Abstract
Objective
Bone cement augmentation procedures such as percutaneous vertebroplasty and balloon kyphoplasty have been shown to be effective treatment for acute or subacute osteoporotic vertebral compression fractures. The purpose of this study was to determine the efficacy of bone cement augmentation procedures for long standing osteoporotic vertebral compression fracture with late vertebral collapse and persistent back pain.
Methods
Among 278 single level osteoporotic vertebral compression fractures that were treated by vertebral augmentation procedures at our institute, 18 consecutive patients were included in this study. Study inclusion was limited to initially, minimal compression fractures, but showing a poor prognosis due to late vertebral collapse, intravertebral vacuum clefts and continuous back pain despite conservative treatment for more than one year. The subjects included three men and 15 women. The mean age was 70.7 with a range from 64 to 85 years of age. After postural reduction for two days, bone cement augmentation procedures following intraoperative pressure reduction were performed. Imaging and clinical findings, including the level of the vertebra involved, vertebral height restoration, injected cement volume, local kyphosis, clinical outcome and complications were analyzed.
Results
The mean follow-up period after bone cement augmentation procedures was 14.3 months (range 12-27 months). The mean injected cement volume was 4.1 mL (range 2.4-5.9 mL). The unipedicular approach was possible in 15 patients. The mean pain score (visual analogue scale) prior to surgery was 7.1, which decreased to 3.1 at 7 days after the procedure. The pain relief was maintained at the final follow up. The kyphotic angle improved significantly from 21.2 ± 4.9° before surgery to 10.4 ± 3.8° after surgery. The fraction of vertebral height increased from 30% to 60% after bone cement augmentation, and the restored vertebral height was maintained at the final follow up. There were no serious complications related to cement leakage.
Conclusion
In the management of even long-standing osteoporotic vertebral compression fracture for over one year, bone cement augmentation procedures following postural reduction were considered safe and effective treatment in cases of non-healing evidence.
Keywords: Long standing, Compression fracture, Osteoporosis, Bone cement
INTRODUCTION
Acute osteoporotic vertebral compression fractures may produce intolerable pain. However, in a number of cases, the pain subsides over a period of weeks or months. Most patients achieve bone union without surgery. Thus, initially, most patients with painful osteoporotic vertebral compression fractures are treated conservatively with bed rest, analgesic medications, bracing and anti-osteoporotic drugs13,14,18). However, the non-operative measures for some symptomatic vertebral compression fractures may not be successful and the patient continues to have intolerable pain, kyphotic deformity, loss of function, or a combination of these problems. Some patients develop chronic pain and a spinal deformity. Vertebral augmentation procedures such as the percutaneous vertebroplasty or balloon kyphoplasty are minimally invasive procedures used to prevent further vertebral collapse and result in rapid pain relief in patients with osteoporotic vertebral compression fractures. However, these procedures have been shown to be effective in acute or subacute fractures, especially one to four months old and treatment after 6 months was thought to be not successful in relieving pain10,21). The treatment of long standing fractures, present for more than 1 year remains controversial. The purpose of this study was to evaluate the effect of bone cement augmentation for long standing osteoporotic vertebral compression fractures which showed late vertebral collapse and continuous back pain, present for more than 1 year.
MATERIALS AND METHODS
This study included 18 patients (15 females, 3 males) with osteoporotic vertebral compression fractures due to severe osteoporosis. Of the 278 single level osteoporotic vertebral compression fractures that were treated at our institute, 18 patients were included in this study. Study inclusion was limited to first, initially with minimal compression fractures; collapsed vertebra and vacuum clefts were present at more than one year follow up, second, in patients with incapacitating continuous back pain despite a variety of conservative treatments. A minimal compression fracture was defined as vertebrae that had collapsed to not more than 80% of their original heights. A collapse was defined by vertebrae that had collapsed to more than 50% of their original heights. Vacuum clefts were defined as areas in the collapsed vertebral body that were gas-like with radiolucency observed in the extension stress view or abnormal signal intensity on MR imaging suggesting avascular necrosis11). MR imaging features of intravertebral clefts, which are varied in appearance, depending on whether they are filled with gas or fluid at the time of imaging. Avascular necrosis usually has a low signal on T1-weighted images and high signal on T2-weighted images. After postural reduction for two days, bone cement augmentation procedures following postural reduction were performed in all patients. The mean age of the patients was 70.7 years with range from 64 to 85. The mean follow-up period after bone cement augmentation procedures was 14.8 months and ranged from 12 to 27 months. Two patients had received steroid therapy due to asthma and nephritis. All patients with T-scores lower than -3.0 by BMD were considered to have severe osteoporosis; the mean T-score of the patients included in this study was -3.82. Lateral radiographs were taken and analyzed at four different points in time; 1) at first admission after injury, 2) preoperative lateral (after conservative treatment including bed rest, medications, and bracing), 3) postoperative lateral (including postural reduction for two days before procedures and intraoperative pressure reduction), and 4) at final follow-up.
