Abstract
Background and Objectives
Aspiration thrombectomy (AT) during primary percutaneous coronary intervention (PCI) is an effective adjunctive therapy for ST-segment elevation myocardial infarction (STEMI). An elevated neutrophil count in STEMI is associated with microvascular dysfunction and adverse outcomes. We evaluated whether AT can improve microvascular dysfunction in patients with STEMI and an elevated neutrophil count.
Subjects and Methods
Seventy patients with STEMI undergoing primary PCI from August 2007 to February 2009 in our institution were classified by tertiles of neutrophil count on admission (<5,300/mm3, 5,300-7,600/mm3, and >7,600/mm3). The angiographic outcome was post-procedural thrombolysis in myocardial infarction (TIMI) flow grade. Microvascular dysfunction was assessed by TIMI myocardial perfusion (TMP) grade and ST-segment resolution on electrocardiography 90 minutes after PCI. The clinical outcome was major adverse cardiac event (MACE), defined as cardiac death, re-infarction, and target lesion revascularization at 9 months.
Results
There were no significant differences in the clinical characteristics and pre- and post-procedural TIMI flow grades between the neutrophil tertiles. As the neutrophil count increased, a lower tendency toward TMP grade 3 (83% vs. 52% vs. 54%, p=0.06) and more persistent residual ST-segment elevation (>4 mm: 13% vs. 26% vs. 58%, p=0.005) was observed. The 9-month MACE rate was similar between the groups. On subgroup analysis of AT patients (n=52) classified by neutrophil tertiles, the same tendency toward less frequent TMP grade 3 (77% vs. 56% vs. 47%, p=0.06) and persistent residual ST-segment elevation (>4 mm: 12% vs. 28% vs. 53%, p=0.05) was observed as neutrophil count increased.
Conclusion
A higher neutrophil count at presentation in STEMI is associated with more severe microvascular dysfunction after primary PCI, which is not improved with AT.
Keywords: Myocardial infarction, Neutrophils
Introduction
Primary percutaneous coronary intervention (PCI) is effective in opening infarct-related arteries in patients with ST-segment elevation myocardial infarction (STEMI). Aspiration thrombectomy (AT) is an effective adjunctive therapy for patients with STEMI, which reduces large thrombotic burden by improving coronary reperfusion.1-3)
However, restoration of epicardial coronary flow in patients with STEMI does not necessarily lead to restoration of microvascular perfusion and protection of myocardial dysfunction. For this reason, identifying factors affecting microvascular perfusion has gained importance to reduce myocardial dysfunction.
Neutrophils, together with platelets, have recently been described as predictors of impaired left ventricular (LV) function and worse clinical prognosis in patients with STEMI. The suggested pathologic mechanisms involving neutrophils are microvascular plugging, spasm, endothelial swelling, and inflammatory response by pro-inflammatory cytokines release, all of which eventually lead to impairment of microvascular perfusion during acute myocardial ischemia and following reperfusion therapy.1),4-10) However, it is unclear whether AT during primary PCI can prevent or reduce microvascular damage in patients with elevated neutrophil counts.
The objective of this study was to determine the effect of neutrophil count on microvascular dysfunction, and the effect of AT on improving microvascular dysfunction during primary PCI in patients with STEMI.
Subjects and Methods
Study population
From August 2007 to February 2009, the medical records of 74 consecutive patients who underwent primary PCI for STE-MI were reviewed. STEMI was defined as symptoms or signs suggesting acute myocardial ischemia lasting >30 minutes, and ST-segment elevation of ≥0.2 mV in the precordial leads and 0.1 mV in limb leads in ≥2 contiguous leads on 12-lead electrocardiography (ECG). Patients pre-treated with fibrinolytic therapy and with co-morbidities which may affect blood cell counts, such as active infections, acute metabolic decompensation, chronic renal failure (defined as a serum creatinine level ≥2 mg/dL), advanced liver disease, malignancies, autoimmune diseases, and those currently under steroid treatment, were excluded (4 patients). As a result, 70 patients were enrolled in this study. All patients gave informed consent to participate in the study before undergoing coronary angiography and AT.
