Abstract
Background and Objectives
The extent of coronary artery calcification (CAC) is closely related to total atherosclerotic plaque burden. However, the pathogenesis of CAC is still unclear. Conditions such as diabetes mellitus, renal failure, smoking, and chronic inflammation have been suggested to link vascular calcification and bone loss. In the present study, we hypothesized that bone loss can contribute to the pathogenesis of CAC in patients with the chronic inflammatory condition that accompanies metabolic syndrome (MetS). The objective of this study was to investigate the relationship between CAC and bone mineral density (BMD) in patients with MetS and in patients without MetS, by using coronary multidetector-row computed tomography (MDCT).
Subjects and Methods
Data from 395 consecutive patients was analyzed retrospectively. From the MDCT database, only those patients who underwent both coronary MDCT and dual-energy X-ray absorptiometry within an interval of one month, were selected. The presence of MetS was determined by the updated criteria as defined by the Third Adult Treatment Panel Report of the National Cholesterol Education Program.
Results
In patients with MetS, a significant correlation was found between CAC and age {odds ratio (OR)=1.139, 95% confidence interval (CI) 1.080 to 1.201, p<0.001}, CAC and male sex (OR=3.762, 95% CI 1.339 to 10.569, p=0.012), and CAC and T-score of L-spine (OR=0.740, 95% CI 0.550 to 0.996, p=0.047) using a forward multiple logistic regression analysis model including clinical variables of gender, age, lipid profile, body mass index, diabetes mellitus, hypertension, smoking, and BMD. But in patients without MetS, BMD by itself was not found to contribute to CAC.
Conclusion
BMD was inversely correlated with CAC only in patients with MetS. This finding suggests that low BMD accompanied by MetS, may have significant clinical implications.
Keywords: Bone density, Metabolic syndrome X, Coronary artery disease
Introduction
Coronary artery calcification (CAC) has been shown to play an important role of a risk marker in the development of atherosclerosis.1) CAC is closely related to total atherosclerotic plaque burden.1) However, the pathogenesis of CAC is still unclear. Some studies have suggested that the degree of CAC correlates with local vascular inflammation.2),3)
Metabolic syndrome (MetS) is associated with low-grade systemic inflammation.4) MetS is characterized by clustering of cardiovascular risk factors including central adiposity, insulin resistance, hypertension, dyslipidemia, and a proinflammatory state.5) Some studies have shown that both insulin resistance and atherosclerosis share a common inflammatory process.6)
Controversially, some studies have reported the association between low bone mineral density (BMD) and coronary artery disease.7),8) Several mechanisms have been suggested to link vascular calicification and bone loss, including ageing, diabetes mellitus, renal failure, smoking, chronic inflammation, and oxidative stress.9) In the present study, we hypothesized that bone loss can contribute to the pathogenesis of CAC in patients with the chronic inflammatory condition that accompanies MetS. Hence in this study, we aimed to investigate the relationship between CAC and BMD in patients with MetS and in patients without MetS, by using coronary multidetector-row computed tomography (MDCT).
Subjects and Methods
Study population
The dataset was acquired from the MDCT database at the Hanyang University Hospital, Seoul, Korea, from March 29th 2007 to June 25th 2009. From this database 3,521 patients who underwent both coronary MDCT and dual-energy X-ray absorptiometry (DEXA) within an interval of one month were enrolled. Finally, data from 395 consecutive patients was analyzed retrospectively.
All of these patients had undergone physical examination at the health promotion center. A fasting lipid profile {total cholesterol, high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-C (LDL-C), and triglycerides} plus blood glucose tests were performed on each of the study participant. Blood pressure (BP) was measured by a mercury sphygmomanometer by the physician and the average of at least two measurements taken five minutes apart, were recorded. Weight and height of each study participant, for calculation of the body mass index (BMI) (kg/m2) were also recorded at the same visit. Clinical information was collected by reviewing each patient's medical records.
