Abstract
Alcohol dependence (AD) is more likely to occur among individuals with rather than without an anxiety disorder. Self-medication theory (SMT) holds that drinking behavior is negatively reinforced when alcohol temporarily reduces anxiety and that the resulting escalation of drinking increases the risk for AD. We set out to empirically scrutinize SMT using the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) dataset. We found that only a minority (about 20%) of anxiety disordered individuals endorsed drinking to control anxiety symptoms. This minority drank more alcohol, had a higher cross-sectional rate of AD, and was at higher risk for developing new AD over four years compared to anxiety disordered non-self-medicators and individuals with no anxiety disorder. Consistent with SMT, increased prospective risk for AD among self-medicators is partially mediated by an increased level of alcohol use. Understanding the processes that promote and inhibit self-medication should be a priority for anxiety disorder researchers.
1. Introduction
Those who meet diagnostic criteria for one or more anxiety disorder also meet criteria for alcohol dependence at a rate that far exceeds chance (Regier et al., 1990; Kessler et al., 1997; Hasin, Stinson, Ogburn, & Grant, 2007). Self-medication theory (SMT) is a widely held explanation for the relationship between these conditions (e.g., Khantzian, 1985; Kushner, Sher, & Beitman, 1990) that draws on the pioneering work of Conger (1956). This model explains the relationship between alcohol problems and anxiety disorders in terms of the tension-reducing properties of alcohol and the negative reinforcement resulting from alcohol-induced tension reduction. Extrapolating from these concepts, SMT posits that negative reinforcement of drinking resulting from alcohol-induced anxiety reduction promotes the escalation of alcohol consumption among anxiety-disordered individuals. This escalation of alcohol consumption, according to the SMT, increases the risk for the development of alcohol use disorder among those with anxiety disorders.
Given the familiarity of SMT to both professional and lay audiences, there is surprisingly little empirical confirmation that SMT processes account for the high rates of alcohol use disorders among those with anxiety disorders. In a review of the literature, Carrigan and Randall (2003) concluded that a significant portion of individuals with social anxiety disorder do consume alcohol to cope; however, evidence bearing on whether self-medicating behavior leads to pathological alcohol outcomes was not examined. Also cited in support of the SMT are the numerous experimental studies showing that acute alcohol intoxication does reduce tension states, stress-responding, and anxiety symptoms in a laboratory setting (e.g., Abrams et al., 2002, Kushner et al., 1996; Sher, 1987). However, laboratory studies do not address operation of SMT processes in the real-world experiences of anxious individuals.
Recent studies utilizing large community samples have begun to include questions about self-medication-motivated drinking in their datasets, allowing for more externally valid investigations of self-medicating behavior and its correlates. For example, it has been found that self-medication of anxiety symptoms with alcohol is indeed reported in a significant minority of anxiety cases in the community (Robinson, Sareen, Cox, & Bolton, 2009a) and at a much higher rate in treatment samples (Robinson, Sareen, Cox, & Bolton, 2009b). Endorsing self-medicating behavior has also been shown to correlate with a number of psychiatric variables, such as increased suicidality and treatment utilization, as well as decreased quality of life (Bolton, Cox, Clara, & Sareen, 2006; Robinson et al., 2009a). However, none of these studies examined key SMT propositions predicting that a self-medicating style of drinking leads to increased alcohol use and, ultimately, alcohol use disorder.
With the aim of filling in some of the remaining gaps in the knowledge base concerning operation of SMT, we examined specific SMT predictions using the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Wave 1 and Wave 2 datasets. We identified those with a current (12-month) anxiety disorder who endorsed self-medicating with alcohol and contrasted this group with anxiety disordered individuals who did not endorse self-medicating with alcohol. As a reference, we also included individuals who did not have an anxiety disorder (it should be noted that the NESARC did not inquire about alcohol use to manage anxiety symptoms for respondents not meeting diagnostic criteria for an anxiety disorder). First, we evaluated predictions related to the amount of alcohol use between the three study groups. Specifically, we predicted that those with an anxiety disorder who self-medicate with alcohol will have consumed more alcohol in the year prior to Wave 1 relative to the other two study groups. Second, we evaluated predictions related to alcohol dependence. Specifically, we predicted that a greater percentage of those with an anxiety disorder who self-medicate with alcohol will meet diagnostic criteria for a 12-month diagnosis of alcohol dependence (cross-sectional) and will develop more new cases of alcohol dependence between Waves 1 and 2 (prospective) relative to the other two study groups.
