Abstract
Background
Previous work has shown that there is a higher frequency of hospitalizations among black heart failure patients relative to white heart failure patients. We sought to determine whether racial differences exist in health literacy and access to outpatient medical care, and to identify factors associated with these differences.
Methods
We evaluated data from 1464 heart failure patients (644 black and 820 white). Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine-Revised (REALM-R), and access to care was assessed through participants’ self-report.
Results
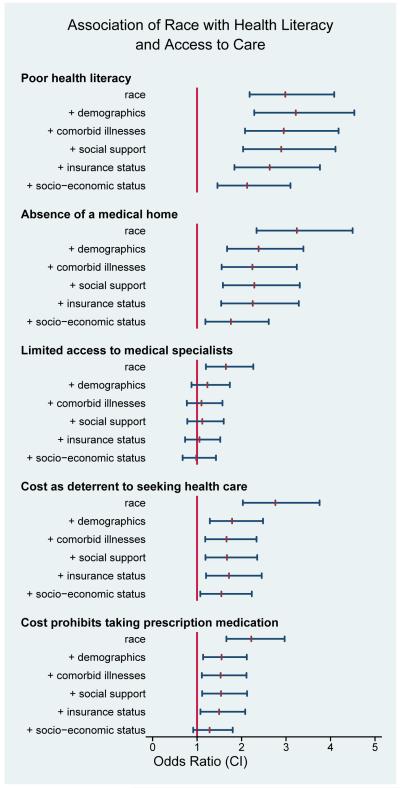
Black race was strongly associated with worse health literacy and all measures of poor access to care in unadjusted analyses. After adjusting for demographics, non-cardiac comorbidity, social support, insurance status, and socio-economic status (income and education), the strongest associations were seen between race and: health literacy (OR 2.13, 95% CI 1.46-3.10), absence of a medical home (OR 1.76, 1.19-2.61), and cost as a deterrent to seeking health care (OR 1.55, 1.07-2.23).
Conclusions
Our findings highlight that important racial differences in health literacy and access to care exist among patients with heart failure. These differences persist even after adjustment for a broad range of potential mediators, including educational attainment, income, and insurance status.
Keywords: Heart Failure, Racial Disparities, Health Literacy, Access to Care
INTRODUCTION
Many studies show a disproportionate burden of heart failure in black patients, with greater prevalence of heart failure and higher rates of heart failure hospitalization compared with whites.1-5 These disparities may be attributable to poorer outpatient management and a greater dependence upon emergency medical services for heart failure exacerbations.
Heart failure is often marked by recurrent episodes of decompensation, necessitating extensive daily management by patients and close monitoring by clinicians. In order to maintain health and manage episodes of heart failure decompensation, patients must monitor sodium and fluid intake, adhere to complicated medication regimens, measure daily body weight, and navigate an often complicated and confusing health care system. Despite the potential importance of health literacy and access to outpatient care in heart failure management, it is unknown whether racial differences exist in these domains. Accordingly, we sought to determine whether differences exist between black and white patients with heart failure in health literacy and access to outpatient medical care. We further analyzed patient characteristics that may mediate the associations between race and the health literacy and access to care outcomes, to determine potential factors that might account for observed disparities.
METHODS
Study Design
The data for this study come from a randomized controlled trial (Telemonitoring to Improve Heart Failure Outcomes, or Tele-HF, NIH Clinical Trials #NCT00303212) designed to evaluate the effect of an automated, daily symptom and weight monitoring intervention in reducing all-cause hospital readmissions and mortality among patients recently hospitalized with decompensated heart failure. The Tele-HF study design has been previously described in detail.6 For the purposes of this analysis, only baseline data (i.e., before any intervention was administered), collected as part of the original clinical trial, were used.
