Abstract
We report a rare case of fibrous dysplasia with the development of a secondary aneurysmal bone cyst presenting as solitary tumor of calvarium. Although fibrous dysplasia with aneurysmal bone cyst is rare, it should be taken into account in differential diagnosis of the osteolytic solitary skull lesion.
Keywords: Aneurysmal bone cyst, Fibrous dysplasia, Skull
INTRODUCTION
Fibrous dysplasia (FD) is a benign skeletal disorder, first described by Lichtenstein, in which abnormal development of fibroblast replaces medullary bone with fibrocellular tissue6,9,14). Among them, craniofacial FD represents approximately 7% of benign bone tumors7). The three most common radiological features of FD are pagetoid, sclerotic, and cystic patterns8). Computed tomographic (CT) scans show widening of diploic spaces, osseous expansion, and ground glass opacity12). Magnetic resonance image (MRI) reveals typically low signal intensity on T1- and T2-weighted images with contrast enhancement2).
Aneurysmal bone cyst (ABC) is an expanding osteolytic lesion superimposed on an existing pathological process of the bone11). ABC appears on plain X-rays as an ovoid lesion with varying degrees of diploic expansion or cortical thinning11). CT scan reveals an expansile bony cyst and MRI demonstrates high signal intensity on T1-weighted images, indicating hemorrhagic transformation5,11). On histopathology, ABC appears as blood-filled cavernous spaces with a paucity of endothelial cells. The cysts are separated by septa composed of fibrous tissue, which contain multinucleated giant cells and osteoid tissue3). ABC involves most commonly in the vertebrae and long bone. However, only a few cases of ABC affecting the calvarium have been reported. Moreover, the occurrence of a concomitant FD and ABC in calvarium is exceedingly rare. In the search of literature using Medline, only 10 cases including our report were retrieved1,10,13,16,18,20) (Table 1). Although the mechanism of the occurrence of FD with ABC is unknown, there is a report that a secondary form of ABC may arise from a disruption in the osseous circulation caused by primary lesion4).
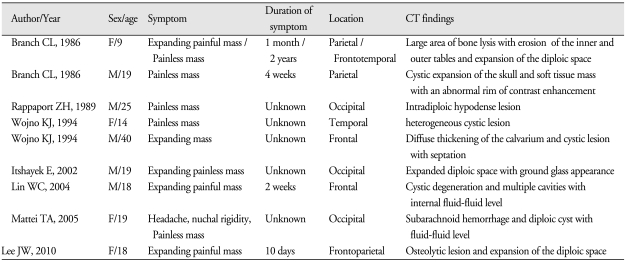
Table 1.
Summary of published cases of fibrous dysplasia in combination with aneurysmal bone cyst presenting with solitary lesion of calvarium
Here, we report a rare case of FD in combination with ABC on the frontoparietal bone presenting as rapidly growing solitary scalp mass with review of literature.
CASE REPORT
This 18-year-old girl presented with painful scalp mass on the right frontoparietal region, 3 cm in diameter. She had no specific medical history and her general condition was good. She experienced severe headache of abrupt-onset 10 days ago and noticed a newly developed scalp mass on the right frontoparietal region. Physical examination was normal except for a bulging, tender scalp mass on the right frontoparietal region. She was neurologically intact. Routine laboratory data, including serum calcium, phosphorus, and alkaline phosphatase, were within normal limits.
A plain skull X-ray revealed an irregular osteolytic lesion involving skull vault (Fig. 1). Brain computed tomography scans showed approximately 2.5 cm sized, lobulated, osteolytic lesion over the right frontoparietal bone (Fig. 2). The center of the lesion was eccentric to the calvaria. As a consideration of her age and radiographic findings, it was initially regarded to be an eosinophilic granuloma involving skull. Plain X-rays and radionuclide bone scan were taken for other long bones and vertebrae for seeking evidence of histiocytosis, but there were no osteolytic bone lesions other than calvarial one.
Fig. 1.

Plain roentgenogram of the skull, lateral view, showing a lobulated osteolytic lesion on the right frontoparietal skull.
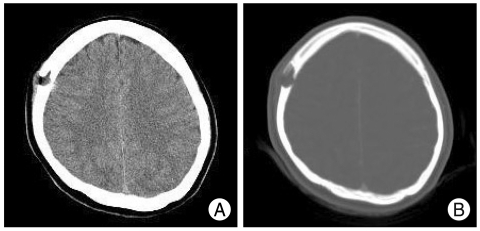
Fig. 2.
Computerized tomographic scans (A) with bone setting (B) revealing an osteolytic lesion with erosion of the inner and outer skull tables and expansion of the diploic space in the right frontoparietal area.