We did not expect significant group differences between those with an anxiety disorder who do not self-medicate and those with no anxiety disorder. This expectation was also extrapolated from SMT, according to which self-medication is the core process that increases risk for alcohol dependence among those with anxiety disorder relative to those with no anxiety disorder. Finally, we employed both the Wave 1 and 2 datasets to test the causal (mediational) model implied by SMT; i.e., that increased alcohol use among those with an anxiety disorder who acknowledge self-medication accounts for the increased prospective risk for developing alcohol dependence in this group.
2. Method
2.1 Participants
Data in this study were drawn from the NESARC, a nationally representative survey of U.S. citizens with Wave 1 response data collected in the years 2001 to 2002 from 43,093 individuals (see Grant et al., 2003b). Fifty seven percent of the sample was female and ages ranged from 18 to 98 (M= 46.4, SD=18.2). Only individuals who were identified in the dataset as consumers of alcohol at Wave 1 were included in analyses (N= 26,946). For this subsample, 51.5% of the sample was female and ages ranged from 18 to 98 (M= 43.3, SD=16.4). All cross-sectional analyses were conducted in this subsample. Of this sample, 22,245 also provided data in Wave 2 of the NESARC dataset (collected in the years 2004 to 2005), with women comprising 51.5% of that sample and ages that ranged from 18 to 96 years (M= 43.4, SD=16.0). All prospective analyses were conducted in this subsample of those who provided data at both Wave 1 and Wave 2.
2.2 Measures
2.2.1 Diagnoses
In the NESARC, current (past 12 month) psychopathology and substance use disorders were assessed using the NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule –DSM-IV version (Grant et al., 2003a), a highly structured diagnostic interview designed for administration by trained laypersons. All interviewers completed 10 days of training specific to the AUDADIS-IV. Ten percent of participants were re-contacted and certain subsets of the interview schedule were re-administered for quality control purposes; very high estimates of reliability were obtained (Grant et al., 2003a). Family history was assessed through a series of questions asking whether any first-degree relatives had ever been “problem drinkers” or “alcoholics.”
2.2.2 Self-Medication
Self-medicating behavior is assessed in the NESARC for each anxiety disorder for which a respondent meets full diagnostic criteria. For example, respondents who met diagnostic criteria for panic disorder were asked if they had at any time in the past year “[drank] alcohol to keep from having panic attacks.” We categorized a respondent as being in the self-medication group if they endorsed using alcohol in the previous 12-months to manage the symptoms of any anxiety disorder for which they met 12-month diagnostic criteria. Those who met criteria for one or more 12-month anxiety disorders without endorsing self-medicating with alcohol were categorized as non-self-medicators. The current study did not utilize specific phobia as a variable in analyses because it is unclear how self-medicating behavior applies in this diagnosis (Kushner et al., 1990). However, since the NESARC categorizes self-medication for “agoraphobia” as self-medication to manage a specific phobia, those with panic disorder with agoraphobia were counted as self-medicators if they endorsed drinking to cope with a specific phobia. It should be noted that although NESARC participants were asked if they had ever used drugs to cope with anxiety symptoms, we did not utilize self-medication with drugs as a variable in our analyses. It should also be noted that the proportion of individuals who endorsed self-medicating anxiety symptoms with alcohol was almost identical at both time points (20.3 percent at Wave 1 and 20.8 percent at Wave 2).
2.3 Statistical Analyses
We used SAS (v. 9.2) PROC SURVEYFREQ to calculate Chi-square tests comparing groups on categorical variables (e.g., rates of alcohol dependence) and PROC SURVEYREG to test for differences on continuous measures (average daily alcohol consumption). We used SAS (v. 9.2) PROC SURVEYLOGISTIC to calculate odds ratios for current alcohol dependence at Wave 1 and new alcohol dependence at Wave 2. All estimates incorporated adjustments (Taylor series linearization) for the complex survey design employed in the NESARC survey. Gender and family history of alcohol problems were entered as covariates in both the regression and logistic regression models.
