 53% vs.7% (OR=14.5) | Poor |
| Whitehead et al. [65] | Retrospective Cohort | Veterans with the hepatitis C virus from the Pacific Northwest | N = 8,224 | Of hepatitis C patients with a pain diagnosis, those with history of SUD were less likely to receive opioids in past year (36% vs. 43%, p<0.001) and in past 3 years (56% vs. 60%, p<0.01) than patients without a history of SUD. | Fair |
| Weisner et al. [64] | Retrospective Cohort | Members of two health plans: Kaiser Permanente of Northern California and Group Health in Washington | All members in both health plans were potentially eligible | Baseline rates for long-term opioid use were higher for those with SUD history than without, and remained higher over time in both health plans (Kaiser, increased from 11.7% to 17.0% for SUD, versus 2.6% to 3.9% for non-SUD; Group Health increased from 7.6% to 18.6% for SUD, versus 2.7% to 4.8% for non-SUD). In both health plans, SUD patients were on higher dose regimens, received more days supply, and were more likely to receive short-and long-acting Schedule II opioids and long-term supplies of sedative-hypnotics, compared to non-SUD patients. | Fair |
In summary, there appear to be two possible explanations for the results observed. The preponderance of the available data suggest that CNCP patients with SUD are more likely to be prescribed opioids, and at higher doses, than CNCP patients without a history of SUD (Grade = Low). Alternatively, however, the likelihood of CNCP patients with SUD receiving an opioid as part of treatment may vary due to the healthcare system in which they are treated, or possibly based on comorbid illness.
3.4. Key Question 4: What is the efficacy of pain treatment in patients with chronic non-cancer pain and SUD?
3.4.1. How effective are opioid medications in improving pain intensity and/or pain functioning in patients with chronic non-cancer pain and SUD?
We found no randomized controlled trials. One open-label treatment study, five cohort studies, and one clinical case series specifically discussed outcomes of opioid medications to improve pain outcome variables based on SUD status. Table 2 provides a summary of the data abstracted from these studies. Regarding compliance with treatment, results from two cohort studies provide mixed data regarding whether CNCP patients with SUD are as likely as non-SUD patients to remain in treatment [32,66]. Of patients who are adherent with treatment, the data suggest that SUD patients do not significantly differ with regard to the benefit received from opioid therapy and/or treatment with a multidisciplinary pain team, compared with CNCP patients without a history of SUD [32,34,57,58,66]. A case series and a prospective cohort study also found that participation in a methadone maintenance-type program to treat CNCP in patients with comorbid SUD was helpful in reducing pain and improving quality of life [49,60]. These studies were generally rated poor to fair due to inconsistent use of validated outcome measures, not controlling for significant confounding variables, not stratifying based on SUD status, and/or high attrition (Grade = Low).
Table 2.
Key Question 4: Efficacy of Interventions to Treat Chronic Non-Cancer Pain in Patients with Substance Use Disorder (SUD).
| Reference | Study Design | Setting | Number enrolled | Intervention | Results stratified by SUD status | Results | Quality Rating |
|---|---|---|---|---|---|---|---|
| Portenoy & Foley [58] | Retrospective Cohort | Outpatient pain clinic | N = 38 | Long-term opioid therapy (no standard dosing noted). | No | 24 of 38 (63%) patients reported partial to fully adequate relief of pain, 14 of 38 (37%) reported inadequate relief, and 2 patients (both with history of SUD) became a management problem. | Poor |
| Kennedy & Crowley [49] | Case Series | Outpatient methadone program | N = 4 | Enrollment in an outpatient methadone maintenance program to treat chronic pain and comorbid SUD. | No | 3 of 4 patients remained in treatment. Treatment completers had slight to moderate improvements in pain intensity scores. All treatment completers had reductions in frequency and severity of substance use. | Poor |
| Dunbar & Katz [34] | Retrospective Cohort | Outpatient pain clinic | N = 20 | Received oral opioids to treat chronic pain (no standard dosing noted). | No | 9 of 20 (45%) patients had improvements in pain. Patients with a history of alcohol abuse alone and enrollment in Alcoholics Anonymous (AA) were successfully managed with opioids and those with history of polysubstance and no participation in AA did poorly. | Poor |
| Newshan & Lefkowitz [57] | Open-label treatment study | Outpatients with AIDS and chronic pain | N = 35 | All patients received 15 days of treatment with oral opioids, and then switched to 15 days with fentanyl treatment. | Yes | At the end of treatment, no differences were detected between patients on Brief Pain Inventory scores based on history of SUD (p=0.09) | Poor |
| Chelminski et al. [32] | Prospective Cohort | Outpatient specialty pain clinic | N = 85 | Multidisciplinary treatment team consisting of medicine, pharmacy, and nursing. | No | There was no difference in rates of prior SUD between treatment completers versus non-completers (40% vs. 55%, p=0.23). Significant improvements were evident for all patients on validated measures of pain functioning, pain severity, and depression severity (all p-values<0.05). | Fair |
