Abstract
Objectives
To compare the efficacy of antidepressant drugs and generic counselling for treating mild to moderate depression in general practice. To determine whether the outcomes were similar for patients with randomly allocated treatment and those expressing a treatment preference.
Design
Randomised controlled trial, with patient preference arms. Follow up at 8 weeks and 12 months and abstraction of GP case notes.
Setting
31 general practices in Trent region.
Participants
Patients aged 18-70 who met research diagnostic criteria for major depression; 103 patients were randomised and 220 patients were recruited to the preference arms.
Main outcome measures
Difference in mean Beck depression inventory score; time to remission; global outcome assessed by a psychiatrist using all data sources; and research diagnostic criteria.
Results
At 12 months there was no difference between the mean Beck scores in the randomised arms. Combining the randomised and patient preference groups, the difference in Beck scores was 0.4 (95% confidence interval –2.7 to 3.5). Patients choosing counselling did better than those randomised to it (mean difference in Beck score 4.6, 0.0 to 9.2). There was no difference in the psychiatrist's overall assessment of outcome between any of the groups. 221/265 (83%) of participants with a known outcome had a remission. Median time to remission was shorter in the group randomised to antidepressants than the other three groups (2 months v 3 months). 33/221 (15%) patients had a relapse.
Conclusions
Generic counselling seems to be as effective as antidepressant treatment for mild to moderate depressive illness, although patients receiving antidepressants may recover more quickly. General practitioners should allow patients to have their preferred treatment.
What is already known on this topic
Antidepressants and specific psychological interventions are effective in major depression.
Generic counselling has not previously been compared with antidepressants in primary care
What this study adds
12 months after starting treatment, generic counselling is as effective as antidepressants
Patients treated with antidepressants may recover more quickly
Given a choice, more patients opt for counselling
Patients who choose counselling may benefit more than those with no strong preference
Introduction
Both antidepressants and psychological interventions have been shown to be effective in patients with major depression.1,2 The counselling and antidepressants in primary care study was set up to compare the efficacy and cost effectiveness of antidepressant drugs and generic counselling in a naturalistic general practice setting. The short term outcomes from this study (at eight weeks) have been published.3 We report here the outcomes at 12 months.
Participants and methods
Recruitment and treatment
Full details of the methods have been published.3 Briefly, we invited a random sample of 410 general practices in the Trent health region to enter patients into the trial. General practitioners recruited participants and obtained informed consent. Eligible patients were those aged 18-70 years who met the research diagnostic criteria (assessed by the general practitioner using a checklist) for major depression.4 We excluded patients with psychosis, suicidal tendencies, postnatal depression, a recent bereavement, or drug or alcohol misuse. The study was approved by 12 local research ethics committees.
For patients who agreed to randomisation, treatment was allocated by telephone with a randomisation strategy using blocks of four stratified by practice. Patients who refused randomisation but agreed to participate in the patient preference trial were given their choice of treatment. Treatment and follow up were identical in the randomised and patient preference groups.
We provided general practitioners with written guidelines on routine drug treatment of depression. Patients in the counselling arms were given six sessions by experienced counsellors, who adopted the counselling approach that they believed to be most suitable.
Data collection and follow up
All patients completed the Beck depression inventory5 and SF-36 questionnaire at enrolment.6,7 At the follow up visits eight weeks and 12 months after enrolment, the general practitioner completed a form that included the research diagnostic criteria and the patient was asked to complete a form including the Beck depression inventory and SF-36. Patients who did not keep their follow up appointments were asked to complete the forms at home.
We also abstracted information from general practitioners' case notes. This included general practitioner appointments; psychiatric and other hospital referrals; inpatient treatment; prescribed treatments (both antidepressants and other drugs); and referral to counsellors outside the study protocol.
Outcome measures
The main outcome measures at 12 months were Beck depression inventory score, time to remission,8,9 global outcome (classified as good, moderate, poor, or unknown), and research diagnostic criteria. Remission was defined as a score of less than 4 on the research diagnostic criteria, a Beck score of less than 10, or clear documentation in the general practitioner's notes that the patient was well. Relapse was defined as deterioration within six months of remission, and recurrence as deterioration after six months of remission.
Global outcome was assessed by a psychiatrist (NB) blind to treatment allocation using the research diagnostic criteria, Beck score, and general practitioners' notes. If the research diagnostic criteria and Beck scores were not available, global outcome was estimated from the case notes. The outcome was considered good if the patient responded to treatment within eight weeks and then remained well; moderate if the patient was slow to respond but then remained well or was well initially and then became unwell; and poor if the patient remained depressed throughout. The criteria for being well were the same as the criteria for remission.