Patient Selection
Study participants were recruited from 33 community-based cardiology practices across the United States from 2005-2009 (Appendix). Practices were selected to enhance generalizability of the study’s results, with particular attention to geographic, racial, and socio-economic diversity. All study participants were recently discharged from a heart failure hospitalization (within 30 days of enrollment into the study). Exclusion criteria were: age less than 18 years; long-term nursing home residence; residence in a correctional facility; inability to speak either English or Spanish; irreversible medical conditions likely to affect 6 month survival; Folstein Mini-Mental State Exam7 score less than 20; no access to a telephone line; currently scheduled for cardiac transplant, left ventricular assist device or valvular surgery; and planned coronary artery bypass grafting or percutaneous coronary intervention within 90 days of enrollment.
The Tele-HF study enrolled 1660 patients. For this study we excluded those who did not identify themselves as “white” or “black” (n=195), and those who identified themselves as both (n=1), leaving 1464 patients for this analyses, as no additional exclusion criteria were applied to data from the original trial.
Data Collection
Baseline interviews were conducted within 30 days of hospital discharge by experienced interviewers, all of whom underwent training.
Study Measures
Race
Self-reported race was used to improve accuracy of racial categorization. Patients were allowed to select all racial categories that applied.
Demographic Information
Age was categorized into less than 45 years; 45-64 years; and at least 65 years. We also included information about sex.
Comorbid Disease
Non-cardiac comorbidities (chronic renal insufficiency, chronic obstructive pulmonary disease [COPD], diabetes mellitus, and hypertension) were assessed through medical record review. We included this category as patients with a greater burden of non-cardiac comorbidities may be under the care of a greater number of specialists, or under the closer care of a primary care physician.
Social Support
Because social support may play an important role in patients’ management of heart failure,8 we included information about living alone as a measure of social support. Living alone has been associated with social isolation and diminished emotional support.9
Insurance Status
To assess the effects of insurance status on the relationship between race and outcomes, we included information about patients’ health insurance coverage. This information was obtained through medical record review, and was categorized as: no medical insurance; insured with Medicaid; and insured, not with Medicaid.
Socio-economic Status
Income information was obtained by asking patients to select the category (<$10,000, $10,000-$29,999, $30,000-$49,999, and at least $50,000) that best described their annual household income. Educational attainment was ascertained by self-report and divided into less than high school, high school graduate, or education beyond high school.
Outcomes
Health Literacy
The American Medical Association defines health literacy as “a constellation of skills, including the ability to perform basic reading… tasks required to function in the health care environment.”10 The Rapid Estimate of Adult Literacy in Medicine-Revised (REALM-R) is a validated measure of health literacy.11 “The REALM-R is an eight-item instrument, with possible scores ranging from zero to eight. A cut-point of six was chosen because it corresponds to a sixth grade reading level, which is associated with difficulty with comprehension of written and oral materials.12The REALM-R was administered in-person, at the time of enrollment into the study. Of note, only 11 participants (all white) were Spanish speaking only, and the REALM-R was administered in Spanish to those participants.
Access to medical care
Given our focus on understanding racial differences in access to medical care that may be related to higher frequency of hospitalizations in black patients, we assessed this domain with 4 items pertinent to outpatient heart failure management. These included, 1) “do you currently have a doctor or care provider who you feel is primarily responsible for your health care?” This was used to assess absence of a medical home, and response options were “yes” or “no.” 2) “I have easy access to the medical specialists I need.” For the purposes of analysis, responses were dichotomized into “strongly agree” and “agree” versus “not sure”, “disagree”, and “strongly disagree.” 3) “In the past year, have you avoided getting health care services because of cost?” The response options were “yes” or “no.” 4) “In the past year, how often have you not taken a medicine that your doctor prescribed for you because of cost?” The response options for this question were dichotomized into “never” versus all other responses (“rarely”, “occasionally”, “frequently”, and “always”), since missing even only a few doses of cardiac medications (such as beta-blockers or diuretics) can affect clinical status.