| Rhodin et al. [60] | Prospective Cohort | Outpatient methadone maintenance program | N = 60 | All patients enrolled in a pilot methadone program to treat chronic non-cancer pain (average treatment duration was 34 months). | No | For patients with follow-up data (48/60, 80%), 75% rated pain relief as “good” and 25% as “moderate.” Quality of life was generally improved for treatment completers. 18 (30%) patients left the program: 3 recovered, 5 died from their original disease, 4 dismissed due to medication misuse, 5 had side effects, and 1 reported insufficient pain relief. | Poor |
| Wiedemer et al. [66] | Retrospective Cohort | Outpatient opioid renewal clinic at a VA medical center | N = 335 | Clinic staffed by nurse practitioner and pharmacist (with consultation from multidisciplinary pain team). | No | Patients referred for aberrant drug taking were more likely to drop out of treatment (38%) than patients with no history of aberrant medication use (100%; no p-value reported). | Poor |
| Khatami et al. [50] | Pre-post intervention study | Individual patients recruited from an addictions clinic | N = 6 | Individual psychotherapy (averaged 31 sessions), focused on “symptom control, stimulus control, and social system modification.” | No | 5 of 6 patients completed treatment. For treatment completers, significant improvements were evident in pain, hopelessness, depression, and anxiety (p<0.05). All patients reported abstinence from illicit substances at the end of treatment. | Poor |
| Currie et al. [33] | Pre-post intervention study | Outpatient group psychotherapy for chronic pain patients completing a substance abuse treatment program | N = 44 | 10-week outpatient pain management group psychotherapy (primarily based on cognitive-behavioral therapy and included focus on relapse prevention). | No | Significant improvements were seen post-treatment and at 12-month follow-up on measures of pain functioning, life control, and affective distress. Pain severity reduced by 35% from pre-treatment to the 12 month follow up. At the three month follow-up, 68% of patients were improved on at least one outcome measure. Addiction Severity Index scores improved on all domains. 15 of 44 patients (34%) dropped out of treatment. | Good |
3.4.2. How effective are non-opioid medications in improving pain intensity and/or pain functioning in patients with chronic non-cancer pain and SUD?
We found no randomized controlled trials, cohort studies, case series, or other systematic observational studies that assessed the efficacy of non-opioid medications to treat CNCP specifically in patients with a history of SUD.
3.4.3. How effective are psychological interventions in improving pain intensity and/or pain functioning in patients with chronic non-cancer pain and SUD?
Two studies were identified. A small poor quality pilot study examined an outpatient treatment for CNCP with six patients recruited from an addictions clinic. Participants averaged 31.2 individual therapy sessions and treatment included three parts: symptom control, stimulus control, and social system modification. Of the five patients who completed treatment, statistically significant improvements were found on measures of pain, hopelessness, anxiety, and depression [50]. An open-label good quality treatment study examined the impact of a 10-week cognitive-behavioral group intervention among 44 patients with CNCP and SUD [33]. Treatment focused on improvement in pain functioning and emphasized prevention of relapse to SUD. Intent-to-treat analyses showed significant improvements in pain severity, functioning, impairment from substance use, and quality of life. Participants also showed significant improvement in self-management and internal coping strategies, as well as reduced use of analgesic medications.
The overall but limited data from studies assessing psychological interventions to treat chronic non-cancer pain in SUD patients indicate these interventions show promise for reducing pain and improving function (Grade = Very Low).
3.5. Key Question 5: What patient factors are associated with improved pain intensity and/or pain functioning in patients with chronic non-cancer pain and SUD?
One poor quality study provided data about baseline patient factors associated with pain outcomes among SUD patients with CNCP. This retrospective cohort study included 20 patients with a history of an alcohol use disorder or SUD who were referred to an outpatient hospital-based pain clinic [34]. Patients were divided into two groups based on whether they were considered at risk for prescription opioid misuse by their treating physician. Of the 11 patients who were not considered at risk for prescription opioid misuse, nine (82%) had improvements in pain control. In contrast, none of the nine patients who were considered high risk for prescription opioid abuse had improvements in pain control. Results suggest that baseline rating of risk for prescription opioid abuse is associated with a decreased likelihood of improvement in pain control (Grade = Very Low).
