Abstract
Vaginal microbiome studies provide information which may change the way we define vaginal flora. Normal flora appears dominated by one or two species of Lactobacillus. Significant numbers of healthy women lack appreciable numbers of vaginal lactobacilli. Bacterial vaginosis (BV) is not a single entity, but different bacterial communities or profiles of greater microbial diversity than is evident from cultivation-dependent studies. BV should be considered a syndrome of variable composition which results in different symptoms, phenotypical outcomes, and responses to different antibiotic regimens. This information may help to elucidate the link between BV and infection-related adverse outcomes of pregnancy.
INTRODUCTION
In normal pregnancy, the resident vaginal microbial flora is thought to provide protection against infection by a number of different mechanisms.1 In non-pregnant women, the presence of bacterial vaginosis (BV) is associated with an increased risk of upper genital tract and sexually transmitted infections2-4 and acquisition of HIV.5-9 In pregnancy, BV increases the risk of post-abortal sepsis,10 early miscarriage11 recurrent abortion,12 late miscarriage,12;13 preterm prelabor rupture of membranes (PPROM),14 spontaneous preterm labor (SPTL) and preterm birth (PTB),13;15-26 histological chorioamnionitis27;28 and postpartum endometritis.29;30 As a result, abnormal vaginal flora may predispose to ascending colonization of the genital tract, infiltration of the fetal membranes, microbial invasion of the amniotic cavity31 and fetal damage.32;33 Preterm birth of infectious etiology is associated with high perinatal mortality and morbidity,34-36 and a high cost to the healthcare system.37-39 Much of our knowledge about the composition of the vaginal microbial flora comes from qualitative and semi-quantitative descriptive studies using cultivation-dependant techniques.40-44 In recent years, the development and introduction of cultivation-independent molecular-based techniques have provided new information about the composition of normal vaginal flora as well as abnormal colonization of the genital tract which complements existing knowledge from cultivation-dependent techniques. This review seeks to inform the busy obstetrician about the background to these new developments and what additional information they provide. These new data might help to elucidate the composition and function of normal flora, and appreciate the microbial diversity, diagnosis, and treatment assessment of abnormal genital tract flora which may affect the outcome of pregnancy.
THE HUMAN MICROBIOME PROJECT
During the conduct of the human genome project, scientists estimated that the number of genes in the human genome that would be needed to code for the proteins required to sustain human physiology, would be approximately 100,000. The researchers were somewhat humbled to find only 20,000 protein coding genes, similar to that of the fruit fly. However, if one considers the human to be a super-organism, (the sum of all human genes plus those of the micro-organisms in, or on us), then the human genome plus the microbial genome [microbiome] which amounts to the collective genome of the symbionts may be considerably more than 100,000 genes. This is supported by the fact that the human microbiome provides traits which the human organism has not needed to evolve for itself.45;46 The NIH in its roadmap for medical research has committed $100,000,000 to the Human Microbiome Project and plans to investigate five sites – the oral and nasal cavities, the gastrointestinal and genito-urinary tracts and the skin. The genital tract microbiome will be studied in health and disease and whether the function of the microbiome (metagenome) can be manipulated to influence physiology and treat disease. The core microbiome, as well as the variable microbiome (influenced inter alia by host lifestyle, genotype, immune response, environment, pathophysiology and transient community members) will be assessed spatially and temporally,47 and different sub-sites will be assessed. The microbial flora on the labial surface of the teeth are different from those on the lingual surface,48 and the lower vagina, upper vagina and cervix also differ in their microbial flora.49 How this relates to the various niches in the female genital tract in pregnancy and to the human microbiome project as a whole is indicated in Figure 1.
Figure 1.
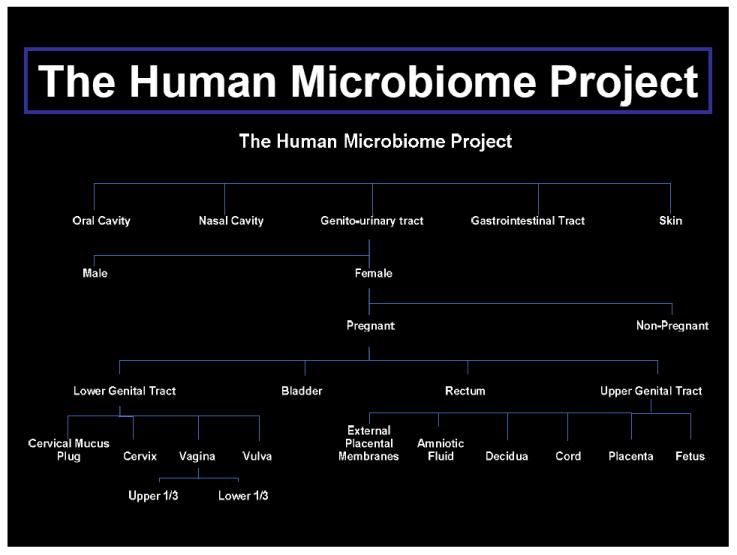
The Human Microbiome Project
MICROBIAL TAXONOMY
Cultivation-independent techniques require us to be aware of different levels of taxonomic classification. Taxonomy is the classification of living organisms into phylogenetic groups. Phylogenetic classifications arrange organisms into groups which reflect genetic similarity and evolutionary relatedness. A taxon is a group, or level of classification, and is hierarchical, whereby broad divisions are divided up into smaller divisions such as Domains, Kingdoms, Phyla, Classes, Orders, Families, Genera, and Species. Not every level is used in every discipline. The species is the basic unit of taxonomy and many molecular based studies use different terms such as “operational taxonomic units”, “taxons/taxa” or “phylotypes” instead of species, because the level of molecular diversity far outstrips that defined by existing microbiological or biochemical means. The human intestine demonstrates the greatest degree of diversity with over 400 phylotypes only 20% of which are cultivatable.50
MOLECULAR BASED TECHNIQUES
Many of the culture-independent studies focus on the detection of novel, previously uncultivated species51-56 or are more concerned with the novel molecular techniques in themselves rather than for the microbiological information they provide.57-60 In addition, theoretical and mathematical models have arisen which address new concepts such as “functional redundancy,” “structural diversity,” “interspecies interaction,” “mutualism,” “cheating,” “the insurance hypothesis,” “drivers” and “passengers”.61-64
Bacterial DNA is extracted from samples, and is amplified using the polymerase chain reaction (PCR) using either universal or specific primers. This is not infallible because PCR inhibitors may be present at varying levels in individual clinical samples, and primers may preferentially amplify certain nucleic acids, and may not complement the entire bacterial kingdom.65
