Abstract
Background.
We tested the hypothesis that a higher level of social activity was associated with decreased risk of incident disability in older adults.
Methods.
Data came from older adults in the Rush Memory and Aging Project, an ongoing longitudinal cohort study of aging. Analyses were restricted to persons without clinical dementia and reporting no need for help performing any task in the particular functional domain assessed. Participants were followed for an average of 5.1 years (SD = 2.5). Social activity, based on 6 items (visiting friends or relatives; going to restaurants, sporting events, or playing games; group meetings; church/religious services; day or overnight trips; unpaid community/volunteer work), was assessed at baseline. Disability in basic activities of daily living, mobility disability, and instrumental activities of daily living was assessed annually. Proportional hazard models adjusted for age, sex, and education were used to examine the association between social activity and incident disability. Fully adjusted models included terms for depression, vascular diseases and risk factors, body mass index, social networks, and self-reported physical activity.
Results.
In fully adjusted models, among 954 persons without baseline disability, the risk of developing disability in activities of daily living decreased by 43% (hazard ratio = 0.57, 95% confidence interval = 0.46, 0.71) for each additional unit of social activity. Social activity was also associated with decreased risk of developing mobility disability (hazard ratio = 0.69, 95% confidence interval = 0.54, 0.88) and disability in instrumental activities of daily living (hazard ratio = 0.71, 95% confidence interval = 0.55, 0.93).
Conclusions.
Social activity is associated with a decreased risk of incident disability in activities of daily living, mobility, and instrumental activities of daily living, among community-dwelling older adults.
Keywords: Disability, Longitudinal, Social activity
SOCIAL activity has long been recognized as an essential component of healthy aging (1) and is associated with a decreased risk of adverse health outcomes including depression (2), cognitive decline (3), dementia (4), motor decline (5), and mortality (6). Social activity also may be related to better everyday functioning and less disability in old age, but limited data are available from longitudinal studies and findings have been mixed, with studies reporting positive associations (7–9), associations only in certain age ranges (10,11) or only one gender (males 12,13, females 14), and even negative associations (15). Importantly, prior studies that have systematically examined this relationship have not focused on the earliest onset of incident disability in persons starting with no disability (7,15) or have only examined onset of one type of disability (10). Establishing a link between social activity and disability in multiple domains along a continuum of severity in persons starting with no disability could help to elucidate social activity's hypothesized role. Persons who do not yet need help with any of a broad range of functional abilities may be those most amenable to intervention, and such work has clear public health implications as the search for modifiable risk factors for disability continues.
We used data from the Rush Memory and Aging Project to test the hypothesis that a higher level of social activity in late life is associated with a lowered risk of incidence of different aspects of disability, that is, disability in basic activity of daily living (ADL), mobility, and instrumental activity of daily living (IADL). As difficulties with household management and mobility are more common and represent less severe disability than difficulty with self-care tasks, these measures represent a continuum of functional ability, ranging from severe disability (ADL) to less severe disability (mobility and IADL). Participants with dementia at baseline, as determined by a rigorous clinical evaluation, were excluded from all analyses to limit recall bias, and analyses were restricted to persons reporting no need for help in performing any task in the particular functional domain assessed. In secondary models, we assessed whether these associations varied by demographic status or were influenced by depression, vascular risk factors, vascular disease, body mass index, social networks, and physical activity. Finally, because one dependency on any of these measures can be a transient state, we conducted a sensitivity analysis repeating our main analyses with a more stringent cut-off point for disability.
METHODS
Participants
The Rush Memory and Aging Project is an ongoing longitudinal cohort study of common chronic conditions of aging (16). Participants were recruited from around 40 retirement and subsidized housing facilities in the Chicago metropolitan area. All participants signed an informed consent agreeing to annual clinical evaluation and organ donation at the time of death. The study was approved by institutional review board of Rush University Medical Center.
The clinical evaluation has been described in detail previously (16). The structured baseline evaluation included medical history and neurological and neuropsychological examinations. Annual follow-up evaluations were identical to the baseline evaluation in essential details, with examiners blinded to previous data. At each evaluation, diagnosis of dementia or Alzheimer's disease was performed by an experienced clinician after review of all available data from the clinical evaluation, following the National Institute of Neurologic and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association criteria (17).