The vertebral height of the fractured vertebra was defined as the distance between identical points on the superior and inferior endplates at the anterior (Haf, line ac) portion. The vertebral height of the normal vertebra was defined as the distance between identical points on the superior and inferior endplates at the anterior portion at adjacent below vertebral body (Han, line eg). The relative anterior height (Ha = Haf / Han) was then calculated. The kyphotic angle was measured as the angle in degrees defined by the intersection of the superior and inferior endplates of the fractured body (line ab & cd) (Fig. 1).
Fig. 1.
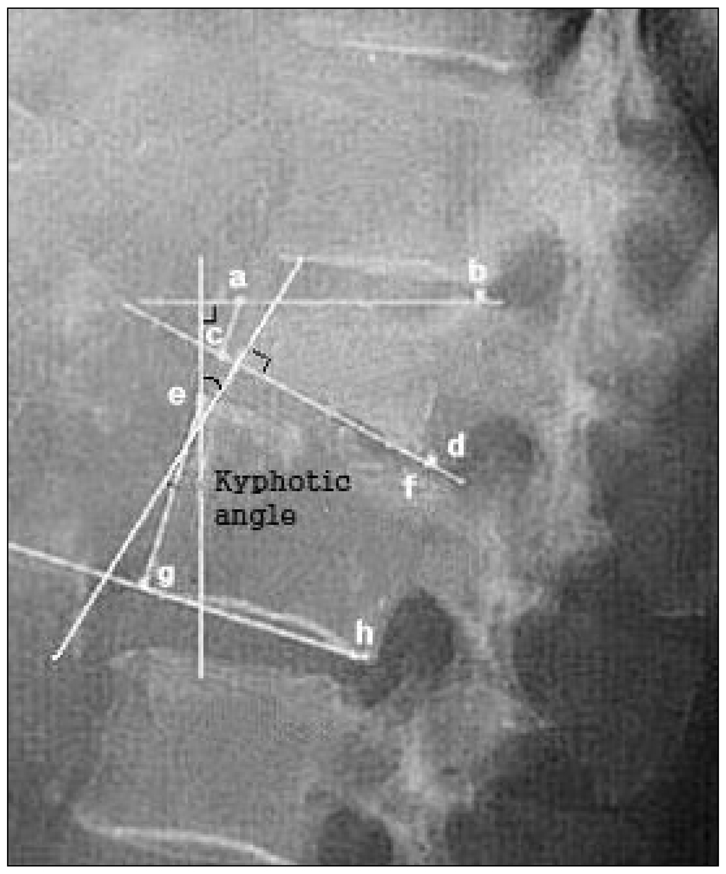
Measurement of kyphotic angle, normal anterior (Han, line ac) vertebral height and fracture anterior (Haf, line eg) vertebral height. The relative anterior heights were reported as fractions of the referenced height (Ha = Haf / Han).
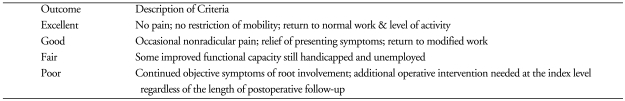
The patients were evaluated according to a modified version of MacNab's criteria (Table 1) and using the visual analogue scale (VAS) for characterizing the clinical outcome after spinal surgery. Statistical analysis, including mean values (MV) and standard deviations (SD), was performed using SAS 6.12 (SAS Institute, Inc., Cary, NC, USA). Comparisons between different points in time were performed using the paired Student's t-test. Differences were considered statistically significant at p < 0.05.