Prevalent diabetes was defined as a self-report of a history of being told by a physician that he/she had diabetes or was having a fasting blood glucose level of greater than or equal to 126 mg/dL. Hypertension was defined as average BP of at least 140/90 mmHg on two consecutive measurements taken five minutes apart or undergoing antihypertensive drug treatment due to a history of hypertension. The presence of MetS was determined by the updated criteria as defined by the Third Adult Treatment Panel (ATP III) Report of the National Cholesterol Education Program.10) We modified the criteria and we used BMI ≥25 kg/m2 instead of waist circumference cutpoints.11) Subjects with three or more of the following criteria: 1) BMI ≥25 kg/m2; 2) Serum triglycerides levels of ≥150 mg/dL or undergoing drug treatment for elevated serum triglycerides levels ; 3) HDL-C levels of ≤40 mg/dL in men and ≤50 mg/dL in women or undergoing drug treatment for low HDL-C; 4) fasting blood glucose level of ≥100 mg/dL or undergoing drug treatment for elevated fasting blood glucose level ; or 5) BP of at least 130/85 mmHg or undergoing antihypertensive drug treatment due to a history of hypertension.
The study protocol was approved by the Institutional Review Board of the Hanyang University Hospital.
Coronary calcification measurements
CT scans were performed on a 64-MDCT scanner (Brilliance 64, Philips Medical Systems, Best, The Netherlands). About sixty, 0.9-mm thick slices of the coronary arteries were obtained during a single breath-hold for the time period of 15-20 seconds, using prospective electrocardiography-gated axial scanning. All the CT images were analyzed for the presence and the extent of CAC according to the Agatston method, by using the coronary calcium quantification software (Aquarius workstation, TeraRecon, Inc., San Mateo, CA, USA).12)
Bone mineral density measurements
BMD was measured at the lumbar spine (L-spine) and femur using DEXA (Discovery-W, Hologic Inc., Bedford, MA, USA). The results were interpreted in terms of BMD (g/cm2) and the T-score. T-score was calculated by taking the difference between a patient's measured BMD and the mean BMD of healthy young adults matched for gender and ethnicity, and dividing by the standard deviation (SD) of the young adult population.
Statistical analysis
All data are presented as the means and standard deviations, and statistical analysis was performed using Statistical Package for the Social Sciences (SPSS, version 13.0; SPSS Inc., Chicago, IL, USA). A p<0.05 was considered statistically significant.
Student's t-test was used for comparison of measured values between the two groups divided according to the presence of MetS. In order to compare the significance between the two groups, chi-square test was used. Univariate logistic regression analyses were used to identify the relationship between CAC and clinical variables. In the univariate logistic regression analysis; lipid profile, fasting blood glucose, age, BP, BMD, and BMI were analyzed as continuous variables.
In the total patients, three multiple logistic regression analysis models were used to estimate the independent correlation between CAC and clinical variables. Gender, age, smoking, BMD, LDL-C, MetS, and interaction of MetS with BMD were included as in all the models. Collinearity was present between MetS and hypertension, MetS and diabetes mellitus, MetS and BMI, MetS and triglycerides, and MetS and HDL-C. Hence these risk factors associated with MetS, were excluded from the models for the total patients. For the total patients, in the first model T-score of L-spine was included. In the second model, T-score of femur was included. In the third model, T-scores of both L-spine and femur were included.
In patients with MetS and in patients without MetS, three multiple logistic regression analysis models were also used to estimate the independent correlation between CAC and clinical variables. Due to the exclusion of MetS from the analysis models, gender, age, lipid profile, BMI, diabetes mellitus, hypertension, smoking, and BMD were included in all the models. Collinearity was seen between LDL-C level and statin medication. Collinearity was also seen between hypertension status and antihypertensive medication. Hence, we excluded medication status from all the multiple logistic regression models. The inclusion criterion for the forward multiple logistic regression analysis was p<0.05 while the exclusion criterion was p>0.10. In all the multiple logistic regress-ion analysis, lipid profile, age, BMD, and BMI were analyzed as continuous variables. Odd ratio (OR) is presented with 95% confidence interval (CI) in parenthesis.