At the time of these analyses, 1,327 participants had completed a baseline evaluation. Of these, 111 persons met the criteria for dementia, 124 died before or had not yet reached their first follow-up, and another 138 persons reported dependence on at least one ADL on the Katz scale (18). This resulted in a final group of 954 participants who completed between 2 and 13 annual evaluations (M = 6.1, SD = 2.5) evaluations. The mean age was 79.6 years (SD = 7.2, range = 55–101), mean education was 14.5 years (SD = 3.2, range = 0–28), and the mean score on the Mini-Mental State Examination (19) was 27.9 (SD = 2.1, range = 18–30) at baseline; 74.7% were women and 88.0% were white, non-Hispanic. The proportions of female and white participants are slightly higher than for this age group in the study's catchment area (65% and 83%, respectively) (20), reflecting the demographic make-up of the area's retirement communities. Out of the 1,471 persons expressing interest based on our recruitment presentations, 90% were enrolled. Among living participants, the follow-up rate for this study is 94%. The primary given reasons for dropout were moving from the area (n = 15), family members not approving the study (n = 14), and being too ill to desire to continue (n = 11).
Assessment of Late-Life Social Activity
A previously established scale (5,16) was used to measure frequency of social activity based on six items (1, go to restaurants, sporting events or teletract [off-track betting], or play bingo; 2, go on day trips or overnight trips; 3, do unpaid community or volunteer work; 4, visit relatives or friends houses; 5, participate in groups, such as senior center, Knights of Columbus, Rosary Society, or something similar; and 6, attend church or religious services). Participants rated how often they participated in each activity based on a 5-point scale (1, once a year or less; 2, several times a year; 3, several times a month; 4, several times a week; and 5, every day or almost every day). The items were summed and divided by the total number of items to obtain a composite measure of social activity for analysis.
Assessment of Disability
ADLs were assessed using a modified version of the Katz Index (18). Participants were asked to rate their ability to perform (no help, help, unable to do) six activities: feeding, bathing, dressing, toileting, transferring, and walking across a small room. Mobility disability was assessed using the Rosow–Breslau scale (21) asked whether participants could perform three tasks that require mobility and strength without help: walking up and down a flight of stairs, walking a half mile, and doing heavy housework. IADLs were assessed using items from the Duke Older Americans Resources and Services project (22). Participants were asked to rate their ability to perform (no help, help, unable to do) eight activities: telephone use, meal preparation, money management, medication management, light and heavy housekeeping, shopping, and local travel. For each measure, participants needing help with (ie, dependency) or unable to perform one or more task were classified as having disability.
Other Covariates
Depressive symptoms were measured using a 10-item version of the Center for Epidemiologic Studies of Depression scale (23). Summary scores indicating number of vascular risk factors (hypertension, diabetes mellitus, and smoking) and vascular diseases (myocardial infarction, congestive heart failure, claudication, and stroke) were created based on self-report, clinical examination, and medical inspection as previously described (24). Body mass index was calculated as weight in kilograms divided by height in meters squared. Social network size was recorded as the number of children, family, and friends participants had seen at least once a month (25). Self-report physical activity assessed five common exercise activities: walking for exercise, gardening or yardwork, calisthenics or general exercise, bicycle riding, and swimming or water exercise (26). Time engaged in each activity was summed and expressed as hours of activity per week, as previously described (27).
Data Analysis
Spearman correlations and t tests were used to assess the relationship between late-life social activity and demographic variables at baseline. t tests and nonparametric tests (chi-square and Wilcoxon rank-sum tests) were used to compare the baseline characteristics of participants who became disabled versus those who did not on each of the disability measures. To examine the associations between social activity and risk of incident disability, we used Cox proportional hazards models (28) adjusted for age, sex, and education with social activity centered at its mean (core models) run separately for each disability measure. In each model, only participants without any dependency in the particular disability were included in the analysis and participants were censured from further analysis if they developed disability. In subsequent models, interaction terms were added to examine whether the associations between social activity and risk of disability varied by demographic characteristics. Models stratified by sex were also examined. To examine whether the associations between social activity and disability were independent of covariates, the core models were repeated including these variables. Finally, to examine whether findings depended on the cut-off point used to define disability, as done in prior studies (29), we repeated the core models with disability defined as dependence in at least two tasks using the same analytic cohort of persons with zero dependencies at baseline. Model diagnostics were performed on the core models using analytic and graphical techniques, including checking the assumption of constant hazard over follow-up. Programming was done in SAS version 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
Baseline social activity scores ranged from 1.0 to 4.17 (M = 2.60, SD = 0.57), with higher values indicating more frequent participation in social activity. Persons with higher levels of social activity were younger (r = −.15, p < .001), more educated (r = .12, p < .001), and had fewer depressive symptoms (r = −.08, p = .02), less vascular disease (r = −.08, p = .01), larger social networks (r = .24, p < .001), and higher levels of physical activity (r = .18, p < .001) than those with lower levels of social activity. There was no significant correlation with body mass index or vascular risk factors. Women had higher levels of social activity (M = 2.63, SD = 0.55) than men (M = 2.52, SD = 0.60), t952 = 2.74, p = .006.