Statistical Analyses
We compared demographic, socio-economic, and clinical characteristics of black and white patients (see Table). Differences between the groups were tested using t-tests for continuous variables and chi-square tests for categorical variables. Because of the possibility that missing data may occur in a non-random pattern, we did not omit missing values, but rather included ‘missing’ as distinct category for dependent variables with missing data.
Table 1.
Characteristics of Study Population, %
| Blacks (N=644) | Whites (N=820) | P Value | |
|---|---|---|---|
| DEMOGRAPHICS | |||
| Age group, years | <0.001 | ||
| <45 | 22 | 7 | |
| 45-64 | 55 | 33 | |
| 65+ | 23 | 58 | |
| Female | 44 | 41 | 0.279 |
| Non-cardiac comorbidity | |||
| Chronic Renal Insufficiency | 29 | 25 | 0.090 |
| Chronic Obstructive Pulmonary Disease | 18 | 25 | 0.003 |
| Diabetes Mellitus | 44 | 49 | 0.085 |
| Hypertension | 85 | 71 | <0.001 |
| SOCIAL SUPPORT | |||
| Lives Alone | 25 | 35 | <0.001 |
| INSURANCE STATUS | <0.001 | ||
| No Medical Insurance | 18 | 8 | |
| Insured by Medicaid | 25 | 9 | |
| Non-Medicaid Medical Insurance | 57 | 83 | |
| SOCIO-ECONOMIC STATUS | |||
| Education | <0.001 | ||
| < High School | 24 | 18 | |
| High School Graduate | 32 | 33 | |
| Post High School Education | 28 | 38 | |
| Annual Household Income | <0.001 | ||
| < $10,000 | 29 | 12 | |
| $10,000- <$30,000 | 25 | 27 | |
| $30,000- <$50,000 | 10 | 17 | |
| $50,000+ | 5 | 18 | |
All variables missing less than 5% of data, except social support (missing in 18% of black patients and 12% of whites); insurance status (missing in 16% of black patients and 11% of whites); education (missing in 16% of black patients and 11% of whites); and income (missing in 31% of black patients and 27% of whites)
In order to understand how patient-level characteristics may mediate the relationships between race and the health literacy and access to care outcomes, we evaluated the contribution of demographic, clinical, and socio-economic characteristics to observed racial differences in outcomes (i.e., health literacy and access to care, as defined above) by sequential, cumulative adjustment. In the first step, the unadjusted association between race and each outcome was examined. In the second step, we adjusted only for demographics; in the third, information about comorbidity was added to the model containing race and demographics; in the fourth step we added social support; in the fifth step we added insurance status; and in the final step we added socio-economic status so that all variables shown in Table 1 were included. Comparing the adjusted race estimates between adjacent steps thus indicates the added effect of a given domain after adjustment for all previous variables.
We used Stata, version 11 (StataCorp, College Station, Texas) to conduct our analyses. A 2-sided P value less than 0.05 was considered statistically significant.
Role of the Funding Source and Approval by Human Investigations Committee
This study was supported by the National Heart, Lung, and Blood Institute (grant no. R01 HL080228). The study was designed, executed, analyzed, interpreted, and reported by the investigators without input from the sponsors.
The study protocol was approved by the Yale Human Investigations Committee. All participants provided written informed consent prior to participating in the study.
RESULTS
Of the 5076 patients screened for enrollment into the Tele-HF trial, 2,634 met eligibility criteria (as defined above in “Patient Selection” section). Compared with patients included in the current analysis, eligible patients who were not enrolled were older ([mean±sd] 67±15 vs. 61±15 years), less often female (41% vs. 42%) and less often black (30% vs. 39%).
Of the 1464 participants included in these analyses, 644 were of black race and 820 were white. As shown in the Table, compared with whites, black patients were younger, and had important clinical differences. Black patients were more likely to have hypertension, but less likely to have COPD. Black patients were less likely to live alone, had higher rates of being uninsured or on Medicaid, and had lower socio-economic status.