3. DISCUSSION
Treating CNCP is a challenge and even the best interventions result in many patients continuing to experience some degree of pain and/or disability [24]. Treating chronic pain among patients with comorbid SUD is more complex, as clinicians not only must treat the pain, but are often additionally concerned about issues of medication safety, misuse, and diversion [5,28]. The purpose of this systematic review was to synthesize evidence on the detection and treatment of CNCP in patients with comorbid SUD. Overall, the literature provides either limited or mixed evidence to guide clinicians in this area. Data indicate that the prevalence of current SUD among CNCP patients is in the range of 3% to 48%, and that the lifetime rate of SUD ranged from 16% to 74%.
Although patients with a history of SUD comprise a significant portion of CNCP patients, they have typically been excluded from chronic pain intervention studies [15,16], leaving a paucity of data on how best to treat this population. We did not identify any randomized controlled trials that examined the efficacy of medication or psychological treatments to reduce pain or improve functioning in CNCP patients with comorbid SUD. The available data from seven treatment studies examining opioids and/or a multidisciplinary treatment approach suggests that, of patients who are adherent with treatment, SUD status is not associated with differences in treatment efficacy. Of note, studies generally did not compare results based on SUD status, none included a control group, and all were rated poor to fair in quality. Two additional studies examining the effectiveness of psychological interventions indicate that cognitive-behavioral therapy holds promise in treating pain-related function, and reducing the risk of relapse, for patients with CNCP and comorbid SUD [33,50].
Although there are limited data available describing treatment approaches for CNCP among patients with a history of SUD, clinical recommendations have been provided by experienced clinicians. Recommendations suggest that a comprehensive evaluation of all patients should be conducted that includes assessment of general psychological functioning, individual factors that contribute to patients’ reports of pain [26], and current and past substance use [23]. Additional recommendations suggest that monitoring of analgesia, activities of daily living, adverse events, and aberrant drug-related behaviors should be a focus of ongoing evaluations [18]. Emerging data indicate that CNCP patients with a history of SUD may need more intensive and ancillary treatment options than usual care in order to have long-term improvements in pain-related function [14]. Although the specific interventions may vary, it is recommended that CNCP patients with a history of SUD will be best served by a multidisciplinary team, including a specialist in addictions [9].
Standardized measures of medication misuse have been developed and may be administered regularly [22]. For patients who are at an elevated risk of medication misuse, it is recommended that treatment be adapted to be more intensive or to otherwise support safe and effective treatment. This may include modifying the type of setting, type of treatment, supply of opioids (frequency and quantity released), additional care (psychotherapy, recovery-oriented groups), and supervision (frequency of clinician visits, urine drug screen monitoring, pill counts) [22]. There are reports of interventions that have demonstrated effectiveness in reducing misuse of opioid medications. For example, an opioid renewal clinic, which includes specific treatment plans, more frequent visits, use of urine drug screens, and limited supplies of opioids, was effective in reducing aberrant medication use and maintaining pain management [66]. Additionally, a recent randomized trial found that treatment compliance monitoring and tailored behavioral interventions were efficacious in reducing misuse of opioid medications in patients who were at high risk for aberrant medication use at baseline [11]. However, the extent to which these interventions impact pain outcome remains uncertain.
We also examined differences in demographic and clinical variables among CNCP patients based on SUD status. A recent systematic review found that 11.5% of CNCP patients taking opioids develop aberrant medication-related behaviors [7]. For studies that preselected CNCP patients who had no history of abuse or addiction, 0.6% developed aberrant medication-related behaviors. However, this review did not compare rates of misuse based on SUD status. We found that patients with a history of SUD appear to be at greater risk for prescription medication misuse [38,56,59,62], but studies have been limited by their cross-sectional or retrospective design. No clear pattern of differences emerged on demographic, pain-related, or psychiatric variables based on SUD status. In terms of ongoing treatment, patients with a history of SUD appear to be more likely to be prescribed opioid medications, and at higher doses, than patients without a history of SUD [31,55,64], though the results are somewhat conflicting and may vary based on healthcare setting or medical comorbidity.
Our last key question related to predictors of treatment outcome among CNCP patients with a history of SUD. One study was available to address this issue, which found that being at high risk for prescription opioid misuse was associated with a decreased likelihood of improvement in pain control [34]. Prior research in other samples of CNCP patients has found that beliefs about pain [8], psychological factors such as somatization, depression or anxiety [4], self-efficacy [27], work status [1], and litigation [13] were all associated with treatment outcomes. These factors should be studied among patients with comorbid SUD to determine whether they predict treatment outcome for this group of patients as well.