The commonest target for molecular identification of bacteria is the small ribosomal subunit of the 16S rRNA gene. The 16S rRNA gene is useful because it is present in all bacteria and has regions of conserved sequence which can be targeted by universal (sometimes referred to as bacterial-domain or broad-range primers) or specific primers, yet also has areas of heterogeneity which can be used to identify bacteria or to infer phylogenetic relationships.66-71 If there is uncertainty with respect to which organisms might be present in a sample or if a broad diversity of organisms are anticipated, then many researchers will use universal primers.53 If, on the other hand, an investigator knows what organisms to expect, or wishes to test for specific organisms then specific primers will be used.72 Once the 16S rRNA gene has been sequenced, the variable regions can be used for species specific PCR in a qualitative or quantitative manner. The sequences obtained are aligned and compared with large databases of 16S rRNA sequences, although diversity for vaginal microbial flora is poorly represented in these databases compared to other sites like the gastro-intestinal tract.54;60
Cultivation-based studies have the disadvantage that they may fail to isolate or detect large numbers of fastidious micro-organisms, or identification tests may not be available. An unknown number of species which are identified purely by molecular methods are cultifiable, but have not been identified by cultivation methods because of a lack of phenotypic tools for the species, their lower relative titers, or inappropriate media (REF: Rabe LK, Antonio M, Austin MA, Stoner K, Pollard R, Petrina M, Leyland B, Chaiworapongsa T, Lamont RF, Hassan S, Romero R, and Hillier S. A 21st Century Description of the Vaginal Microflora of Pregnant Women. Proceedings of the Annual Meeting of the Infectious Diseases Society for Obstetrics and Gynecology, Santa Fe, New Mexico, USA, Aug 6th 2010.
This is an important distinction, since it shifts the focus of new research from developing novel culture media to using molecular tools to identify the under-characterized colonies that already grow in current formulations. This also restricts the development of their phenotypic profiles and hence the understanding of their roles in the whole population. In addition, this suggests that before the development of molecular techniques, culture-based assessments of the vaginal microbiome did not “miss” 80% of the species, but simply had no labels to impose on many colonies. As a result these organisms were included only as members belonging to a broad phenotypic or phylogenetic branch.
Cultivation-independent techniques may show greater diversity by overcoming cultivation problems with and identification of fastidious organisms, but are limited by their tendency to sample only the most prevalent bacteria in a community, such that low abundance or minority species are likely to be missed.73 Since PCR amplification of DNA is a competitive enzymatic reaction, the 16S rRNA templates in a sample are amplified in accordance with their abundance. As a result, the 16S rRNA genes of the numerically dominant population will be the most abundant amplicons following PCR. Populations that constitute <1% of the total community (yet may still be present in >106/g of vaginal fluid) may not be represented in such profiles, so this represents the threshold of detection. This being the case, despite their limitations, cultivation studies remain an important part of vaginal microbiology and will need to be used in combination with cultivation-independent techniques.74 The development of the next generation of ultra-high throughput sequencing technologies (pyrosequencing) may remove an important quantitative barrier by increasing the number of reads from a gene or genome by many orders of magnitude in one experimental run.75 The power of next generation sequencing, however, is not without limitations. Until recently, error rates using pyrosequencing were high enough to generate reading errors that generated false microdiversity at the species or subspecies levels. However, improvements in the technology in 3rd generation systems now produces sequencing with error rates similar to Sanger sequencing, which should minimize this is future experiments. Even this improvement does not overcome the best read lengths among these, (~ 350-400 bases). The variable domains of 16S rDNA, which allow best species discrimination, are spread out over >1kb, so only some can be captured in this run length. This limits discrimination to the genus level for some phylogenetic branches with minimal diversity at this locus.76 This obstacle remains a stumbling block for most of the next generation sequencing methods, less so as read lengths are steadily improving via technical advancements. For an insight into the pros and cons of the various techniques and their limitations the reader is directed to three excellent reviews.77-79
NORMAL VAGINAL FLORA
Most studies, whether cultivation-dependent or independent, give the impression that the vaginal microbial flora is static, because most studies are carried out as a “snap-shot” in time and do not consider that vaginal microbial communities undergo shifts in their representation, abundance and virulence over time, and are affected by many factors.
Identification of Lactobacilli to the Species Level Using Molecular-based Techniques
Culture and microscopy of “normal” vaginal flora typically shows a predominance of Lactobacillus species which are believed to promote a healthy vaginal milieu by providing numerical dominance but also by producing lactic acid to maintain an acid environment that is inhospitable to many bacteria and is negatively correlated with BV.80 Lactobacilli also produce hydrogen peroxide (H2O2),81 antibiotic toxic hydroxyl radicals, bacteriocins,82 and probiotics.83 Prior to molecular-based techniques, lactobacilli were generally identified only to the genus level.
In 1892, Professor Albert Döderlein (1860-1941) published his definitive monograph in which he recorded that cultured organisms were a source of lactic acid which could inhibit the growth of pathogens in vitro and in vivo.84 In 1928, Stanley Thomas identified Doderlein’s bacillus as Lactobacillus acidophilus, adding prophetically, that this was either a characteristic group of related species, or a species which underwent a remarkable transformation.85 In 1980, in keeping with the observation of Thomas, a group of organisms previously collectively known as L .acidophilus was shown to be highly heterogeneous.86 As a result, the group was divided into DNA homologous groups that could not be distinguished biochemically,87 to form a number of separate species within the L. acidophilus complex (Table 1).88-90 The closely related species within the L. acidophilus complex are difficult to differentiate by phenotypic methods which may account for the variation in species of lactobacilli found in different studies.91-93
Table 1.
