Abstract
Objective
To compare chemotherapy given at home with outpatient treatment in terms of colorectal cancer patients' safety, compliance, use of health services, quality of life, and satisfaction with treatment.
Design
Randomised controlled trial.
Setting
Large teaching hospital.
Participants
87 patients receiving adjuvant or palliative chemotherapy for colorectal cancer.
Interventions
Treatment with fluorouracil (with or without folinic acid or levamisole) at outpatient clinic or at home.
Main outcome measures
Treatment toxicity; patients' compliance with treatment, quality of life, satisfaction with care, and use of health resources.
Results
42 patients were treated at outpatient clinic and 45 at home. The two groups were balanced in terms of age, sex, site of cancer, and disease stage. Treatment related toxicity was similar in the two groups (difference 7% (95% confidence interval −12% to 26%)), but there were more voluntary withdrawals from treatment in the outpatient group than in the home group (14% v 2%, difference 12% (1% to 24%)). There were no differences between groups in terms of quality of life scores during and after treatment. Levels of patient satisfaction were higher in the home treatment group, specifically with regard to information received and nursing care. There were no significant differences in use of health services.
Conclusions
Home chemotherapy seemed an acceptable and safe alternative to hospital treatment for patients with colorectal cancer that may improve compliance and satisfaction with treatment.
What is already known on this topic
Home chemotherapy programmes have been proposed as an alternative to hospital treatment
However, they are more costly, and there is little evidence on their impact on outcomes such as compliance, quality of life, or use of other health services
What this study adds
Home chemotherapy was not associated with an increased use of health services such as primary care or emergency departments
Home chemotherapy had no effect on patients' quality of life but increased their compliance with treatment and satisfaction, particularly with regard to nursing care
Home chemotherapy seems an acceptable and safe alternative to outpatient treatment that may improve compliance with treatment
Introduction
There is increasing interest in home care as an alternative to hospitalisation, particularly because of its potential for achieving cost savings by reducing levels of inpatient care.1 However, evidence for cost savings from home care has been limited to specific pathologies such as chronic obstructive pulmonary disease.2 The feasibility and cost effectiveness of home care depends on the setting studied, the type of treatment given, and the analytical methods used,3 and few trials have assessed the impact of home care on outcomes that would be relevant in the context of a given organisational change.
Most oncology centres give chemotherapy in an outpatient setting. Chemotherapy is often cited as a procedure that may be suitable for home administration.4,5 However, only one trial has assessed the effect of administering chemotherapy at home (on quality of life, satisfaction, costs, and safety for paediatric cancer patients),6 while one other trial has compared the effectiveness of administering chemotherapy in inpatient and outpatient settings.7 The first of these studies found that administration of selected chemotherapy at home reduced costs, and the second study found that outpatient care was significantly less costly than inpatient care. Recently, two Australian crossover trials produced inconsistent results with regard to patients' preferences for home chemotherapy but consistently indicated that it is more costly than outpatient care, although the benefits to patients (travel time, family costs, etc) were not assessed.8,9
The aim of the present study was to analyse safety, compliance, satisfaction with treatment, quality of life, and use of health services for adult cancer patients receiving chemotherapy for colorectal cancer in an outpatient clinic compared with a home setting.
Participants and methods
Patients
Between October 1997 and October 1998 we selected patients referred to the medical oncology department of the Catalan Institute of Oncology with a diagnosis of colorectal cancer for whom treatment with adjuvant or palliative chemotherapy was indicated. To be eligible for our study, patients had to be between 18 and 75 years old, have a diagnosis of colorectal cancer, and be suitable for treatment with bolus fluorouracil based chemotherapy as adjuvant treatment or as treatment for disseminated disease according to the institutional protocol. We excluded patients living outside a 30 km radius of the hospital. All but one of the patients invited to participate in the study accepted. The patients gave their written informed consent, and the hospital ethics and research committee approved the study protocol.