All patients had blood drawn for white blood cell (WBC) and differential counts, creatine kinase-myocardial band (CK-MB), troponin-T (Tn-T), and high sensitive C-reactive protein (hs-CRP) before primary PCI, and lipid profiles the next morning. An automated hematology analyzer (Sysmex SE-2100; Sysmex Corporation, Kobe, Japan) measured total WBC and neutrophil counts. The plasma concentrations of hs-CRP were measured by fully automated latex-enhanced immunoturbidmetric assays (Olympus AU 680; Munich, Germany).
Patients were classified into tertiles of neutrophil counts on admission (<5,300/mm3, 5,300-7,600/mm3, and >7,600/mm3) to compare microvascular dysfunction as the neutrophil count increased.
Patients were also compared based on whether or not AT was performed, and subgroups of patients who underwent AT were classified by neutrophil tertiles and analyzed.
Primary percutaneous coronary intervention, aspiration thrombectomy, and analysis of angiography
Primary angioplasty of the culprit lesion was performed by standard techniques via the transfemoral approach with a 6-Fr sheath and catheters and a loading dose of intravenous heparin (6,000 IU). Antiplatelet therapy was consisted of a loading dose of aspirin (300 mg) and clopidogrel (300-600 mg), and a subsequent maintenance dose of aspirin (100 mg) and clopidogrel (75 mg). The first procedural step involved passing a guidewire through the culprit lesion, then advancing the 6-Fr guiding compatible Thrombuster aspiration catheter (crossing profile, 5.1 Fr; Kaneca Inc. Tokyo, Japan) was inserted into the target coronary segment based on angiographic selection criteria, when the pre-procedural thrombolysis in myocardial infarction (TIMI) flow grade was 0-1, or the large visible thrombotic burden existed in the infarct-related artery was >2.5 mm in diameter on coronary angiogram. AT was defined as 'technically successful' when the thrombectomy catheter was easily placed distal to the target lesion and considered 'effective', when grossly-visible thrombotic material was retrieved in the aspirated sample. After primary PCI, postprocedural TIMI flow grades were assessed for angiographic outcome, and TIMI myocardial perfusion (TMP) grades for microvascular dysfunction.11) The coronary angiograms were reviewed by two unbiased cardiologists. Glycoprotein IIb/IIIa inhibitor (GPI) was administered at the discretion of the attending physician.
Analysis of electrocardiography
A 12-lead ECG was acquired at presentation and 90 minutes after PCI, and the ST-segments on the post-procedural ECG was compared with the ECG at presentation. The degree of resolution of ST-segment elevation was categorized as complete (>70%), partial (30-70%), or none (<30%) according to the TAPAS study. Residual ST-segment elevation was classified into 3 groups (<1 mm, 1-4 mm, and >4 mm) and assessed.
Study endpoints
The angiographic outcome was post-procedural TIMI flow grades. Microvascular dysfunction was assessed by TMP grades and ST-segment resolution on ECG 90 minutes after primary PCI. The clinical outcome was major adverse cardiac event (MACE), defined as cardiac death, re-infarction, and target lesion revascularization (TLR) 9 months after the index procedure. Cardiac death was defined as death due to myocardial infarction, cardiac perforation or tamponade, arrhythmia, death due to a complication of the procedure, and any death in which cardiac cause could not be excluded. Re-infarction was defined as recurrent symptoms with new ST-segment elevation and elevation of cardiac markers 2-fold more than the upper limit of normal range. TLR was defined as ischemia-driven revascularization of the infarct-related artery by PCI, or bypass surgery during the follow-up period.
Statistical analysis
Data were reported as the mean±standard deviation for continuous variables and as percentages for categorical variables. For testing of significance, continuous variables were compared using an independent t-test, and categorical data were compared using a chi-square test. Statistical comparisons were performed using Statistical Package for the Social Sciences (SPSS, version 12.0; SPSS Inc., Chicago, IL, USA). All significant tests were 2-sided, and the results were considered statistically significant when p≤0.05.