Obligately Homofermentative Species Within the Lactobacillus acidophilus Complex.
|
Cultivation-based techniques, because they fail to detect fastidious organisms, underestimate the diversity of vaginal microbial flora, but because of deficiencies in the phenotypic identification of lactobacilli they overestimate the diversity of Lactobacillus species in the vagina.94
Some 20 years ago, using cultivation-based phenotypic techniques, Redondo-Lopez et al concluded that no two women were colonized by the same two Lactobacillus species.92 Using cultivation-independent techniques this would appear now not to be the case and because of their significant role in health and disease, there has been much attention to the identification of lactobacilli using genotypic means.51;65;91;95-98
Lactobacillus iners: under-detected and under-appreciated
The existence of Lactobacillus iners was unknown prior to 1999 but is now known to play a significant role in vaginal microbial flora. Selective media such as Rogosa or MSR agar are normally used to culture lactobacilli, so the use of cultivation-based techniques, even those followed by molecular methods, will not detect L. iners because it only grows on blood agar.90 Hence, some very important molecular based studies failed to isolate L. iners because Rogosa or MRS agar were used rather than blood agar.51;95;99-101
The first report of isolation of L. iners in a woman with a normal Nugent score was in 2002.65 Cultivation-independent methods have identified L. iners, a lactic acid producing bacterium, as one of the organisms most frequently isolated from the vagina of healthy women.62;65;97;98;102-104 In contrast to L. crispatus, which is rarely dominant in BV,53 L. iners can be detected at high levels in most subjects with and without BV,53;65;105;106 and in three studies it was the only Lactobacillus species detected in BV positive women.52;53;105 It has been postulated that this may be because L. iners may be better adapted to the conditions associated with BV, i.e. the polymicrobial state of the vaginal flora and elevated pH.105 Alternatively, the observations could result from relative resistance of L. iners to unknown factors that lead to the demise of other Lactobacillus species during the onset of BV, or to a relative lack of antagonism of L. iners to the BV-associated anaerobes, so that their dominance predisposes the individual to acquiring BV.
Numerical Supremacy of Lactobacilli
Over 120 species of Lactobacillus have been identified, and more than 20 species have been detected in the vagina. Using molecular-based techniques, we now know that healthy vaginal microflora does not contain high numbers of many different species of Lactobacillus. Rather, one or two lactobacilli from a range of three or four species (mainly L.crispatus and L. iners but also L. jensenii and L. gasseri) are dominant, whereas other species are rare, lower in titer, and tend to be novel phylotypes.51;52;55;62;65;97;100;101;103;106-109
In healthy Swedish women with a normal Nugent score,110 202 vaginal isolates were tested against 26 type and reference strains of Lactobacillus. 97 In 18/23 women, the vaginal flora was dominated by a single species of Lactobacillus and only five women had two different species or two different strains of the same species of Lactobacillus. The only species detected were L. cripsatus, L. gasseri, L. iners, and L. jensenii. 97 In a follow up study only one women was colonized by more than two Lactobacillus species, four were colonized by two different species and 17 were colonized by one single species.98 Although this study was severely limited by the small number of colonies examined per patient (10 from blood, 100 from Rogosa agar), the exclusion of other species is in keeping with the theory of “competitive exclusion”55 and the superior ability of L. iners and L. crispatus to compete with other bacteria for vaginal resources, a survival strategy known as “bacterial interference”.111 Alternatively, the rare co-existence of multiple dominant species of Lactobacillus could be due to pre-emptive colonization by a particular species, or due to host factors that strongly influence which species are able to colonize the environment.
Cultivation-independent studies using molecular techniques have been published on different populations such as adolescent girls,55 post menopausal women65;112 and women from Belgium,52;107;109 Brazil,113 Bulgaria,94 Canada,57;65;112 China,108 Germany,106 Holland,114 India,115 Italy,99 Japan,100;116 Nigeria,102;117 Sweden,97;98 both Turkey and the USA,118 the USA,54;55;58;62;95;103 African-American women,105 Caucasian and black North American women103 and a multinational group of women from seven different countries.51
Racial variation and geographical area are important51 and different racial groups within the same geographical region have significant differences in what is the dominant vaginal organism.103 In most populations, L. crispatus is the commonest dominant isolate,51-53;58;62;97;103;104 and white women are more likely to be dominated by L. crispatus and/or L. jensenii than any other species of Lactobacillus. 95 A number of genetic as well as environmental factors might explain at least in part this observation. Alternatively,diet might influence the Lactobacillus species resident in the gastro-intestinal tract and hence the vagina since the lactobacilli of the gut varies between Japanese and Western subjects.119-121
Production of H2O2 by Lactobacilli and the Association with Bacterial Vaginosis
Lactobacilli differ in their ability to produce H2O2 and a reduction in the prevalence and concentration of H2O2 producing bacteria is associated with the development of BV and vaginal infections.81;122 With the introduction of molecular based techniques, it is now possible to relate the production of H2O2 to individual species or strains of the same species of Lactobacillus rather than the genus as a whole. Three studies using molecular based techniques have addressed the production of H2O2 by lactobacilli.95;100;101 In Japanese women who did not have BV, L.crispatus and L. gasseri were found in the vagina of 52.7% and 20.8% of women respectively. L. jensenii was not detected, All strains of L. crispatus were strongly positive for H2O2, whereas 41% and 59% of L. gasseri strains were strongly and weakly positive for H2O2 respectively.100
Antonio et al (1999) demonstrated that Lactobacillus species detected among 302 women with and without BV differed in their ability to produce H2O2. L. crispatus and L. jensenii were found to colonize 32% and 23 % of women respectively and 95% and 94% of their strains, respectively, were shown to produce H2O2. In contrast, L. gasseri and L. iners colonized 5% and 15% of women respectively and only 71% and 9% of their strains respectively produced H2O2. Not surprisingly, BV was present in 9% and 7% of women colonized by L. crispatus and L. jensenii respectively, and in 43% and 36% of women colonized by L. gasseri and L. iners respectively. Of the women without BV by Nugent score,110 16% had no lactobacilli present, and none of the women colonized by L. crispatus and L. jensenii had BV; however, the latter argument is circular, since the Lactobacillus morphotype is part of the Nugent score. The association between L. gasseri and BV has been confirmed in a study of homosexual women. Detection of L. gasseri was associated with a 4.2 fold increased risk of BV,123 and attributed to a higher rectal colonization by L. gasseri and sexual practices which increase the risk of vaginal colonization from the rectum.124
Using culture-based techniques Eschenbach et al122 and McGroarty et al125 found that 100% of L. jensenii produced H2O2, yet Nagy et al126 found only 46%. Similarly, with L. acidophilus the range of species which produced H2O2 varied from 43% to 77%.122;125;126 This may have been due to the inability of biochemical assays to differentiate between the species belonging to the L. acidophilus complex. However, this led Nagy et al to conclude, that the ability of lactobacilli to produce H2O2 was associated with the origin of strain (whether from women with or without BV) rather than the Lactobacillus strain itself.126 In light of the findings of molecular-based techniques, and the current ability to identify H2O2 producing lactobacilli to the species level,95 we might alternatively conclude that it is whether or not the strain/species of Lactobacillus produces H2O2 that dictates whether BV is present or absent. However, given that H2O2-producing L. gasseri are found in BV patients, albeit at lower incidence, one might also argue that in vitro production of H2O2 is only a biomarker of a protective species of Lactobacillus, not an active factor in limiting the growth of vaginal anaerobes. Indeed, it is not clear whether bacterial H2O2 production is active in the microaerobic to anaerobic vaginal flora. Other factors may include the extent to which a species can dominate numerically over its competitors, e.g. 95% versus 99.99%.