Randomisation
We randomly assigned the patients to receive chemotherapy either at the outpatient clinic (standard care) or at home. The patient was the randomisation unit. Random numbers were selected in block of eight, stratified according to the type of tumour (colon, rectum, or advanced disease). We calculated sample size (two sided, α=0.05, 1−b=0.80) to detect a difference of 8 (SD 3) between groups for self rated general health status and then increased this calculated sample size (41 patients for each group) by a total of six patients to allow for patients withdrawing from the trial.
Treatment
Colon cancer adjuvant chemotherapy consisted of bolus fluorouracil (450 mg for five consecutive days during the first cycle and once a week thereafter) with levamisole (50 mg/8 hours, oral, for three consecutive days every 15 days) until completion of 12 months' treatment. Rectal cancer adjuvant chemotherapy consisted of bolus fluorouracil (500 mg/m2) for five consecutive days a week (or three consecutive days in case of combined chemoradiotherapy) until completion of six cycles of treatment. Palliative chemotherapy consisted of bolus fluorouracil (425 mg/m2) with folinic acid (20 mg/m2) for five consecutive days a week every four weeks until completion of six to eight cycles if disease was stable or disease progression was observed.
A trained nurse delivered the home chemotherapy. Decisions to modify the dose were made by the medical oncologist at the monthly visit to consider toxicity during the previous cycle. A protocol, including a telephone call to an oncologist, was established in order to manage acute adverse effects that could appear while delivering home chemotherapy.
Outcome measures
Treatment toxicity
—We measured and recorded treatment toxicity every four weeks using the ECOG classification.10 Grade 3 or 4 toxicity resulted in withdrawal from the trial.
Withdrawal from trial—We classified reasons for withdrawing from the trial as unacceptable toxicity of chemotherapy (grade 3 or greater), disease progression, or voluntary withdrawal not related to previous causes. Only the last category was considered as patient non-compliance.
Use of healthcare resources—We asked patients about any unplanned use of primary care or emergency department or hospitalisation. We categorised any use of health services not covered in the protocol, including visits to the emergency department or outpatient clinics and admission to hospital or to a primary care centre. We considered all primary care visits to be unscheduled even when they were related to comorbid conditions.
Quality of life—We measured patients' quality of life with the EORTC QOL-C30 questionnaire.11 This includes five functional scales (physical, role (related to interference of disease with family life or social activities), emotional, cognitive, and social), a global health status quality of life scale, and single measures of symptom severity (fatigue, nausea and vomiting, pain, dyspnoea, insomnia, appetite loss, constipation, diarrhoea, and financial difficulties). We also measured quality of life using the Karnofsky index.12
Satisfaction with health care—We assessed patients' satisfaction using a questionnaire translated into Spanish for this study (available from JMB).13 This included several items that measured general satisfaction with health care received, availability of doctors, nursing availability (related to waiting time), continuity of care, personal qualities of nurses (related to perceived interest in the patient), and communication with doctors and nurses. We scored the responses on a scale of 1 (completely disagree) to 5 (completely agree). Raw scores were linearly transformed to values between 0 and 100. In all domains a higher score indicated greater satisfaction. We determined the internal consistency (reliability) of the scales using Cronbach's coefficient α,14 with coefficients over 0.7 being considered sufficient for group comparisons.15 The α coefficient fell below this threshold in only one domain (nursing availability).
We administered the quality of life and satisfaction questionnaires at the start of the trial, every three months, and at the end of treatment.
Statistical analysis
We calculated point estimates and 95% confidence intervals for the differences in percentages and means between groups. We used analysis of variance for repeated measures to compare patients' quality of life and satisfaction scores, both before and after treatment and between the groups. We calculated means and 95% confidence intervals for the difference in the size of the change between the initial and final questionnaire scores for the two groups.