We masked abstracts of general practitioners' notes by erasing words identifying the treatment group. To check the effectiveness of the masking, the assessor recorded the treatment group to which she thought that the first 20 patients had been allocated.
Patients with unknown outcomes or time to remission were independently reviewed by two senior psychiatrists (CD, AL). For assessments based on Beck scores and where the scores at eight weeks and 12 months were both high, it was assumed that the patient had remained unwell in the intervening period; if the patient was not in remission at eight weeks but was in remission at 12 months, the time to remission was taken as 12 months in all comparative analyses.
The secondary outcome measures were change in SF-36 score, number of psychiatric referrals, number of hospital admissions, and suicide.
Statistical analysis
We conducted analyses to compare the randomised groups and investigate the interaction between treatment outcome and whether the patients were randomised. Before the study started we decided that if there was no evidence of interaction, the randomised and patient preference groups would be combined to investigate treatment outcome in all patients. Because the study had low power to detect interactions, we would also do a stratified analysis. If an interaction was found between treatment and preference interaction we would do only a stratified analysis.
We analysed all data using SPSS version 8. We investigated differences in baseline characteristics and outcome measures between the groups using descriptive statistics, unpaired t tests, χ2 tests, and Fisher's exact test. The analyses stratified by randomised or patient preference status used Mantel-Haenszel techniques. The time to remission was analysed by the Kaplan-Meier method, and differences were tested with the logrank test.10,11 We censored observations at the last recorded visit to the general practitioner.
Study size
We originally planned to use a binary outcome: recovery or not, based on change in Beck score. With a recovery rate of 50% in one group and 40% in the other, two sided significance of 0.05, and power of 0.90, we required 400 patients in each arm. Because recruitment was slow, we resized the study using the difference in mean Beck scores at 12 months as the outcome. Based on a clinically important difference between the groups in mean Beck scores of 5 points, and assuming a standard deviation of 8.3 with two sided significance of 0.05, we required 44 patients per arm for power of 80% and 60 per arm for power of 90%.
Results
Response rates
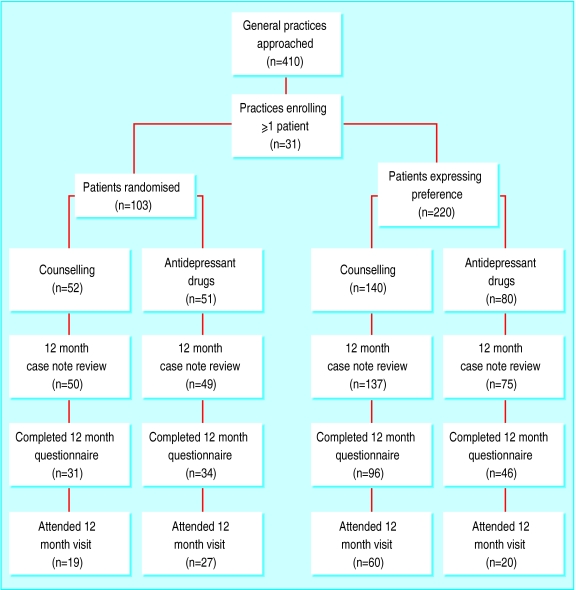
The figure shows the numbers of patients recruited and followed up. There was no systematic difference between the proportions of patients completing the 12 month questionnaire in terms of treatment or whether they were randomised (P=0.34 for heterogeneity between the four groups). Sixty five (63%) patients in the randomised trial completed the Beck depression inventory and SF-36 at 12 months compared with 142 (65%) in the patient preference trial. The proportions of patients in each group who kept their 12 month appointment differed (P=0.01), with attendance ranging between 25% for patients choosing antidepressants and 53% for those randomised to antidepressants.
We abstracted the general practitioner's notes for 96% (99/103) of patients in the randomised trial and 96% (212/220) in the patient preference. There was sufficient information to carry out the psychiatrist's overall assessment on 79% (81/103) of patients in the randomised trial and 74% (163/220) in the patient preference trial.
Patient characteristics at entry
The patients were predominantly women, there were roughly equal numbers in social classes I/II, III, and IV/V, and 57% were married (table 1). Patients preferring counselling were less severely depressed than the randomised patients or those preferring antidepressants.3
Table 1.