Healthy vaginal flora not dominated by lactobacilli
Using culture-independent techniques several investigators have demonstrated that a significant proportion (7-33%) of healthy women lack appreciable numbers of Lactobacillus species in the vagina52;58;62;102;103 which may be replaced by other lactic acid producing bacteria such as Atopobium vaginae, Megasphaera and Leptotrichia species.62;103 Although the structure of the communities may differ between populations, health can be maintained provided the function of these communities i.e. the production of lactic acid, continues.55;62 Consequently, the absence of lactobacilli or the presence of certain organisms such as G.vaginalis, or species of Peptostreptococcus, Prevotella, Pseudomonas, and/or Streptococcus, does not constitute an abnormal state.58 This issue is still unclear, however, because the studies do not address whether some proportion of “healthy” women are patients in transition to or from BV, or whether they have asymptomatic BV, ie. abnormal flora but no symptoms due to genetic or other factors. Indeed, a recent molecular study further confuses the issue by pointing out that G. vaginalis may produce transient dominance in healthy women as a result of perturbations such as increase in pH, during menstruation.127
Vaginal Probiotic Lactobacilli
The first example of vaginal probiotics use we could detect was that of Stanley Thomas in 1928 following his observation that Lactobacilli were absent in the presence of gonococci. He reported on two experiments, one in-vitro and the other in vivo in which addition of a thin layer of whey broth from a culture of L. acidophilus demonstrated eradication of Neisseria gonorrhoeae.85
Exogenous strains of Lactobacilli have been suggested as a means of establishing or re-establishing normal vaginal flora. L. fermentum and L. rhamnosi probiotic strains have been used with poor results in urogenital infection and this may be because they are not normally prevalent in the vagina.104;128;129 In contrast, L. crispatus might be a better choice because it is commonly found to be numerically dominant in the healthy vagina and 95% of the strains produce H2O2.95 L. crispatus may have a superior capacity to persist in the vagina130 and strains of probiotic L.crispatus CTV-05 have been demonstrated to have high mean adherence to vaginal epithelial cells in vitro 131 and established vaginal colonization in 7 of 9 women when administered vaginally.132 Combined vaginal and rectal colonization by H2O2 producing Lactobacilli is associated with a four-fold decrease in the incidence of BV.131
Using molecular based techniques in a double blind, randomized, single centre study of 90 non-pregnant, sexually active women, who were free from genital infection, and had a normal Nugent score, the ability of the probiotic L. crispatus CTV-05 to establish vaginal colonization was studied.133 The study demonstrated that L. crispatus CTV-05 established vaginal colonization at one or more follow-up visits in 69% of women overall and 90% of those not already colonized with L. crispatus. Of women who were never colonized with L. crispatus CTV-05, 85% were already colonized by endogenous L. crispatus at enrollment. The authors saw this as self regulatory rather than a shortcoming of the probiotic, and the dosage regimen did not result in overgrowth of Lactobacilli since there seemed to be a physiological adjustment to around 106 or 108 cfu/mL of vaginal fluid. They also recommended that future research should concentrate on Lactobacilli which are prevalent in the vagina133 rather than species such as L. fermentum and L. rhamnosus.