Results
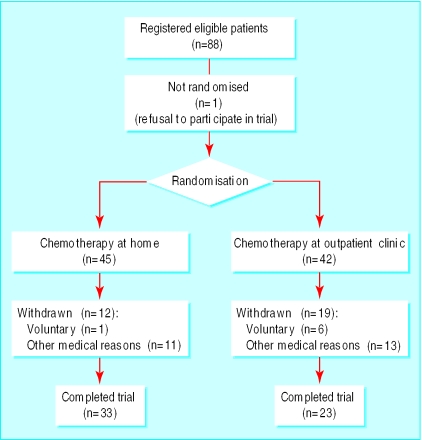
We recruited 87 patients to the trial, 42 assigned to hospital outpatient treatment and 45 to home treatment (figure). The groups were balanced according to age, sex, and type of treatment received (table 1), and there were no differences in toxicity.
Table 1.
Baseline characteristics of 87 patients with colorectal cancer assigned to chemotherapy at hospital outpatient clinic or at home. Values are numbers (percentages) unless stated otherwise
| Characteristic | Treatment
|
|
|---|---|---|
| Outpatient (n=42) | Home (n=45) | |
| Male | 24 (57) | 21 (47) |
| Mean age (years) | 60.8 | 59.8 |
| Site of tumour: | ||
| Colon | 19 (45) | 21 (47) |
| Rectum | 14 (33) | 13 (29) |
| Advanced disease | 9 (21) | 11 (24) |
| Unacceptable treatment toxicity*: | ||
| Haematological | 13 (31) | 12 (27) |
| Biochemical | 0 | 0 |
| Clinical | 15 (36) | 12 (27) |
| Treatment type: | ||
| Palliative | 8 (19) | 9 (20) |
| Adjuvant | 34 (81) | 36 (80) |
| Preoperative radiotherapy | 3 (7) | 2 (4) |
| Postoperative radiotherapy | 12 (29) | 14 (31) |
Grade 3 or 4 on ECOG classification.
Withdrawals and treatment toxicity—Voluntary withdrawals from chemotherapy were significantly higher in the outpatient treatment group (difference 12% (95% confidence interval 1% to 24%)), but there were no differences between groups for withdrawals due to medical reasons (toxicity or disease progression). Overall, one in three patients did not complete chemotherapy (table 2).
Table 2.
Compliance with treatment by 87 patients with colorectal cancer assigned to chemotherapy at hospital outpatient clinic or at home. Values are numbers (percentages) unless stated otherwise
| Reason for non-compliance | Treatment
|
Difference in % (95% CI) | |
|---|---|---|---|
| Outpatient (n=42) | Home (n=45) | ||
| Voluntary withdrawal from treatment | 6 (14) | 1 (2) | 12 (0.6 to 24) |
| Withdrawal for other reasons* | 13 (31) | 11 (24) | 7 (−12 to 25) |
| Total | 19 (45) | 12 (27) | 18 (−1 to 38) |
Unacceptable toxicity (16 cases), disease progression (6), doctor's discretion (2).
Use of healthcare resources—The groups showed no significant differences in use of healthcare resource for unplanned visits (table 3).
Table 3.
Non-programmed use of healthcare resources by 56 patients with colorectal cancer assigned to chemotherapy at hospital outpatient clinic or at home. Values are mean (SD) number of visits during treatment unless stated otherwise
| Healthcare resource used | Treatment
|
Difference in means (95% CI) | |
|---|---|---|---|
| Day hospital | Home | ||
| Hospital admissions | 0 (1) | 0 (1) | 0 (0 to 0) |
| Other visits: | 9 (6) | 10 (9) | −1.0 (−4 to 2) |
| Emergency | 1 (1) | 1 (19) | 0.4 (0 to 1) |
| Ambulatory | 2 (2) | 2 (2) | 0.1 (−1 to 1) |
| Primary care | 6 (5) | 7 (8) | −1.0 (−4 to 2) |
Quality of life—There were no differences between groups in quality of life, neither at the initial assessment or once treatment was completed nor in terms of changes in scores during the trial (table 4). Insomnia was the commonest symptom, followed by fatigue, pain, and appetite loss. Role functioning improved after treatment in both groups, although changes in scores were not significant. Scores on the Karnofsky scale and global health status remained stable.
Table 4.