Shown in the Figure are the unadjusted and sequentially adjusted multivariable models comparing black and white patients with respect to the outcomes, health literacy and access to health care.
Poor health Literacy
In unadjusted analyses, black patients were significantly more likely than white patients to have poor health literacy: 24.4% of black patients had poor health literacy and 9.7% of whites (odds ratio [OR] 2.98, 95% CI, 2.18-4.08). Adjustment for age and sex, comorbidity, social support, and insurance status had little effect on the relationship between race and health literacy (OR 2.63, 95% CI 1.84-3.76). Adding information about education and income attenuated the relationship, though it remained statistically significant (OR 2.13, 95% CI 1.46-3.10). The fully adjusted (i.e., adjusted for all variables shown in Table 1) rates of having poor health literacy were 20.4% in black patients (95% confidence interval [CI] 17.1-23.6) and 11.7% in whites (95% CI 9.2-14.2).
Absence of medical home
Black patients were much more likely to report absence of a medical home in unadjusted analyses: 23.6% of black patients compared with 8.7% of whites (OR 3.24, 95% CI 2.34-4.50). The addition of demographic information attenuated the relationship (OR 2.38, 95% CI 1.67-3.39). Adding information about comorbidity, social support, insurance had little effect on the relationship between race and absence of a medical home (OR 2.25, 95% CI 1.54-3.29), which was then attenuated with addition of information about socio-economic status (final OR 1.76, 95% CI 1.19-2.61). The fully adjusted event rates of absence of a medical home were 18.0% in black patients (95% CI 15.0-20.9) and 11.9% in whites (95% CI 9.2-14.6).
Limited access to medical specialists
The unadjusted association between race and access to medical specialists was the weakest in these analyses. In unadjusted analyses, 17.9% of black patients reported limited access to medical specialists compared with 11.7% of whites (OR 1.65, 95% CI 1.20-2.26). Adjustment for demographics attenuated the association (OR 1.23, 95% CI 0.87-1.74), with additional attenuation as other factors were added to the model (final OR 0.98, 95% CI 0.67-1.42). The fully adjusted event rates of having limited access to medical specialists were nearly identical in black and white patients: 14.5% in black patients (95% CI 11.5-17.4) and 14.5% in whites (95% CI 11.5-17.4).
Cost as a deterrent to seeking health care
Black patients were more likely than white patients (25.0% versus 10.8%, respectively) to report that cost was a deterrent to seeking health care in unadjusted analyses (OR 2.76, 95% CI 2.03-3.75). This association remained significant, but was attenuated, with the addition of demographic information (OR 1.79, 95% CI 1.29-2.48), and other factors (final OR 1.55, 95% CI 1.07-2.23). The fully adjusted event rates of cost as a deterrent to seeking health care were 19.5% in black patients (95% CI 16.5-22.5) and 14.3% in whites (95% CI 11.4-17.1).
Cost prohibits taking prescription medication
Black patients were significantly more likely than white patients (25.3% versus 13.2%, respectively) to report that cost prohibited them from taking prescription medication in unadjusted analyses (OR 2.22, 95% CI 1.66-2.97). Adding demographic information attenuated the strength of the association (OR 1.55, 95% CI 1.14-2.12), which then remained stable with addition of information on comorbidity, social support, and insurance status. Addition of socio-economic information attenuated the relationship (final OR 1.28, 95% CI 0.91-1.80). The fully adjusted event rates of cost as a prohibitor to taking prescription medication were 20.2% in black patients (95% CI 17.0-23.3) and 16.8% in whites (13.7-19.8).
DISCUSSION
Our study demonstrates that important differences in health literacy and access to care exist between black and white patients with heart failure. The unadjusted associations between black race and these outcomes were clinically and statistically significant, and demonstrate that important challenges exist in eliminating disparities among black patients with heart failure. The strongest unadjusted (and adjusted) associations were seen between race and health literacy, absence of a medical home, and cost as a deterrent to seeking health care.