ABNORMAL VAGINAL FLORA
Abnormal vaginal flora may occur because of a sexually transmitted infection (STI) eg trichononiasis, colonization by an organism which is not part of the normal vaginal community e.g. Streptococcus pneumoniae, Haemophilus influenzae, or Listeria monocytogenes, or by overgrowth or increased virulence of an organism that is a constituent part of normal vaginal flora e.g. Escherichia coli. Alterations in vaginal flora do not necessarily imply disease or result in symptoms. Disease results from interplay between microbial virulence, numerical dominance, and the innate and adaptive immune response of the host.134 The most common disorder of vaginal flora is BV. BV is a polymicrobial condition, characterized by a decrease in the quality or quantity of Lactobacilli and a one thousand-fold increase in the number of other organismsas determined by cultivation-dependent techniques, particularly anaerobes Mycoplasma hominis, Gardnerella vaginalis and Mobiluncus species. The prevalence of BV in pregnancy in the USA is 1,080,000 cases annually.135 In pregnancy, BV has been associated with early,11 and late miscarriage,12;136 recurrent abortion,12 post abortal sepsis,10 post partum endometritis,30 and preterm birth.12;21;136-138
BV and HIV
BV is also associated with acquisition of HIV.5-9 Healthy lactic acid producing vaginal flora acts as a barrier against acquisition of HIV139;140 and is negatively correlated with BV80 which acts as a co-factor for HIV and conversion to seropositivity.5-9 HIV infected women with BV have higher levels of HIV viral load in genital secretions than do HIV infected women without BV.6;141;142 BV is also associated with increased susceptibility to other STIs including herpes simplex virus -2, gonorrhoea, Trichomonas vaginalis and Chlamydia trachomatis.141;143-145 Molecular based studies suggest a trend towards increased diversity in the microbiome of HIV positive women with BV compared to those HIV positive women who do not have BV suggesting that HIV infection per se is associated with changes in the diversity of genital microbiota.146
Individual bacteria as a cause of BV
Many of the models necessary to demonstrate that bacteria function as mono-etiological agents require a change in the micro-environment before an infectious event is observed. Infective peritonitis is easier to induce in experimental animals if blood is instilled into the peritoneal cavity, experimental gangrene develops better if calcium chloride is implanted into muscle along with Clostridium species, and rodents will not develop vaginal candidiasis without the addition of estrogen.42 In the definitive paper of Gardner and Dukes (1955), the instillation of pure cultures Haemophilus vaginalis (now known as Gardnerella vaginalis) only successfully induced vaginal colonization in one of 13 volunteers.147 In contrast, 11 of 15 volunteers were successfully inoculated when the vaginal secretions of donors (screened for other genital tract infections) were instilled into the vagina. This supports the later view of others, that since vaginal secretions from donors were much more successful at causing disease than pure cultures, G. vaginalis probably acts synergistically with other organisms to cause BV.148
Atopobium vaginae: under-detected and under-appreciated
The genus Atopobium lies within the family Coriobacteriaceae and forms a distinct branch within the phylum Actinomycetes.149 Following sequence analysis, three species formally designated Lactobacillus minutus,150 Lactobacillus rimae,151 and Streptococcus parvulus152 within the lactic acid producing group of bacteria,153 have been reclassified as genus Atopobium. In 1999, an organism similar but not identical to these three species was isolated from the vagina of a healthy woman in Sweden and the organism was named Atopobium vaginae.154 Since that time, using molecular-based techniques, A. vaginae has frequently been detected in the vagina and is found much more commonly in women with BV than in those with normal flora.52-55;59;62;72;103;105-107;109;112;113;155-160 In addition to producing lactic acid,161;162 some species of Atopobium have peptidyl peptidase activity and produce significant amounts of ammonia in other environments163-165 where sugars are a scarce source of energy. This may be why A. vaginae is found more often in the vagina of postmenopausal women, not on hormone replacement therapy (HRT) compared to those who are taking HRT.112 Prevotella bivia (formerly Bacteroides bivia) also produces ammonia which is known to act as a substrate to promote the growth of G. vaginalis.166 A. vaginae is strictly anaerobic and in-vitro is very sensitive to clindamycin157 but highly resistant to nitro-imidazoles such as metronidazole157 and secnidazole.156
High Diversity of flora in BV compared to normal flora
Using various molecular-based techniques and usually Amsel clinical criteria167 or Nugent score110 to classify normal or abnormal flora, a number of studies have demonstrated a high diversity of organisms in women with BV compared to women with normal flora. Collectively, these studies demonstrate the presence of novel bacterial species previously unidentified using cultivation-dependent techniques.51-56 They have also demonstrated that many of these organisms have specificity for BV and that the number of phylotypes found in association with BV is statistically significantly greater than the number detected in the presence of intermediate flora (a distinct entity in its own right)168;169 or normal flora.49;52-54;56;65;105-107;109;157 This statistic is largely due to the extreme dominance of lactobacilli in healthy women, which makes detection of other species unlikely, even when they are present 100,000 or more cells per sample.
Many of these organisms will be unfamiliar to clinicians (Table 2) though for many of them, there is evidence of disease association. The renamed Atopobium parvulum, Atopobium minitum and Atopobium rimae have been associated with dental abscesses and oral infections,151;162;165;170;171 tubo-ovarian abscesses,172 and abdominal wound infection, supporting the view that these organisms may be pathogenic to the host. Leptotrichia sanguinegens/amnionii has been reported in association with post-partum endometritis, adnexal masses and fetal death,173-175 and has been detected in the amniotic fluid of women with PTL, PPROM and preeclampsia.176-178 Also, in a study of 45 women with salpingitis and 44 controls (women seeking tubal ligation), bacterial 16S rRNA sequences were found in the fallopian tube specimens of 24% of cases and in no controls. Bacteria phylotypes closely related to Leptotrichia species and A.vaginae were among those identified in cases.179 In addition, Dialister pneumosintes was found as the sole agent in blood culture from a women with suppurative postpartum ovarian thrombosis.180
Table 2.
Previously unfamiliar vaginal organisms identified by molecular based techniques
|
A bacterium distantly related to Eggerthella hongkongensis (92% sequence similarity)
In summary, these studies have demonstrated that different subjects with BV have different microbial profiles indicating heterogeneity in the composition of bacterial taxa in women with BV. Women without BV had bacterial communities dominated by Lactobacillus species accounting for 86% of all sequences. In contrast, women with BV did not possess a single dominant phylotype but contained a diverse array of vaginal bacteria, often at relative low abundance.
Molecular-based tools for diagnosis of BV
BV can be diagnosed clinically, or using composite clinical criteria,167 microscopically,110;181-186 enzymatically,187-190 chromatographically191;192 or using qualitative or semi-quantative culture methods.19 Currently, the gold standard is Nugent score110 but the number of methods testifies to the fact that no single test is ideal and that they can all provide false positive and false negative results. Findings from molecular-based studies are now highlighting possible explanations for why diagnosis by microscopy may be inconsistent and why molecular methods may replace them.