Summary of baseline characteristics. Values are numbers (percentages) unless stated otherwise
| Characteristic | Randomised
|
Patient preference
|
P value for comparison of 4 groups | |||||
|---|---|---|---|---|---|---|---|---|
| Counselling (n=52) | Antidepressants (n=51) | P value | Counselling (n=140) | Antidepressants (n=80) | P value | |||
| Men | 16 (31) | 8 (16) | 0.12 | 36 (26) | 21 (26) | 1.00 | 0.34 | |
| Mean (SD) age | 37.3 (11.2) | 38.4 (11.8) | 0.60 | 36.4 (10.1) | 38.1 (12.7) | 0.27 | 0.60 | |
| Married* | 17/35 (49) | 23/36 (64) | 0.29 | 58/101 (57) | 25/45 (56) | 1.00 | 0.63 | |
| Living alone* | 7/35 (20) | 2/36 (6) | 0.14 | 11/101 (11) | 5/45 (11) | 1.00 | 0.29 | |
| Family history of depression* | 15/34 (44) | 19/36 (53) | 0.47 | 51/94 (54) | 21/43 (49) | 0.56 | 0.76 | |
| Mean (SD) age at onset* | 33.3 (24.2) | 35.6 (18.6) | 0.65 | 35.1 (20.7) | 34.1 (20.6) | 0.79 | 0.96 | |
| Social class*: | ||||||||
| I or II | 6/30 (20) | 12/31 (39) | 0.24 | 38/91 (42) | 12/41 (29) | 0.28 | 0.30 | |
| III non-manual or manual | 12/30 (40) | 11/31 (35) | 34/91 (37) | 16/41 (39) | ||||
| IV or V | 12/30 (40) | 8/31 (26) | 19/91 (21) | 13/41 (32) | ||||
| Beck inventory score: | ||||||||
| Mean (SD) | 27.1 (8.0) | 27.0 (8.0) | 0.97 | 25.8 (7.7) | 25.4 (9.5) | 0.78 | 0.57 | |
| Not known | 2 | 2 | 6 | 8 | ||||
| Research diagnostic criteria score: | ||||||||
| 4 or 5 | 19 (37) | 14 (27) | 0.44 | 59 (42) | 22 (28) | 0.04 | 0.10 | |
| 6-8 | 32 (62) | 36 (71) | 81 (58) | 58 (73) | ||||
| Not known | 1 (2) | 1 (2) | 0 | 0 | ||||
| General practitioner's rating: | ||||||||
| Mild | 12 (24) | 10 (19) | 0.29 | 45 (32) | 10 (13) | 00.001 | 0.004 | |
| Moderate | 33 (66) | 31 (61) | 87 (62) | 62 (78) | ||||
| Severe | 3 (6) | 8 (16) | 5 (4) | 8 (10) | ||||
| Not known | 2 (4)† | 2 (4) | 3 (2) | 0 | ||||
Some patients did not have the telephone interview immediately after recruitment.
Data were not completed by the general practitioner for two further patients.
Beck inventory scores at 12 months
Mean Beck scores did not differ significantly between the two groups in the randomised controlled trial (P=0.49, table 2). There was no evidence for an interaction between treatment and preference (P=0.6) so we combined the randomised and patient preference groups. Mean Beck scores were similar in counselled patients and those receiving antidepressants (13.2 v 12.8, 95% confidence interval for difference −2.7 to 3.5).
Table 2.
Scores on Beck depression inventory scale at 12 months
| Counselling
|
Antidepressants
|
Difference (95% CI) | P value | ||||
|---|---|---|---|---|---|---|---|
| No of patients | Mean (SD) score | No of patients | Mean (SD) score | ||||
| Randomised patients | 31 | 16.7 (11.5) | 34 | 14.6 (13.1) | 2.1 (−4.0 to 8.2) | 0.49 | |
| All patients* | 127 | 13.2 (11.3) | 80 | 12.8 (10.7) | 0.4 (−2.7 to 3.5) | 0.81 | |
Score adjusted for patient preference or randomised group and baseline score for research diagnostic criteria: P=0.34.
We investigated the effect of patient preference by comparing the randomised and patient preference groups for the two treatments separately. There was no difference in the mean Beck scores for the patients treated with antidepressants (mean difference 3.1, 95% confidence interval –1.8 to 7.8), but the patients choosing counselling did better than those randomised to counselling (mean difference 4.6, 95% confidence interval 0.0 to 9.2).
Global outcome and time to remission
We found no differences in global outcome between the randomised or patient preference trials when outcome was split into good or moderate versus poor (table 3). Stratification by randomised or patient preference status gave similar outcomes for antidepressants and counselling (Mantel Haenszel P=0.63). Similar results were obtained by splitting the outcomes into good versus moderate or poor. The treatment allocations were guessed correctly by the assessor in nine of the 20 sets of notes, indicating that the masking was satisfactory.
Table 3.
