Abstract
Purpose
To report the effectiveness of a prenatal intervention and to provide evidence that prenatal visits provide an opportune time for health assessment and counseling with abused women.
Methods
Fifty ethnically diverse pregnant women who presented for routine prenatal care and who also reported being at risk for intimate partner violence (IPV) were recruited to the study. Participants were assigned to either usual care or the Video Doctor plus Provider Cueing intervention. At baseline and 1-month later at another routine prenatal visit, intervention group participants received a 15-minute Video Doctor assessment and interactive tailored counseling. Their providers received a printed Cue Sheet alert and suggested counseling statements.
Main findings
Participants in the intervention group were significantly more likely to report provider-patient discussions of IPV compared to participants receiving usual care at baseline (81.8% vs. 16.7%, p < 0.001) and at the 1-month follow-up (70.0% vs. 23.5%, p = 0.005). Summing the number of patient-provider discussions across the two visits at baseline and one month later, intervention participants were significantly more likely to have IPV risk discussion with their providers at one or both visits (90.0% vs. 23.6%, p< 0.001) compared to the participants who received usual care. When specifically asked about the helpfulness of these IPV-related discussions, 20 out of 22 (90.9%) participants rated the discussion as helpful or very helpful at baseline and all 18 (100%) participants rated the discussion as helpful or very helpful at the 1-month follow-up.
Conclusions
Video Doctor plus Provider Cueing intervention significantly increases the likelihood of provider-patient IPV discussion with pregnant women with a history of abuse.
Introduction and Background
Intimate partner violence (IPV) is a significant public health threat that disproportionately affects women (Breiding, Black, & Ryan, 2008). The Centers for Disease Control and Prevention (CDC) (Saltzman, Fanslow, McMahon, & Shelley, 1999; Saltzman, Fanslow, McMahon, & Shelley, 2002) definition for IPV can be summarized as follows: IPV refers to physical or sexual violence or the threat of such violence; or psychological/emotional abuse and/or coercive tactics when there has been prior physical and/or sexual violence between persons who are partners or former partners. In North American population-based surveys, the lifetime prevalence of IPV ranged from 10% to 44%, between 7% and 25% of women reported physical assault in the previous year (Breiding et al., 2008; Thompson et al., 2006). IPV can occur in all kinds of intimate relationships, including marriage, committed same-sex or opposite-sex relationships, and dating relationships of adults and adolescents; IPV most often is committed by men against women (Briere, 1992).
IPV is a common threat to the health and well being of pregnant women. In a large review of studies in the United States, Gazmararian and colleagues (Gazmararian et al., 2000) found that the incidence of IPV during pregnancy ranged between 0.9% to 20%, with most estimates between 4% and 8%; these figures translate into approximately 156,000 to 332,000 pregnant women who experience IPV each year. In fact, IPV is more common in pregnancy than placenta previa, gestational diabetes, or pregnancy-induced hypertension (Gazmararian et al., 2000).
IPV during pregnancy has been linked in studies with poor maternal weight gain and anemia, bleeding, placental abruption, uterine rupture, chorioamnionitis, vaginal infections, and kidney infection (Berenson, Wiemann, Wilkinson, Jones, & Anderson, 1994; Cokkinides, Coker, Sanderson, Addy, & Bethea, 1999; Curry, Perrin, & Wall, 1998; El Kady, Gilbert, Xing, & Smith, 2005; El Kady, 2007; Greenberg, McFarlane, & Watson, 1997; McFarlane, Parker, & Soeken, 1996). In a systematic review and meta-analysis of eight studies, Murphy et al. (Murphy, Schei, Myhr, & Du Mont, 2001) concluded that women reporting IPV had 1.4 times greater odds of giving birth to a low birth weight infant than nonabused women [95% CI 1.1– 1.8].
Leading healthcare organizations have recommended that pregnant women be routinely screened for IPV (American College of Obstetricians and Gynecologists, 1995), and that health professionals be educated about how to respond to IPV and other forms of family violence (Institute of Medicine, 2002). Pregnancy provides an opportune time to assess and engage in risk-reduction efforts in health care settings with women for several reasons: 1) the vast majority of pregnant women, even those who do not routinely have access to care at other times, receive prenatal care (National Center for Health Statistics, 1999; Ventura, Martin, Curtin, & Mathews, 1999); 2) many pregnant women are particularly motivated to change their behavior as part of taking on the maternal role (Mercer, 2004) and in order to protect their unborn baby and their other children (Higgins, Clough, Frank, & Wallerstedt, 1995); and 3) repeated prenatal appointments offer the opportunity to develop a trusting relationship with a health care provider, which can facilitate increased willingness to disclose risky behaviors and to heed risk-reduction messages. For IPV, pregnancy is an especially opportune time for providers to intervene because, for many women living in the isolation often imposed by an abusive partner, prenatal appointments may be the only time they can speak to a concerned professional in the absence of their partners (Herzig et al., 2006). In fact, studies have reported that the proportion of women disclosing IPV increases over the duration of pregnancy, underscoring the benefit of routine assessment at every prenatal visit (Gazmararian et al., 2000).
Despite the importance of, and opportunities for, assessment and intervention with prenatal behavioral risks, evidence exists that many physicians and other prenatal health care providers do not routinely assess for IPV. Petersen and colleagues' (Petersen, Connelly, Martin, & Kupper, 2001) analysis of the multi-state, population-based Pregnancy Risk Assessment Monitoring System (PRAMS) data found that while pregnant women usually reported having received some level of counseling from a health care professional about smoking and alcohol, relatively few reported any assessment or counseling about other risks, including IPV. This was true for women with and without these risks.
Other surveys confirm that few physicians assess pregnant women for IPV. One study in Alaska, a state with high rates of IPV, found that only 27% of physicians often or always assessed pregnant women for abuse at their first prenatal visit, and only 7% often or always screened at any subsequent prenatal visits (Chamberlain & Perham-Hester, 2000). Two surveys of California physicians reported that only 11% and 13% respectively routinely assessed primary care patients for IPV (Gerbert et al., 2002; Rodriguez, Bauer, McLoughlin, & Grumbach, 1999).