Analyses of mediation effects with a dichotomous outcome were conducted using equations derived by Kenney based on MacKinnon and Dwyer’s (1993) work in this area. Ideally, a putative mediator should be measured after the predictor with a time-lag sufficient to allow the latter to fully impact the former. Similarly, the putative mediator should be measured prior to the outcome with a time-lag sufficient to allow the former to fully impact the latter. In this study, however, the mediator (i.e., the amount of alcohol consumed) was measured once in Wave 1 contemporaneously with the predictor (i.e. self-medication status) and once in Wave 2 contemporaneously with the outcome (i.e., alcohol disorder status). This precludes access to a measure of alcohol use (the mediator) at an intermediate time-point between the predictor and outcome that would be ideal for this mediator analysis. Given these limitations in the data, we chose to use Wave 1 alcohol consumption as the mediating variable in this analysis. This makes sense if self-medication status is considered to be a relatively stable; i.e., those who report self-medicating at Wave 1 were also likely to be self-medicating prior to Wave 1. This assumption seems reasonable given the high stability of self-medication status between Waves 1 and 2 (see above).
3. Results
3.1 Group Characteristics
Table 1 contrasts relevant sample characteristics among the three study groups at Wave 1. Between 6% and 7% of the sample met criteria for a “current” (12-month) diagnosis of at least one anxiety disorder included in the study. Of this group, 20.3% endorsed drinking alcohol to manage their anxiety symptoms. The proportion males and females was nearly even (slightly more males) in both the non-anxiety group and the anxiety-disordered self-medicating group. However, approximately two-thirds of the anxiety-disordered non-self-medicating group was female. In other words, anxiety disordered cases who self-medicated were much more likely to be male than were anxiety cases who did not self-medicate (Wald χ2 (1)=39.2, p<.0001, φ=.12).
Table 1.
Sample Characteristics1
| No Lifetime Anxiety Diagnosis |
Current Anxiety Disorder: Does not endorse drinking to reduce anxiety |
Current anxiety disorder: Does endorse drinks to reduce anxiety |
|
|---|---|---|---|
| Sample Size | N= 25342 | N= 1321 | N= 337 |
| % Male | 54.5 | 35.3 a | 54.0 b |
| % Family history of alcohol problems |
32.6 a | 49.8 b | 64.7 c |