Social Activity and Risk of Incident ADL Disability
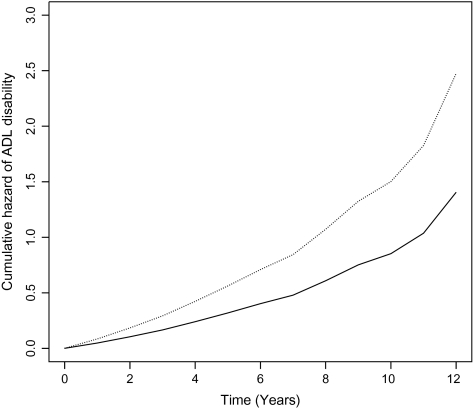
Over a mean of 5.1 years (SD = 2.5) of follow-up, 364 persons (38% of 954) developed ADL disability. Differences between those who did and did not develop ADL disability over follow-up are listed in Table 1. In a Cox proportional hazards model controlling for age, sex, and education, the relative risk of incident disability decreased by 46% for every one-point increase in frequency of social activity (Table 2). Because the association of social activity with ADL disability may vary by age, sex, or education, we repeated the previous analysis with additional terms to test for interactions with these demographic variables. No significant interactions were found (data not shown), but in separate models for men and women, the association was stronger for men (hazard ratio [HRmen] = 0.42, 95% confidence interval [CI]: 0.27, 0.64 vs. HRwomen = 0.59, 95% CI: 0.47, 0.74). We then repeated the initial model with terms to control for the effects of social networks, physical activity, depression, vascular risk factors, vascular disease, and body mass index. The association between social activity and disability remained significant and was essentially unchanged after adjustment for covariates (Table 2). As shown in Figure 1, a person who reported high level of social activity (score = 3.3, 90th percentile) was about twice as likely to remain free of ADL disability than a person with a low level of social activity (score = 1.8, 10th percentile).
Table 1.
Baseline Characteristics of Participants Who Became Disabled Versus Those Who Did Not Become Disabled on the Katz Activity of Daily Living (ADL) Scale, Roslow–Breslau Scale, and Instrumental Activity of Daily Living (IADL)
| ADL |
Roslow–Breslau |
IADL |
||||
| Disabled |
Not disabled |
Disabled |
Not disabled |
Disabled |
Not disabled |
|
| Characteristics | n = 364 | n = 590 | n = 361 | n = 218 | n = 353 | n = 189 |
| Social activity score | 2.46 (0.57)** | 2.69 (0.54) | 2.60 (0.55)* | 2.76 (0.51) | 2.65 (0.52)* | 2.80 (0.54) |
| Age (SD) | 81.98 (6.29)** | 78.17 (7.28) | 80.39 (6.11)** | 75.45 (7.76) | 79.61 (6.35)** | 74.62 (7.30) |
| % Women | 281 (77%) | 432 (73%) | 261 (72%) | 142 (65%) | 254 (72%)* | 117 (62%) |
| Years of education | 14.45 (2.93) | 14.47 (3.29) | 14.72 (2.97) | 14.81 (3.81) | 14.60 (3.09) | 14.79 (3.93) |
| Center for Epidemiologic Studies of Depression scale | 1.31 (1.78) | 1.17 (1.71) | 1.07 (1.62) | 0.98 (1.64) | 1.04 (1.59) | 0.93 (1.60) |
| Vascular risk sum | 1.10 (0.79) | 1.11 (0.83) | 1.02 (0.81) | 1.06 (0.82) | 1.05 (0.81) | 1.02 (0.79) |
| Vascular disease sum | 0.36 (0.61)** | 0.27 (0.55) | 0.27 (0.55)* | 0.16 (0.40) | 0.29 (0.57)* | 0.16 (0.40) |
| Body mass index | 27.55 (5.29)** | 26.85 (4.97) | 26.64 (4.65) | 26.46 (4.54) | 26.98 (5.05) | 27.06 (4.71) |
| Social networks | 6.53 (5.43) | 7.23 (6.27) | 6.89 (5.41) | 7.56 (7.15) | 7.49 (6.05) | 7.85 (7.57) |
| Physical activity score | 2.60 (2.99)** | 3.59 (4.08) | 3.27 (3.37)* | 4.43 (4.51) | 3.37 (3.41)* | 4.53 (4.77) |
*Difference between disabled and nondisabled group significant at 0.001 < p < 0.05.