Table 1.
Modified MacNab's criteria for characterizing the outcome after spinal surgery
RESULTS
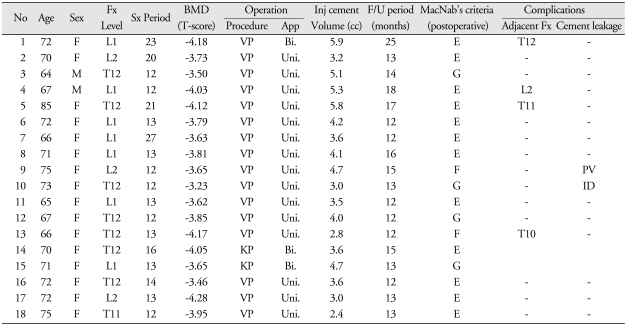
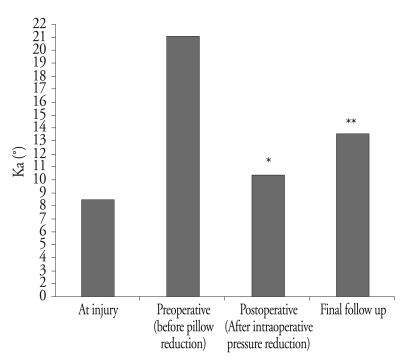
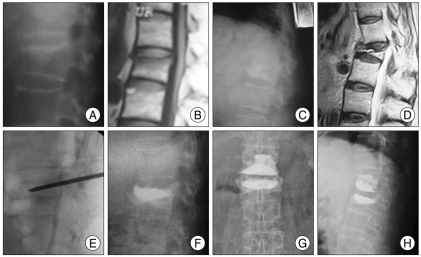
All fractures occurred in the thoracolumbar junction. The levels were T11 (n = 1), T12 (n = 7), L1 (n = 7) and L2 (n = 3). Percutaneous vertebroplasty was performed in 16 patients, and balloon kyphoplasty was performed in 2 patients (Table 2). The mean length of time from initial injury to the bone cement augmentation procedure was 15 months. The mean injected cement volume was 4.1 mL (range 2.4-5.9 mL). Unipedicular percutaneous vertebroplasty was performed in 15 patients and bipedicular cement injection was performed in three patients. The kyphotic angle improved significantly from 21.2 ± 4.9° before surgery to 10.4 ± 3.8° after surgery. The improved alignments were maintained on a true lateral X-ray at the final follow-up evaluation. At the final follow up visit, the mean correction loss for the kyphotic deformity was a 3.2° from the angle after procedure (Fig. 2). The fraction of involved vertebral height also increased significantly from 0.30 ± 0.12 to 0.60 ± 0.10 (p < 0.05). The mean pain score (visual analogue scale) prior to vertebroplasty was 7.1, which decreased to 3.1 at 7 days after procedure. Pain relief was maintained and no patient complained of aggravated pain at the final follow up visit. No patient experienced neurological deterioration as a result of the procedure. All patients subjectively reported relief of their pain, and none of them complained of severe worsening of pain during the follow-up (Fig. 3). Sixteen patients were graded as having an excellent or good result according to modified MacNab's criteria (Excellent : 12, Good : 4, Fair : 2). Asymptomatic cement leakage into the paravertebral area or adjacent upper disc occurred in two patients. However, there were no major complications such as spinal cord compression, pulmonary embolism, or serious infection. During the follow up, another fracture occurred on the adjacent level in 4 patients; these fractures were also successfully treated by bone cement augmentation with vertebroplasty or kyphoplasty (Fig. 4).
Table 2.
Demographic and clinical characteristics of the patients
No : number, Fx : fracture, Sx : symptom, BMD : bone mineral densitometry, OP : operative, Redu : reduction, F/U : follow-up, Inj : injection, VP : vertebroplasty, KP: kyphoplasty, App : approach, Uni : unipedicular, Bi : bipedicular, PV : paravertebral, ID : intradiscal
Fig. 2.