One of the three organisms quantified as part of the Nugent score is Mobiluncus. Several cloning and sequencing studies have identified Mobiluncus only rarely.53;58;106 Fluorescence in situ hybridization (FISH) technology has demonstrated that BV associated bacterium (BVAB)-1 has a curved rod morphology,53 similar to Mobiluncus morphotypes, and it is possible that with microscopic examination of vaginal smears, Mobiluncus species may have been overrepresented and mistaken for BVAB-1.62;193 Alternatively, since species specific PCR agrees with the Nugent score Mobiluncus may be missed in universal PCR studies because it frequently falls below a threshold titre where it can be detected.78
Zhou et al (2004) observed that the urea produced by Atopobium species was associated with halitosis,164 and that similar species of Megasphaera caused beer spoilage by turbidity, off-flavors and off-colors.194;195 They concluded that if two genera associated with malodorous metabolites can be found in the vagina of healthy women, and amines can be found in women without BV, then diagnostic techniques to diagnose BV, based on upon amine production and odor formation167;189;192 may need to be amended.62
Microscopically, Atopobium species are gram positive, elliptical cocci or rod-shaped organisms that occur, singly, in pairs or short chains. The variable cell morphology of Atopobium renders it well camouflaged among the mixture of other species present in bacterial communities where the Nugent score is ≥4. A. vaginae is fastidious, grows anaerobically and forms small pin-head colonies on culture that are easily missed.154 Although phylogenetically different from other lactic acid producing bacteria, they are not phenotypically exceptional and it is not difficult to see why the significance of this organism based on culture, microscopy and phenotype may be overlooked and under-appreciated.
Using species specific primers, the relationship between five fastidious organisms associated with BV, were compared with BV diagnosed by Amsel and/or Nugent scores, and also with the individual clinical criteria of Amsel.196 The two biovars of Ureaplasma urealyticum (U. parvum and U. urealyticum – biovar 2) were associated with vaginal discharge and raised pH, but not with BV by either Amsel or Nugent criteria or any of the individual Amsel clinical criteria. In contrast, with Leptotrichia sanguinegens/amnionii, A.vaginae and BVAB-1, elevated pH > 4.5 was a universal feature and they were all associated with BV by both Amsel and Nugent criteria, and with the finding of >20% of epithelial cells as clue cells, a feature already reported.53 A positive test for amine odor on addition of 10% solution of potassium hydroxide was significantly more likely in women testing positive for BVAB-1. Douching is a recognized risk factor for BV197 and the detection of Leptotrichia and A. vaginae was three times more likely and BVAB-1 twice as likely when women reported douching.196
Fredricks et al, in two linked studies noted that some organisms or combination of organisms had high sensitivities or specificities for the diagnosis of BV using Amsel criteria53;72 and Nugent score.53 (Table3).Using quantitative real time PCR, Menard et al firstly examined qualitatively the association of individual organisms with BV diagnosed by Nugent score. To optimize the molecular methods for routine practice, an adjusted quantification was made creating a threshold of DNA copies/mL for lactobacilli and several organisms known to be associated with BV (Table 4). At a threshold of ≥108 DNA copies/mL, Lactobacillus species was predictive of normal flora (Sensitivity 44%, Specificity 100%). BVAB-1, BVAB-2 and BVAB-3 alone or in combination had high specificity for BV diagnosed by Amsel criteria.
Table 3.
The sensitivities and specificities for individual or combinations of organisms for the diagnosis of BV using Amsel criteria or Nugent score
| Study | Diagnosis of BV | Organism | Sensitivity | Specificity |
|---|---|---|---|---|
| Frederick et al53 | Amsel | BVAB-1 | 40.7 | 97.8 |
| Frederick et al53 | Amsel | BVAB-2 | 88.9 | 95.7 |
| Frederick et al53 | Amsel | BVAB-3 | 40.7 | 97.8 |
| Frederick et al53 | Amsel | G.vaginalis | 100 | 41.3 |
| Frederick et al53 | Amsel | BVAB-1 and BVAB-3 | 33.3 | 100 |
| Frederick et al53 | Amsel | BVAB-2 or Megasphaera | 100 | 91.3 |
| Fredericks et al72 | Amsel | Either Megasphaera or BVAB-1, BVAB-2, or BVAB-3 | 99 | 89 |
| Fredericks et al72 | Nugent | Either Megasphaera or BVAB-1, BVAB-2, or BVAB-3 | 95.9 | 95.7 |
BVAB = bacterial vaginosis associated bacteria
Table 4.
Quantification of vaginal organisms for the production of BV using Nugent score159
| Organism | Threshold Quantification (DNA copies/mL) | Sensitivity | Specificity | NPV | PPV | ROC AUC |
|---|---|---|---|---|---|---|
| A. vaginae | ≥108 | 90 | 99 | 99 | 95 | 0.964 |
| G. vaginalis | ≥109 | 50 | 100 | 94 | 100 | 0.946 |
| M. curtisii | ≥105 | 45 | 100 | - | - | 0.798 |
| M. hominis | ≥106 | 30 | 98 | - | - | 0.691 |
NPV = Negative predictive value
PPV = Positive predictive value
ROC = Receiver operating characteristic
AUC = Area under the curve (The closer the AUC comes is to 1.0, the better the bacterial count predicts BV)
The combination of A. vaginae and G. vaginalis for the diagnosis of BV
Since A. vaginae and G. vaginalis are frequently detected in association with BV a number of authors using molecular-based techniques have examined the possibility of combining these two organisms as a means of diagnosing BV.52;53;59;112;155;159;160 Using DNA quantitation, 19/20 BV samples had either a DNA level for A. vaginae ≥108 copies/mL or G.vaginalis ≥ 109 copies/mL and 9/20 had both. The combination of an A.vaginae DNA level ≥108 copies/mL and a G.vaginalis DNA level ≥109 copies/mL demonstrated the best predictive criteria for the diagnosis of BV with excellent sensitivity (95%) specificity (99%) negative predictive value (NPV) (99%) and positive predictive value (PPV) (95%).159 When the quality and reproducibility of this combination was applied prospectively for validation of the Nugent score in 56 pregnant women the NPV was 96% and the PPV was 99%.159
Culture-Independent Techniques to Assess the Treatment of Recurrent, Persistent or Resistant BV
Cure of BV or improvement in symptoms following recommended treatments with metronidazole or clindamycin135 reaches 83-94% by seven to 21 days.198;199 While the short term treatment response is acceptable, BV persists or recurs in 11-29% of women at one month,198;200;201 30% of patients relapse within three months and recurrence rates may be more than 50% within a year.155;202-204 Only 48% of women will be colonized by H2O2 producing Lactobacilli 70-90 days after treatment with either clindamycin or metronidazole.201;205