Difference between disabled and nondisabled group significant at p < 0.001.
Table 2.
Results From Cox Proportional Hazards Models of Association Between Social Activity and Incident Disability on the Katz Activity of Daily Living (ADL) Scale, Roslow–Breslau Scale, and Instrumental Activity of Daily Living (IADL)
| ADL |
Roslow–Breslau |
IADL |
|||||||
| Hazard ratio (HR) | 95% Confidence interval (CI) | p | HR | 95% CI | P | HR | 95% CI | p | |
| Core model | 0.54 | 0.44, 0.67 | <0.001 | 0.65 | 0.51, 0.82 | <0.001 | 0.65 | 0.51, 0.84 | <0.001 |
| Fully adjusted† | 0.57 | 0.46, 0.71 | <0.001 | 0.69 | 0.54, 0.88 | 0.003 | 0.71 | 0.55, 0.93 | 0.01 |
*Adjusted for age, sex, and education.
Adjusted for age, sex, education, depression, vascular risk factors, vascular diseases, body mass index, social networks, and physical activity.
Figure 1.
Cumulative hazard of activity of daily living disability. From Cox proportional hazards models adjusted for age, sex, education, depression, vascular diseases and risk factors, body mass index, social networks, and self-reported physical activity. Solid line = 90th percentile of social activity (score = 3.3) and dotted line = 10th percentile of social activity (score = 1.8).
Social Activity and Risk of Incident Mobility Disability
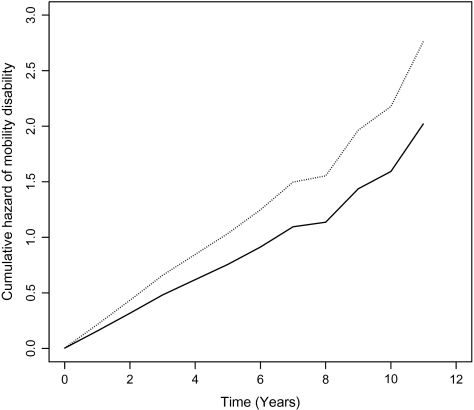
Of the 579 persons (61% of 954) who reported no mobility disability at baseline, 361 persons (62% of 579) developed mobility disability over a mean of 5.3 (SD = 2.6) years of follow-up. Differences between those who did and did not develop mobility disability over follow-up are listed in Table 1. In the Cox proportional hazards model adjusted for age, sex, and education, the relative risk of incident mobility disability decreased by 35% for every one-point increase in frequency of social activity (Table 2). The association of social activity with mobility disability did not vary significantly by age, sex, or education (data not shown), though in stratified models, the association was stronger for men (HRmen = 0.53, 95% CI: 0.35, 0.80 vs. HRwomen = 0.73, 95% CI: 0.55, 0.97). After adjustment for covariates, the association was slightly attenuated, but remained statistically significant (Table 2). As shown in Figure 2, a person who reported high level of social activity (score = 3.3, 90th percentile) was 1.5 times as likely to remain free of mobility disability as a person with a low level of social activity (score = 2.0, 10th percentile).
Figure 2.
Cumulative hazard of mobility disability. From Cox proportional hazards models adjusted for age, sex, education, depression, vascular diseases and risk factors, body mass index, social networks, and self-reported physical activity. Solid line = 90th percentile of social activity (score = 3.3) and dotted line = 10th percentile of social activity (score = 2.0).