Changes of kyphotic angle after bone cement augmentation procedures. Values are given as mean ± SD; comparisons by means of paired t-test. *p < 0.01 for preoperative versus postoperative, **p < 0.05 for preoperative versus final follow up.
Fig. 3.
Osteoporotic compression fracture at T12 level in a 64-year-old man. A : Simple lateral radiograph at initial injury shows minimal compression fracture at T12. B : T12 body had collapsed 3 months after injury. C, D and E : T12 body had more collapsed 12 months after injury and vacuum cleft was observed in extension stress view. F and G : Simple radiographs obtained after percutaneous vertebroplasty show complete filling of T12 body without any leakage.
Fig. 4.
Osteoporotic compression fracture at L1 level in a 72-year-old woman. A and B : Simple lateral radiograph and magnetic resonance image show minimal compression fracture at L1. C and D : L1 vertebral body had seriously collapsed 23 months after injury and intravertebral fluid was observed in the T2-weighted magnetic resonance image. E : Vertebroplasty needle insertion is shown after intraoperative pressure reduction. F : Postoperative simple radiograph after percutaneous vertebroplasty shows effective filling of L1 body without any leakage. G and H : Another fracture that occured on the adjacent upper level at 7 months after percutaneous vertebroplasty, and this was also effectively treated by percutaneous vertebroplasty.
DISCUSSION
Osteoporotic compression vertebral fractures are common and a leading cause of disability and morbidity in the elderly9). The pain associated with acute osteoporotic vertebral compression fractures may be initially intolerable. In a number of cases, the pain subsides over a period of several weeks or months17). However, some patients develop secondary vertebral collapse or intravertebral vacuum clefts, which can trigger continuous back pain and kyphotic deformity and it is possible that the pain can become chronic after conservative treatments without surgical management20).
Bone cement augmentation procedures such as percutaneous vertebroplasty and balloon kyphoplasty have been widely used to treat painful osteoporotic compression fractures. However, these procedures have been shown to be effective for acute and subacute fractures, especially for those fractures that are less than four months old10,19). One study reported good result treating a post traumatic osteoporotic vertebral compression fracture that was 5-years-old, and another study reported successful management of chronic symptomatic compression fractures with percutaneous vertebroplasty4,8). They insisted that chronic symptomatic osteoporotic compression fracture, even showing isointense on T1-weighted images, could be caused by compressive force acting on the nociceptor endings in the bone marrow. Enhancing the rigidity and strength by bone cement reduces bone deformation and painful micromotion at the fracture site. Moreover, pain relief can be thought to be induced by the destruction of sensitive nerve endings in the matrix by the bone cement, which is directly toxic due to enhanced production of free radicals and heating during polymerization. Despite these reports, outcomes in patients with chronic fractures treated by bone cement augmentation have still remained unclear.
The causes of chronic pain after osteoporotic vertebral compression fracture are caused by : 1) incomplete vertebral healing with progressive osseous collapse, 2) altered spine kinematics as a consequence of spinal deformity, or 3) the development of a pseudarthrosis at the involved vertebra6). These problems can also lead to an impaired quality of life and depression. Kümmell first described delayed post-traumatic vertebral collapse in 1895. There are many possible explanations for these events, such as poor nutrition, vascular disruption with microhemorrhage and thrombosis, and biomechanical failure3,7,12,15,16). However, understanding of the exact causes of this entity remains unclear. Some investigators agree that the intraosseous vacuum phenomenon results from a vascular insult causing secondary bone necrosis2). Others suggest that the cleft in the affected vertebral body of the osteoporotic spine is a false joint lined by fibrocartilaginous tissue and significant movement consistent with a pseudarthrosis. The radiographic signs of this disease have been described as the presence of a band-like radiolucency in a collapsed vertebral body, referred to as an intraosseous vacuum cleft. The cleft is hypointensive on the T1-weighted MRI scans. On T2-weighted images, the cleft may be either hypointensive or hyperintensive, depending on whether it is occupied by gas or fluid. In a study of vertebral collapse, the vacuum phenomenon was seen in 15% of patients by plain radiography and in 21% when all imaging modalities were considered13). Magnetic resonance imaging helped to show the cleft when the findings of the radiographs were ambiguous or unclear. Kim et al.11) suggested that flexion-extension radiographs obtained in patients with osteoporotic compression fractures increases the detection of the intravertebral vacuum phenomenon.