A number of molecular-based studies53;105;155;206;207 have addressed the problems of recurrent or persistent BV over time, and why some women with BV may be resistant to cure. A consistent finding in these studies as women lapse in and out of being BV positive and BV negative is the stability of vaginal flora requiring few phylotypes and Lactobacillus dominance with L.crispatus and/or L. jensenii in women who remain or become BV negative. In contrast, those who become BV positive are commonly colonized by L. iners with many other non-Lactobacillus species present.53;105 Three studies have addressed the problem of persistent or recurrent BV using culture–independent techniques.155;206;207 Women with BV were appropriately treated and followed up in a large, prospective, cross-sectional cohort study over a 12 month period. A. vaginae was detected in 75% and G. vaginalis in 100% of women with recurrent BV. Women in whom both organisms were detected had higher rates of recurrence of BV (83%) compared to women with G. vaginalis alone (38%) (p<0.001). Of relevance is the fact that >90% of a biofilm indentified on vaginal epithelial cells of women with BV was composed of A. vaginae and G. vaginalis.208;209 The biofilm may have interfered with treatment, but the authors were unable to determine whether recurrence was due to inadequate treatment and undetectably low levels of residual organisms after treatment (i.e. relapse), or re-infection from sexual partners, which they thought was feasible, or disruption of normal flora from other exogenous factors.155
In an isolated study, several bacterial species were detected, none of which are commonly associated with BV. Organisms normally associated with BV were not detected. This atypical form of BV might explain why conventional therapy did not work and may indicate that other anti-microbial therapies may have been more effective.206 Finally, using species specific 16S rDNA PCR assays targeting 17 different BV associated bacteria in 131 women with BV, the vaginal microbiome was sampled pre-treatment and one month after for test of cure. Treatment was with a five day course of intravaginal metronidazole gel. At one month after treatment, BV was still present in 26% of women. The baseline detection of BVAB -1, BVAB -2, and BVAB -3, Peptoniphilus lacrimalis or Megasphaera phylotype was significantly associated with persistence of BV at test of cure. The authors concluded that pretreatment vaginal microbiology at diagnosis might define the risk of antibiotic failure.207 We anticipate that these correlations will become clearer and more meaningful when studies are repeated with quantitative PCR instead of simply using detection / incidence.
Culture-independent studies in pregnancy
Culture independent techniques have been used to measure prevalence, diversity and abundance of organisms particularly ureaplasmas210 in amniotic fluid in association with suspected cervical insufficiency,211 preterm labor,176;212 PPROM,178;213 babies small for gestational age,214 preeclampsia177 and the potential for bacteria from the oral cavity to colonize amniotic fluid.215 However, apart from combining pregnant women with non-pregnant women to swell sample numbers,52;160 the information with respect to the vaginal microbiome in pregnant women is limited particularly with respect to the outcome of pregnancy, especially preterm birth.
Using species specific primers, Wilks et al,101 quantified the production of H2O2 by lactobacilli from swabs taken at 20 weeks gestation from the vagina of 73 women considered to be at high risk of preterm birth according to the Creasy criteria.216 The amounts of H2O2 production varied between species of Lactobacillus. The presence of lactobacilli producing high levels of H2O2 was associated with a reduced incidence of BV at 20 weeks gestation and subsequent chorioamnionitis. The authors postulated that H2O2-producing lactobacilli reduced the incidence of ascending genital tract colonization in pregnancy which leads to infection and preterm birth.101 Unfortunately the role of L. iners, was not tested, because MRS agar culture medium was used in the study.90
In pregnant Japanese women, Tamrakar et al116 largely confirmed the findings of Fredricks et al 200553 in non-pregnant women. The prevalence of L.crispatus, L. jensenii, and L. gasseri was significantly higher, while that of BVAB-2, Megasphaera, Leptotrichia and Eggerthella-like bacterium were significantly lower in women with a normal Nugent score, compared to those with BV. The prevalence of L. iners did not differ between the these groups, and women with L. iners were more likely to be colonized by BVAB-2, Megasphaera, Leptotrichia and Eggerthella-like bacterium.116
In a longitudinal study of 100 pregnant women, vaginal swabs were obtained at mean gestational ages of 8.6, 21.2, and 32.4 weeks respectively.217 In first trimester, 77 women had normal or Lactobacillus dominated flora, 13 of whom developed abnormal flora in the second or third trimester. When first trimester normal flora was dominated by L. gasseri or L. iners there was a 10-fold risk of conversion to abnormal flora. In contrast, normal flora comprising L. crispatus had a five-fold decreased risk of conversion to abnormal flora.217 This may be because L. gasseri and L. iners only produce H2O2 in a small percentage of strains.95;131
CONCLUSIONS
Molecular based techniques provide important new information about vaginal microbial flora and permit identification of previously under-detected and hence under-appreciated organisms such as L. iners and A. vaginae. Molecular based techniques are not without their problems, and will not replace culture based techniques, but, when used in combination, add greatly to our understanding of vaginal flora. In the majority of circumstances, normal vaginal flora is dominated by Lactobacillus species. In the absence of lactobacilli, normality can be maintained by other, more fastidious lactic acid producing bacteria. In keeping with the theories of “competitive exclusion” and “bacterial interference”, when lactobacilli dominate the vaginal flora, culture-independent techniques have demonstrated that the healthy vagina is usually colonized by only one or two dominant Lactobacillus species, mainly from L. crispatus, L. iners, L. jensenii and L. gasseri. The dominant Lactobacillus species may differ racially or geographically, but the principle of numerical dominance persists, and may be an important defense mechanism. Without molecular based techniques, phenotypic identification of lactobacilli is difficult and so is normally only carried out to the genus level. By being able to identify lactobacilli to the species level, we should be better able to understand the role of different species of Lactobacillus, particularly with respect to their ability to produce H2O2 and to function as a probiotic.
Molecular-based techniques indicate that there is a far greater diversity of microorganisms associated with BV than has been evident from cultivation-dependant techniques. These diverse organisms accumulate to form different communities or profiles which make it likely that BV is not a single entity, but a syndrome of variable composition which cause a variety of symptoms, different phenotypical outcomes, and may result in variable responses to different antibiotic regimens. Some organisms or combinations of organisms have a high specificity for BV such that in future using molecular quantification, we may better diagnose each sub-type of BV and tailor treatment appropriately. The information with respect to the vaginal microbiome in pregnant women is limited particularly with respect to preterm birth. This gap is striking, given the importance of preterm birth problem worldwide, and must become a research and funding priority. By better understanding the vaginal microbiome during pregnancy, we may be able to predict and prevent some of the great obstetric syndromes like PPROM, preterm labor and preterm birth which is associated with infection and significant infant mortality and morbidity. This better understanding is imminent, with the onset of studies using much more powerful sequencing technologies.