Results
General characteristics of the subjects
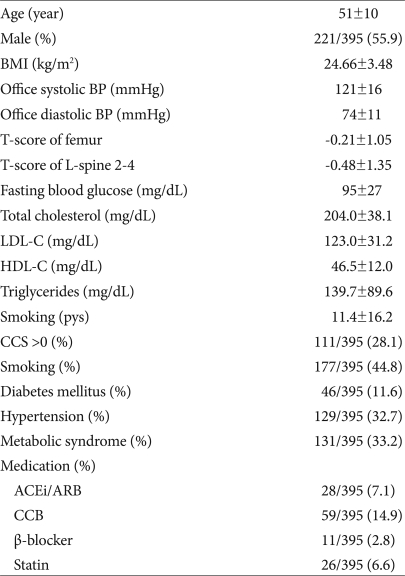
The clinical characteristics of the study population are displayed in Table 1. The mean (±SD) age of the subjects was 51±10 years and the proportion of males was 55.9%. Proportion of diabetes was 11.6%, proportion of hypertension was 32.7%, and proportion of MetS was 33.2%.
Table 1.
Clinical characteristics of the patients
Data is reported as mean (±SD) or percentage. BMI: body mass index, BP: blood pressure, L-spine: lumbar spine, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, CCS: coronary calcium score, ACEi: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, CCB: calcium channel blocker
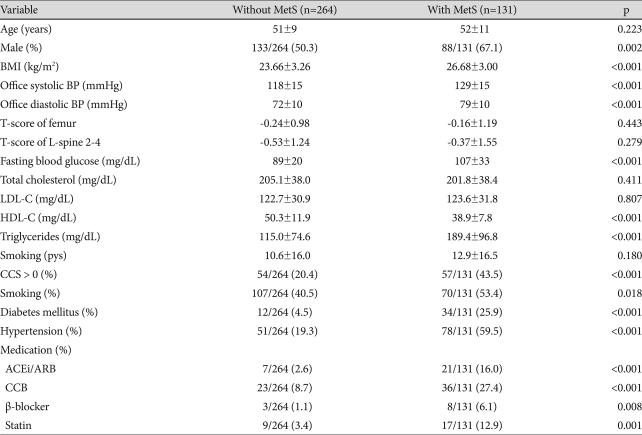
In the two groups divided by the presence of MetS, there were 264 subjects without MetS and there were 131 subjects with MetS. The significant differences between the group without MetS versus the group with MetS respectively were as follows: proportion of males: 50.3% vs. 67.1%, p=0.002, BMI: 23.66±3.26 vs. 26.68±3.00 kg/m2, p<0.001, office systolic BP: 118±15 vs. 129±15 mmHg, p<0.001, office diastolic BP: 72±10 vs. 79±10 mmHg, p<0.001, Fasting blood glucose: 89±20 vs. 107±33 mg/dL, p<0.001, HDL-C: 50.3±11.9 vs. 38.9±7.8 mg/dL, p<0.001, triglycerides: 115.0±74.6 vs. 189.4±96.8 mg/dL, p<0.001, proportion of CCS >0: 20.4% vs. 43.5%, p<0.001, proportion of smokers: 40.5% vs. 50.4%, p=0.018, proportion of diabetes mellitus: 4.5% vs. 25.9%, p<0.001, and proportion of hypertension: 19.3% vs. 59.5%, p<0.001 (Table 2).
Table 2.