Results
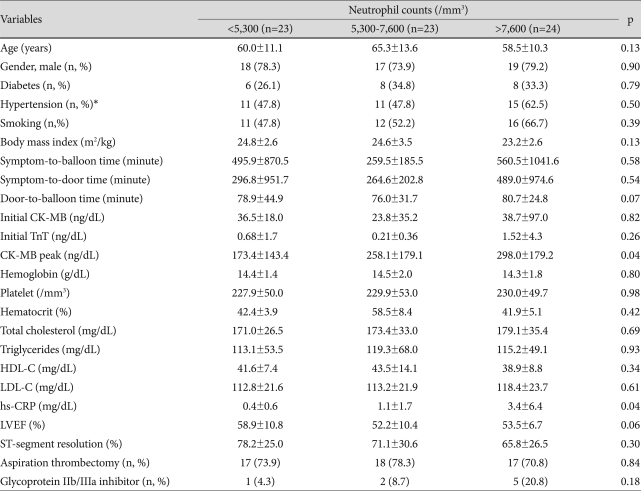
The baseline clinical characteristics of the 70 patients classified by tertiles of the neutrophil count at presentation are listed in Table 1. The median neutrophil count was 6,220/mm3 (range, 2,090-22,100/mm3). For clinical characteristics, there were no significant differences in age, gender, prevalence of diabetes, hypertension, history of smoking, body mass index, symptom-to-door time, and door-to-balloon time between the neutrophil tertiles. There were no significant differences at presentation with respect to CK-MB, Tn-T, hemoglobin, total cholesterol, high density lipoprotein-cholesterol, triglycerides, low density lipoprotein-cholesterol levels and platelet counts between the three groups. However, higher neutrophil tertiles had significantly higher levels of peak CK-MB (173±143 ng/dL vs. 258±179 ng/dL vs. 298±179 ng/dL, p=0.04) and hs-CRP (0.4±0.6 mg/dL vs. 1.1±1.7 mg/dL vs. 3.4±6.4 mg/dL, p=0.04).
Table 1.
Baseline characteristics of patients grouped by tertiles of neutrophil counts
Data are expressed as the mean±SD and number (percentage). *Blood pressure >140/90 mmHg or anti-hypertensive medication. CK-MB: creatine-kinase-MB, Tn-T: troponin-T, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, hs-CRP: high-sensitivity C-reactive protein, LVEF: left ventricular ejection fraction
AT was performed in 52 of 70 patients (74%) and GPI was administered in 8 of 70 patients (11%). The frequency of performing AT and the use of GPI were not significantly different between the neutrophil tertiles. Technical success of AT was achieved in all patients, and effective AT was achieved in 43 of 52 patients (83%).
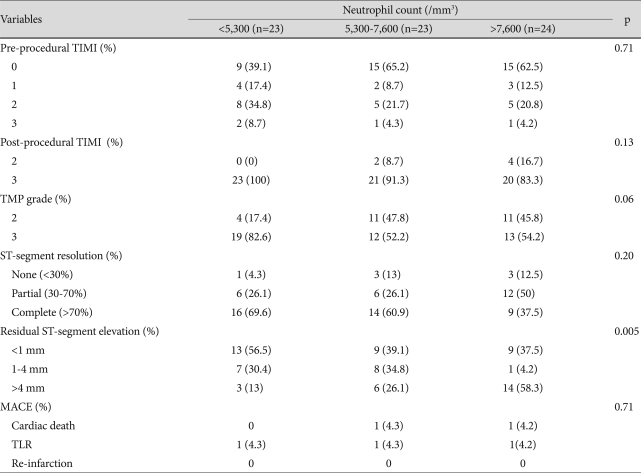
Comparison of angiographic, electrocardiographic, and clinical outcomes between neutrophil tertiles is summarized in Table 2. Pre- and post-procedural TIMI flow grades were similar between neutrophil tertiles, and a final TIMI flow grade of 2-3 was achieved in all patients. However, a TMP grade of 3 was marginally less frequently achieved in the higher neutrophil tertiles (83% vs. 52% vs. 54%, p=0.06) (Fig. 1A). Although ST-segment resolution rate was not significantly different (p=0.20), residual ST-segment elevation was significantly persistent with higher neutrophil tertiles (>4 mm; 13% vs. 26% vs. 58%, p=0.005) (Fig. 1C). MACEs occurred in 5 of 70 patients (7.1%), including 2 cardiac deaths and 3 TLRs during 9 months of follow-up. There was no significant difference in the MACE rate between neutrophil tertiles (Table 2).
Table 2.