Global outcome, remission, and relapse in randomised and patient preference groups. Values are numbers (percentages) of patients. Totals exclude missing data but include patients in whom outcome was uncertain
| Randomised patients
|
Patient preference
|
P value for Mantel Haenszel χ2 test | ||||||
|---|---|---|---|---|---|---|---|---|
| Counselling (n=52) | Antidepressants (n=51) | P value | Counselling (n=140) | Antidepressants (n=80) | P value | |||
| Global outcome: | ||||||||
| Good or moderate | 29 (56) | 33 (65) | 0.854* | 90 (64) | 54 (68) | 0.803* | 0.626 | |
| Good | 13 (25) | 21 (41) | 0.196* | 50 (36) | 22 (28) | 0.191* | 0.868 | |
| Ever remitted | 33/48 (69) | 39/50 (78) | 0.633* | 95/129 (74) | 54/78 (69) | 0.872* | 0.739 (yes v no) | |
| Ever relapsed | 5/33 (15) | 4/39 (10) | 0.820† | 18/95 (19) | 6/54 (11) | 0.615* | 0.455 | |
| Outpatient psychiatric referral | 2 (4) | 0 | 0.505† | 10 (7) | 5 (6) | 0.927* | 0.668 | |
| Inpatient treatment for depression | 1‡ (2) | 2 (4) | 0.970† | 2 (1) | 0 | 0.849† | § | |
| Other inpatient treatment | 6 (12) | 8 (16) | 0.711* | 22 (16) | 14 (18) | 0.706* | 0.498 | |
χ2 test.
Fisher's exact test.
One patient attended twice.
Invalid because of small numbers.
Overall, 68% (221/323) of patients had a remission or 83% (221/265) of those with a known outcome. The proportions of patients who had a remission were similar in each group (table 3). Median time to remission was three months in all groups except the group randomised to antidepressants, where the median time to remission was two months (comparing randomised groups logrank statistic 2.74, P=0.1; pooled logrank statistic for randomised and patient preference trials 0.82, P=0.36). Thirty three (15%) of the 221 patients had a relapse. There were no differences between the groups.
Research diagnostic criteria scores
Of the randomised patients who kept their 12 month follow up, nine (47%) in the counselling group were no longer depressed compared with 21 (78%) in the antidepressant group (P=0.07, table 4). When we assumed that all those failing to attend had recovered, then 81% in the counselling group and 88% in the antidepressant group were no longer depressed. The figures when we assumed that patients failing to attend were treatment failures were 17% and 41% respectively (P=0.01).
Table 4.
Comparison of outcome at 12 months on research diagnostic criteria in patients receiving counselling or antidepressants
| Research diagnostic criteria score | Randomised
|
Patient preference
|
|||||
|---|---|---|---|---|---|---|---|
| No (%) counselling | No (%) antidepressants | χ2 test (P value) | No (%) counselling | No (%) anti-depressants | χ2 test (P value) | ||
| Omitting patients with missed visits: | |||||||
| ⩾4 | 10 (53) | 6 (22) | 3.30 (0.07) | 12 (20) | 3 (15) | 0.03 (0.87) | |
| <4 | 9 (47) | 21 (78) | 48 (80) | 17 (85) | |||
| Assuming missed visit is treatment success: | |||||||
| ⩾4 | 10 (19) | 6 (12) | 0.60 (0.44) | 12 (9) | 3 (4) | 1.18 (0.28) | |
| <4 | 42 (81) | 45 (88) | 128 (91) | 77 (96) | |||
| Assuming missed visit is treatment failure: | |||||||
| ⩾4 | 43 (83) | 30 (59) | 6.00 (0.01) | 92 (66) | 63 (79) | 3.55 (0.06) | |
| <4 | 9 (17) | 21 (41) | 48 (34) | 17 (21) | |||
In the patient preference trial, 48 (80%) patients choosing counselling and 17 (85%) choosing antidepressants had recovered at 12 months (P=0.87). If missed appointments were assumed to be treatment successes the outcomes were similar, but if all missed appointments were treatment failures, patients choosing counselling would do better than those choosing antidepressants.
Secondary outcomes
There were no differences in scores between patients randomised to counselling or antidepressants on any of the SF-36 domains (data not shown). The scores were also similar when the randomised and preference arms were combined. Patients who chose counselling did consistently better than those randomised to counselling on all dimensions of the SF-36.
Two (2%) randomised patients and 15 (7%) preference patients were referred for outpatient assessment (P=0.1, table 3). Few patients received inpatient treatment relating to depression, and there were no differences between the groups. There were no differences in the proportions of patients attending as inpatients for unrelated conditions.