There has been an attempt to classify the several seemingly minor differences in shape of the vertebrae in the early radiographs, to better predict the prognosis of vertebral compression fractures in the elderly, and to clarify the relationship between the initial radiographs and the clinical results. Ito et al.7) reported the pathogenesis of progression to delayed vertebral collapse, and the initial radiograph of their case indicated a bow-shaped type. Moreover, an intravertebral cleft and instability of the affected vertebra were risk factors for late collapse resulting in neurological deficits. They concluded that the correct initial diagnosis and immobilization were important factors in preventing delayed collapse with neurological deficits. Sugita et al.22) classified the early features into five types based on lateral radiographs : the swelled-front-type, bow-shaped-type, and projecting-type fractures had a poor prognosis with late collapse and commonly showed a vacuum cleft. On the other hand, the concave and dented-type of fractures had a good prognosis and achieved almost complete fusion without surgical treatment. However, in this series, we did not analyze the relationship between the fractures type and frequency of late collapse due to the non specific diagnosis of the initial fracture types. A substantial correction of kyphosis and the restoration of anterior vertebral height could be obtained by extended posture despite the long standing length of time from the initial injury. In addition to using the technique of postural reduction, we found that placing bolsters under the chest and pelvis, to hyperextend the spine while patients were in a prone position, helped restore the vertebral body height and enlarge the vacuum cleft. This study shows that bone cement can fill easily the entire vacuum cleft usually via the unipedicular approach in most patients. Due to the pre-existent cleft, the majority of the procedures could be performed successfully via the unipedicular approach. The usefulness of postural reduction for a thoracolumbar spinal fracture and conservative treatment of compression fractures with postural reduction have been advocated by many authors5). Bedbrook1) noted that 90% of the fractures of the thoracic and lumbar spine could be treated using this closed method. Although intravertebral clefts are thought to represent trabecular defects caused by bone destruction associated with fractures, within the post-traumatic period, there is the risk of progression, destruction of new trabeculae, and circulatory disturbances. These conditions can result in disturbances and delays in the normal healing process of the fracture resulting in nonunion. Therefore, postural reduction in the supine hyperextended position and intraoperative pressure reduction can re-expand the collapsed vertebral body in patients with an intravertebral cleft. The results of this study suggest that patient selection for vertebral augmentation procedures should not be based on the stage of the compression fracture but rather on evidence of non-healing on the dynamic stress radiographs or MR images as well as the degree of persistent pain.
CONCLUSION
Kyphotic deformity and chronic pain caused by long-standing osteoporotic vertebral compression fractures may occur and limit the patient's activities of daily living as well as quality of life. Patients with long-standing but non-healing osteoporotic compression fractures can be successfully managed with bone cement augmentation procedures following postural reduction and intraoperative pressure reduction.