Angiographic, electrocardiographic, and clinical outcomes according to neutrophil counts in all patients
Data are expressed as number (percentage). TIMI: thrombolysis in myocardial infarction, PCI: percutaneous coronary intervention, TMP grade: TIMI myocardial perfusion grade, MACE: major adverse cardiac outcome, TLR: target lesion revascularization
Fig. 1.
TMP grades, ST-segment resolution, and residual ST-segment elevation in all patients. A: TMP grade. B: ST-segment resolution. C: residual ST-segment elevation. TMP: thrombolysis in myocardial infarction myocardial perfusion.
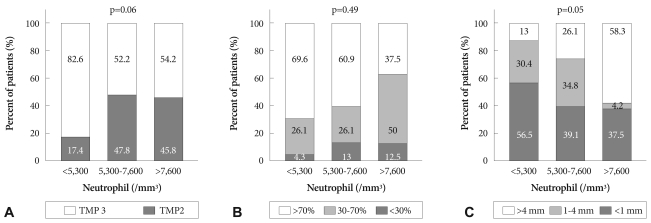
Comparison of patients who did and did not undergo aspiration thrombectomy
Of 70 patients, AT was performed in 52 patients (AT+ group) and not performed in 18 patients (AT- group). Table 3 summarizes the comparison between the two groups. In the AT+ group, 41 patients (79%) had a pre-procedural TIMI flow grade of 0-1 and the remaining 11 patients (21%) had a TIMI flow grade of 2-3 with large visible thrombi. The pre-procedural TIMI flow grade of 0-1 was significantly worse in the AT+ group than the AT- group (79% vs. 39%, p=0.01), which suggested a greater thrombotic burden requiring AT. In the AT- group (n=18), the pre-procedural TIMI flow grade was 0-1 in 7 patients (grade 0, n=5; and grade 1, n=2) but AT was not performed because upon the guidewire crossing the culprit lesion, a TIMI flow grade of 3 was immediately restored without grossly-visible thrombus, which suggested very small or negligible thrombus not requiring AT. Other than pre-procedural TIMI flow, there were no significant differences in baseline characteristics, laboratory findings, post-procedural TIMI flow grades, TMP grades, and ST-segment resolution rates between the two groups.
Table 3.
Comparison of patients with and without aspiration thrombectomy
Data are expressed as the mean±SD and number (percentage). *Blood pressure >140/90 mmHg or anti-hypertensive medication. AT: aspiration thrombectomy, CK-MB: creatine-kinase-MB, Tn-T: troponin-T, hs-CRP: high-sensitivity C-reactive protein, LVEF: left ventricular ejection fraction, TIMI: thrombolysis in myocardial infarction, TMP grade: TIMI myocardial perfusion grade
Subgroup analysis of patients undergoing aspiration thrombectomy classified by neutrophil tertiles
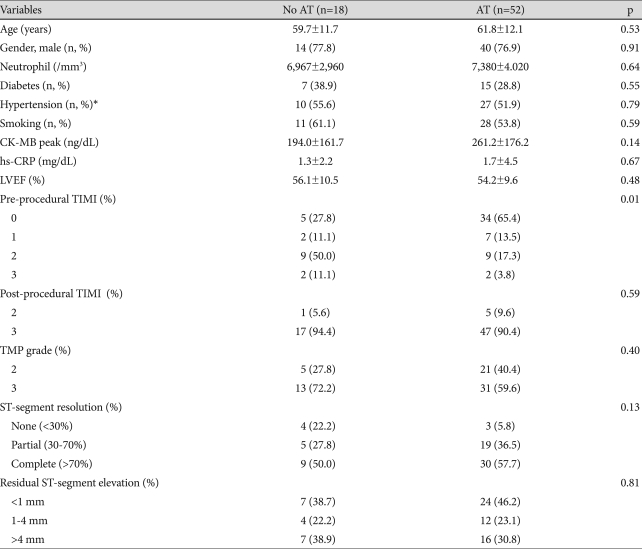
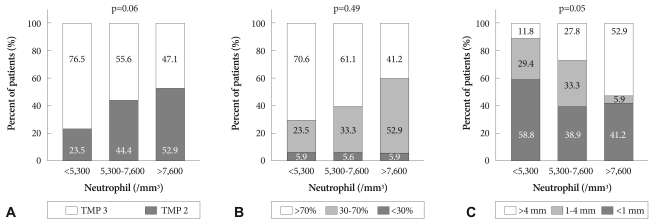
Subgroup analysis was performed on the AT+ group (n=52) divided by neutrophil tertiles (Table 4) (Fig. 2) to evaluate the effect of AT on patients with elevated neutrophil counts. There were no significant differences in pre- and post-procedural TIMI flow grades and the ST-segment resolution rates (Fig. 2B) between the neutrophil tertiles. However, the higher the neutrophil counts, a lower tendency toward TMP grade 3 (77% vs. 56% vs. 47%; p=0.06) (Fig. 2A) was observed. Residual ST-segment elevation was persistent in the higher neutrophil tertiles (>4 mm; 12% vs. 28% vs. 53%, p=0.05) (Fig. 2C).