One 46 year old man committed suicide two months after enrolling in the study in the patient preference antidepressants arm. His Beck score at entry was 43. In accordance with the study protocol, the patient's general practitioner was notified of this score.
Discussion
The data from our randomised controlled trial suggest that at 12 months follow up generic counselling and antidepressants are equally effective in patients with mild to moderate depression; remission rates are impressive with both treatments. These conclusions are based on the Beck depression inventory scores and the overall assessment by the psychiatrist. Patients treated with antidepressants recovered more quickly than those receiving counselling. A recent randomised comparison of non-directive counselling and general practitioner care found that at four months the counselled patients had improved more than those receiving usual care, but by 12 months there were no differences between the groups.12 The results of the research diagnostic criteria questionnaire are less clear. They are based on less than 50% of patients, the number who returned to their general practitioner at 12 months, and the sensitivity analysis gave divergent results depending on the assumptions made. Choice of treatment seemed to be beneficial, but this applied only to counselling. This finding should be treated with caution as the power of the study to detect interactions was low.
The larger numbers of patients choosing counselling in this trial suggests that patients prefer counselling to antidepressants.3 A survey of people attending general practice had similar findings.13 A higher proportion of patients in the patient preference trial than in the randomised trial were referred to outpatients. This may reflect the slightly higher proportion of people in social classes I and II in the patient preference trial (38% v 30% in randomised trial). Most patients presenting with depression in primary care, however, will not be referred to secondary care.
Several caveats must be taken into account when interpreting these data. Firstly, we had difficulty recruiting patients into the randomised controlled trial. The patient preference arms, although increasing the power of the study, tend to make our findings less robust. Secondly, the counselling offered in the study was of a high standard; patients were referred within two weeks, and all the counsellors were experienced. Thirdly, although we found some benefit associated with choice, we did not investigate the effect of giving an alternative treatment to those with a specific preference.
What conclusions should commissioners and general practitioners draw from this study? Firstly, that both counselling and antidepressant drugs are effective, but antidepressants may result in more rapid recovery. Secondly, that given the choice more patients with depression will choose counselling and those who choose antidepressants are likely to be more severely depressed. We recommend that general practitioners should allow patients to have their choice of treatment. However, if the patient does not have a preference, antidepressant drugs should be prescribed because counselling is a scarce resource that is best reserved for those patients who express a preference for it.
Figure.
Recruitment and follow up of patients
Acknowledgments
We thank Helen Bounds and Joanne Elliott for secretarial and clerical support and Paddy Hawtin for help with data collection. We thank the general practitioners who recruited the patients for this study, and the patients who participated.
Footnotes
Funding: NHS Executive Trent.
Competing interests: None declared.
References
- 1.American Psychiatric Association. Practice guidelines for major depressive disorder in adults. Am J Psychiatry. 1993;150(suppl):4. doi: 10.1176/ajp.150.4.1. [DOI] [PubMed] [Google Scholar]
- 2.Churchill R, Dewey M, Gretton V, Duggan C, Chilvers C, Lee AS. Should general practitioners refer patients with major depression to counsellors? A review of current published evidence. Br J Gen Pract. 1999;49:737–743. [PMC free article] [PubMed] [Google Scholar]
- 3.Counselling versus Antidepressants in Primary Care Study Group. Assessing treatment effectiveness in depression: results from a PRPT trial. Br J Psychiatry. 2000;177:312–318. [Google Scholar]
- 4.Spitzer RL, Endicot J, Robins E. Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- 5.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 6.Brazier JE, Harper R, Jones NMB, O'Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jenkinson C, Coulter A, Wright L. Short form 36 (SF-36) health survey questionnaire: normative data for adults of working age. BMJ. 1993;306:1437–1440. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paykel ES, Priest RG.on behalf of conference participants. Recognition and management of depression in general practice: consensus statement BMJ 19923051198–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frank E. Response, remission, recovery, relapse, recurrence. J Clin Psychiatry. 1991;52(suppl 2):2–16. [Google Scholar]
- 10.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 11.Mantel N, Haenszel P. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 12.Ward E, King M, Lloyd M, Bowen P, Sibbald B, Farrelly S, et al. Randomised controlled trial of non-directive counselling, cognitive behaviour therapy, and usual general practitioner care for patients with depression. I. Clinical effectiveness. BMJ. 2000;321:1383–1388. doi: 10.1136/bmj.321.7273.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Churchill R, Khaira M, Gretton V, Chilvers C, Dewey M, Duggan C, et al. Treating depression in general practice: factors affecting patients' treatment preferences. Br J Gen Pract. 2000;50:905–906. [PMC free article] [PubMed] [Google Scholar]