This systematic review highlights the need for additional research in several areas for patients with CNCP and comorbid SUD. First, given the high rates of SUDs among samples of CNCP patients, it is strongly recommended that CNCP patients with a history of SUD not be excluded from randomized trials of chronic pain intervention studies. Including SUD patients in randomized trials will improve generalizability of results and help to provide empirical data regarding the efficacy of interventions for this population. Furthermore, we recommend that researchers utilize clear definitions of clinical constructs, valid and reliable assessment measures, and that studies be adequately powered to detect differences based on a priori hypotheses. A number of recommendations have been suggested regarding the use of psychometric instruments and convergent clinical constructs that should be included in chronic pain trials [6,25]. Utilizing well-validated outcome instruments, assessing more than one clinical domain, and increasing attention to attrition and potential confounding variables will help to improve the quality of research in this area.
Studies are needed that examine the prevalence of SUDs across different clinical settings (e.g., primary care, specialty pain, orthopedics and rehabilitation, emergency department). Although data indicate patients with a history of SUD are more likely to misuse prescription medications, prior studies are limited by their cross-sectional or retrospective design. Longitudinal studies are needed to clearly assess whether SUD status predicts future aberrant medication-related behaviors. Prospective cohort studies are also needed to evaluate differences in pain care, based on SUD status, and to assess treatment side effects and outcomes over time. Adequately powered randomized controlled trials are needed to examine the effectiveness of different interventions to treat chronic pain in this population. Interventions that may be evaluated include different classes of medications, such as NSAIDs and opioids, as well as cognitive-behavior therapy, which has preliminary support for treating CNCP in patients with comorbid SUD [33]. Furthermore, given the strong evidence indicating that multidisciplinary settings are the optimal method for providing care for CNCP [24], studies examining outcomes for SUD patients in pain clinics are recommended as well.
There are several limitations in research methodology that should be considered when reviewing the results of this systematic review. We limited our search to manuscripts published in peer-reviewed journals and in English language. Abstracts, non-published studies, and book chapters were not included. Our search strategy included studies that had substance use disorder or addiction as a keyword; there may be other studies available that included patients with a history of SUD that we did not identify. For example, studies that examined populations with high rates of SUDs may have not been included [e.g., 18], though the results may relate to this review. We did not exclude studies based on quality rating alone, which impacts the strength of our conclusions. However, we did review each cohort and treatment outcome study using a rigorously developed approach [10]. Many of the studies reviewed relied on the investigators ratings of patients’ aberrant behaviors, yet research suggests that observer determination underestimates the prevalence of abuse and misuse [29,48]. Future studies of aberrant medication-related behaviors should include objective measures, such as urine toxicology screening.
In summary, the results of this systematic review suggest that there are a large proportion of CNCP patients with a history of SUD. However, no consistent pattern of differences was evident when comparing CNCP patients with a history of SUD versus those without on demographic, pain, or psychiatric variables. Furthermore, little empirical data are available to guide clinicians in the most appropriate methods for treating chronic pain in this population. Research is clearly needed to improve our understanding of pain assessment and treatment approaches in patients with comorbid SUD.
Supplementary Material
Table 3.
Summary of Results.
| Key Question | Result | Quality of Evidence |
|---|---|---|
| 1. What is the prevalence of comorbid SUD in patients with CNCP? | The proportion of CNCP patients with current SUD ranged from 3% – 48%. Lifetime prevalence ranged from 16% – 74%. Results varied by clinical sample and methodology used to assess SUD. | |
| 2. How do patients with CNCP and comorbid SUD differ from CNCP patients without a history of SUD on demographic and clinical factors? | ||
| (a) Demographic variables | Mixed data regarding whether age, gender, or employment status is associated with a history of SUD. No differences found for race/ethnicity, marital status, or years of education | Very Low |
| (b) Pain variables | Contradictory results regarding whether CNCP patients differ on pain intensity or pain-related function based on SUD status. | Very Low |
| (c) Psychiatric variables | Some data suggests that pain patients with SUD report more depression, anxiety, and tobacco use; however, results were not replicated. | Very Low |
| (d) Prescription medication misuse | History of SUD is associated with current prescription medication misuse. | Moderate |
| 3. In what ways does pain treatment differ when comparing patients who have comorbid CNCP and SUD to CNCP patients who do not have SUD? | CNCP patients with SUD are more likely to be prescribed opioids and at higher doses, though the results may vary based on the healthcare system and/or medical comorbidity. | Low |
| 4. What is the efficacy of pain treatment in patients with CNCP and SUD? | ||
| (a) How effective are opioid medications in improving pain intensity and/or pain functioning in patients with CNCP and SUD? | Of patients that adhere to treatment, SUD patients do not differ in their response to treatment with opioids and/or a multidisciplinary pain team | Low |
| (b) How effective are non-opioid medications in improving pain intensity and/or pain functioning in patients with CNCP and SUD? | Non-opioid medications to treat CNCP in patients with comorbid SUD have not been tested. | No data available |
| (c) How effective are psychological interventions in improving pain intensity and/or pain functioning in patients with CNCP and SUD? | Cognitive-behavioral therapy has preliminary support for reducing pain and improving function in patients with comorbid SUD. | Very Low |
| 5. What patient factors are associated with improved pain intensity and/or pain functioning in patients with CNCP and SUD? | Baseline rating as being at risk for prescription opioid abuse is associated with a lower likelihood of improvement in pain control. | Very Low |
Note. CNCP = Chronic non-cancer pain. SUD = Substance use disorder. The overall quality of evidence for each key question was graded on a 4-point scale from “Very Low” to “High” [2].