Social Activity and Risk of Incident IADL Disability
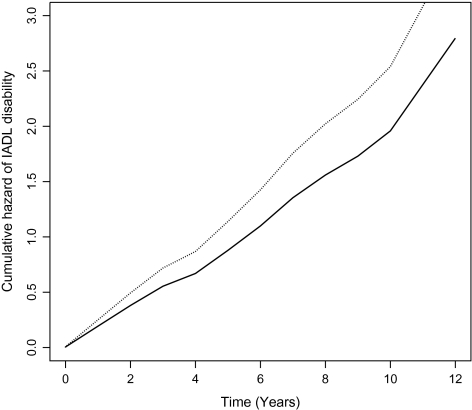
Finally, because relatively little is known about the relationship of social activity with the risk of developing IADL disability, which often occurs at the beginning of the disablement process, we examined this association. These analyses were restricted to the 542 (57% of 954 persons) who reported no IADL disability at baseline. Over a mean of 5.3 (SD = 2.6) years of follow-up, 353 persons (65% of 542) developed disability in IADLs. Differences between those who did and did not develop IADL disability over follow-up are listed in Table 1. In the Cox proportional hazards model adjusted for age, sex, and education, the relative risk of incident IADL disability decreased by 35% for every one-point increase in frequency of social activity (Table 2). Because the IADL scale includes an item that is similar to items in the social activity measure (local travel), we reran the analysis with this item removed, and results were essentially the same (HR = 0.68, 95% CI: 0.54, 0.87); thus the full IADL scale was used for all analyses. The association of social activity with IADL disability did not vary significantly by age, sex, or education (data not shown), though in stratified models the association was stronger for men (HRmen = 0.57, 95% CI: 0.36, 0.88 vs. HRwomen = 0.71, 95% CI: 0.53, 0.96). After adjustment for covariates, the association was slightly attenuated but remained statistically significant (Table 2). As shown in Figure 3, a person who reported high level of social activity (score = 3.3, 90th percentile) was 1.5 times as likely to remain free of IADL disability as a person with a low level of social activity (score = 2.0, 10th percentile).
Figure 3.
Cumulative hazard of instrumental activity of daily living disability. From Cox proportional hazards models adjusted for age, sex, education, depression, vascular diseases and risk factors, body mass index, social networks, and self-reported physical activity. Solid line = 90th percentile of social activity (score = 3.3) and dotted line = 10th percentile of social activity (score = 2.0).
Sensitivity Analyses With Alternate Cut-off Point for Disability
Though a single dependency on any of the three disability measures examined previously is commonly used to define disability, older persons may transition into and out of disability using such a cut-off point (30). Therefore, we repeated the core models for each of the three disability measures with a more stringent definition of disability, that is,, that is, dependency on two or more tasks. With this cut-off point, 208 persons developed ADL disability, 190 persons developed mobility disability, and 195 persons developed IADL disability. The associations between social activity and incident disability were very similar to the original core model estimates for ADL disability (HR = 0.54, 95% CI 0.44, 0.67, p < .001), mobility disability (HR = 0.62, 95% CI 0.47, 0.83, p = .001), and IADL disability (HR = 0.60, 95% CI 0.44, 0.82, p = .001).
DISCUSSION
In a large, community-based cohort of older persons free of dementia, more frequent social activity was associated with a reduced risk of developing disability in three domains: ADLs, mobility, and IADLs. Thus, social activity appears to be associated with disability along a continuum of functional ability ranging from activities requiring advanced facilities (ie, IADLs) and physical mobility (Rosow–Breslau) to the ability to perform basic self-care tasks (ADLs). These results were robust to adjustment for depressive symptoms, vascular risk factors and disease, body composition, social networks, and physical activity. Associations also persisted in sensitivity analyses examining a more severe level of disability as the study outcome. These findings indicate that more socially active older persons may be less likely to become disabled.