A substantial body of literature has documented barriers to assessment and counseling for IPV. Physician barriers to assessment of and intervening with IPV are well researched and include lack of time and support resources, lack of education and training, fear of offending the patient, inability to “fix it,” patients not disclosing, and frustration with lack of change in the patient's situation or the patient's unresponsiveness to advice (Ferris, 1994; Gerbert, Caspers, Bronstone, Moe, & Abercrombie, 1999; McGrath et al., 1997; Sugg & Inui, 1992). Mandatory reporting laws for health care providers in some states further complicate assessment for IPV and contribute to providers' reluctance to approach the topic. Providers are concerned that reporting to law enforcement officials could violate the patient's wishes or her safety (Rodriguez, Quiroga, & Bauer, 1996; Salber, 1997). Patients report that they do not disclose abuse to health care professionals because of fear of their partner's retaliation, shame, humiliation, denial about the seriousness of the abuse, and concern over confidentiality, including the possibility of reporting to authorities (Gerbert et al., 1996; Martins, Holzapfel, & Baker, 1992; Rodriguez et al., 1996).
The purpose of this paper is to report on the effectiveness of a prenatal patient and provider-focused intervention to increase discussions about IPV at 1-month follow-up and to provide evidence in support for our position that prenatal visits provide an opportune time for health assessment and counseling with abused women.
Methods
This study is part of the Health in Pregnancy (HIP) Study, a randomized, controlled trial to determine if a brief, interactive, multimedia intervention for pregnant women can reduce their risks related to IPV, smoking, alcohol, and illicit drug use. The current report focuses on the HIP program IPV intervention and its impact on patient-provider discussions of IPV at two consecutive monthly prenatal routine visits for the 50 participants who reported ever experiencing IPV. In a prior publication, we reported baseline data from the first 37 of these participants who self-reported IPV risk at the baseline assessment (Calderon, Gilbert, Jackson, Kohn, & Gerbert, 2008). In addition, 14 of these participants who reported both IPV risk and tobacco use at baseline were included in another publication that reported the impact of the Video Doctor plus Provider Cueing intervention for smoking-related advice and smoking outcomes (Tsoh, Kohn, & Gerbert, 2010). This paper provides a full report of the entire study sample who reported IPV and includes additional participants and new longitudinal data collected across two consecutive prenatal routine visits at baseline and 1-month follow-up.
Procedures
Details of the HIP study and recruitment have been previously reported (Calderon et al., 2008). HIP was launched in five prenatal clinics in the San Francisco Bay Area in June 2006. Participant recruitment was completed in December 2007. Participants were English-speaking women 18 years or older who were less than 26-weeks pregnant, receiving prenatal care at one of the participating clinics, and not presenting for their first prenatal visit. Prior to a regularly scheduled prenatal appointment, participants completed a risk assessment using a digitized pen on an IBM touch screen laptop computer via a low-literacy computerized interview with audio voiceover (i.e., Video Doctor). The computer program collected socio-demographic information and pregnancy history, and assessed for tobacco, alcohol, drug use, and IPV. Women reporting risks were stratified by risk combination and randomly assigned by the computer to intervention or usual care groups. All participants were reassessed using a similar computerized interview at 1-month following the initial (baseline) assessment. At both baseline and 1-month assessments, participants also completed a brief post-visit interview with a research assistant to report whether IPV or other reported behavioral risks had been discussed with their provider. All participants received a gift card to a grocery or department store as compensation for completing an assessment in the amounts of $30 at baseline, and $40 at 1-month follow-up. Study procedures were approved by the University of [blinded by WHI editors] and the institutional review boards responsible for each site. In each location on the day of the baseline visit, we used a private room adjacent to the waiting room to formally obtain consent. Written informed consent was obtained from all participants prior to implementation of any study procedures.
To recruit providers, we first contacted the attending or department/division chair of the clinic who was also designated the site PI. With his or her help and as part of the informed consent process for providers, we gave a brief overview of the project and showed an example of a cue sheet that did not include content on IPV to clinic providers at a regularly scheduled meeting. Written consent was obtained from all providers. All providers were physicians; some were residents.
Intervention group
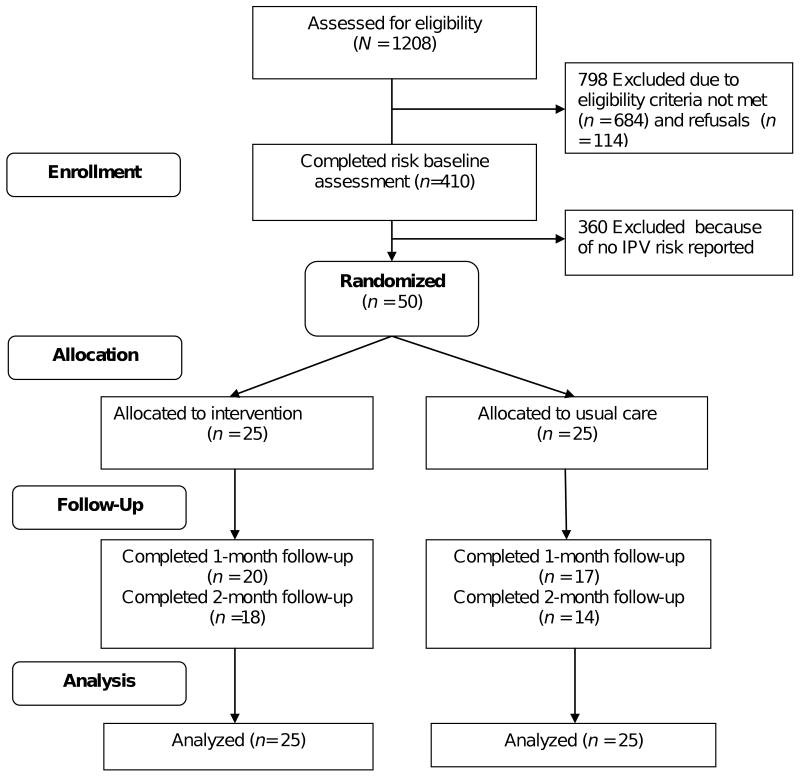
Participants assigned to the intervention group received the Video Doctor plus Provider Cueing intervention. The Video Doctor model was selected by the Centers for Disease Control and Prevention in 2008 as one of the best evidence-based practices in reducing HIV risks (Kuehn, 2008). The Video Doctor is a multimedia interactive intervention delivered on a laptop computer via a secure internet connection. An actor-portrayed Video Doctor delivered interactive risk-reduction messages, designed to simulate an ideal discussion with a prenatal health care provider who provided non-judgmental counseling following key principles of Motivational Interviewing (Rollnick & Miller, 1995; Rollnick & Miller, 2008). Using a library of digital video clips, extensive branching logic, and participant input, the program tailored messages to the participant's risk profile and intention to change. In addition, at the end of the participant's session, the Video Doctor closes with the following statements: “I suggest that you speak with your doctor about your relationship today. Talking about abuse isn't easy, but it can help.” The program also automatically printed two documents: 1) a Cueing Sheet for providers, which offered a summary of the patient's risk profile and suggested risk-reduction counseling statements, and 2) an Educational Worksheet for participants with questions for self-reflection, harm reduction tips, and local resources. The Cueing Sheet was placed in the patient's medical record for the provider's use during the prenatal appointment. All providers received a brief orientation to the use of the Cueing Sheets, but received no training in IPV assessment or counseling. Figure 1 shows a graphical illustration of the intervention components.