Table 4.
Angiographic, electrocardiographic, and clinical outcomes according to neutrophil counts in patients undergoing aspiration thrombectomy
Data are expressed as the number (percentage). TIMI: thrombolysis in myocardial infarction, PCI: percutaneous coronary intervention, TMP: TIMI myocardial perfusion
Fig. 2.
TMP grades, ST-segment resolution, and residual ST-segment elevation in patients undergoing aspiration thrombectomy. A: TMP grade. B: ST-segment resolution. C: residual ST-segment elevation. TMP: thrombolysis in myocardial infarction myocardial perfusion.
Discussion
A unique contribution of our study is the assessment of the effect of AT on microvascular dysfunction, in terms of initial neutrophil counts in patients with STEMI. A major finding was that elevated neutrophil counts at the time of admission in patients with STEMI is associated with more severe microvascular dysfunction, even after AT.
Several randomized trials of patients with STEMI demonstrated that manual thrombus aspiration improved myocardial perfusion, when compared to conventional PCI.2),12) The role of AT has been particularly emphasized in patients with high-risk angiographic characteristics.13) Increased neutrophil count has been reported to be associated with increased risk of adverse clinical events and impaired microvascular perfusion in patients with acute myocardial infarction.9)
Recently Kirtane et al.14) and Mehta et al.15) reported that an elevated neutrophil count correlated with reduced patency of the epicardial coronary arteries after thrombolysis and impaired microvascular perfusion with longer corrected TIMI frame count, possibly as a result of neutrophil-mediated microvascular plugging. Sezar et al.8) also reported an association between neutrophilia on admission and severe microvascular dysfunction evaluated 48 hours after primary PCI. It is known that during myocardial ischemia-reperfusion, neutrophils cause capillary plugging in coronary microcirculation and damage endothelial function, resulting in reduced coronary vasodilator reserve.16-18) A growing body of evidence also suggests that inflammation plays an important role in acute coronary syndrome, leading to progression of atherosclerosis, plaque rupture, and thrombotic occlusion. Neutrophils release pro-inflammatory cytokines, which cause local and systemic inflammatory responses, resulting in microvascular swelling and blood flow impairment.12),19)
In the current study, patients with higher neutrophil tertiles had higher levels of blood peak CK-MB, indicating more severe myocardial necrosis. Microvascular dysfunction assessed by TMP grades and residual ST-segment changes were also more severe as the neutrophil counts increased, and the tendency continued, even with AT. The above findings suggest that higher neutrophil counts in patients with STEMI is associated with more severe microvascular dysfunction, which was not successfully treated, even with AT.
The role of inflammation in the pathophysiology of STEMI should be emphasized. In our study, patients with higher neutrophil counts had higher levels of hs-CRP. Consistent with previous studies, an elevated hs-CRP implies increased inflammation mediated by the endothelium and blood cells, including neutrophils, in patients with STEMI may be associated with more atheromas and myocardial injury,16-18) and further aggravate myocardial damage, even after removal of thrombi in the coronary circulation. Both WBC count and CRP level are markers of inflammation and predictors of outcomes after STEMI, but the association between neutrophils and adverse clinical outcomes is known to be independent of CRP.20)
Another interesting finding is that the prevalence of persistent residual ST-segment elevation on ECG after PCI was significantly higher in the elevated neutrophil tertiles, which remained unchanged after AT. This suggests that AT was unable to sufficiently prevent microvascular dysfunction in patients with elevated neutrophil counts.