Comparison of the clinical characteristics between the two patient groups, divided by the presence of metabolic syndrome
Data is reported as mean (±SD) or percentage. MetS: metabolic syndrome, BMI: body mass index, BP: blood pressure, L-spine: lumbar spine, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, CCS: coronary calcium score, ACEi: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, CCB: calcium channel blocker
Crude relationship between coronary artery calcification and clinical variables
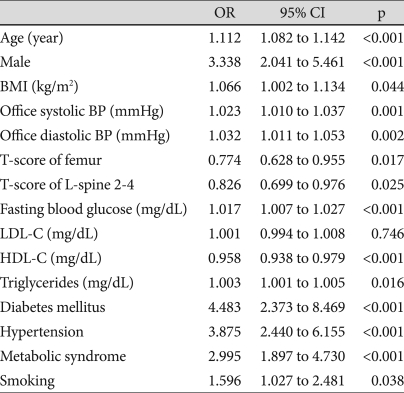
Univariate correlation between CAC and clinical variables are listed in Table 3. A significantly positive correlation was found between: CAC and age (OR=1.112, 95% CI 1.082 to 1.142, p<0.001), CAC and male sex (OR=3.338, 95% CI 2.041 to 5.461, p<0.001), CAC and BMI (OR=1.066, 95% CI 1.002 to 1.134, p=0.044), CAC and office systolic BP (OR=1.023, 95% CI 1.010 to 1.037, p=0.001), CAC and office diastolic BP (OR=1.032, 95% CI 1.011 to 1.053, p=0.002), CAC and fasting blood glucose (OR=1.017, 95% CI 1.007 to 1.027, p<0.001), CAC and triglycerides (OR=1.003, 95% CI 1.001 to 1.005, p=0.016), CAC and diabetes mellitus (OR=4.483, 95% CI 2.373 to 8.469, p<0.001), CAC and hypertension (OR=3.875, 95% CI 2.440 to 6.155, p<0.001), CAC and MetS (OR=2.995, 95% CI 1.897 to 4.730, p<0.001), and CAC and smoking (OR=1.596, 95% CI 1.027 to 2.481, p=0.038).
Table 3.
Univariate correlation between coronary artery calcification and clinical variables using a univariate logistic regression analysis
OR: odds ratio, CI: confidence interval, BMI: body mass index, BP: blood pressure, L-spine: lumbar spine, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol
CAC was inversely correlated with T-score of femur (OR=0.774, 95% CI 0.628 to 0.955, p=0.017), with T-score of L-spine (OR=0.826, 95% CI 0.699 to 0.976, p=0.025), and with HDL-C (OR=0.958, 95% CI 0.938 to 0.979, p<0.001).
Independent relationship between coronary artery calcification and clinical variables in the total patients
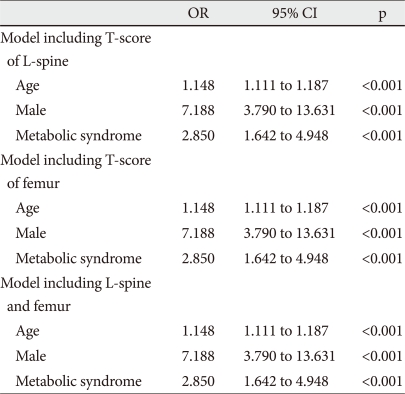
In the three multiple logistic regression analysis models, a significant correlation was found between: CAC and age (OR=1.148, 95% CI 1.111 to 1.187, p<0.001), CAC and male sex (OR=7.188, 95% CI 3.790 to 13.631, p<0.001), and CAC and MetS (OR=2.850, 95% CI 1.642 to 4.948, p<0.001) (Table 4). T-score of femur and/or L-spine was not an independent predictor of CAC. No significant correlation was found between CAC and the interaction between MetS and BMD.
Table 4.
Independent predictors of coronary artery calcification in the total patients using a forward multiple logistic regression analysis
OR: odds ratio, CI: confidence interval, L-spine: lumbar spine
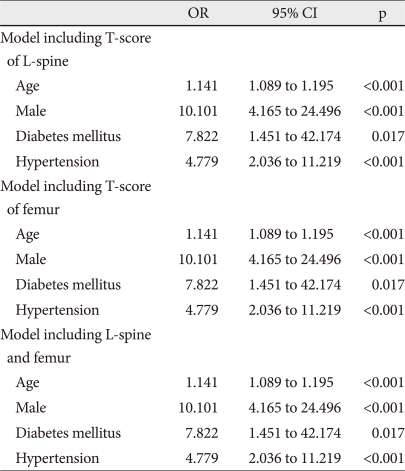
Independent relationship between coronary artery calcification and clinical variables in patients without metabolic syndrome
In the three multiple logistic regression analysis models, a significant correlation was found between: CAC and age (OR=1.141, 95% CI 1.089 to 1.195, p<0.001), CAC and male sex (OR=10.101, 95% CI 4.165 to 24.496, p<0.001), CAC and diabetes mellitus (OR=7.822, 95% CI 1.451 to 42.174, p=0.017) and CAC and hypertension (OR=4.779, 95% CI 2.036 to 11.219, p<0.001) (Table 5). T-score of femur and/or L-spine was not an independent predictor of CAC.