Figure 1.
Intervention Components of the Video Doctor Plus Provider Cueing
Usual care group
Participants in the usual care group did not interact with the Video Doctor and the program did not produce a Cueing Sheet or Educational Worksheet. Following completion of the computer-based assessment, participants assigned to the usual care group proceeded to their prenatal appointment and received the clinic's usual care. Behavioral counseling for the usual care group was determined solely by the provider without the benefit of cueing of any kind.
Measures
Background characteristics
As part of the computerized baseline assessment, these demographic variables were assessed: age, race/ethnicity, educational attainment, marital status, and self-reported height and weight for computation of body mass index. Pregnancy history and status variables included whether participants were previously pregnant, and gestational weeks and months into pregnancy at the time of their first prenatal visit were also obtained at baseline. Behavior risk profiles for IPV (Petersen et al., 2001), alcohol, illicit drug use, and tobacco (Survey Research Group, Cancer Surveillance and Research Branch, 2009) use were assessed using items taken from validated scales. Participants were coded to have IPV risk if they reported having ever been pushed, shoved, hit, kicked, or otherwise physically hurt (physical violence) or ever been forced to have sexual activities (sexual violence) from a partner or someone important to them.
IPV specific measures
At baseline, participants who screened positive for IPV risk were asked additional IPV-related items. Assessment of recent physical or sexual violence was conducted using an adapted version of the Abuse Assessment Screen (McFarlane, Parker, Soeken, & Bullock, 1992). The items on this measure inquired about prevalence and frequency of physical and sexual violence in the year before the pregnancy, and the interval since the pregnancy began. Participants who reported recent IPV experience were asked to indicate their relationship to the abuser. Those who reported recent physical violence were further asked to indicate the most severe event experienced in the year prior to pregnancy and since pregnancy selecting from one of the following descriptive categories: i) threats of abuse; ii) slapping, pushing; no injuries or lasting pain; iii) punching, kicking, bruises, cuts, and/or continuing pain; iv) beaten up, severe contusions, burns, broken bones; v) head, internal, and/or permanent injury; vi) use of weapon or wound from weapon.
The intention to make changes regarding IPV was assessed at baseline by asking participants if they were seriously thinking of making a change and if so, did they expect to make that change within the next 30 days or 6 months.
Outcome measures
The outcome measures for the study included the occurrence of patient-provider discussion of IPV risk and participants' perceived helpfulness of the discussion. During each post visit interview at baseline and 1-month follow-up, participants were asked “Did you talk about domestic violence with your doctor today?” An affirmative response to this question was used to indicate that a patient-provider discussion of IPV took place. If a participant indicated that a patient-provider discussion of IPV occurred, she was then asked “Would you say that the discussion with your doctor was helpful or not?” and to rate the helpfulness of the discussion using a 4-point scale from “very helpful” to “not helpful at all”. The determination of whether or not a patient-provider discussion of IPV occurred and the degree of helpfulness were assessed at baseline and at the 1-month follow-up. The total number of discussions was computed by summing the occurrence of discussion at two time points.
Data analyses
We compared intervention and usual care groups on baseline sample characteristics using the t test for continuous variables, Pearson's chi-square for categorical variables, and Fisher's Exact Test for dichotomous variables with any cell size < 5. For the outcome variables, we used Pearson's chi-square tests to compare the occurrence of patient-provider discussion of IPV risks (yes vs. no) at each time point, and perceived helpfulness of the discussions (coded as helpful vs. not helpful) between the two groups. The Wilcoxon rank-sum test was used to compare the two groups for discrete count variables such as the total number of discussions of IPV risks across two time points. We assessed the sensitivity of the results to losses to follow-up by making the assumption that in the absence of outcome data, no discussion occurred.
Results
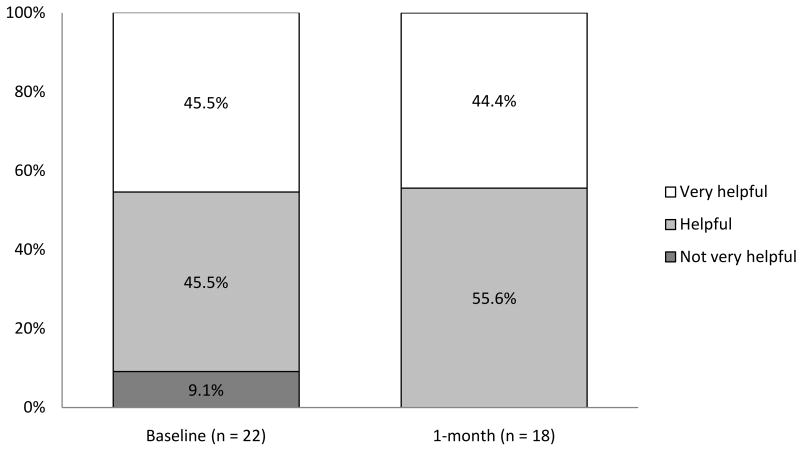
Of 410 eligible pregnant women who completed baseline risk assessments, 50 (12.2%) reported ever experiencing IPV in the form of physical and/or sexual violence from a partner or someone important to them. All 50 women with IPV risk were randomized (Figure 2).