Several studies have suggested that neutrophil counts at the time of initial presentation in patients with STEMI can predict outcomes at both short- and long-term follow-up evaluations.1),4-10),21-24) There was no significant difference in the 9-month MACE rate between the neutrophil tertiles. The reason why a higher neutrophil count did not result in worse clinical outcomes may be attributed to the low incidence of MACEs (7%) in our study. This finding was also consistent with another study which revealed a discrepancy between reperfusion and clinical outcome in patients with STEMI after AT.25) A further study is needed to clarify in this regard.
Early and sustained restoration of flow into the infarct-related artery is the aim of reperfusion therapy in patients with STEMI. AT and GPIs during primary PCI have been the mainstay of adjunctive treatment in sustaining reperfusion and improving microvascular dysfunction. However, in our study AT had a limited role in improving microvascular dysfunction in patients with higher neutrophil counts.
This study had several inherent limitations. It was a single center study and the patient population was small. For detailed analysis, such as ST segment changes and TMP grades, we were unable to use a large registry data. In addition, AT was selectively performed, rather than randomized. Although a large portion of patients in our study required AT, we believe that routine aspiration is not always indicated in primary PCI. Therefore, we performed AT in select patients with large thrombotic burdens at the discretion of experienced cardiologists. In our opinion, that is the more realistic way to evaluate the effect of AT in high-risk patients. Without randomization of aspiration, however, we were able to assess the effect of AT according to the neutrophil tertiles, which generated the key find-ings in this study.
Further large-scale randomized trials is needed to validate our findings, and define the role of AT in improving microvascular dysfunction in high risk patients with STEMI.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Arakawa K, Yasuda S, Hao H, et al. Significant association between neutrophil aggregation in aspirated thrombus and myocardial damage in patients with ST-segment elevation acute myocardial infarction. Circ J. 2009;73:139–144. doi: 10.1253/circj.cj-08-0609. [DOI] [PubMed] [Google Scholar]
- 2.Kang WC, Ahn TH, Han SH, et al. Efficacy of thrombosuction using the export aspiration catheter before primay percutaneous coronary intervention in acute myocardial infarction. Korean Circ J. 2005;35:172–179. [Google Scholar]
- 3.Koh YY, Kim WG, Hwang HK. Aspiration thromboembolectomy in the management of acute coronary occlusion during percutaneous transluminal coronary angiography. Korean Circ J. 1998;28:1905–1909. [Google Scholar]
- 4.Huang G, Zhong XN, Zhong B, et al. Significance of white blood cell count and its subtypes in patients with acute coronary syndrome. Eur J Clin Invest. 2009;39:348–358. doi: 10.1111/j.1365-2362.2009.02107.x. [DOI] [PubMed] [Google Scholar]
- 5.Chia S, Nagurney JT, Brown DF, et al. Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. Am J Cardiol. 2009;103:333–337. doi: 10.1016/j.amjcard.2008.09.085. [DOI] [PubMed] [Google Scholar]
- 6.Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102:653–657. doi: 10.1016/j.amjcard.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Turner SJ, Ketch TR, Gandhi SK, Sane DC. Routine hematologic clinical test and prognostic markers in patients with acute coronary syndrome. Am Heart J. 2008;155:806–816. doi: 10.1016/j.ahj.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 8.Sezer M, Okcular I, Goren T, et al. Association of haematologic indices with the degree of microcvascular injury in patients with acute anterior wall myocardial infarction treated with primary percutaneous coronary intervention. Heart. 2007;93:313–318. doi: 10.1136/hrt.2006.094763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takahashi T, Hiasa Y, Ohara Y, et al. Relation between neutrophil counts on admission, microvascular injury, and left ventricular functional recovery in patients with an anterior wall first acute myocardial infarction treated with primary coronary angioplasty. Am J Cardiol. 2007;100:35–40. doi: 10.1016/j.amjcard.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 10.Mariani M, Fetiveau R, Rossetti E, et al. Significance of total and differential leukocyte count in patients with acute myocardial infarction treated with primary coronary angioplasty. Eur Heart J. 2006;27:2511–2515. doi: 10.1093/eurheartj/ehl191. [DOI] [PubMed] [Google Scholar]