We also determined that the demographic, clinical, and socio-economic characteristics differ significantly between black and white patients. Our approach of sequential adjustment for these groups of factors allows for an understanding of how they affect the relationship between race and outcomes. It is notable that race remains strongly associated with health literacy even after adjusting for education, suggesting that the association between race and health literacy is not entirely explained by level of education. Similarly, although one might expect that the relationship between race and absence of a medical home is largely explained by insurance status, adjustment for this had minimal affect. In the analyses of cost as a deterrent to seeking health care, adding information about insurance and socio-economic status also had modest effects. In contrast, it is notable that adding demographic information (age and sex) led to the greatest diminution in association between race and access to care outcomes. While the sex distribution of blacks and whites was quite similar (44% of black patients were female and 41% of whites were female), 22% of black patients in our study were <45 years of age, compared with only 7% of whites. Our findings suggest that interventions to improve health care access for black patients may need to focus on younger patients, and extend beyond providing insurance coverage.
At the core of high quality outpatient health care is an ongoing partnership between an informed, “activated” patient and a clinician who is familiar with the patient and takes primary responsibility for delivering coordinating the patient’s care. Poor health literacy diminishes patients’ self-management abilities,12, 13 and is associated with worse outcomes, including increased risk for hospital admission.14 A recently completed clinical trial (PILL-CVD) will shed light on whether a pharmacist intervention can improve improve medication use among patients with low health literacy.15 Every day, patients with heart failure must adhere to complicated medication regimens and maintain vigilance regarding dietary sodium and fluid intake. In addition to monitoring signs and symptoms related to heart failure decompensation, such as weight gain, orthopnea and lower extremity edema, patients must be able to access and navigate the medical system when such signs and symptoms arise. These tasks are likely made even more challenging with the added burden of difficulty recognizing and interpreting basic health care terms.
Absence of a medical home can only exacerbate the challenges of poor health literacy, as care is more fragmented with greater onus on patients to communicate pertinent details as care is shifted between clinicians. Given the disjointed nature of our current health care system, with little to no sharing of information across settings, important clinical details can become lost. The importance of a medical home is supported by a large body of research demonstrating its association with improved outcomes, including cardiovascular and all-cause mortality.16-18
Previous large scale studies19, 20 21, 22 examining differences in the characteristics of black and white patients with heart failure have focused on demographics, comorbid illness, and echocardiographic findings, but have not assessed patients’ health literacy or their own experience of access to the health care system. One study of 314 participants also found that black race was associated with worse health literacy, but this study did not assess potential mediators between race and health literacy.23 The generalizability of our results is enhanced by the fact that study patients were recruited from community-based practices across the United States. Clinical information was provided by clinicians responsible for providing ongoing heart failure care, and detailed review of inpatient and outpatient medical records was conducted.
Several issues should be considered in the interpretation of our results. First, these data derive from a clinical trial whose participants may not represent the general population of heart failure patients. Notably, Tele-HF participants were somewhat younger than potential participants who declined to participate in the trial, and younger than heart failure patients included in the National Health and Nutrition Examination Survey, in which 38% of blacks and 66% of whites were age 65 and older24 (compared with 23% and 58%, respectively, in our study). All patients were under the care of a cardiologist, which may further affect generalizability of our findings, and potentially attenuated the prevalence of limited access to health care among participants. The requirement for informed consent may have biased our estimates of health literacy, as those with limited literacy may have been more likely to decline participation. The REALM-R is a brief assessment of health literacy, and it is possible that a more exhaustive assessment, such as the Wide Range Achievement Test-Revised (WRAT-R)25, would have provided different estimates of health literacy in our study sample. We would not expect these potential biases of access to care and health literacy to have differential effects on black versus white participants, however. We used information about living alone as a measure of social support, and it is possible that a more complete assessment about sources and extent of support would provide more accurate information. Rates of missing data were generally quite low, except for social support (missing in 18% of black patients and 12% of whites); insurance status (missing in 16% of black patients and 11% of whites); education (missing in 16% of black patients and 11% of whites); and income (missing in 31% of black patients and 27% of whites). Although we retained “missing” as a distinct category for these variables in the sequential models, our multivariable results may have differed with more complete information, though the crude associations we observed would not be affected.