Figure 2.
Flowchart of study participants
The baselines characteristics for the abused women in the intervention and usual care groups are summarized in Table 1. The total sample (N = 50) was ethnically diverse consisting of 34% Latino, 22% Black, 30% White, and 14% of other or multiple races. The mean age was 27.7 (SD = 7.1; range = 18 to 43 years old). At the time of their participation, one-third (38%) of the sample was married or in a domestic partnership; 40% had education beyond high school. A majority (76.0%) had previous pregnancies. The average gestational age was 20.5 weeks (SD = 4.9; range = 8 to 26 weeks) and on average participants had their first prenatal visit 2.3 months into their pregnancy (range = 1 to 5 months). Seventy percent (n = 35) of the sample screened positive for IPV risk only. Current tobacco use was the most common concurrent behavioral risk (28%). Very few participants reported using alcohol (2%) or illicit drugs (6%). Sixty-four percent (n = 32) of the participants reported the intention to make changes regarding IPV within the 30 days to 6 months. Participants in the intervention (N = 25) and usual care groups (N = 25) were similar in demographics, pregnancy history, and risk profiles (p > 0.05). The two groups differed significantly only on their intention to make changes regarding IPV with the intervention group reporting that they were less likely to make changes compared with the women in the usual care group.
Table 1. Baseline characteristics of abused women study participants.
| All (N = 50) | Intervention (n = 25) | Usual Care (n = 25) | p value* | |
|---|---|---|---|---|
| Age, mean (SD) | 27.7 (7.1) | 29.1 (6.8) | 26.4 (7.3) | 0.18 |
| Race/ethnicity, f (%) | ||||
| Hispanic/Latino | 17 (34.0) | 9 (32.0) | 9 (36.0) | 0.28 |
| Black or African-American | 11 (22.0) | 7 (28.0) | 4 (16.0) | |
| White | 15 (30.0) | 5 (20.0) | 10 (40.0) | |
| Other or multiple races | 7 (14.0) | 5 (20.0) | 2 (8.0) | |
| Marital status, f (%) | ||||
| Never married | 23 (46.0) | 10 (40.0) | 13 (52.0) | 0.65 |
| Currently married | 19 (38.0) | 11 (44.0) | 8 (32.0) | |
| Formerly married | 8 (16.0) | 4 (16.0) | 4 (16.0) | |
| Educational attainment, f (%) | ||||
| Less than high school diploma | 11 (22.0) | 7 (28.0) | 4 (16.0) | 0.80 |
| High school diploma or GED | 18 (36.0) | 8 (32.0) | 10 (40.0) | |
| Some College | 14 (28.0) | 7 (28.0) | 7 (28.0) | |
| College Degree | 5 (12.0) | 3 (12.0) | 3 (12.0) | |
| Missing | 1 (2.0) | 0 (0.0) | 1 (4.0) | |
| Pregnancy history, f (%) | ||||
| Previously pregnant | 38 (76.0) | 21 (84.0) | 17 (68.0) | 0.19 |
| Gestational weeks, mean (SD) | 20.5 (4.9) | 19.6 (4.4) | 21.4 (5.3) | 0.19 |
| First prenatal visit (months pregnant), mean (SD) | 2.3 (1.1) | 2.4 (0.9) | 2.4 (1.2) | 0.51 |
| Risk profile,a f (%) | ||||
| IPV only with no other risks | 35 (70.0) | 17 (68.02) | 18 (72.0) | 0.83 |
| Alcohol use in past 30 days | 1 (2.0) | 1 (4.0) | 0 (4.0) | 1.00 |
| Illicit drug use in past 30 days | 3 (6.0) | 2 (8.0) | 1 (4.0) | 1.00 |
| Tobacco use in past 30 days | 14 (28.0) | 7 (28.0) | 7 (28.0) | 1.00 |
| Intention to make changes regarding IPV, f (%) | ||||
| within the next 30 days | 24 (48.0) | 13 (52.0) | 11 (44.0) | 0.047 |
| within the next 6 months | 8 (16.0) | 1 (4.0) | 7 (28.0) | |
| no intention to change | 17 (34.0) | 11 (44.0) | 6 (24.0) | |
| Missing | 1 (2.0) | 0 (0.0) | 1 (4.0) |
Notes: GED, general educational development test; SD, standard deviation; IPV, intimate partner violence
Percentages may not add up to 100% because of round up errors
Categories are not mutually exclusive
p-values of comparisons of non-missing observations between Intervention and Usual Care groups. Fisher's Exact Test was used instead of Pearson chi-square test when sample size of any cell is < 5.
Table 2 summarizes the physical violence experiences of the sample. While all of the study participants had a history of IPV, 86% reporting physical violence in the year prior to pregnancy, with half (50%) of the sample reported experiencing IPV episodes at least four times during that time period. Since pregnancy, 38% reported physical violence, with 14% of the sample reporting experiencing violence 4 or more times since becoming pregnant. Among those who experienced physical violence during the year prior to pregnancy or since the pregnancy, slapping, pushing, punching, kicking, bruises, or cuts were the most severe events reported. There was no significant difference in the violence experiences reported between the two groups. Sexual violence experiences (not reported in Table 2) were less common and occurred with similar frequency in both the intervention and usual care groups. Only 34% (n = 17) of the sample reported ever experiencing sexual violence and 20% (n = 10) and 8% (n = 4) reported having experienced sexual violence in the year before, and since pregnancy, respectively. Among those who recently experienced sexual violence, 6 out of 10 (60%) and 2 out of the 4 (50%) participants reported experiencing sexual violence at least 4 times in the year prior to pregnancy and since pregnancy, respectively.