Note: Subscript letters attached to individual values in Table 1 indicate significant differences between groups; i.e., in a single row, “a” is significantly different from “b” is significantly different from “c.”
All individuals included in all analyses reported “current” alcohol use at Wave 1. “Current” anxiety disorder and drinking to manage anxiety was keyed to “past year” with reference to the Wave 1 and Wave 2 data collection.
Also shown in Table 1 is that about one-third of non-anxious individuals at Wave 1 reported a family history of alcohol problems, compared to about half of the anxious non-self-medicating group (Wald χ2 (1)=304.7, p<.0001, φ=.09) and over sixty percent of the anxious self-medicating group (Wald χ2 (1)=330.9, p<.0001, φ=.09). The difference in family history between self-medicators and non-self-medicators was also significant (Wald χ2 (1)=39.2, p<.0001, φ=.12).
3.2 Alcohol Consumption Volume
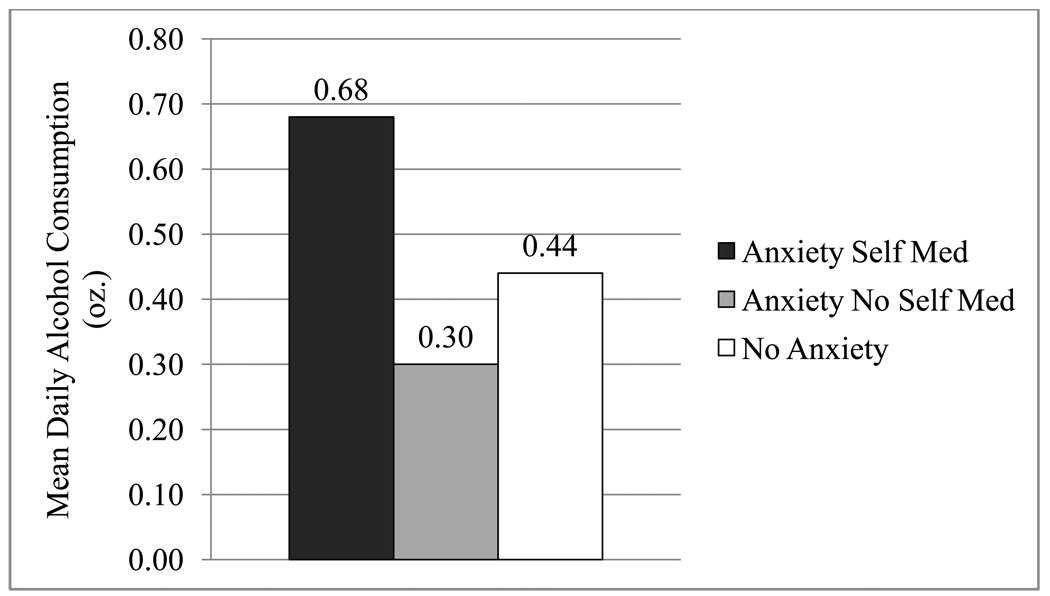
Figure 1 shows the mean ounces of ethanol consumed per day reported for the year preceding the Wave 1 assessment by study group (note that there are about .6 oz of pure ethanol in a standard drink). Consistent with study predictions, anxiety disordered individuals who self-medicate consumed significantly more alcohol per day on average in the past year than anxiety disordered individuals who do not self-medicate (F(1,369)=7.09, p=.008, r=.14). Notably, individuals with an anxiety disorder who do not self-medicate consumed significantly less alcohol than non-anxious individuals (F(1,369)=22.2, p=<.001, r=.24), which is contrary to our prediction that non-anxious and anxiety-disordered non-self-medicators would not differ on alcohol outcome variables.
Figure 1.
Drinking Volume Between the Groups at Wave 1 2
2 Data in Figure 1 excludes individuals with a current alcohol disorder diagnosed at Wave 1 as drinking variability in this subgroup would be largely restricted to the high range.
3.3 Alcohol Dependence
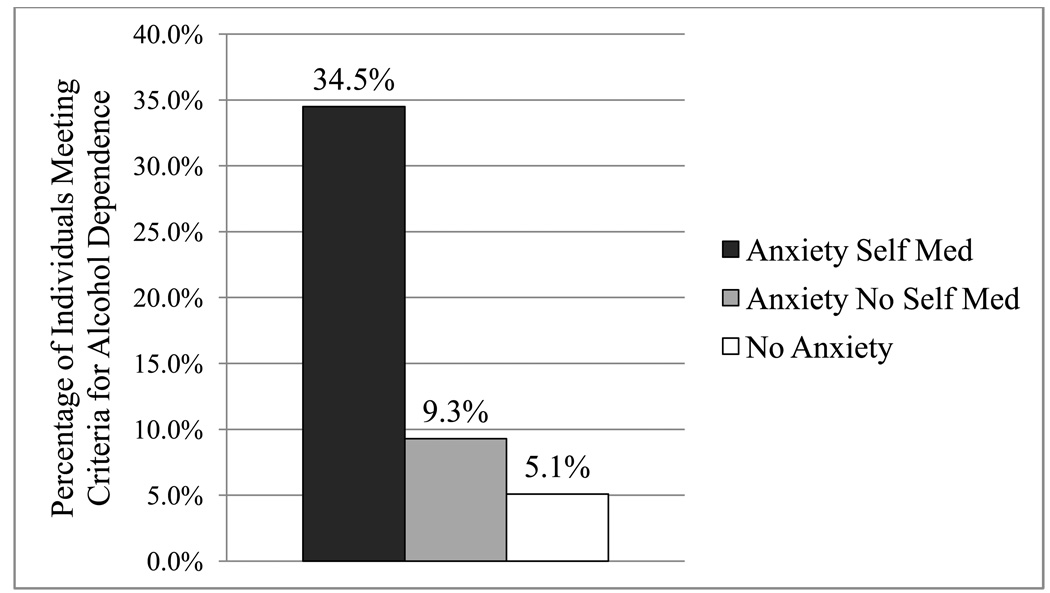
Figure 2 shows that 12-month Wave 1 alcohol dependence was most prevalent among anxiety disordered individuals who self-medicate (34.5%) followed by those with an anxiety disorder who do not self-medicate (9.3%) and was lowest among those with no anxiety disorder (5.1%) (χ2(2)=219.8, p<.0001, φ=.07). So, the rate of alcohol dependence among non-self-medicating anxiety disordered individuals was only about four percent higher than among those with no anxiety disorder. However, the rate of alcohol dependence was over 29 percent higher in those who self-medicated their anxiety disorder compared to those with no anxiety disorder.
