Abstract
Paraplegia following spinal epidural anesthesia is extremely rare. Various lesions for neurologic complications have been documented in the literature. We report a 66-year-old female who developed paraplegia after left knee surgery for osteoarthritis under spinal epidural anesthesia. In the recovery room, paraplegia and numbness below T4 vertebra was checked. A magnetic resonance image (MRI) scan showed a spinal thoracic intradural extramedullary (IDEM) tumor. After extirpation of the tumor, the motor weakness improved to the grade of 3/5. If a neurologic deficit following spinal epidural anesthesia does not resolve, a MRI should be performed without delay to accurately diagnose the cause of the deficit and optimal treatment should be rendered for the causative lesion.
Keywords: Spinal epidural anesthesia, Spinal intradural extramedullary tumor
INTRODUCTION
Neurologic complications following spinal epidural anesthesia are rare. Horlocker et al.5) reported that neurologic complications related to spinal epidural anesthesia occurred in 6 of 30,413 patients (0.02%). Nevertheless, neurologic complications following spinal epidural anesthesia can be devastating to the patient6,12). Various causes for neurologic complications have been documented in the literature2,6,7). Paraplegia due to an incidental spinal tumor following spinal epidural anesthesia is extremely rare1). Nicholson and Everson first reported sudden paralysis after spinal epidural anesthesia in a patient with a metastatic spinal tumor in 194610). We report a patient who developed paraplegia and numbness following spinal epidural anesthesia for a total knee arthroplasty and underwent emergency surgery for a previously unrecognized thoracic intradural extramedullary (IDEM) tumor, which was thought to be the cause of neurologic complication.
CASE REPORT
A 67-year-old female with pain in the left knee for 3 months was diagnosed with osteoarthritis and admitted orthopedic surgery. For 18 months, she had complained of squeezing pain in the chest, which was suspicious for angina pectoris, however, there were no remarkable abnormalities on cardiac evaluation. She had taken medications for hypertension for 5 years. On laboratory findings, no abnormal hematologic findings were noted. In the operating room, using a 23G spinal needle with the patient in the left lateral position, 10 mg of bupivacaine was injected into the L3-L4 interspace. She underwent a total left knee arthroplasty of 120 minutes duration. Post-operatively, she was transferred to the recovery room and complained of motor weakness and a sensory disturbance. On neurologic exam, complete paraplegia and numbness was checked in both legs. Initially, it was thought that the residual effect of spinal epidural anesthesia had lasted for a prolonged time period, thus she was observed closely without radiologic evaluation. After 8 hours, the persistent paraplegia and numbness were thought to represent a myelopathy. Thus, a MRI was performed for exclusion of other lesions. A whole spine MRI scan showed a thoracic spinal mass involving the T2 vertebra level and no hematoma, except multiple bulging lumbar discs (Fig. 1). The thoracic spinal mass was homogenous-enhanced and a left eccentric spinal IDEM tumor (Fig. 2). She was transferred to the neurosurgery service. On further neurologic exam, the Babinski and Chaddock signs were positive bilaterally and hyper-reactive deep tendon reflex was checked with a decrease in anal sphincter tone. Temperature sense and pain below T4 vertebra was lost. Emergency surgery was planned. Under general anesthesia, a left hemilaminectomy of T1, T2, and T3 with total removal of the tumor mass was performed. A meningioma of meningotheliomatous type was confirmed (Fig. 3). One week later, motor weakness improved to a grade of 3/5 and numbness existed in the soles of the feet bilaterally and the left distal calf. Four weeks later, she could stand with minimal assistance. She was transferred for the extensive rehabilitation program.
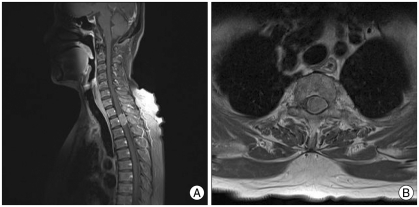
Fig. 1.