During operation, a dark hemorrhagic cystic lesion was attached to the subcutaneous tissue and had completely eroded the inner and outer tables of skull, but there was no evidence of invasion of the dura. At the margins of the lesion, the skull was thickened and gritty in an area 1 to 1.5 cm around the lesion. En-bloc resection of the bony lesion including surrounding healthy bone enough to clear resection margin and curettage of the soft tissue involvement were performed. The cranial defect was repaired with the molded methyl methacrylate plate. After operation, no neurological deficit was found and a good cosmetic result was achieved.
On histopathological examination, the two different components were noted. The tissue removed from the solid component was composed of overgrowth of fibrous matrix and haphazardly scattered bony trabeculae characteristic of FD (Fig. 3). And, tissue removed from the cystic component showed cystic spaces containing red blood cells separated by septa containing spindle cell and multinucleated giant cells characteristic of ABC (Fig. 4). The final pathologic findings were consistent with FD in combination with ABC.
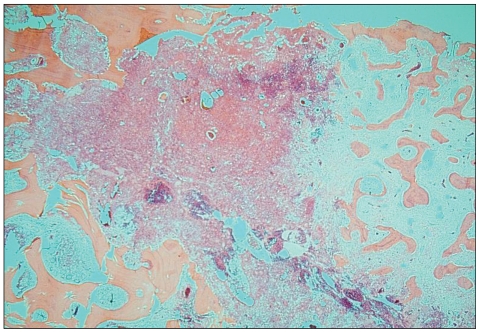
Fig. 3.
Photomicrograph demonstrating abundant fibrous stroma and irregularily arranged woven bone spicules revealing no conspicuous rimming consistent with fibrous dysplasia (H&E stain, original magnification ×20).
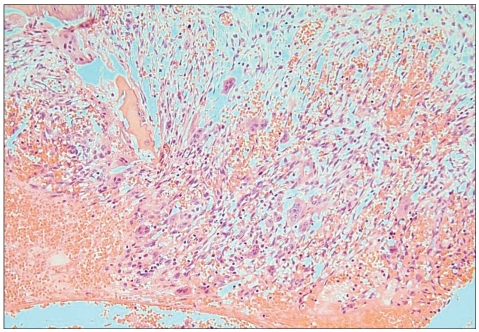
Fig. 4.
Photomicrograph showing blood filling cavernous space surrounded by multinucleated osteoclastic giant cells, proliferating fibroblasts and capillaries (H&E stain, original magnification ×200).
DISCUSSION
FD with ABC presenting with solitary calvarial lesion is an extremely rare entity. This lesion is first reported by Branch1) in 1986. The primary diseases known to be associated with ABC are osteoclastoma, osteosarcoma, osteoblastoma and hemangioma1). The report of ABC associated with FD is very rare, and moreover, the occurrence in skull vault is even rarer. Martinez et al.15) found only one case (2.4%) of ABC in the 42 patients with FD. All the cases of calvarial FD with ABC retrieved by Medline search in literature have been reviewed and are summarized in Table 1.
On the analysis of the reported 9 cases, the most common clinical feature is expanding mass on the scalp with or without pain during a short period. The nature of rapid growth may come from the malignant change of FD. However, FD is a benign disease, even though malignant transformation has been reported in 0.5% of patients with monostotic FD and in 4% of polyostotic FD19). Therefore, the possibility of ABC transformation or abrupt cystic hemorrhage should be considered especially in patients who are younger than 20 years old. The most common radiological appearance of ABC transformation is the osteolytic lesion involving the inner and outer table of skull and expansion of the diploic space. The fluid-fluid level may suggest intracystic hemorrhage11).
On histopathology, FD with ABC has two components. FD component is irregular bony trabeculae with varying number of fibroblasts. ABC component is blood-filled cavernous space surrounded by multinucleated giant cells10).
The differential diagnosis of solitary osteolytic skull lesion includes hemangioma, epidermoid cyst, and eosinophilic granuloma17). Skull hemangioma is usually solitary lytic diploic space lesions. Hemorrhagic transformation can be seen on magnetic resonance images. Epidermoid cyst involves both the inner and outer tables and is well-defined lesions that lack central trabeculae and have a sclerotic rim. On the other hand, eosinophilic granulomas are round or oval nonsclerotic skull lesion with sharply defined margins. However, the differential diagnosis of these lesions is difficult on the radiological findings, confirmation by histopathologic finding is essential.
In review of the literature, the treatment of choice for FD with ABC is en-bloc resection and cranioplasty. Also, close follow-up to the resected lesion is recommended. In selected cases, preoperative embolization can be helpful to perform the excision with minimal blood loss10).
CONCLUSION
We report a rare case of FD with secondary hemorrhage from ABC. Although this disease entity is very rare, we should take it consideration in differential diagnosis of osteolytic calvarial lesions when the characteristic fluid-fluid level on CT scans and rapidly growing scalp mass is presented.