In conclusion, our findings highlight that important racial differences in health literacy and access to care exist among patients with heart failure. These differences persist even after adjustment for a broad range of potential mediators, including educational attainment, income, and insurance status. Interventions to improve outcomes for black patients with heart failure may benefit from efforts to improve access to health care, but our findings suggest that such efforts should extend beyond just providing health insurance. Achieving equity in the U.S. health care system is a national priority.26 Future research is needed to determine how best to reduce disparities in heart failure.
Fig 1.
Racial Differences in Health Literacy and Access to Health Care
Acknowledgments
This work was supported by R01 HL080228. Dr. Chaudhry is supported by a Beeson Career Development Award (K23 AG030986).
Abbreviations List
- SD
standard deviation
- OR
odds ratio
- CI
confidence interval
Appendix
A complete listing of sites that participated in the Tele-HF study is as follows:
Baylor University Medical Center, Baylor Heart & Vascular Institute, Dallas, TX
Bridgeport Hospital, Bridgeport, CT
Cardiology Consultants of South Florida, Tamarac, FL
Cardiology Associates, Mobile, AL
Cardiology Associates of New Haven, Guilford, CT
Cardiology Associates Research, LLC, Tupelo, MS
Cardiology Diagnostics, Ltd., St. Louis, MO
Cardiology Specialists, Ltd., Westerly, RI
Chabert Medical Center, Louisiana State University Health System, Houma, LA
Cooper Health System, Camden, NJ
The Dayton Heart Center, Dayton, OH
The Emory Clinic, Atlanta, GA
Forsyth Medical Center, Winston-Salem, NC
Hackensack Heart Failure Program, Hackensack, NJ
Heart Clinic of Louisiana, Marrero, LA
Howard University, Washington, DC
Indiana Heart Physicians, Indianapolis, IN
Iowa City Heart Center, Iowa City, IA
Loyola University Medical Center, Maywood, IL
MetroHealth Medical Center, Cleveland, OH
Morehouse School of Medicine, Atlanta, GA
New York University, New York, NY
Oregon Health & Science University (OHSU), Portland, OR
Piedmont Hospital Research Institute, Atlanta, GA
The Queen’s Medical Center, Honolulu, HI
Sentara Cardiovascular Research Institute, Norfolk, VA
St. Joseph’s Regional Medical Center, Paterson, NJ
St. Luke’s Hospital / Mid America Heart Institute, Kansas City, MO
Truman Medical Center Cardiology, Kansas City, MO
UCLA Harbor Medical Center, Torrance, CA
UC Irvine Medical Center, Orange, CA
University of Pittsburgh Medical Center (UPMC), Pittsburgh, PA
Washington University School of Medicine, St. Louis, MO
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trial Registration Information:
http://www.clinicaltrials.gov/ct2/show/NCT00303212?term=Yale+%2B+Heart+Failure&rank=1
Financial Disclosures:
The authors have no financial disclosures or conflicts of interest.