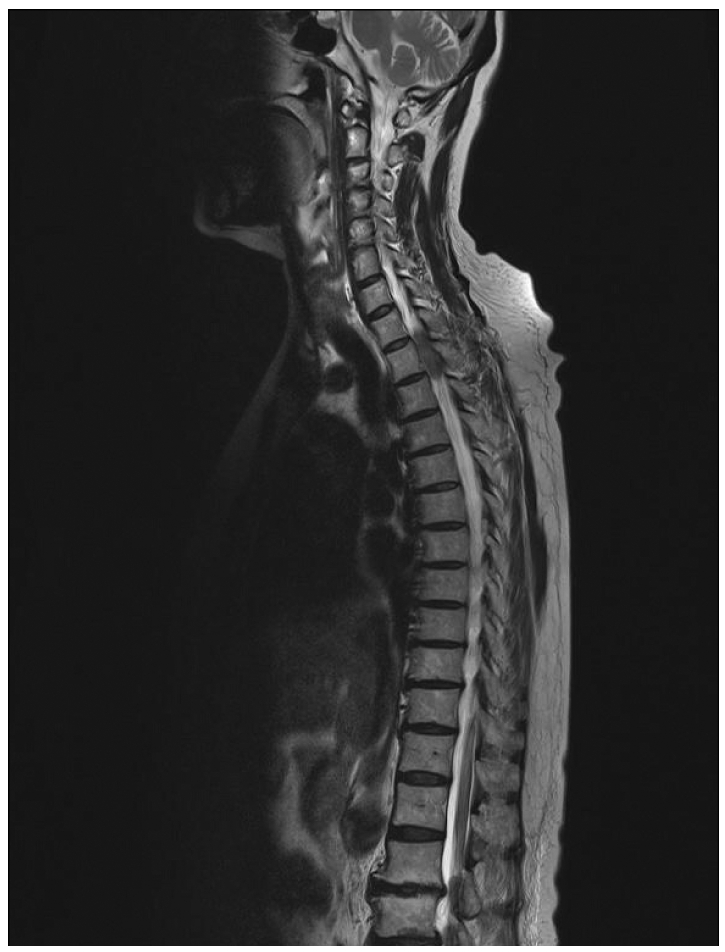
Whole spine magnetic resonance imaging findings. T2-weighted saggital scan shows homogenous low signal mass in T2 vertebra level and no hematoma, except multiple bulging discs in L2/3, L3/4, L4/5, and L5/S1.
Fig. 2.
Thoracic spine magnetic resonance imaging findings. Enhanced studies show well demacrated and homogenously enhanced intradural extramedullary tumor in T2 vertebra level (A) and left eccentric tumor mass compressing the spinal cord (B). A : sagittal section. B : axial section.
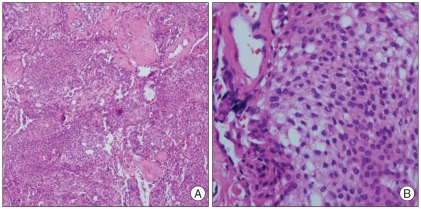
Fig. 3.
Pathologic findings. Histologic section discloses vague whorling pattern of tumor cells and scattered psammoma bodies (A). Tumor cells are usually uniform, with oval nuclei and on occasion intranuclear inclusions (B). A : Hematoxylin and eosin stain, ×100. B : Hematoxylin and eosin stain, ×400.
DISCUSSION
Though rare, neurologic complications, like paresthesias, cauda equina syndrome and paraplegia following spinal epidural anesthesia are reported in the literature2,6,7,10,12). For causes of neurologic sequelae, direct trauma by direct needle injury, anesthetic drug factor, management-related factors, and underlying space-occupying lesions are documented2,6,7,10). First, direct trauma by spinal needle injury is usually related to multiple attempts with spinal cord or nerve root injuries7). Kane reported that hematomas by spinal needle injury can lead to paraplegias by spinal cord compression7). Indeed, if a patient has hemostatic abnormalities, it is considered that the cause of paraplegia after spinal epidural anesthesia is spinal hematoma13). In our case, based on the laboratory examination before total knee arthroplasty, the patient did not have hemostatic abnormalities and post-operatively, the MRI scan did not show any lesions, such as hematomas in the lumbar region. Second, local anesthetic drugs can directly irritate nerve roots by osmotic effects11). Also, the addition of epinephrine can induce vasospasm and ischemic injury of spinal arteries7). Recently, the incidence of neurologic complications following spinal epidural anesthesia has decreased with the use of a lower concentration of the local anesthetic drug3). Third, for management related factors, the main cause of paraplegia following spinal epidural anesthesia is hypotension, which can induce spinal cord ischemia and thromobosis of the spinal arteries7). In our patient, during the total knee arthroplasty, hypotension was not recorded in the anesthetic record. Fourth, the mechanism of neurologic damage following spinal epidural anesthesia with underlying space-occupying lesions, such as spinal tumors, is still unknown.Nicholson reported that the cause of neurologic complications following spinal epidural anesthesia is the blockade of cerebrospinal fluid by space-occupying lesions. The injected drug cannot be diluted and stagnated with the accumulation of drug, which can induce neurologic toxicity10). Another mechanism leading to neurologic complications is spinal coning. Hollis reported that spinal coning results from compartmental pressure differences. The lumbar puncture exacerbates the dangerous pressure differentials above and below the spinal tumor and can induce neurologic complications. The incidence of spinal coning is between 14% and 26%4). Hollis suggested that another mechanism for neurologic complications is epidural venous engorgement exacerbated by lumbar puncture, thus compromising venous drainage from the spinal cord below the tumor mass4).