Gerontologists have long recognized that older persons who have higher levels of daily activity (31) and larger social networks (32–35) have less disability in later life. Recently, it has been suggested that social activity, in particular, may confer health benefits to older persons above and beyond those provided by either physical activity (6) or the structural properties of social relationships (ie, size of network) (36). Some studies have shown that social activity is associated with disability as a secondary objective (8,9,11–14), but of the three studies that systematically examined social activity as the primary predictor, two examined change in functional status in persons with and without impairments at baseline (7,15), and the other included only one follow-up observation 1.5 years after baseline and did not differentiate between disability in ADLs and IADLs (10). Our findings expand upon previous research in a number of ways. First, we tested the relationship between social activity and first onset of disability along a continuum of function including an early manifestation of disability, IADL disability, among persons without any evidence of disability at baseline. Second, our incident analysis included longer follow-up and more observations than other studies. Third, we were able to exclude persons with dementia as determined by a rigorous clinical evaluation, and all data on social activity and functional status were assessed through self-report (rather than proxy report); thus, our findings are less likely to be influenced by recall bias or inaccurate reporting. Finally, our cohort was older (mean age of 82 years) than the cohorts in previous studies. Our results indicate consistent associations of social activity with various types of disability even among very old persons and in both men and women.
The mechanisms underlying the association between social activity and disability are unknown. Social activity may reinforce the neural networks and musculoskeletal function required to maintain functional dependence in the face of declining physiologic reserve capacity in later life, in what may be a case of “use it or lose it” with regard to function. Indeed, work by our group has shown that social activity is associated with a slower rate of decline in motor function (5). That association was independent of physical activity levels, as was the association of social activity and disability in the current study of disability. Thus, although socially active older adults tend to be more physically active and physical activity is associated with a reduced risk of disability (37), these findings suggest alternate pathways aside from the physiologic benefits of exercise (6). As a caveat, we adjusted for specific exercise activities, so it is possible that observed associations were at least partially due to the benefits conferred by more general forms of physical activity inherent to social activities. From a psychosocial perspective, social activity may provide and reinforce meaningful social roles, thereby providing a sense of value and belonging to an older adult's post-retirement life (38). This sense of attachment to family, friends, and community may provide a strong motivation to maintain functional performance in later life (10). Voluntarily chosen social activities may be a better indicator of this sense of attachment than social network size (not associated with disability onset in our adjusted models), which could include ties that involve neutral or even negative social interactions. This may be especially important for older men who frequently have smaller social networks (39), and there was some evidence that social activity had a stronger association with reduced risk for disability in men. More research is needed to inform potential gender differences in this relationship. Finally, aspects of social integration have been associated with positive physiologic responses including better cardiovascular function and immune response (40,41) and reduced cortisol response to stress (42). Alternatively, because social activity requires a certain degree of functional capacity, we cannot rule out the possibility that low social activity is not a true risk factor for disability but rather a sentinel indicator of impending disability.
Strengths of this study include the use of a large, well-characterized community-based cohort of older persons free of dementia with an average of six annual evaluations and a high rate of follow-up participation. We measured social activity using an established measure of late-life social activities that has been correlated with other health outcomes (5,43), and disability using three separate measures of disability that measure different domains of activity in which older persons commonly experience difficulty. Limitations of this study include the use of a volunteer cohort recruited from retirement homes who have agreed to annual evaluations and postmortem organ donation, which may limit generalizeability to the general older U.S. population. Social activity and disability were measured by self-report, and inferences may be subject to recall bias or same-source bias. Furthermore, the content validity of the IADL scale may be questioned, as reasons for not performing certain items may be more related to characteristics such as gender or environment than to actual disability. Despite these limitations in measurement, the findings were relatively consistent across three different measures of disability, and persons with dementia were excluded to limit inaccuracies in reporting. Finally, in conducting an incident analysis, we treated disability as a dichotomous variable and an absorbing state. Although this is only one of several methods of operationalizing disability, it is a commonly used method in research and clinical settings, and prior research has shown that, although older persons can transition in and out of disability (30), those who are disabled at any point in time are likely to remain disabled or show further progression of disability (44). Findings from secondary analyses utilizing an alternate cut-off point for disability were very similar. Although further research on the relationship between social activity and disability using more sophisticated transition models is warranted, this study suggests that more socially active older persons are less likely to become disabled. Future research is needed to determine whether interventions aimed at increasing late-life social activity can play a part in delaying or preventing disability.
FUNDING
Illinois Department of Public Health to B.D.J.; National Institute on Aging (R01AG17917 to D.A.B., R01AG34374 to P.A.B., R01AG33678 to P.A.B., R01AG24480 to A.S.B.); Robert C. Borwell Endowment Fund to D.A.B.