Table 2. Physical violence experience reported by abused women study participants.
| All N (%) | Intervention n (%) | Usual Care n (%) | p-value* | |
|---|---|---|---|---|
| Prevalence | ||||
| ever from a partner/someone important | 50 (100) | 25 (100) | 25 (100) | 1.00 |
| in the year prior to pregnancy | 43 (86.0) | 23 (92.5) | 20 (80.0) | 0.22 |
| since pregnancy | 19 (38.0) | 7 (28.0) | 12 (48.0) | 0.15 |
| Frequencies | ||||
| in the year prior to pregnancy | (n = 50) | (n = 25) | (n = 25) | |
| None | 7 (14.0) | 2 (8.0) | 5 (20.0) | 0.66 |
| 1-3 times | 18 (36.0) | 10 (40.0) | 8 (32.0) | |
| 4-6 times | 14 (28.0) | 7 (28.0) | 7 (28.0) | |
| >6 times | 11 (22.0) | 6 (24.0) | 5 (20.0) | |
| since pregnancy | (n = 50) | (n = 25) | (n = 25) | |
| None | 31 (62.0) | 18 (72.0) | 13 (52.0) | 0.37 |
| 1-3 times | 12 (24.0) | 5 (20.0) | 7 (28.0) | |
| 4-6 times | 4 (8.0) | 1 (4.0) | 3 (12.0) | |
| >6 times | 1 (2.0) | 0 (0.0) | 1 (4.0) | |
| Missing | 2 (4.0) | 1 (4.0) | 1 (4.0) | |
| Types of most severe eventsa | ||||
| in the year prior to pregnancy | (n = 43) | (n = 23) | (n = 20) | |
| Threats of abuse | 7 (16.3) | 4 (17.4) | 3 (15.0) | 0.83 |
| Slapping, pushing; no injuries or lasting pain | 21 (48.8) | 10 (43.5) | 11 (55.0) | 0.45 |
| Punching, kicking, bruises, cuts, and/or continuing pain | 15 (34.9) | 8 (34.8) | 7 (35.0) | 0.99 |
| Beaten up, severe contusions, burns, broken bones | 2 (4.7) | 2 (8.7) | 0 (0.0) | 0.49 |
| Head, internal, and/or permanent injury | 1 (2.3) | 0 (0.0) | 1 (5.0) | 0.46 |
| Use of weapon; wound from weapon | 1 (2.3) | 1 (4.0) | 0 (0.0) | 1.00 |
| Missing | 1 (2.3) | 0 (0.0) | 1 (5.0) | 0.47 |
| since pregnancy | (n = 19) | (n = 7) | (n = 12) | |
| Threats of abuse | 3 (15.8) | 1 (14.3) | 2 (16.7) | 1.00 |
| Slapping, pushing; no injuries or lasting pain | 7 (36.8) | 1 (14.3) | 6 (50.0) | 0.17 |
| Punching, kicking, bruises, cuts, and/or continuing pain | 7 (36.8) | 4 (57.1) | 3 (25.0) | 0.33 |
| Beaten up, severe contusions, burns, broken bones | 0 (0.0) | 0 (0.0) | 0 (0.0) | ** |
| Head, internal, and/or permanent injury | 0 (0.0) | 0 (0.0) | 0 (0.0) | ** |
| Use of weapon; wound from weapon | 0 (0.0) | 0 (0.0) | 0 (0.0) | ** |
| Missing | 2 (10.5) | 1 (14.3) | 1 (8.3) | 1.00 |
Notes: Physical violence is defined as having been pushed, shoved, hit, kicked, or otherwise physically hurt by someone including a partner or someone important.
The most severe type of events experienced in at least one of the abuser relationship groups; categories are not mutually exclusive, more than one category may be selected.
P-values of comparisons of non-missing observations between Intervention and Usual Care groups. Fisher's Exact Test was used instead of Pearson chi-square test when sample size of any cell is < 5.
No p value due to null response.
Patient-provider discussion of IPV
Complete data about patient-provider discussions were collected from 46 (92%) participants at baseline and 37 (74%) participants at the 1-month follow-up. There was no statistical difference in data completion rates at 1- month follow-up between the two treatment groups (p = 0.33). Table 3 presents the outcomes of patient-provider discussion of IPV at each time point and the sum across two time points (baseline and 1-month follow-up). Consistent with the previous report (N = 37) (Calderon et al., 2008) and in the current report (N = 50), at baseline, significantly more intervention participants had a discussion of IPV with their providers at the prenatal visit than those in usual care (81.8% vs 16.7%, p < 0.001). Our follow-up data now show that at the 1-month follow-up, significantly more intervention participants, when compared to those in usual care, reported having a discussion of IPV risk with their prenatal providers (70.0% vs. 23.5%, p = 0.008). Summing the number of patient-provider discussion across the two visits at baseline and 1-month, 90% of the intervention participants had IPV risk discussion with their providers at one or both visits as compared to only 23.6% of the participants who received usual care (p< 0.001). Similar differences were obtained in a sensitivity analysis that imputed missing data as the absence of patient-provider discussion of IPV at each time point or across the two assessments (Table 3).
Table 3. IPV discussion by group (intervention vs. usual care).
| Observed a | Sensitivity Analysis b | |||||
|---|---|---|---|---|---|---|
| Intervention | Usual Care | p-value | Intervention | Usual Care | p-value | |
| Occurrence of IPV Discussion at each time point (Yes) | ||||||
| (n = 22) | (n = 24) | (n = 25) | (n = 25) | |||
| At Baseline | 18 (81.8%) | 4 (16.7%) | <0.001c | 18 (72.0%) | 4 (16.0%) | <0.001c |
| (n = 20) | (n = 17) | (n = 25) | (n = 25) | |||
| At 1-month Follow-up | 14 (70.0%) | 4 (23.5%) | 0.008c | 14 (56.0%) | 4 (16.0%) | 0.007 c |
| Total Number of IPV Discussions Occurred with provider on IPV across two time points | ||||||
| (n = 20) | (n = 17) | <0.001d | (n = 25) | (n = 25) | <0.001d | |
| 0 (no discussion at either visits) | 2 (10.0%) | 13 (76.5%) | 5 (20.0%) | 19 (76.0%) | ||
| 1 (discussion at one of the 2 visits) | 6 (30.0) | 2 (11.8%) | 8 (32.0%) | 4 (16.0%) | ||
| 2 (discussion at both visits) | 12 (60.0%) | 2 (11.8%) | 12 (48.0%) | 2 (8.0%) | ||
Observed rates were computed based on participants who provided data.
Rates calculated with missing data imputed as no advice or no abstinence correspondingly.