- 11.van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Circulation. 1998;97:2302–2306. doi: 10.1161/01.cir.97.23.2302. [DOI] [PubMed] [Google Scholar]
- 12.Svilaas T, Vlaar PJ, van der Hosr IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–567. doi: 10.1056/NEJMoa0706416. [DOI] [PubMed] [Google Scholar]
- 13.Javaid A, Siddiqi NH, Steinberg DH, et al. Adjunct thrombus aspiration reduces mortality in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction with high-risk angiographic characteristics. Am J Cardiol. 2008;101:452–456. doi: 10.1016/j.amjcard.2007.09.091. [DOI] [PubMed] [Google Scholar]
- 14.Kirtane AJ, Bui A, Murphs SA, Barron HV, Gibson DM. Association of peripheral neutrophilia with adverse angiographic outcome in ST-elevation myocardial infarction. Am J Cardiol. 2004;93:532–536. doi: 10.1016/j.amjcard.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Mehta JL, Nichols WW, Mehta P. Neutrophils as potential participants in acute myocardial ischemia: relevance to reperfusion. J Am Coll Cardiol. 1988;11:1309–1316. doi: 10.1016/0735-1097(88)90297-5. [DOI] [PubMed] [Google Scholar]
- 16.Nichols WW, Metha HL, Donnelly WH, Lawson D, Thompson L, ter Riet M. Reduction in coronary vasodilator reserve following coronary occlusion and reperfusion in anesthetized dog: role of endothelium derived relaxing factor, myocardial neutrophil infiltration and prostaglandins. J Mol Cell Cardiol. 1988;20:943–954. doi: 10.1016/s0022-2828(88)80148-2. [DOI] [PubMed] [Google Scholar]
- 17.Kloner RA, Giacomelli F, Alker KJ, Hale SL, Matthews R, Bellows S. Influx of neutrophils in the walls of large epicardail coronary arteries in response to ischemia/perfusion. Circulation. 1991;84:1758–1772. doi: 10.1161/01.cir.84.4.1758. [DOI] [PubMed] [Google Scholar]
- 18.Miyao Y, Miyazaki S, Goto Y, et al. Role of cytokines and adhesion molecules in ischemia and reperfusion in patients with acute myocardial infarction. Jpn Circ J. 1999;63:362–366. doi: 10.1253/jcj.63.362. [DOI] [PubMed] [Google Scholar]
- 19.Merlini PA, Cugno M, Rossi ML, et al. Activation of the contact system and inflammation after thrombolytic therapy in patients with acute myocardial infarction. Am J Cardiol. 2004;93:822–825. doi: 10.1016/j.amjcard.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Sabatine MS, Morrow DA, Cannon CP, et al. Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: A TACTICS-TIMI 18 substudy. J Am Coll Cardiol. 2002;40:1761–1768. doi: 10.1016/s0735-1097(02)02484-1. [DOI] [PubMed] [Google Scholar]
- 21.Shin SH, Oh DJ, Lim HE, et al. The source of inflammatory response and platelet activation in patients with acute myocardial infarction. Korean Circ J. 2005;35:155–162. [Google Scholar]
- 22.Kim KY, Hae JH. The clinical usefulness of decreased mean platelet component concentration in patients with acute coronay syndrome. Korean Circ J. 2005;35:240–246. [Google Scholar]
- 23.Han J, Youn TJ, Hong ES, et al. The relationship between initial leukocyte count and the extent of myocardial injury in patients with acute myocardial infarction who received reperfusion therapy. Korean Circ J. 2004;34:735–742. [Google Scholar]
- 24.Lee JH, Kim HS, Kwon YS, et al. The prognostic value of mean platelet volume in acute myocardial infarction. Korean Circ J. 2003;33:878–883. [Google Scholar]
- 25.Mongeon FP, Bélisle P, Joseph L, Eisenberg MJ, Rinfret S. Adjunctive thrombectomy for acute myocardial infarction: a bayesian meta-analysis. Circ Cardiovasc Interv. 2010;3:6–16. doi: 10.1161/CIRCINTERVENTIONS.109.904037. [DOI] [PubMed] [Google Scholar]