Acknowledgments
We are indebted to the participants and the staff of the Rush Memory and Aging Project and the Rush Alzheimer's Disease Center for this work and to Sue Leurgans, PhD, for biostatistical consultation.
References
- 1.Rowe JW, Kahn RL. Successful aging. Gerontologist. 1997;37:433–440. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- 2.Glass TA, De Leon CF, Bassuk SS, Berkman LF. Social engagement and depressive symptoms in late life: longitudinal findings. J Aging Health. 2006;18:604–628. doi: 10.1177/0898264306291017. [DOI] [PubMed] [Google Scholar]
- 3.Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med. 1999;131:165–173. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]
- 4.Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–353. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- 5.Buchman AS, Boyle PA, Wilson RS, Fleischman DA, Leurgans S, Bennett DA. Association between late-life social activity and motor decline in older adults. Arch Intern Med. 2009;169:1139–1146. doi: 10.1001/archinternmed.2009.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glass TA, de Leon CM, Marottoli RA, Berkman LF. Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ. 1999;319:478–483. doi: 10.1136/bmj.319.7208.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unger JB, Johnson CA, Marks G. Functional decline in the elderly: evidence for direct and stress-buffering protective effects of social interactions and physical activity. Ann Behav Med. 1997;19:152–160. doi: 10.1007/BF02883332. [DOI] [PubMed] [Google Scholar]
- 8.Zunzunegui MV, Rodriguez-Laso A, Otero A, et al. Disability and social ties: comparative findings of the CLESA study. Eur J Ageing. 2005;2:40–47. doi: 10.1007/s10433-005-0021-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michael YL, Berkman LF, Colditz GA, Kawachi I. Living arrangements, social integration, and change in functional health status. Am J Epidemiol. 2001;153:123–131. doi: 10.1093/aje/153.2.123. [DOI] [PubMed] [Google Scholar]
- 10.Avlund K, Lund R, Holstein BE, Due P. Social relations as determinant of onset of disability in aging. Arch Gerontol Geriatr. 2004;38:85–99. doi: 10.1016/j.archger.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Grand A, Grosclaude P, Bocquet H, Pous J, Albarede JL. Predictive value of life events, psychosocial factors and self-rated health on disability in an elderly rural French population. Soc Sci Med. 1988;27:1337–1342. doi: 10.1016/0277-9536(88)90198-0. [DOI] [PubMed] [Google Scholar]
- 12.Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010;39:319–326. doi: 10.1093/ageing/afq020. [DOI] [PubMed] [Google Scholar]
- 13.Nilsson CJ, Lund R, Avlund K. Cohabitation status and onset of disability among older Danes: is social participation a possible mediator? J Aging Health. 2008;20:235–253. doi: 10.1177/0898264307310474. [DOI] [PubMed] [Google Scholar]
- 14.Strawbridge WJ, Camacho TC, Cohen RD, Kaplan GA. Gender differences in factors associated with change in physical functioning in old age: a 6-year longitudinal study. Gerontologist. 1993;33:603–609. doi: 10.1093/geront/33.5.603. [DOI] [PubMed] [Google Scholar]
- 15.Mendes de Leon CF, Glass TA, Berkman LF. Social engagement and disability in a community population of older adults: the New Haven EPESE. Am J Epidemiol. 2003;157:633–642. doi: 10.1093/aje/kwg028. [DOI] [PubMed] [Google Scholar]
- 16.Bennett DA, Schneider JA, Buchman AS, Mendes de Leon C, Bienias JL, Wilson RS. The Rush Memory and Aging Project: study design and baseline characteristics of the study cohort. Neuroepidemiology. 2005;25:163–175. doi: 10.1159/000087446. [DOI] [PubMed] [Google Scholar]
- 17.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 18.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Census Bureau. Census 2000 Summary Table 1; Using American Fact Finder. 2010. http://factfinder.census.gov. [Google Scholar]
- 21.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 22.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 23.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]