Fisher's exact test
Wilcoxon rank-sum test
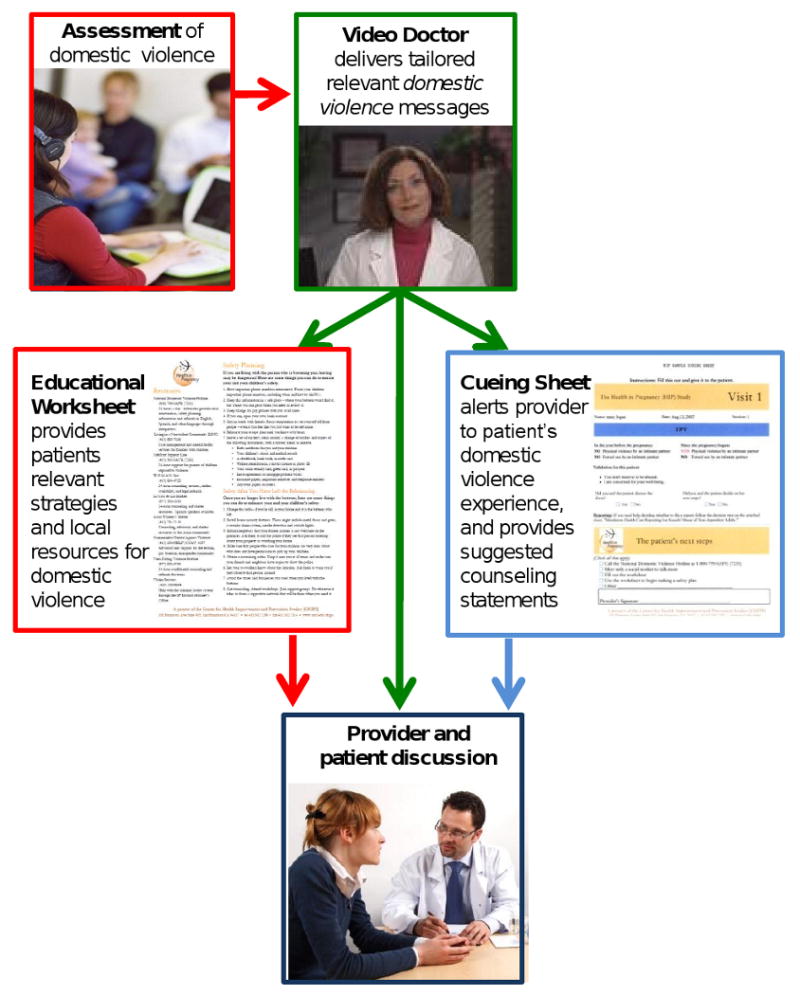
Helpfulness of IPV discussions
Helpfulness ratings were obtained from all participants (100%) who provided data about patient-provider discussions at each assessment. At baseline, 20 out of 22 (90.9%) participants who reported discussing IPV risk with their providers rated the discussion as helpful or very helpful. At the 1-month follow-up, all 18 (100%) participants who had a discussion of IPV risk with their prenatal providers rated the discussion as helpful or very helpful. There was no significant difference in helpfulness ratings between the two time points; baseline and 1-month follow-up (p > 0.05). Figure 3 shows the perceived helpfulness ratings of the IPV discussions at each time point for all participants combined from the two groups.
Figure 3.
Perceived helpfulness of provider discussion on IPV by time point
Discussion
The results of our study show that Video Doctor plus Provider Cueing significantly increases health care provider-patient IPV discussion with pregnant women with a history of abuse. Moreover, these increases in patient-provider discussions continued to occur over a 1-month time period. In fact, in this sample of ethnically diverse women, 90% of the participants in the intervention group had a discussion at least once compared with only 23.5% of the participants in the usual care group.
We do not know who actually initiated the provider-patient IPV discussion, but we hypothesize that the Video Doctor plus Provider Cueing approach increases these discussions through three possible means. First, the actor-portrayed Video Doctor interactive risk-reduction message introduces the topic of IPV to intervention group participants. Gerbert and colleagues (Gerbert et al., 2000; Gerbert et al., 2002) suggested that just asking equals success. Next the Video Doctor suggests “Speak with your doctor about your relationship today”. It is possible that this recommendation to discuss IPV with the health care provider encourages or empowers women to bring up the issue. Finally, the Provider Cueing sheets with recommended statements may give impetus to providers who would not necessarily raise the issue of IPV. Regardless of the means, our data provide support for the benefits of a seamless manner of assessment of IPV at routine prenatal visits. The ability to increase and sustain provider IPV assessment and counseling at routine prenatal visits is particularly important for reasons described in the introduction.
The vast majority of pregnant women receive prenatal care (National Center for Health Statistics, 1999; Ventura et al., 1999). In addition, there is evidence that abuse during pregnancy is a red flag for a particularly dangerous abuser and, thus, highlights the importance of assessment during pregnancy. Furthermore, repeated prenatal appointments offer the opportunity to develop a trusting relationship with providers (Herzig et al., 2006). Finally, many pregnant women are particularly motivated to make changes as part of taking on the maternal role and in order to protect their unborn baby and their other children (Higgins et al., 1995).
In addition to increasing discussions of IPV, in our study more than 90% of the women who had an IPV discussion with their provider at baseline and 100% of the women who had such a discussion at the 1-month follow-up reported that it was helpful. These findings must be considered in light of the fact that provider IPV training was not part of our study. Indeed, the provider Cue Sheet only listed a few recommended statements. Providers were under no obligation to use the statements nor were they trained in IPV assessment or counseling as part of our study. As noted, the IOM (Institute of Medicine, 2002) has already reported that educational preparation is often minimal. We are in full agreement with the IOM that all healthcare providers would greatly benefit from additional didactic and experiential education around IPV. Our findings show, however, that whether providers had limited or vast amounts of IPV educational preparation, the Video Doctor plus Provider Cueing provided a seamless, effective, and sustained way of increasing patient-provider discussions of IPV that was viewed as helpful by the vast majority of the participants.