Figure 2.
Rates of Alcohol Dependence Between the Groups at Wave 1
This means that the difference in alcohol dependence rates between the non-self-medicating anxiety disorder group and the group with no anxiety disorder was, while significant, relatively small (χ2(1)=61.8, p<.0001, φ=.04) compared to the group differences between the self-medicating anxiety disorder group and either the other anxiety disordered cases or those with no anxiety disorder (χ2=137.7, p<.0001, φ=.23; and, χ2=163.8, p<.0001, φ=.07, respectively). This pattern mirrors the results shown above for alcohol consumption; both consumption and rates of dependence were significantly elevated among self-medicating individuals, which comprise the minority (20%) of all anxiety-disordered individuals in our sample.
3.4 Mediation Analysis
As outlined in the Introduction, SMT posits that the increase in risk for alcohol disorder among those with an anxiety disorder is conferred by the increase in alcohol consumption due to the negative reinforcement of drinking behavior inherent in the self-medication process. We specified this mediator model by identifying risk for alcohol dependence at Wave 2 as the outcome, self-medication status at Wave 1 as the predictor, and alcohol consumption volume at Wave 1 as the mediator (see the Method section for additional information concerning constraints in the dataset affecting the way in which the mediator model could be specified). Without Wave 1 alcohol consumption in the analysis, the presence of self-medicating behavior at Wave 1 increases risk for the development of new dependence at Wave 2 by an OR of 3.77 (95% CI=2.58–5.51). When Wave 1 alcohol consumption is included in the analysis, self-medication still confers some risk for new dependence at Wave 2, but the odds ratio drops to 2.71 (95% CI=1.74–4.19). A Sobel test of mediation, adjusted for a dichotomous outcome (MacKinnon & Dwyer, 1993) found that alcohol consumption did significantly mediate the effect of self-medication on new alcohol dependence at Wave 2 (Sobel statistic=3.36, p<.001). With that said, the fact that a significant OR association between self-medication and risk for later alcohol dependence remains even after controlling for drinking amount indicates that the latter does not completely mediate the former.
4. Discussion
The core tenet of SMT is that alcohol is used to cope with negative affect (e.g., anxiety symptoms). We found that only about 20% of drinkers with a current anxiety disorder reported using alcohol in the past year for the explicit purpose of coping with their anxiety symptoms. This is consistent with previous studies of self-medication in community samples (e.g., Robinson et al, 2009a). Because it can be reasonably inferred from SMT that all anxious individuals who drink would be prone to self-medication (i.e., via negative reinforcement), the small proportion of anxiety disordered individuals who actually report this behavior fails to fully comport with SMT; however, the force of this conclusion is mitigated by two further considerations.
First, SMT does not speak directly to the obvious fact that forces/motives besides managing negative affect (including those that strongly inhibit drinking when anxious) contribute to drinking behavior (or lack thereof). Therefore, the lack of drinking for the purpose of anxiety management among some (even a majority of) individuals with an anxiety disorder does not frankly contradict SMT; although it does suggest its application should be more narrowly specified. Second, the assumption that individuals would be able and willing to report their drinking motives accurately is not itself above suspicion (e.g., Nisbett & Wilson, 1977). Therefore, the small proportion of individuals admitting to this practice may underestimate the actual degree of self-medication oriented drinking in this population.
However, if the measurement of self-medication in the NESARC grossly underestimated the true rate of self-medication oriented drinking, we would not expect see substantial differences between identified self-medicators and other anxiety disordered individuals in terms of alcohol use and outcomes. But we do, in fact, find differences between these groups that are highly consonant with SMT-based predictions. Specifically, those with an anxiety disorder who reported self-medication motivated drinking consumed more alcohol and faced a higher risk for alcohol dependence than did those with an anxiety disorder who did not endorse self-medicating. Additionally, the rates of self-medicating drinking remained relatively constant from Wave 1 to Wave 2. At Wave 1, 20.3 percent of anxiety-disordered individuals endorsed self-medicating, and at Wave 2, 20.8 percent of anxiety-disordered individuals endorsed the same behavior. The implications of these findings are discussed in greater detail below but are noted here as supportive evidence for the validity of how self-medication was assessed in the NESARC.