Table 5.
Independent predictors of coronary artery calcification in patients without metabolic syndrome using a forward multiple logistic regression analysis
OR: odds ratio, CI: confidence interval, L-spine: lumbar spine
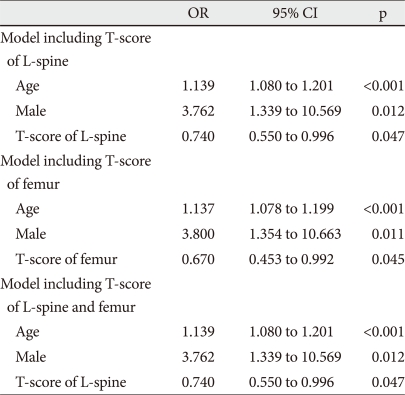
Independent relationship between coronary artery calcification and clinical variables in patients with metabolic syndrome
In the multiple logistic regression analysis model including T-score of L-spine, a significant correlation was found between: CAC and age (OR=1.139, 95% CI 1.080 to 1.201, p<0.001), CAC and male sex (OR=3.762, 95% CI 1.339 to 10.569, p=0.012), and CAC and T-score of L-spine (OR=0.740, 95% CI 0.550 to 0.996, p=0.047) (Table 6).
Table 6.
Independent predictors of coronary artery calcification in patients with metabolic syndrome using a forward multiple logistic regression analysis
OR: odds ratio, CI: confidence interval, L-spine: lumbar spine
In the multiple logistic regression analysis model including T-score of femur, a significant correlation was found between: CAC and age (OR=1.137, 95% CI 1.078 to 1.199, p<0.001), CAC and male sex (OR=3.800, 95% CI 1.354 to 10.663, p=0.011), and CAC and T-score of femur (OR=0.670, 95% CI 0.453 to 0.992, p=0.045) (Table 6).
In the multiple logistic regression analysis model including T-scores of both femur and L-spine, a significant correlation was found between: CAC and age (OR=1.139, 95% CI 1.080 to 1.201, p<0.001), CAC and male sex (OR=3.762, 95% CI 1.339 to 10.569, p=0.012), and CAC and T-score of L-spine (OR=0.740, 95% CI 0.550 to 0.996, p=0.047) (Table 6).
Discussion
The main finding of this study is that BMD is an independent determinant of CAC, only in patients with MetS. BMD is not an independent predictor of CAC in total patients nor in patients without MetS. Based on this finding, we could speculate that low BMD may contribute to the pathogenesis of CAC only in those patients with the low-grade chronic inflammatory condition that accompanies MetS.