Quality of life reported by 87 patients with colorectal cancer assigned to chemotherapy at hospital outpatient clinic or at home. Values are means (SD) unless stated otherwise
| Item | Outpatient treatment
|
Home treatment
|
Difference in change in mean scores (95% CI) | |||
|---|---|---|---|---|---|---|
| Initial score (n=42) | Final score (n=23) | Initial score (n=45) | Final score (n=33) | |||
| EORTC QOL-C30 questionnaire* | ||||||
| Function: | ||||||
| Physical | 61 (26) | 67 (29) | 63 (24) | 68 (26) | −2 (−15 to 10) | |
| Role | 54 (41) | 3 (35) | 58 (37) | 81 (30) | 4 (−15 to 23) | |
| Emotional | 71 (24) | 79 (19) | 66 (23) | 76 (24) | 1 (−8 to 11) | |
| Cognitive | 89 (18) | 76 (29) | 87 (20) | 82 (21) | 7 (−2 to 17) | |
| Social | 82 (23) | 76 (23) | 83 (23) | 82 (19) | 5 (−6 to 17) | |
| Symptom: | ||||||
| Fatigue | 31 (28) | 30 (30) | 25 (21) | 29 (26) | 5 (−7 to 18) | |
| Nausea | 5 (15) | 7 (16) | 2 (8) | 6 (14) | 2 (−6 to 10) | |
| Pain | 21 (23) | 19 (25) | 22 (20) | 20 (24) | 1 (−10 to 12) | |
| Dyspnoea | 6 (15) | 7 (18) | 7 (16) | 11 (21) | 3 (−8 to 13) | |
| Insomnia | 39 (35) | 32 (38) | 35 (37) | 23 (32) | −4 (−22 to 14) | |
| Appetite loss | 28 (38) | 16 (33) | 21 (32) | 14 (27) | 7 (−13 to 28) | |
| Constipation | 15 (22) | 22 (30) | 10 (21) | 14 (23) | −2 (−15 to 10) | |
| Diarrhoea | 17 (28) | 17 (23) | 13 (23) | 16 (21) | 2 (−11 to 15) | |
| Financial difficulties | 8 (21) | 12 (24) | 5 (14) | 7 (21) | −1 (−12 to 10) | |
| General health status | 68 (20) | 68 (20) | 67 (20) | 71 (17) | 4 (−5 to 13) | |
| Karnofsky index† | ||||||
| Score | 84 (9) | 85 (11) | 83 (9) | 85 (11) | 0 (−5 to 6) | |
Scales range from 1 to 100, with higher scores representing better health (functional scales and global health status) or more problems (symptoms items).
Scale of performance status ranging from 1 to 100%, with higher scores representing better performance.
Satisfaction with health care—There were no differences between groups in scores on the initial satisfaction questionnaire (results not shown). However, when we assessed patients' satisfaction after completion of treatment we found a significant difference between groups in the perception of nursing availability, with the hospital outpatients considering that they had to wait longer to receive chemotherapy than the patients treated at home (table 5). Communication with nurses and the personal qualities of the nurses were also rated more highly by the home group. Global satisfaction with health care was higher in the home group, but the difference was not significant.
Table 5.
Satisfaction* with medical care reported by 56 patients with colorectal cancer after chemotherapy at hospital outpatient clinic or at home. Values are means (SD) unless stated otherwise
| Type of care | Treatment
|
Difference in means (95% CI) | |
|---|---|---|---|
| Outpatient (n=23) | Home (n=33) | ||
| Health care in general | 78 (19) | 86 (13) | −8 (−17 to 0) |
| Availability of doctor | 13 (17) | 13 (19) | 0 (−10 to 10) |
| Availability of nurse | 54 (16) | 87 (7) | −33 (−39 to −26) |
| Continuity of care | 51 (21) | 54 (23) | −3 (−16 to 9) |
| Personal qualities of nursing | 84 (15) | 98 (6) | −14 (−20 to −8) |
| Communication with nurse | 82 (25) | 100 (0) | −18 (−26 to −9) |
| Communication with doctor | 70 (26) | 70 (22) | 1 (−12 to 14) |
Satisfaction scales range from 1 to 100, with higher scores representing greater satisfaction.