Relationship with industry: none
REFERENCES
- 1.Yancy CW. Heart failure in African Americans. Am J Cardiol. 2005;96:3i–12i. doi: 10.1016/j.amjcard.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 2.Dries DL, Exner DV, Gersh BJ, Cooper HA, Carson PE, Domanski MJ. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med. 1999;340:609–616. doi: 10.1056/NEJM199902253400804. [DOI] [PubMed] [Google Scholar]
- 3.Yancy CW. Heart failure in African Americans: a cardiovascular engima. J Card Fail. 2000;6:183–186. doi: 10.1054/jcaf.2000.17610. [DOI] [PubMed] [Google Scholar]
- 4.Alexander M, Grumbach K, Remy L, Rowell R, Massie BM. Congestive heart failure hospitalizations and survival in California: patterns according to race/ethnicity. Am Heart J. 1999;137:919–927. doi: 10.1016/s0002-8703(99)70417-5. [DOI] [PubMed] [Google Scholar]
- 5.Alexander M, Grumbach K, Selby J, Brown AF, Washington E. Hospitalization for congestive heart failure. Explaining racial differences. Jama. 1995;274:1037–1042. [PubMed] [Google Scholar]
- 6.Chaudhry SI, Barton B, Mattera JA, Spertus J, Krumholz HM. Randomized Trial of Telemonitoring to Improve Heart Failure Outcomes (Tele-HF): Study Design. Journal of Cardiac Failure. 13:709–714. doi: 10.1016/j.cardfail.2007.06.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 8.Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self-care of patients with heart failure. Ann Behav Med. 2008;35:70–79. doi: 10.1007/s12160-007-9003-x. [DOI] [PubMed] [Google Scholar]
- 9.Russell D, Taylor J. Living alone and depressive symptoms: the influence of gender, physical disability, and social support among Hispanic and non-Hispanic older adults. J Gerontol B Psychol Sci Soc Sci. 2009;64:95–104. doi: 10.1093/geronb/gbn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Health literacy: report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Jama. 1999;281:552–557. [PubMed] [Google Scholar]
- 11.Bass PF, 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18:1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 13.Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14:267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnipper JL, Roumie CL, Cawthon C, et al. Rationale and design of the Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study. Circ Cardiovasc Qual Outcomes. 3:212–219. doi: 10.1161/CIRCOUTCOMES.109.921833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21:427–440. doi: 10.3122/jabfm.2008.05.070287. [DOI] [PubMed] [Google Scholar]
- 18.Schoen C, Osborn R, Doty MM, Bishop M, Peugh J, Murukutla N. Toward higher-performance health systems: adults’ health care experiences in seven countries, 2007. Health Aff (Millwood) 2007;26:w717–734. doi: 10.1377/hlthaff.26.6.w717. [DOI] [PubMed] [Google Scholar]
- 19.Kamath SA, Drazner MH, Wynne J, Fonarow GC, Yancy CW. Characteristics and outcomes in African American patients with decompensated heart failure. Arch Intern Med. 2008;168:1152–1158. doi: 10.1001/archinte.168.11.1152. [DOI] [PubMed] [Google Scholar]
- 20.Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA. Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol. 2006;98:806–808. doi: 10.1016/j.amjcard.2006.03.066. [DOI] [PubMed] [Google Scholar]
- 21.Martin TC. Comparison of Afro-Caribbean patients presenting in heart failure with normal versus poor left ventricular systolic function. Am J Cardiol. 2007;100:1271–1273. doi: 10.1016/j.amjcard.2007.05.047. [DOI] [PubMed] [Google Scholar]
- 22.Philbin EF, DiSalvo TG. Influence of race and gender on care process, resource use, and hospital-based outcomes in congestive heart failure. Am J Cardiol. 1998;82:76–81. doi: 10.1016/s0002-9149(98)00233-1. [DOI] [PubMed] [Google Scholar]
- 23.Morrow D, Clark D, Tu W, et al. Correlates of health literacy in patients with chronic heart failure. Gerontologist. 2006;46:669–676. doi: 10.1093/geront/46.5.669. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Data. [Google Scholar]
- 25.Jastak S, Wilkinson G. Wide Range Achievement Test-Revised 3. Wilmington: 1993. [Google Scholar]
- 26.Institute of Medicine (U.S.). Committee on Quality of Health Care in America . Crossing the quality chasm : a new health system for the 21st century. National Academy Press; Washington, D.C.: 2001. [Google Scholar]