4.1 Conclusions
Predictions inferred from the SMT concerning alcohol use and risk for alcohol dependence among self-medicating individuals were supported both by cross-sectional and prospective analyses. Those who reported self-medicating anxiety symptoms with alcohol drank a significantly greater volume of alcohol in the year preceding the Wave 1 assessment than those who did not endorse self-medicating their anxiety symptoms with alcohol. Similarly, self-medicators were more likely to be alcohol dependent at Wave 1 and more likely to develop a new alcohol dependence diagnosis between the Wave 1 and Wave 2 assessments than were those who did not endorse self-medicating their anxiety symptoms with alcohol. Additionally, and also consistent with the SMT, mediator analyses showed that quantity of alcohol consumption accounted for a significant proportion of the association between self-medicating drinking status and the increased risk for development of new alcohol dependence among those with anxiety disorder. However, it is interesting to note that volume of alcohol consumption did not account for the entirety of the risk for alcohol dependence conferred by self-medicating behavior. This suggests that SMT mechanisms may only partially account for the increased risk for alcohol disorder experienced by self-medicating anxiety-disordered individuals.
We predicted that anxiety-disordered individuals who do not acknowledge self-medicating (found to be 80% of all anxiety disordered cases) would not significantly differ from non-anxiety disordered individuals in terms of either drinking volume or risk for alcohol dependence. However, we found that anxiety disordered non-self-medicators actually drank somewhat less than non-anxious individuals at Wave 1 and yet were about two times more likely than non-anxious individuals to meet criteria for alcohol dependence at Wave 1. These findings cannot be explained by SMT, because by definition non-self-medicating individuals are not attempting to alleviate anxiety symptoms with alcohol and therefore should have no increased risk for alcohol dependence according to SMT. These findings point to processes distinct from self-medication and related changes in drinking behavior that can elevate risk for alcohol dependence among those with anxiety disorder. With this said, the elevated risk for alcohol dependence in anxiety-disordered non-self-medicators was rather small compared to the elevated risk in self-medicators (see Figure 2).
As alluded to above, while our findings support SMT-based predictions concerning anxiety-disordered individuals who self-medicate, it is also important to note that this population comprises a rather small subset (i.e., about 20%) of all individuals with anxiety disorders. At a practical level, this is seemingly advantageous. That is, efforts aimed at reducing the "high risk" for alcohol dependence that has previously been associated with anxiety disorder in general (e.g., Kushner et al., 1990, 2000) might appropriately be concentrated on the much smaller subset of those who report self-medicating anxiety symptoms with alcohol. Also relevant here are recent studies showing that self-medication is associated with multiple psychiatric variables like suicidality, treatment utilization, and overall mental health (Bolton et al., 2006; Robinson et al., 2009); perhaps multiple clinical resources besides alcohol-reduction interventions should be focused on this particular subgroup.
With this said, a clearer understanding of the critical processes that increase and inhibit risk for pathological alcohol use among those with an anxiety disorder would likely follow from increased knowledge of the mechanisms that incite (or inhibit) self-medicating behavior among anxiety-disordered individuals. Here we are asking the question: "Why do some individuals with anxiety self-medicate with alcohol while others do not?" Cognitive factors such as alcohol outcome expectancies may be relevant. For instance, Kushner, Sher, Wood, and Wood (1994) found that among college undergraduates, those with higher expectancies for alcohol to be anxiety reducing showed a stronger correlation between measures of anxiety and alcohol use compared to individuals with lower expectancies for alcohol’s tension-reducing effects. Kushner, Abrams, Thuras and Hanson (2000) expanded this concept from college students to individuals with panic disorder showing that expectancies for alcohol to be anxiety reducing significantly predicted a self-medicating style of drinking. Such pathogenic alcohol expectancies may be associated with individual differences at the level of the brain/personality (e.g., Cloninger, 1987) but may still be malleable via focused psycho-social learning experiences (Darkes & Goldman, 1998).
4.2 Limitations
It is important to note that this study was limited by the use of an unvalidated measure of self-medication (i.e., single-item self-report). In addition to reliability and validity concerns, the use of such a measure begs an important question: Does an individual have to be aware of the motivations for his or her drinking in order to be classified as a “self-medicator?” That is, must an individual be explicitly aware of the tension reduction created by alcohol in order to receive negative reinforcement from drinking? We cannot answer this vexing question; however, we have shown that self-medicating behavior, when measured as an explicit, conscious set of motivations for drinking, has significant implications for an individual’s volume of alcohol consumption and risk for alcohol dependence among anxious individuals.