References
- 1.Branch CL, Challa VR, Kelly DL. Aneurysmal bone cyst with fibrous dysplasia of the parietal bone. reports of two cases. J Neurosurg. 1986;64:331–335. doi: 10.3171/jns.1986.64.2.0331. [DOI] [PubMed] [Google Scholar]
- 2.Brown EW, Megerian CA, McKenna MJ, Weber A. Fibrous dysplasia of the temporal bone: imaging findings. AJR Am J Roentgenol. 1995;165:679–682. doi: 10.2214/ajr.164.3.7863893. [DOI] [PubMed] [Google Scholar]
- 3.Burger PC, Scheithauer BW, Vogel FS. Surgical pathology of the nervous system and its coverings. ed 3. Edinburgh: Churchill Livingstone; 1991. pp. 1–17. [Google Scholar]
- 4.Cacdac MA, Malis LI, Anderson PJ. Aneurysmal parietal bone cyst. Case report. J Neurosurg. 1972;37:237–241. doi: 10.3171/jns.1972.37.2.0237. [DOI] [PubMed] [Google Scholar]
- 5.Calliauw L, Roels H, Caemaert J. Aneurysmal bone cysts in the cranial vault and base of skull. Surg Neurol. 1985;23:193–198. doi: 10.1016/0090-3019(85)90345-3. [DOI] [PubMed] [Google Scholar]
- 6.Casselman JW, De Jonge, I, Neyt L, De Clercq C, D'Hont G. MRI in craniofacial fibrous dysplasia. Neuroradiology. 1993;35:234–237. doi: 10.1007/BF00588505. [DOI] [PubMed] [Google Scholar]
- 7.Edgerton MT, Persing JA, Jane JA. The surgical treatment of fibrous dysplasia : With emphasis on recent contributions from cranio-maxillofacial surgery. Ann Surg. 1985;202:459–479. doi: 10.1097/00000658-198510000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fries JW. The roentgen features of fibrous dysplasia of the skull and facial bones; a critical analysis of thirty-nine pathologically proved cases. Am J Roentgenol Radium Ther Nucl Med. 1957;77:71–76. [PubMed] [Google Scholar]
- 9.Ha SK, Park JY, Kim SH, Lim DJ, Park YK, Chung YK, et al. Fibrous dysplasia involving the fronto-orbital bone: surgical experience. J Korean Neurosurg Soc. 2003;34:23–26. [Google Scholar]
- 10.Itshayek E, Spector S, Gomori M, Segal R. Fibrous dysplasia in combination with aneurysmal bone cyst of the occipital bone and the clivus: case report and review of the literature. Neurosurgery. 2002;51:815–818. [PubMed] [Google Scholar]
- 11.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst : concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573–580. doi: 10.2214/ajr.164.3.7863874. [DOI] [PubMed] [Google Scholar]
- 12.Laine FJ, Kuta AJ. Imaging of sphenoid bone and basiocciput : pathological consideration. Semin Ultrasound CT MR. 1993;14:160–177. doi: 10.1016/s0887-2171(05)80077-0. [DOI] [PubMed] [Google Scholar]
- 13.Lin WC, Wu HT, Wei CJ, Chang CY. Aneurysmal bone cyst arising from fibrous dysplasia of the frontal bone. Eur Radiol. 2004;14:930–932. doi: 10.1007/s00330-003-2181-4. [DOI] [PubMed] [Google Scholar]
- 14.Lichtenstein L. Bone tumors. ed 5. St Louis: CV Mosby; 1977. pp. 403–422. [Google Scholar]
- 15.Martinez V, Sissons HA. Aneurysmal bone cyst. a review of 123 cases including primary lesions and those secondary to other bone pathology. Cancer. 1988;61:2291–2304. doi: 10.1002/1097-0142(19880601)61:11<2291::aid-cncr2820611125>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 16.Mattei TA, Mattei JA, Ramina R, Aguiar PH. Fibrous dysplasia in combination with aneurysmal bone cyst presenting as a subarachnoid haemorrhage. Neurol Sci. 2005;26:178–181. doi: 10.1007/s10072-005-0458-x. [DOI] [PubMed] [Google Scholar]
- 17.Osborn AG. Diagnostic Neuroradiology. ed 1. St. Louis: Mosby; 1994. p. 516. [Google Scholar]
- 18.Rappaport ZH. Aneurysmal bone cyst associated with fibrous dysplasia of the skull. Neurochirurgia. 1989;32:192–194. doi: 10.1055/s-2008-1054037. [DOI] [PubMed] [Google Scholar]
- 19.Ruggieri P, Sim FH, Bond JR. Malignancies in fibrous dysplasia. Cancer. 1994;73:1411–1424. doi: 10.1002/1097-0142(19940301)73:5<1411::aid-cncr2820730516>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 20.Wojno KJ, McCarthy EF. Fibro-osseous lesions of the face and skull with aneurysmal bone cyst formation. Skeletal Radiol. 1994;23:15–18. doi: 10.1007/BF00203695. [DOI] [PubMed] [Google Scholar]