There are, however, limitations to this study. All study measures were self-report and were not confirmed by independent assessment. It is most likely that IPV was thus underreported. In addition, follow-up occurred at only one point in time, 1 month after the initial assessment. Patients were not randomized within each provider. It is possible that there were individual differences among providers that might have come to light if they could have been tracked and patients clustered accordingly. As is typical of the academic health centers, however, multiple providers, including residents, provide prenatal care to the participants in our study and thus it was not possible to analyze the data clustered by provider. Future studies may wish to consider such an approach. Furthermore, because we did not attempt to educate providers about IPV or motivational interviewing or videotape and code the visits, we do not know what actually transpired during the patient-provider discussion beyond the participants' report that discussion of domestic violence did or did not occur. Further research is needed to determine the relative effectiveness of different IPV content and means of delivery. Finally, we have no data on any changes in IPV exposure that may have occurred during or following the study. Future studies should address each of these limitations. Nevertheless, our study provides compelling evidence that prenatal provider and patient-focused intervention seamlessly integrated into routine prenatal care can significantly increase IPV-related provider-patient discussion. Furthermore, in our sample, IPV discussions of any kind were viewed as helpful by our ethnically diverse sample of women with recent histories of abuse.
Conclusions
The results of our randomized controlled trial provide empirical evidence for the benefits and sustained effects (1 month) of a brief, interactive, multimedia intervention in enhancing provider-patient discussions with pregnant women at risk for IPV. Given the well documented barriers to IPV assessment and counseling reported in the literature and the pervasiveness and seriousness of IPV for both women and their infants, the Video Doctor plus Provider Cueing offers great promise for the seamless implementation of IPV prevention into routine prenatal care in a variety of settings.
Acknowledgments
The Health in Pregnancy study was funded by a grant from the U.S. DHHS National Institute on Drug Abuse (R01 DA 15597). The preparation of this manuscript was in part supported by a NIDA center grant (P50 DA 009253). None of the authors has any conflict of interest. Dr. Barbara Gerbert, PI, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Janice Humphreys, Email: Janice.humphreys@nursing.ucsf.edu, Department of Family Health Care Nursing, University of California, San Francisco, 2 Koret Way, Box 0606, San Francisco, CA 94143-0606, (415) 476-4432, (415) 753-2161.
Janice Y. Tsoh, Email: janice.tsoh@ucsf.edu, Department of Psychiatry, University of California, San Francisco, 401 Parnassus Avenue (0984-TRC), San Francisco, CA 94143-0984, (415) 502-8438, (415) 476-7734.
Michael A. Kohn, Email: Michael.kohn@ucsf.edu, Department of Epidemiology & Biostatistics, University of California, San Francisco, 185 Berry Street, Lobby 5, Suite 5700, San Francisco, CA 94107-1762, (415) 514-8142.
Barbara Gerbert, Email: Barbara.gerbert@ucsf.edu, Division of Behavioral Sciences, Professionalism, and Ethics, University of California, San Francisco, 707 Parnassus Avenue, Room 1032, Box 0758, San Francisco, CA 94143-0758, (415) 502-7283, (415) 476-0858.
References
- American College of Obstetricians and Gynecologists. ACOG technical bulletin. domestic violence. Number 209--August 1995 (replaces no. 124, January 1989). American College of Obstetricians and Gynecologists. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics. 1995;51(2):161–170. [PubMed] [Google Scholar]
- Berenson AB, Wiemann CM, Wilkinson GS, Jones WA, Anderson GD. Perinatal morbidity associated with violence experienced by pregnant women. American Journal of Obstetrics and Gynecology. 1994;170(6):1760–6. doi: 10.1016/s0002-9378(94)70352-3. discussion 1766-9. [DOI] [PubMed] [Google Scholar]
- Breiding MJ, Black MC, Ryan GW. Prevalence and risk factors of intimate partner violence in eighteen U.S. States/Territories, 2005. American Journal of Preventive Medicine. 2008;34(2):112–118. doi: 10.1016/j.amepre.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Briere J. Medical symptoms, health risk, and history of childhood sexual abuse. Mayo Clinic Proceedings: Mayo Clinic. 1992;67(6):603–604. doi: 10.1016/s0025-6196(12)60471-6. [DOI] [PubMed] [Google Scholar]
- Calderon SH, Gilbert P, Jackson R, Kohn MA, Gerbert B. Cueing prenatal providers effects on discussions of intimate partner violence. American Journal of Preventive Medicine. 2008;34(2):134–137. doi: 10.1016/j.amepre.2007.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain L, Perham-Hester KA. Physicians' screening practices for female partner abuse during prenatal visits. Maternal and Child Health Journal. 2000;4(2):141–148. doi: 10.1023/a:1009530523057. [DOI] [PubMed] [Google Scholar]
- Cokkinides VE, Coker AL, Sanderson M, Addy C, Bethea L. Physical violence during pregnancy: Maternal complications and birth outcomes. Obstetrics and Gynecology. 1999;93(5 Pt 1):661–666. doi: 10.1016/s0029-7844(98)00486-4. [DOI] [PubMed] [Google Scholar]
- Curry MA, Perrin N, Wall E. Effects of abuse on maternal complications and birth weight in adult and adolescent women. Obstetrics and Gynecology. 1998;92(4 Pt 1):530–534. doi: 10.1016/s0029-7844(98)00258-0. [DOI] [PubMed] [Google Scholar]
- El Kady D. Perinatal outcomes of traumatic injuries during pregnancy. Clinical Obstetrics and Gynecology. 2007;50(3):582–591. doi: 10.1097/GRF.0b013e31811eab82. [DOI] [PubMed] [Google Scholar]
- El Kady D, Gilbert WM, Xing G, Smith LH. Maternal and neonatal outcomes of assaults during pregnancy. Obstetrics and Gynecology. 2005;105(2):357–363. doi: 10.1097/01.AOG.0000151109.46641.03. [DOI] [PubMed] [Google Scholar]
- Ferris LE. Canadian family physicians' and general practitioners' perceptions of their effectiveness in identifying and treating wife abuse. Medical Care. 1994;32(12):1163–1172. doi: 10.1097/00005650-199412000-00001. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Petersen R, Spitz AM, Goodwin MM, Saltzman LE, Marks JS. Violence and reproductive health: Current knowledge and future research directions. Maternal and Child Health Journal. 2000;4(2):79–84. doi: 10.1023/a:1009514119423. [DOI] [PubMed] [Google Scholar]