If data concerning frequency and intensity of self-medication had been available in the NESARC, a more powerful test of the SMT would have been possible. For example, perhaps more frequent or more intense self-medicating drinking confers an increased risk for escalation of alcohol consumption and future development of alcohol dependence. Frequency and intensity of self-medication may even be determined in part by cognitive or family history factors described above. Again, absence of frequency information, unfortunately, precludes finer grained tests of SMT predictions.
This study was also limited by the lack of continuous measures of alcohol consumption over time. Alcohol consumption was only measured as average daily volume for the 12 months preceding Wave 1 and 2 assessments. Multiple measures during the approximately four-year interim separating Waves 1 and 2 would have been more informative, especially in regard to our formal mediator analysis. We have shown that alcohol consumption accounts for a significant portion of the variance in prospective development of alcohol dependence, but the magnitude of this mediation effect would be more accurately estimated with more detailed alcohol consumption data over the follow-up period.
In summary, the present study investigated the relationship between alcohol dependence and anxiety disorders using the theoretical framework of SMT as a base from which to generate and test hypotheses. The purpose of this study was not simply to offer more support for an already popular explanation for the relationship between alcohol and anxiety. Rather, we attempted to specify and test the oft-referenced and intuitively appealing set of ideas embodied in SMT within an empirical framework using a dataset that is broadly generalizable. The implication of our results is that while SMT mechanisms do not seem to be operative in a majority (80%) of individuals with an anxiety disorder, the theory does offer an empirically sound, parsimonious explanation for the increased risk for alcohol dependence among the subgroup of anxiety-disordered individuals (20%) who do self-medicate their anxiety symptoms with alcohol. When applied specifically to this substantial subpopulation, self-medicating behavior and an associated escalation of alcohol use can increase the risk for the development of alcohol dependence.
Acknowledgments
The paper is based on research conducted by Matt Kushner Ph.D., as a part of his NIAAA grant R01AA0105069.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrams K, Kushner MG, Medina KL, Voight A. Self-administration of alcohol before and after a public speaking challenge by individuals with social phobia. Psychology of Addictive Behavior. 2002;16:121–128. [PubMed] [Google Scholar]
- Bolton J, Cox B, Clara I, Sareen J. Use of alcohol and drugs to self-medicate anxiety disorders in a nationally representative sample. The Journal of Nervous and Mental Disease. 2006;194:818–825. doi: 10.1097/01.nmd.0000244481.63148.98. [DOI] [PubMed] [Google Scholar]
- Carrigan MH, Randall CL. Self-medication in social phobia: A review of the alcohol literature. Addictive Behaviors. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236:410–416. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- Conger JJ. Alcoholism: theory, problem and challenge II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Process and structure in the alcohol expectancy network. Experimental and Clinical Psychopharmacology. 1998;6:64–76. doi: 10.1037//1064-1297.6.1.64. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003a;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism; 2003b. [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;53:232–240. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Khantzian E. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL. Individual differences predictive of drinking to manage anxiety among non-problem drinkers with panic disorder. Alcoholism: Clinical & Experimental Research. 2000;24:448–458. [PubMed] [Google Scholar]
- Kushner MG, Mackenzie TB, Fiszdon J, Valentiner DP, Foa E, Wangensteen D. The effects of alcohol consumption on laboratory induced panic and state anxiety. Archives of General Psychiatry. 1996;53:264–270. doi: 10.1001/archpsyc.1996.01830030086013. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. American Journal of Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Wood MD, Wood PK. Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research. 1994;18:852–860. doi: 10.1111/j.1530-0277.1994.tb00050.x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- Nisbett RE, Wilson TD. Telling more than we can know: Verbal reports on mental processes. Psychological Review. 1977;84:231–259. [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox B, Bolton J. Correlates of self-medication for anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Nervous and Mental Disease. 2009a;197:873–878. doi: 10.1097/NMD.0b013e3181c299c2. [DOI] [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox B, Bolton J. Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. Journal of Anxiety Disorders. 2009b;23:38–45. doi: 10.1016/j.janxdis.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Sher KJ. Stress response dampening. In: Blane HT, Leonard KE, editors. Psychological Theories of Drinking and Alcoholism. New York, NY: Guilford Press; 1987. pp. 227–264. [Google Scholar]