Acknowledgments
This study was supported in part by award K23DA023467 from the National Institute on Drug Abuse to Dr. Morasco. During the past 12 months, Dr. Turk has received research support from Endo, Johnson & Johnson, Philips Respironics, and the National Institutes of Health, and consulting fees from Eli Lilly, Empi, Johnson & Johnson, Pfizer, Philips Respironics, and SK LifeScience. He is also a Special Government Employee of the U.S. Food and Drug Administration. No other author reports having any potential conflict of interest with this study. We appreciate the assistance of Mark Helfand, M.D., Devan Kansagara, M.D., and Roger Chou, M.D., for help in drafting or editing the key questions, Michele Freeman, M.P.H. for technical assistance, and research librarians Rose Campbell and Andrew Hamilton for developing the literature search strategies. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Department of Veterans Affairs, U.S. Food and Drug Administration, or another private entity.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anderson PA, Schwaegler PE, Cizek D, Leverson G. Work status as a predictor of surgical outcome of discogenic low back pain. Spine. 2006;31:2510–2515. doi: 10.1097/01.brs.0000239180.14933.b7. [DOI] [PubMed] [Google Scholar]
- 2.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW, Jr, Zaza S. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braden JB, Sullivan MD, Ray GT, Saunders K, Merrill J, Silverberg MJ, Rutter CM, Weisner C, Banta-Green C, Campbell C, Von Korff M. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31:564–570. doi: 10.1016/j.genhosppsych.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Celestin J, Edwards RR, Jamison RN. Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: a systematic review and literature synthesis. Pain Med. 2009;10:639–653. doi: 10.1111/j.1526-4637.2009.00632.x. [DOI] [PubMed] [Google Scholar]
- 5.Dobscha SK, Corson K, Flores JA, Tansill EC, Gerrity MS. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9:564–571. doi: 10.1111/j.1526-4637.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 6.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Fishbain DA, Cole B, Lewis J, Rosomoff HL, Rosomoff RS. What percentage of chronic nonmalignant pain patients exposed to chronic opioid analgesic therapy develop abuse/addiction and/or aberrant drug-related behaviors? A structured evidence-based review. Pain Med. 2008;9:444–459. doi: 10.1111/j.1526-4637.2007.00370.x. [DOI] [PubMed] [Google Scholar]
- 8.Galli U, Ettlin DA, Palla S, Ehlert U, Gaab J. Do illness perceptions predict pain-related disability and mood in chronic orofacial pain patients? A 6-month follow-up study. Eur J Pain. 2009 doi: 10.1016/j.ejpain.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: A rational approach to the treatment of chronic pain. Pain Med. 2005;6:107–112. doi: 10.1111/j.1526-4637.2005.05031.x. [DOI] [PubMed] [Google Scholar]
- 10.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20:21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 11.Jamison RN, Ross EL, Michna E, Chen LQ, Holcomb C, Wasan AD. Substance misuse treatment for high-risk chronic pain patients on opioid therapy: A randomized trial. Pain. doi: 10.1016/j.pain.2010.02.033. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz NP, Sherburne S, Beach M, Rose RJ, Vielguth J, Bradley J, Fanciullo GJ. Behavioral monitoring and urine toxicology testing in patients receiving long-term opioid therapy. Anesth Analg. 2003;97:1097–1102. doi: 10.1213/01.ANE.0000080159.83342.B5. [DOI] [PubMed] [Google Scholar]
- 13.LaCaille RA, DeBerard MS, Masters KS, Colledge AL, Bacon W. Presurgical biopsychosocial factors predict multidimensional patient: outcomes of interbody cage lumbar fusion. Spine J. 2005;5:71–78. doi: 10.1016/j.spinee.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Morasco BJ, Corson K, Turk DC, Dobscha SK. Association between substance use disorder status and pain-related function following 12 months of treatment in primary care patients with musculoskeletal pain. J Pain. doi: 10.1016/j.jpain.2010.07.010. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nedeljkovic SS, Wasan A, Jamison RN. Assessment of efficacy of long-term opioid therapy in pain patients with substance abuse potential. Clin J Pain. 2002;18:S39–51. doi: 10.1097/00002508-200207001-00005. [DOI] [PubMed] [Google Scholar]