References
- 1.Bedbrook GM. Stability of spinal fractures and fracture dislocations. Paraplegia. 1971;9:23–32. doi: 10.1038/sc.1971.3. [DOI] [PubMed] [Google Scholar]
- 2.Bhalla S, Reinus WR. The linear intravertebral vacuum : a sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170:1563–1569. doi: 10.2214/ajr.170.6.9609175. [DOI] [PubMed] [Google Scholar]
- 3.Brower AC, Downey EF., Jr Kümmell disease : report of a case with serial radiographs. Radiology. 1981;141:363–364. doi: 10.1148/radiology.141.2.7291557. [DOI] [PubMed] [Google Scholar]
- 4.Brown DB, Gilula LA, Sehgal M, Shimony JS. Treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol. 2004;182:319–322. doi: 10.2214/ajr.182.2.1820319. [DOI] [PubMed] [Google Scholar]
- 5.Chin DK, Kim YS, Cho YE, Shin JJ. Efficacy of Postural Reduction in Osteoporotic Vertebral Compression Fractures Followed by Percutaneous Vertebroplasty. Neurosurgery. 2006;58:695–700. doi: 10.1227/01.NEU.0000204313.36531.79. [DOI] [PubMed] [Google Scholar]
- 6.Gold DT. The clinical impact of vertebral fractures : quality of life in women with osteoporosis. Bone. 1996;18(3 Suppl):185S–189S. doi: 10.1016/8756-3282(95)00500-5. [DOI] [PubMed] [Google Scholar]
- 7.Ito Y, Hasegawa Y, Toda K. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2:101–106. doi: 10.1016/s1529-9430(01)00165-6. [DOI] [PubMed] [Google Scholar]
- 8.Irani FG, Morales JP, Sabharwal T, Dourado R, Gangi A, Adam A. Successful treatment of a chronic post-traumatic 5-year-old osteoporotic vertebral compression fracture by percutaneous vertebroplasty. Br J Radiol. 2005;78:261–364. doi: 10.1259/bjr/55389916. [DOI] [PubMed] [Google Scholar]
- 9.Johnell O. Advances in osteoporosis: better identification of risk factors can reduce morbidity and mortality. J Intern Med. 1996;239:299–304. doi: 10.1046/j.1365-2796.1996.429781000.x. [DOI] [PubMed] [Google Scholar]
- 10.Kaufmann TJ, Jensen ME, Schweickert PA, Marx WF, Kallmes DF. Age of fracture and clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2001;22:1860–1863. [PMC free article] [PubMed] [Google Scholar]
- 11.Kim DY, Lee SH, Jang JS, Chung SK, Lee HY. Intravertebral vacuum phenomenon in osteoporotic ompression fracture: Report of 67 patients with quanitative evaluation of intravertevbral instability. J Neurosurg. 2004;100(1 Suppl Spine):24–31. doi: 10.3171/spi.2004.100.1.0024. [DOI] [PubMed] [Google Scholar]
- 12.Kumpan W, Salomonowitz E, Seidl G, Wittich GR. The intravertebral vacuum phenomenon. Skeletal Radiol. 1986;15:444–447. doi: 10.1007/BF00355102. [DOI] [PubMed] [Google Scholar]
- 13.Lafforgue PF, Chagnaud CJ, Daver LM, Daumen-Legré VM, Peragut JC, Kasbarian MJ, et al. Intervertebral disk vacuum phenomenon secondary to vertebral collapse: prevalence and significance. Radiology. 1994;193:853–858. doi: 10.1148/radiology.193.3.7972837. [DOI] [PubMed] [Google Scholar]
- 14.Lukert BP. Vertebral compression fractures: how to manage pain, avoid disability. Geriatrics. 1994;49:22–26. [PubMed] [Google Scholar]
- 15.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129:23–29. doi: 10.1148/129.1.23. [DOI] [PubMed] [Google Scholar]
- 16.Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, et al. Intravertebral vacuum cleft : changes in content after supine positioning. Radiology. 1993;187:483–487. doi: 10.1148/radiology.187.2.8475295. [DOI] [PubMed] [Google Scholar]
- 17.Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine. 1993;18:955–970. [PubMed] [Google Scholar]
- 18.Rapado A. General management of vertebral fractures. Bone. 1996;18(3 Suppl):191S–196S. doi: 10.1016/8756-3282(95)00501-3. [DOI] [PubMed] [Google Scholar]
- 19.Ryu KS, Park CK. The Prognostic Factors Influencing on the Therapeutic Effect of Percutaneous Vertebroplasty in Treating Osteoporotic Vertebral Compression Fractures. J Korean Neurosurg Soc. 2009;45:16–23. doi: 10.3340/jkns.2009.45.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13(Suppl 2):S27–S31. doi: 10.1016/8756-3282(92)90193-z. [DOI] [PubMed] [Google Scholar]
- 21.Stallmeyer MJ, Zoarski GH, Obuchowski AM. Optimizing patient selection in percutaneous vertebroplasty. J Vasc Interv Radiol. 2003;14:683–696. doi: 10.1097/01.rvi.0000064859.87207.fa. [DOI] [PubMed] [Google Scholar]
- 22.Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T. Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech. 2005;18:376–381. doi: 10.1097/01.bsd.0000168716.23440.61. [DOI] [PubMed] [Google Scholar]