Discussion
The results of this study indicate that home chemotherapy for patients with colorectal cancer is a safe and acceptable alternative to outpatient hospital treatment. All but one of the eligible patients we asked agreed to participate in the trial. No major complications occurred, showing that this type of chemotherapy can be safely administered outside hospital. From the point of view of implementation and impact on healthcare systems, it is worth noting that we found no differences between groups in use of non-programmed health resources, suggesting that home chemotherapy did not increase the use of other health services such as primary care or emergency departments.
Quality of care
There were no differences in quality of life or toxicity between the two groups, as was found in a recent study.9 In patients with advanced disease it has been found that quality of life could be affected by the psychological and social impact of the disease and its treatment, which can be more stressful in hospital.16 Patients receiving chemotherapy at home reported higher levels of satisfaction with care, which was largely due to higher levels of satisfaction with the nursing staff. Home care probably allowed the nurses to establish a better relationship with patients. With home treatment, nurses are able to devote time exclusively to the patient, thereby leading to improved perceptions of nurses' personal qualities and availability.
The issue of compliance has not received much attention in oncology.17,18 A review of non-compliance with drugs administered by a provider, as in our study, found rates of non-compliance ranging from 16% to 33%.19 In total, 8% of our patients voluntarily withdrew from treatment. Obviously, the drug provider may play an important role in reducing non-compliance, and of our 8% of patients who did not comply with treatment, the proportion in the home group was only 2%. This difference might have been because withdrawal from treatment and reduced appointment keeping are due more to the interference of adverse effects on daily activities than to the adverse effects themselves.20 This type of interference is probably easier to manage when treatment is administered at home.
Study limitations
Our study was limited to a specific treatment for colorectal cancer. This treatment was common at the time our study was planned, but the results may not apply to newer or more complicated chemotherapy regimens. However, our results would probably be applicable to other tumours and some chemotherapy programmes.
We did not perform a detailed cost analysis because the study was planned under a hospital perspective in a context of increasing demand for cancer treatments, where it was fairly obvious that a home programme would require additional resources. However, home chemotherapy could be an economically realistic alternative to hospital treatment if we consider indirect benefits to patients.21
Conclusions
This study is one of the first trials in chemotherapy to evaluate the impact of organisational change on a variety of outcomes. It is surprising that, while considerable effort is devoted to assessing the benefits and risks of drugs, much less attention is paid to understanding how the mode of administration affects important outcomes such as use of health services or satisfaction with care. A recent review of the effect of home care programmes on the quality of life of patients with incurable cancer and on use of hospital resources concluded that the effectiveness of such programmes remains unclear and that research is needed before such programmes are expanded.22 Our study contributes to the assessment of home care for cancer patients and has shown that home chemotherapy could be advantageous for patients by increasing satisfaction and compliance with treatment.
Figure.
Progress of participants through trial
Acknowledgments
We thank the EORTC for permission given to use the EORTC QOL-C30 quality of life questionnaire. We thank C Fernandez, M Garcia, X Puig, and V Moreno for helping to make this study possible, and M Herdman for his revision of the English version of this manuscript. Preliminary results of this study were presented at the seventh meeting of the Spanish Society of Medical Oncology and at the sixth annual meeting of the International Society for Quality of Life Research.
Footnotes
Funding: Research grant from the Catalan Agency for Technology Assessment in Health Care (contract 1996/273).
Competing interests: None declared.