- 16.Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35:214–228. doi: 10.1016/j.jpainsymman.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 17.Passik SD, Kirsh KL, Donaghy KB, Portenoy RK. Pain and aberrant drug-related behaviors in medically ill patients with and without histories of substance abuse. Clin J Pain. 2006;22:173–181. doi: 10.1097/01.ajp.0000161525.48245.aa. [DOI] [PubMed] [Google Scholar]
- 18.Passik SD, Kirsh KL, Whitcomb L, Portenoy RK, Katz NP, Kleinman L, Dodd SL, Schein JR. A new tool to assess and document pain outcomes in chronic pain patients receiving opioid therapy. Clin Ther. 2004;26:552–561. doi: 10.1016/s0149-2918(04)90057-4. [DOI] [PubMed] [Google Scholar]
- 19.Potter JS, Prather K, Weiss RD. Physical pain and associated clinical characteristics in treatment-seeking patients in four substance use disorder treatment modalities. Am J Addict. 2008;17:121–125. doi: 10.1080/10550490701862902. [DOI] [PubMed] [Google Scholar]
- 20.Pud D, Cohen D, Lawental E, Eisenberg E. Opioids and abnormal pain perception: New evidence from a study of chronic opioid addicts and healthy subjects. Drug Alcohol Depend. 2006;82:218–223. doi: 10.1016/j.drugalcdep.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 21.Rosenblum A, Joseph H, Fong C, Kipnis S, Cleland C, Portenoy RK. Prevalence and characteristics of chronic pain among chemically dependent patients in methadone maintenance and residential treatment facilities. JAMA. 2003;289:2370–2378. doi: 10.1001/jama.289.18.2370. [DOI] [PubMed] [Google Scholar]
- 22.Savage SR. Management of opioid medications in patients with chronic pain and risk of substance misuse. Curr Psychiatry Rep. 2009;11:377–384. doi: 10.1007/s11920-009-0057-2. [DOI] [PubMed] [Google Scholar]
- 23.Savage SR, Kirsh KL, Passik SD. Challenges in using opioids to treat pain in persons with substance use disorders. Addict Sci Clin Pract. 2008;4:4–25. doi: 10.1151/ascp08424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turk DC. Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin J Pain. 2002;18:355–365. doi: 10.1097/00002508-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB, Cleeland C, Dionne R, Farrar JT, Galer BS, Hewitt DJ, Jadad AR, Katz NP, Kramer LD, Manning DC, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robinson JP, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Witter J. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106:337–345. doi: 10.1016/j.pain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Turk DC, Okifuji A. Assessment of patients’ reporting of pain: An integrated perspective. Lancet. 1999;353:1784–1788. doi: 10.1016/S0140-6736(99)01309-4. [DOI] [PubMed] [Google Scholar]
- 27.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007;127:276–286. doi: 10.1016/j.pain.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21:652–655. doi: 10.1111/j.1525-1497.2006.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wasan AD, Butler SF, Budman SH, Benoit C, Fernandez K, Jamison RN. Psychiatric history and psychologic adjustment as risk factors for aberrant drug-related behavior among patients with chronic pain. Clin J Pain. 2007;23:307–315. doi: 10.1097/AJP.0b013e3180330dc5. [DOI] [PubMed] [Google Scholar]
- 30.Berndt S, Maier C, Schutz H-W. Polymedication and medication compliance in patients with chronic non-malignant pain. Pain. 1993;52:331–339. doi: 10.1016/0304-3959(93)90167-N. [DOI] [PubMed] [Google Scholar]
- 31.Breckenridge J, Clark J. Patient Characteristics Associated With Opioid Versus Nonsteroidal Anti-inflammatory Drug Management of Chronic Low Back Pain. J Pain. 2003;4:344–350. doi: 10.1016/s1526-5900(03)00638-2. [DOI] [PubMed] [Google Scholar]