- 24.Boyle PA, Wilson RS, Aggarwal NT, et al. Parkinsonian signs in subjects with mild cognitive impairment. Neurology. 2005;65:1901–1906. doi: 10.1212/01.wnl.0000188878.81385.73. [DOI] [PubMed] [Google Scholar]
- 25.Bennett DA, Schneider JA, Tang Y, Arnold SE, Wilson RS. The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol. 2006;5:406–412. doi: 10.1016/S1474-4422(06)70417-3. [DOI] [PubMed] [Google Scholar]
- 26.McPhillips JB, Pellettera KM, Barrett-Connor E, Wingard DL, Criqui MH. Exercise patterns in a population of older adults. Am J Prev Med. 1989;5:65–72. [PubMed] [Google Scholar]
- 27.Wilson RS, Mendes De Leon CF, Barnes LL, et al. Participation in cognitively stimulating activities and risk of incident Alzheimer disease. JAMA. 2002;287:742–748. doi: 10.1001/jama.287.6.742. [DOI] [PubMed] [Google Scholar]
- 28.Cox DR. Regression models and life tables. J Soc Stat Soc B. 1972;74:187–220. [Google Scholar]
- 29.Krueger KR, Wilson RS, Shah RC, Tang Y, Bennett DA. Personality and incident disability in older persons. Age Ageing. 2006;35:428–433. doi: 10.1093/ageing/afl028. [DOI] [PubMed] [Google Scholar]
- 30.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 31.Everard KM, Lach HW, Fisher EB, Baum MC. Relationship of activity and social support to the functional health of older adults. J Gerontol B Psychol Sci Soc Sci. 2000;55:S208–S212. doi: 10.1093/geronb/55.4.s208. [DOI] [PubMed] [Google Scholar]
- 32.Seeman TE, Bruce ML, McAvay GJ. Social network characteristics and onset of ADL disability: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci. 1996;51:S191–S200. doi: 10.1093/geronb/51b.4.s191. [DOI] [PubMed] [Google Scholar]
- 33.Mendes de Leon CF, Glass TA, Beckett LA, Seeman TE, Evans DA, Berkman LF. Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. J Gerontol B Psychol Sci Soc Sci. 1999;54:S162–S172. doi: 10.1093/geronb/54b.3.s162. [DOI] [PubMed] [Google Scholar]
- 34.Mendes de Leon CF, Gold DT, Glass TA, Kaplan L, George LK. Disability as a function of social networks and support in elderly African Americans and Whites: the Duke EPESE 1986–1992. J Gerontol B Psychol Sci Soc Sci. 2001;56:S179–S190. doi: 10.1093/geronb/56.3.s179. [DOI] [PubMed] [Google Scholar]
- 35.Unger JB, McAvay G, Bruce ML, Berkman L, Seeman T. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 1999;54:S245–S251. doi: 10.1093/geronb/54b.5.s245. [DOI] [PubMed] [Google Scholar]
- 36.House JS, Robbins C, Metzner HL. The association of social relationships and activities with mortality: prospective evidence from the Tecumseh Community Health Study. Am J Epidemiol. 1982;116:123–140. doi: 10.1093/oxfordjournals.aje.a113387. [DOI] [PubMed] [Google Scholar]
- 37.Boyle PA, Buchman AS, Wilson RS, Bienias JL, Bennett DA. Physical activity is associated with incident disability in community-based older persons. J Am Geriatr Soc. 2007;55:195–201. doi: 10.1111/j.1532-5415.2007.01038.x. [DOI] [PubMed] [Google Scholar]
- 38.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 39.Antonucci TC, Akiyama H. An examination of sex differences in social support among older men and women. Sex Roles. 1987;17:737–749. [Google Scholar]
- 40.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 41.Cohen S, Gottlieb BH, Underwood LG. Social relationships and health. In: Cohen S, Gottlieb BH, Underwood LG, editors. Measuring and Intervening in Social Support. New York: Oxford University Press; 2000. pp. 3–25. [Google Scholar]
- 42.Ditzen B, Schmidt S, Strauss B, Nater UM, Ehlert U, Heinrichs M. Adult attachment and social support interact to reduce psychological but not cortisol responses to stress. J Psychosom Res. 2008;64:479–486. doi: 10.1016/j.jpsychores.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 43.Wilson RS, Krueger KR, Arnold SE, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- 44.Hardy SE, Allore HG, Guo Z, Dubin JA, Gill TM. The effect of prior disability history on subsequent functional transitions. J Gerontol A Biol Sci Med Sci. 2006;61:272–277. doi: 10.1093/gerona/61.3.272. [DOI] [PubMed] [Google Scholar]