A few studies have documented the increased risk of coronary atherosclerosis associated with CAC, in the subjects with low BMD.7),8),13) However, it is still unclear whether low BMD can be an independent predictor of CAC, even after a careful adjustment of the other risk factors for coronary artery disease. In the present study, no statistically significant correlation was found between CAC and BMD in the total patients, nor in the patients without MetS. These findings are partially consistent with some studies which suggest that bone loss and CAC are two independent processes.14),15) From a clinical viewpoint, the results of the present study suggest that so far, low BMD is less likely to be regarded as one of the major risk factors for coronary artery disease, inspite of the numerous experimental results suggesting an association between low BMD and vascular calcification. But the results in patients with MetS, might call attention to low BMD as a marker for CAC. However considering MetS with regards to coronary atherosclerosis; a low-grade inflammatory process with visceral obesity is strongly associated with coronary atherosclerosis. 16),17) In this study, there was a significant correlation between CAC and MetS. This result is consistent with the result from the previous study which demonstrated the relationship between CAC and Mets.18-20) It has also been shown that insulin resistance and atherosclerosis share a common inflammatory mechanism.6)
Specifically in this study, an independent relationship was found between CAC and BMD, only in patients with MetS. Chronic low-grade inflammatory processes or mediators are also known to be involved in the mechanism by which low BMD contributes in the pathogenesis of atherosclerosis. IL-6 and oxidized LDL are reported to be involved in vascular calcification by osteogenic de-differentiation of vascular smooth muscle cells.21) Potentially, low BMD could provide a milieu favoring vascular calcification through impaired phosphorous and calcium metabolism. Theoretically, there may be three possible explanations for interpreting this finding. Firstly, both the inflammatory process and impaired calcium/phosphorous metabolism are essential for CAC. This is less likely because MetS alone is independently associated with CAC. Secondly, even with an impaired calcium/phosphorus metabolism, MetS plays a permissive role in the pathogenesis of CAC. Thirdly, there might be a synergistic interaction between MetS and BMD. Since there was no synergistic interaction between BMD and MetS in this study, we can speculate that impaired calcium/phosphorous metabolism aggravates the pathogenesis of CAC only with accompanying MetS, associated with the chronic low-grade inflammation, whereas impaired calcium/phosphorous metabolism alone does not trigger the pathogenesis of CAC.
However, there are some limitations to our study. The major limitation is the possibility of a type II error due to the small sample size. Also because of the cross-sectional design of this study, we cannot conclude whether low BMD is pathogenetically linked to coronary calcification or it just represents one of the markers for subclinical coronary atherosclerosis in patients with MetS. Secondly in this study, the criteria of waist circumference was not used. Although use of ATP III criteria to define MetS in Korean populations11) is not appropriate, since we have used measures of BMI instead of waist circumference there is a possibility that we may have misclassified some subjects who would have been classified differently based on measures of waist circumference. Thirdly, since data on menopause was not available, we could not include menopause status as a variable in the multiple logistic regression analysis models. Some reports have shown that estrogen deficiency could possibly affect both vascular calcification and osteoporosis in women.22) Due to the possibility that the confounding factor was not fully adjusted, these findings cannot be applied to perimenopausal women. Fourthly, serum inflammatory marker such as hs-CRP, known to trigger the pathogenesis of CAC, was not available in this study. Hence , we could not demonstrate the direct relationship of vascular inflammation and CAC.
In conclusion, BMD is an independent determinant of CAC in patients with MetS. This finding suggests that it may therefore be meaningful to check for the presence of MetS, when evaluating patients with low BMD for the risk of developing coronary artery disease.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation. 1995;92:2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 2.Mazzini MJ, Schulze PC. Proatherogenic pathways leading to vascular calcification. Eur J Radiol. 2006;57:384–389. doi: 10.1016/j.ejrad.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 3.Moe SM, Chen NX. Inflammation and vascular calcification. Blood Purif. 2005;23:64–71. doi: 10.1159/000082013. [DOI] [PubMed] [Google Scholar]