- 32.Chelminski PR, Ives TJ, Felix KM, Prakken SD, Miller TM, Perhac JS, Malone RM, Bryant ME, DeWalt DA, Pignone MP. A primary care, multi-disciplinary disease management program for opioid-treated patients with chronic non-cancer pain and a high burden of psychiatric comorbidity. BMC Health Services Research. 2005;5:3. doi: 10.1186/1472-6963-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Currie SR, Hodgins DC, Crabtree A, Jacobi J, Armstrong S. Outcome from integrated pain management treatment for recovering substance abusers. J Pain. 2003;4:91–100. doi: 10.1054/jpai.2003.17. [DOI] [PubMed] [Google Scholar]
- 34.Dunbar SA, Katz NP. Chronic opioid therapy for nonmalignant pain in patients with a history of substance abuse: report of 20 cases. J Pain Symptom Manage. 1996;11:163–171. doi: 10.1016/0885-3924(95)00165-4. [DOI] [PubMed] [Google Scholar]
- 35.Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129:355–362. doi: 10.1016/j.pain.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 36.Fishbain DA, Cutler R, Rosomoff H, Rosomoff R. Validity of self-reported drug use in chronic pain patients. Clinical Journal of Pain. 1999;15:184–191. doi: 10.1097/00002508-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Fishbain DA, Goldberg M, Meagher BR, Steele R, Rosomoff H. Male and female chronic pain patients categorized by DSM-III psychiatric diagnostic criteria. Pain. 1986;26:181–197. doi: 10.1016/0304-3959(86)90074-6. [DOI] [PubMed] [Google Scholar]
- 38.Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain. 2007;8:573–582. doi: 10.1016/j.jpain.2007.02.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friedman R, Li V, Mehrotra D. Treating pain patients at risk: evaluation of a screening tool in opioid-treated pain patients with and without addiction. Pain Med. 2003;4:182–185. doi: 10.1046/j.1526-4637.2003.03017.x. [DOI] [PubMed] [Google Scholar]
- 40.Gorman DM, Potamianos G, Williams KA, Frank AO, Duffy SW, Peters TJ. Relationship between alcohol abuse and low back pain. Alcohol Alcoholism. 1987;22:61–63. [PubMed] [Google Scholar]
- 41.Hoffmann NG, Olofsson O, Salen B, Wickstrom L. Prevalence of abuse and dependency in chronic pain patients. Int J Addict. 1995;30:919–927. doi: 10.3109/10826089509055820. [DOI] [PubMed] [Google Scholar]
- 42.Hooten WM, Townsend CO, Bruce BK, Warner DO. The effects of smoking status on opioid tapering among patients with chronic pain. Anesth Analg. 2009;108:308–315. doi: 10.1213/ane.0b013e31818c7b99. [DOI] [PubMed] [Google Scholar]
- 43.Hoyt MJ, Nokes K, Newshan G, Staats JA, Thorn M. The effect of chemical dependency on pain perception in persons with AIDS. J Assoc Nurses AIDS Care. 1994;5:33–38. [PubMed] [Google Scholar]
- 44.Ives TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM, Shilliday BB, DeWalt DA, Pignone MP. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Services Research. 2006;6:46. doi: 10.1186/1472-6963-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnson KM, Bradley KA, Bush K, Gardella C, Dobie DJ, Laya MB. Frequency of mastalgia among women veterans: Association with psychiatric conditions and unexplained pain syndromes. Journal of General Internal Medicine. 2006;21:S70–S75. doi: 10.1111/j.1525-1497.2006.00378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaplan R, Slywka J, Slagle S, Ries K. A titrated morphine analgesic regimen comparing substance users and non-users with AIDS-related pain. J Pain Symptom Manage. 2000;19:265–273. doi: 10.1016/s0885-3924(00)00117-2. [DOI] [PubMed] [Google Scholar]
- 47.Katon W, Egan K, Miller D. Chronic pain: lifetime psychiatric diagnoses and family history. Am J Psychiatry. 1985;142:1156–1160. doi: 10.1176/ajp.142.10.1156. [DOI] [PubMed] [Google Scholar]
- 48.Katz NP, Sherburne S, Beach M, Rose RJ, Vielguth J, Bradley J, Fanciullo GJ. Behavioral monitoring and urine toxicology testing in patients receiving long-term opioid therapy. Anesth Analg. 2003;97:1097–1102. doi: 10.1213/01.ANE.0000080159.83342.B5. [DOI] [PubMed] [Google Scholar]
- 49.Kennedy JA, Crowley TJ. Chronic pain and substance abuse: a pilot study of opioid maintenance. J Subst Abuse Treat. 1990;7:233–238. doi: 10.1016/0740-5472(90)90046-s. [DOI] [PubMed] [Google Scholar]