Of patients with spinal cord lesions, 80-95% experience back pain during the course of their disease8). The small lesion in the spinal cord may not have any symptoms and neurologic deficits9). In our case, the patient had complained of chest pain for 18 months. Because it was suspicious for angina pectoris, and only cardiac evaluation was done and no remarkable abnormalities were noted. Thus, a spinal tumor was not suspected and no work-up was performed pre-operatively. In this case, the chest pain likely have been caused by spinal IDEM tumor involving the T2 vertebra level (Fig. 1).
In our case, about 8 hours passed until the radiologic evaluation was performed. It is not easy to differentiate whether a neurologic deficit following a spinal block results from the residual effect of anesthetic drugs. In such cases, there are no guidelines about the time of the observation considering the residual effect of the drug. If a patient shows persistent neurologic symptoms post-operatively, a careful neurologic exam should be performed and a MRI scan should be done within hours with the consideration of other lesions.
CONCLUSION
Despite the low incidence of neurologic complications following spinal epidural anesthesia, it can lead to serious neurologic sequelae. If a patient is scheduled to undergo surgery by spinal epidural anesthesia, a complete history and a careful neurologic examination is essential. If neurologic deficits following spinal epidural anesthesia do not recover within hours, a MRI scan should be done without delay to exclude spinal lesions compressing the spinal cord.
Acknowledgements
This work was supported for two years by Pusan National University Research Grant.
References
- 1.Cherng YG, Chen IY, Liu FL, Wang MH. Paraplegia following spinal anesthesia in a patient with an undiagnosed metastatic spinal tumor. Acta Anaesthesiol Taiwan. 2008;46:86–90. doi: 10.1016/S1875-4597(08)60033-8. [DOI] [PubMed] [Google Scholar]
- 2.Faccenda KA, Finucane BT. Complications of regional anesthesia. Drug Saf. 2001;24:413–442. doi: 10.2165/00002018-200124060-00002. [DOI] [PubMed] [Google Scholar]
- 3.Greene NM. Neurological sequelae of spinal anesthesia. Anesthesiology. 1961;22:682–698. doi: 10.1097/00000542-196109000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hollis PH, MAlis LI, Zappulla RA. Neurological deterioration after lumbar puncture below complete spinal subarachnoid block. J Neurosurg. 1986;64:253–256. doi: 10.3171/jns.1986.64.2.0253. [DOI] [PubMed] [Google Scholar]
- 5.Horlocker TT, Abel MD, Messick JM, Jr, Schroeder DR. Small risk of serious neurologic complications related to lumbar epidural catheter placement in anesthetized patients. Anesth Analg. 2003;96:1547–1552. doi: 10.1213/01.ANE.0000057600.31380.75. [DOI] [PubMed] [Google Scholar]
- 6.Horlocker TT. Complications of spinal and epidural anesthesia. Anesthesiol Clin North America. 2000;18:461–485. doi: 10.1016/s0889-8537(05)70172-3. [DOI] [PubMed] [Google Scholar]
- 7.Kane RE. Neurologic deficits following epidural or spinal anesthesia. Anesth Analg. 1981;60:150–161. [PubMed] [Google Scholar]
- 8.Lewis DW, Packer RJ, Raney B, Rak IW, Belasco J, Lange B. Incidence, presentation and outcome of spinal cord disease in children with systemic cancer. Pediatrics. 1986;78:438–443. [PubMed] [Google Scholar]
- 9.Livingston K, Parrin RG. The neurosurgical management of spinal metastases causing cord and cauda equina compression. J Neurosurg. 1978;49:839–843. doi: 10.3171/jns.1978.49.6.0839. [DOI] [PubMed] [Google Scholar]
- 10.Nicholson MJ, Everson UH. Neurologic complications of spinal anesthesia. J Am Med Assoc. 1946;132:679–685. doi: 10.1001/jama.1946.02870470005002. [DOI] [PubMed] [Google Scholar]
- 11.Noble AB, Murray JG. A review of the complications of spinal anesthesia with experience in Canadian teaching hospitals from 1959 to 1969. Can Anaesth Soc J. 1971;18:5–17. doi: 10.1007/BF03025422. [DOI] [PubMed] [Google Scholar]
- 12.Seigne TD. Aseptic meningitis following spinal analgesia. Anaesthesia. 1970;25:402–407. doi: 10.1111/j.1365-2044.1970.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 13.Vandermeulen EP, Van Aken H, Vermylen J. Anticuagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165–1177. doi: 10.1213/00000539-199412000-00024. [DOI] [PubMed] [Google Scholar]