- 4.Festa A, D'Agostino R, Jr, Howard G, Mykkanen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–47. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 5.Sakkinen PA, Wahl P, Cushman M, Lewis MR, Tracy RP. Clustering of procoagulation, inflammation, and fibrinolysis variables with metabolic factors in insulin resistance syndrome. Am J Epidemiol. 2000;152:897–907. doi: 10.1093/aje/152.10.897. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez-Real JM, Ricart W. Insulin resistance and inflammation in an evolutionary perspective: the contribution of cytokine genotype/phenotype to thriftiness. Diabetologia. 1999;42:1367–1374. doi: 10.1007/s001250051451. [DOI] [PubMed] [Google Scholar]
- 7.Farhat GN, Strotmeyer ES, Newman AB, et al. Volumetric and areal bone mineral density measures are associated with cardiovascular disease in older men and women: the health, aging, and body composition study. Calcif Tissue Int. 2006;79:102–111. doi: 10.1007/s00223-006-0052-0. [DOI] [PubMed] [Google Scholar]
- 8.Barengolts EI, Berman M, Kukreja SC, Kouznetsova T, Lin C, Chomka EV. Osteoporosis and coronary atherosclerosis in asymptomatic postmenopausal women. Calcif Tissue Int. 1998;62:209–213. doi: 10.1007/s002239900419. [DOI] [PubMed] [Google Scholar]
- 9.Hofbauer LC, Brueck CC, Shanahan CM, Schoppet M, Dobnig H. Vascular calcification and osteoporosis: from clinical observation towards molecular understanding. Osteoporos Int. 2007;18:251–259. doi: 10.1007/s00198-006-0282-z. [DOI] [PubMed] [Google Scholar]
- 10.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol. 2006;21:1–6. doi: 10.1097/01.hco.0000200416.65370.a0. [DOI] [PubMed] [Google Scholar]
- 11.Lee WY, Park JS, Noh SY, Rhee EJ, Kim SW, Zimmet PZ. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Res Clin Pract. 2004;65:143–149. doi: 10.1016/j.diabres.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 13.Choi SH, An JH, Lim S, et al. Lower bone mineral density is associated with higher coronary calcification and coronary plaque burdens by multidetector row coronary computed tomography in pre- and postmenopausal women. Clin Endocrinol (Oxf) 2009;71:644–651. doi: 10.1111/j.1365-2265.2009.03535.x. [DOI] [PubMed] [Google Scholar]
- 14.Sinnott B, Syed I, Sevrukov A, Barengolts E. Coronary calcification and osteoporosis in men and postmenopausal women are independent processes associated with aging. Calcif Tissue Int. 2006;78:195–202. doi: 10.1007/s00223-005-0244-z. [DOI] [PubMed] [Google Scholar]
- 15.Farhat G, Cauley J, Matthews K, et al. Volumetric BMD and vascular calcification in middle-aged women: the Study of Women's Health Across the Nation. J Bone Miner Res. 2006;21:1839–1846. doi: 10.1359/jbmr.060903. [DOI] [PubMed] [Google Scholar]
- 16.Cha BS, Kim HJ. Metabolic syndrome and cardiovascular disease. Korean Circ J. 2003;33:645–652. [Google Scholar]
- 17.Noh HJ, Kwon NH, Joo SB. Severity of coronary atherosclerosis: influence of metabolic syndrome risk factor clustering and hs-CRP. Korean Circ J. 2006;36:802–808. [Google Scholar]
- 18.Kim D, Choi SY, Choi EK, et al. Distribution of coronary artery calcification in an asymptomatic Korean population: association with risk factors of cardiovascular disease and metabolic syndrome. Korean Circ J. 2008;38:29–35. [Google Scholar]
- 19.Reilly MP, Wolfe ML, Rhodes T, Girman C, Mehta N, Rader DJ. Measures of insulin resistance add incremental value to the clinical diagnosis of metabolic syndrome in association with coronary atherosclerosis. Circulation. 2004;110:803–809. doi: 10.1161/01.CIR.0000138740.84883.9C. [DOI] [PubMed] [Google Scholar]
- 20.Wong ND, Sciammarella MG, Polk D, et al. The metabolic syndrome, diabetes, and subclinical atherosclerosis assessed by coronary calcium. J Am Coll Cardiol. 2003;41:1547–1553. doi: 10.1016/s0735-1097(03)00193-1. [DOI] [PubMed] [Google Scholar]
- 21.Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24:1161–1170. doi: 10.1161/01.ATV.0000133194.94939.42. [DOI] [PubMed] [Google Scholar]
- 22.Christian RC, Harrington S, Edwards WD, Oberg AL, Fitzpatrick LA. Estrogen status correlates with the calcium content of coronary atherosclerotic plaques in women. J Clin Endocrinol Metab. 2002;87:1062–1067. doi: 10.1210/jcem.87.3.8354. [DOI] [PubMed] [Google Scholar]