- 50.Khatami M, Woody G, O’Brien C. Chronic pain and narcotic addiction: a multitherapeutic approach--a pilot study. Compr Psychiatry. 1979;20:55–60. doi: 10.1016/0010-440x(79)90059-2. [DOI] [PubMed] [Google Scholar]
- 51.Mahowald ML, Singh JA, Majeski P. Opioid use by patients in an orthopedics spine clinic. Arthritis Rheum. 2005;52:312–321. doi: 10.1002/art.20784. [DOI] [PubMed] [Google Scholar]
- 52.Manchikanti L, Damron KS, McManus CD, Barnhill RC. Patterns of illicit drug use and opioid abuse in patients with chronic pain at initial evaluation: a prospective, observational study. Pain Physician. 2004;7:431–437. [PubMed] [Google Scholar]
- 53.Manchikanti L, Giordano J, Boswell MV, Fellows B, Manchukonda R, Pampati V. Psychological factors as predictors of opioid abuse and illicit drug use in chronic pain patients. J Opioid Manag. 2007;3:89–100. doi: 10.5055/jom.2007.0045. [DOI] [PubMed] [Google Scholar]
- 54.Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, Fiellin DA. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 55.Massey GM, Dodds HN, Roberts CS, Servoss TJ, Blondell RD. Toxicology screening in orthopedic trauma patients predicting duration of prescription opioid use. J Addict Dis. 2005;24:31–41. doi: 10.1300/j069v24n04_03. [DOI] [PubMed] [Google Scholar]
- 56.Morasco BJ, Dobscha SK. Prescription medication misuse and substance use disorder in VA primary care patients with chronic pain. Gen Hosp Psychiatry. 2008;30:93–99. doi: 10.1016/j.genhosppsych.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 57.Newshan G, Lefkowitz M. Transdermal fentanyl for chronic pain in AIDS: A pilot study. J Pain Symptom Manage. 2001;21:69–77. doi: 10.1016/s0885-3924(00)00238-4. [DOI] [PubMed] [Google Scholar]
- 58.Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: Report of 38 cases. Pain. 1986;25:171–186. doi: 10.1016/0304-3959(86)90091-6. [DOI] [PubMed] [Google Scholar]
- 59.Reid M, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. Journal of General Internal Medicine. 2002;17:173–179. doi: 10.1046/j.1525-1497.2002.10435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rhodin A, Gronbladh L, Nilsson LH, Gordh T. Methadone treatment of chronic non-malignant pain and opioid dependence--a long-term follow-up. Eur J Pain. 2006;10:271–278. doi: 10.1016/j.ejpain.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 61.Sandstrom J, Andersson GB, Wallerstedt S. The role of alcohol abuse in working disability in patients with low back pain. Scand J Rehabil Med. 1984;16:147–149. [PubMed] [Google Scholar]
- 62.Schieffer BM, Pham Q, Labus J, Baria A, Van Vort W, Davis P, Davis F, Naliboff BD. Pain medication beliefs and medication misuse in chronic pain. J Pain. 2005;6:620–629. doi: 10.1016/j.jpain.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 63.Sheu R, Lussier D, Rosenblum A, Fong C, Portenoy J, Joseph H, Portenoy RK. Prevalence and characteristics of chronic pain in patients admitted to an outpatient drug and alcohol treatment program. Pain Med. 2008;9:911–917. doi: 10.1111/j.1526-4637.2008.00420.x. [DOI] [PubMed] [Google Scholar]
- 64.Weisner CM, Campbell CI, Ray GT, Saunders K, Merrill JO, Banta-Green C, Sullivan MD, Silverberg MJ, Mertens JR, Boudreau D, Von Korff M. Trends in prescribed opioid therapy for non-cancer pain for individuals with prior substance use disorders. Pain. 2009;145:287–293. doi: 10.1016/j.pain.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Whitehead AJ, Dobscha SK, Morasco BJ, Ruimy S, Bussell C, Hauser P. Pain, substance use disorders and opioid analgesic prescription patterns in veterans with hepatitis C. J Pain Symptom Manage. 2008;36:39–45. doi: 10.1016/j.jpainsymman.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 66.Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med. 2007;8:573–584. doi: 10.1111/j.1526-4637.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 67.Wilsey BL, Fishman SM, Tsodikov A, Ogden C, Symreng I, Ernst A. Psychological comorbidities predicting prescription opioid abuse among patients in chronic pain presenting to the emergency department. Pain Med. 2008;9:1107–1117. doi: 10.1111/j.1526-4637.2007.00401.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.