- Gerbert B, Caspers N, Bronstone A, Moe J, Abercrombie P. A qualitative analysis of how physicians with expertise in domestic violence approach the identification of victims. Annals of Internal Medicine. 1999;131(8):578–584. doi: 10.7326/0003-4819-131-8-199910190-00005. [DOI] [PubMed] [Google Scholar]
- Gerbert B, Gansky SA, Tang JW, McPhee SJ, Carlton R, Herzig K, et al. Domestic violence compared to other health risks: A survey of physicians' beliefs and behaviors. American Journal of Preventive Medicine. 2002;23(2):82–90. doi: 10.1016/s0749-3797(02)00460-9. [DOI] [PubMed] [Google Scholar]
- Gerbert B, Johnston K, Caspers N, Bleecker T, Woods A, Rosenbaum A. Experiences of battered women in health care settings: A qualitative study. Women & Health. 1996;24(3):1–17. doi: 10.1300/j013v24n03_01. [DOI] [PubMed] [Google Scholar]
- Gerbert B, Moe J, Caspers N, Salber P, Feldman M, Herzig K, et al. Simplifying physicians' response to domestic violence. The Western Journal of Medicine. 2000;172(5):329–331. doi: 10.1136/ewjm.172.5.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerbert B, Moe J, Caspers N, Salber P, Feldman M, Herzig K, et al. Physicians' response to victims of domestic violence: Toward a model of care. Women & Health. 2002;35(2-3):1–22. doi: 10.1300/J013v35n02_01. [DOI] [PubMed] [Google Scholar]
- Greenberg EM, McFarlane J, Watson MG. Vaginal bleeding and abuse: Assessing pregnant women in the emergency department. MCN: The American Journal of Maternal Child Nursing. 1997;22(4):182–186. doi: 10.1097/00005721-199707000-00005. [DOI] [PubMed] [Google Scholar]
- Herzig K, Danley D, Jackson R, Petersen R, Chamberlain L, Gerbert B. Seizing the 9-month moment: Addressing behavioral risks in prenatal patients. Patient Education and Counseling. 2006;61(2):228–235. doi: 10.1016/j.pec.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Higgins PG, Clough DH, Frank B, Wallerstedt C. Changes in health behaviors made by pregnant substance users. The International Journal of the Addictions. 1995;30(10):1323–1333. doi: 10.3109/10826089509105137. [DOI] [PubMed] [Google Scholar]
- Cohn F, Salmon ME, Stobo JD, editors. Institute of Medicine. Confronting chronic neglect. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- Kuehn BM. Reducing HIV risks. JAMA: The Journal of the American Medical Association. 2008;299(24):2847. [Google Scholar]
- Martins R, Holzapfel S, Baker P. Wife abuse: Are we detecting it? Journal of Women's Health. 1992;1(1):77–90. [Google Scholar]
- McFarlane J, Parker B, Soeken K. Abuse during pregnancy: Associations with maternal health and infant birth weight. Nursing Research. 1996;45(1):37–42. doi: 10.1097/00006199-199601000-00007. [DOI] [PubMed] [Google Scholar]
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. severity and frequency of injuries and associated entry into prenatal care. JAMA: The Journal of the American Medical Association. 1992;267(23):3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- McGrath ME, Bettacchi A, Duffy SJ, Peipert JF, Becker BM, St Angelo L. Violence against women: Provider barriers to intervention in emergency departments. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine. 1997;4(4):297–300. doi: 10.1111/j.1553-2712.1997.tb03552.x. [DOI] [PubMed] [Google Scholar]
- Mercer RT. Becoming a mother versus maternal role attainment. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2004;36(3):226–232. doi: 10.1111/j.1547-5069.2004.04042.x. [DOI] [PubMed] [Google Scholar]
- Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: A risk factor for low birth weight? A systematic review and meta-analysis. CMAJ: Canadian Medical Association Journal. 2001;164(11):1567. [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 1999. Hyattsville, MD: U.S. Department of Health and Human Services; 1999. [Google Scholar]
- Petersen R, Connelly A, Martin SL, Kupper LL. Preventive counseling during prenatal care: Pregnancy risk assessment monitoring system (PRAMS) American Journal of Preventive Medicine. 2001;20(4):245–250. doi: 10.1016/s0749-3797(01)00302-6. [DOI] [PubMed] [Google Scholar]
- Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse: Practices and attitudes of primary care physicians. JAMA : The Journal of the American Medical Association. 1999;282(5):468–474. doi: 10.1001/jama.282.5.468. [DOI] [PubMed] [Google Scholar]
- Rodriguez MA, Quiroga SS, Bauer HM. Breaking the silence. battered women's perspectives on medical care. Archives of Family Medicine. 1996;5(3):153–158. doi: 10.1001/archfami.5.3.153. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller W. What is motivational interviewing? Behavioural and Cognitive Psychotherap. 1995;23:325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller W. Motivational interviewing in health care. New York: Guildford Press; 2008. [Google Scholar]
- Salber P. Mandatory reporting of domestic violence: Understanding the risks versus the benefits. Action Notes: Physicians for a Violence-Free Society. 1997;23:2–5. [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: Uniform definitions and recommended data elements. Atlanta: Centers of Disease Control and Prevention; 1999. [Google Scholar]
- Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: Uniform definitions and recommended data elements, version 1.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Prevention; 2002. [Google Scholar]
- Sugg NK, Inui T. Primary care physicians' response to domestic violence. opening Pandora's box. JAMA: The Journal of the American Medical Association. 1992;267(23):3157–3160. [PubMed] [Google Scholar]
- Survey Research Group, Cancer Surveillance and Research Branch. California adult tobacco survey. 2009 Retrieved from http://www.surveyresearchgroup.org/download/projects/2008%20CATS%20Doc.pdf.
- Thompson RS, Bonomi AE, Anderson M, Reid RJ, Dimer JA, Carrell D, et al. Intimate partner violence: Prevalence, types, and chronicity in adult women. American Journal of Preventive Medicine. 2006;30(6):447–457. doi: 10.1016/j.amepre.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Tsoh JY, Kohn MA, Gerbert B. Promoting smoking cessation in pregnancy with video doctor plus provider cueing: A randomized trial. Acta Obstetricia Et Gynecologica Scandinavica. 2010;89(4):515–523. doi: 10.3109/00016341003678419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: Final data for 1997. National Vital Statistics Reports : From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 1999;47(18):1–96. [PubMed] [Google Scholar]