References
- 1.Benjamin AE. An historical perspective on home care policy. Milbank Q. 1993;71:129–166. [PubMed] [Google Scholar]
- 2.Sodestrom L, Tonsignant P, Kaufman T. The health and costs effects of substituting home care for inpatient acute care: a review of the evidence. Can Med Assoc J. 1999;160:1151–1155. [PMC free article] [PubMed] [Google Scholar]
- 3.Shepperd S, Illife S Cochrane Collaboration, editors. Cochrane Library. Issue 3. Oxford: Update Software; 1998. Effectiveness of hospital at home compared with intrahospital care. [Google Scholar]
- 4.Pfister DG. Oncology and high-tech home care. In: Arras J, editor. Bringing hospital to home. Baltimore: Johns Hopkins University Press; 1996. pp. 65–78. [Google Scholar]
- 5.Marks L. Home and hospital care: redrawing the boundaries. London: King's Fund; 1992. [Google Scholar]
- 6.Close P, Burkey E, Kazak A, Danz P, Lange B. A prospective controlled evaluation of home chemotherapy for children with cancer. Pediatrics. 1995;95:896–900. [PubMed] [Google Scholar]
- 7.Mor V, Stalker MZ, Gralla R, Scher HI, Cimma C, Park D, et al. Day hospital as an alternative to inpatient care for cancer patients: a random assignment trial. J Clin Epidemiol. 1988;41:771–785. doi: 10.1016/0895-4356(88)90164-3. [DOI] [PubMed] [Google Scholar]
- 8.Rischin D, White MA, Matthews JP, Toner GC, Watty K, Sulkowski AJ, et al. A randomised crossover trial of chemotherapy in the home: patient preferences and cost analysis. Med J Aust. 2000;173:125–127. [PubMed] [Google Scholar]
- 9.King MT, Hall J, Caleo S, Gurney HP, Harnet PR. Home or hospital? An evaluation of the costs, preferences and outcomes of domiciliary chemotherapy. Int J Health Serv. 2000;30:557–579. doi: 10.2190/CY03-EV15-K38Y-X4AA. [DOI] [PubMed] [Google Scholar]
- 10.WHO handbook for reporting results of cancer treatment. Neoplasma. 1980;20:37–46. [Google Scholar]
- 11.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The EORTC QOL-C30: a quality of life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 12.Karnofsky DA, Buchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: Mackad CM, editor. Evaluation of chemotherapeutic agents. New York: Columbia University Press; 1949. [Google Scholar]
- 13.McCusker J. Development of scales to measure satisfaction and preferences regarding long-term and terminal care. Med Care. 1984;22:476–493. doi: 10.1097/00005650-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Cronbach LJ. Coefficient alpha and the internal structure of the tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 15.Nunally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- 16.Payne SA. A study of quality of life in cancer patients receiving palliative chemotherapy. Soc Sci Med. 1992;35:1505–1509. doi: 10.1016/0277-9536(92)90053-s. [DOI] [PubMed] [Google Scholar]
- 17.Lewis C, Linet MS, Abeloff MD. Compliance with cancer therapy by patients and physicians. Am J Med. 1983;74:673–678. doi: 10.1016/0002-9343(83)91026-4. [DOI] [PubMed] [Google Scholar]
- 18.Green JA. Compliance and cancer chemotherapy. BMJ. 1983;287:778–779. doi: 10.1136/bmj.287.6395.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barofsky I. Therapeutic compliance and the cancer patient. Health Educ Q. 1984;10(suppl):43–56. [PubMed] [Google Scholar]
- 20.Richardson JL, Martis G, Levine A. The influence of symptoms of disease and side effects of treatment on compliance with cancer therapy. J Clin Oncol. 1988;6:1746–1752. doi: 10.1200/JCO.1988.6.11.1746. [DOI] [PubMed] [Google Scholar]
- 21.Lowenthal RM, Piaszczyk A, Arthur GE, O'Malley S. Home chemotherapy for cancer patients: a cost analysis and safety. BMJ. 1999;319:1547–1550. doi: 10.5694/j.1326-5377.1996.tb124921.x. [DOI] [PubMed] [Google Scholar]
- 22.Smeenk F, van Haastregt J, de Witte LP, Crebolder H. Effectiveness of home care programmes for patients with incurable cancer on their quality of life and time spent in hospital: systematic review. BMJ. 1998;316:1939–1944. doi: 10.1136/bmj.316.7149.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]