Acknowledgments
Supported (in part) by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
Footnotes
Contribution to authorship – all authors have contributed
Details of ethics approval and Funding – not applicable
Disclosure of interests - None
Reference List
- 1.Witkin SS, Linhares IM, Giraldo P. Bacterial flora of the female genital tract: function and immune regulation 3. Best Pract Res Clin Obstet Gynaecol. 2007;21(3):347–354. doi: 10.1016/j.bpobgyn.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Plitt SS, Garfein RS, Gaydos CA, Strathdee SA, Sherman SG, Taha TE. Prevalence and correlates of chlamydia trachomatis, neisseria gonorrhoeae, trichomonas vaginalis infections, and bacterial vaginosis among a cohort of young injection drug users in Baltimore, Maryland. Sex Transm Dis. 2005;32(7):446–453. doi: 10.1097/01.olq.0000154567.21291.59. [DOI] [PubMed] [Google Scholar]
- 3.Schwebke JR. Gynecologic consequences of bacterial vaginosis. Obstet Gynecol Clin North Am. 2003;30(4):685–694. doi: 10.1016/s0889-8545(03)00086-x. [DOI] [PubMed] [Google Scholar]
- 4.Soper DE, Bump RC, Hurt WG. Bacterial vaginosis and trichomoniasis vaginitis are risk factors for cuff cellulitis after abdominal hysterectomy. Am J Obstet Gynecol. 1990;163(3):1016–1021. doi: 10.1016/0002-9378(90)91115-s. [DOI] [PubMed] [Google Scholar]
- 5.Cohen CR, Duerr A, Pruithithada N, Rugpao S, Hillier S, Garcia P, et al. Bacterial vaginosis and HIV seroprevalence among female commercial sex workers in Chiang Mai, Thailand. AIDS. 1995;9(9):1093–1097. doi: 10.1097/00002030-199509000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Cu-Uvin S, Hogan JW, Warren D, Klein RS, Peipert J, Schuman P, et al. Prevalence of lower genital tract infections among human immunodeficiency virus (HIV)-seropositive and high-risk HIV-seronegative women. HIV Epidemiology Research Study Group. Clin Infect Dis. 1999;29(5):1145–1150. doi: 10.1086/313434. [DOI] [PubMed] [Google Scholar]
- 7.Martin HL, Richardson BA, Nyange PM, Lavreys L, Hillier SL, Chohan B, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis. 1999;180(6):1863–1868. doi: 10.1086/315127. [DOI] [PubMed] [Google Scholar]
- 8.Sewankambo N, Gray RH, Wawer MJ, Paxton L, McNaim D, Wabwire-Mangen F, et al. HIV-1 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet. 1997;350(9077):546–550. doi: 10.1016/s0140-6736(97)01063-5. [DOI] [PubMed] [Google Scholar]
- 9.Taha TE, Hoover DR, Dallabetta GA, Kumwenda NI, Mtimavalye LA, Yang LP, et al. Bacterial vaginosis and disturbances of vaginal flora: association with increased acquisition of HIV. AIDS. 1998;12(13):1699–1706. doi: 10.1097/00002030-199813000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Larsson PG, Platz-Christensen JJ, Dalaker K, Eriksson K, Fahraeus L, Irminger K, et al. Treatment with 2% clindamycin vaginal cream prior to first trimester surgical abortion to reduce signs of postoperative infection: a prospective, double-blinded, placebo-controlled, multicenter study. Acta Obstet Gynecol Scand. 2000;79(5):390–396. [PubMed] [Google Scholar]
- 11.Ralph SG, Rutherford AJ, Wilson JD. Influence of bacterial vaginosis on conception and miscarriage in the first trimester: cohort study. BMJ. 1999;319(7204):220–223. doi: 10.1136/bmj.319.7204.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Llahi-Camp JM, Rai R, Ison C, Regan L, Taylor-Robinson D. Association of bacterial vaginosis with a history of second trimester miscarriage. Hum Reprod. 1996;11(7):1575–1578. doi: 10.1093/oxfordjournals.humrep.a019440. [DOI] [PubMed] [Google Scholar]
- 13.Hay PE, Lamont RF, Taylor-Robinson D, Morgan DJ, Ison C, Pearson J. Abnormal bacterial colonisation of the genital tract and subsequent preterm delivery and late miscarriage 665. BMJ. 1994;308(6924):295–298. doi: 10.1136/bmj.308.6924.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azargoon A, Darvishzadeh S. Association of bacterial vaginosis, trichomonas vaginalis, and vaginal acidity with outcome of pregnancy 1. Arch Iran Med. 2006;9(3):213–217. [PubMed] [Google Scholar]
- 15.Eschenbach DA, Gravett MG, Chen KC, Hoyme UB, Holmes KK. Bacterial vaginosis during pregnancy. An association with prematurity and postpartum complications 1973. Scand J Urol Nephrol Suppl. 1984;86:213–222. [PubMed] [Google Scholar]
- 16.Gratacos E, Figueras F, Barranco M, Vila J, Cararach V, Alonso PL, et al. Spontaneous recovery of bacterial vaginosis during pregnancy is not associated with an improved perinatal outcome 1971. Acta Obstet Gynecol Scand. 1998;77(1):37–40. [PubMed] [Google Scholar]
- 17.Gravett MG, Nelson HP, DeRouen T, Critchlow C, Eschenbach DA, Holmes KK. Independent associations of bacterial vaginosis and Chlamydia trachomatis infection with adverse pregnancy outcome 1969. JAMA. 1986;256(14):1899–1903. [PubMed] [Google Scholar]
- 18.Holst E, Goffeng AR, Andersch B. Bacterial vaginosis and vaginal microorganisms in idiopathic premature labor and association with pregnancy outcome 1972. J Clin Microbiol. 1994;32(1):176–186. doi: 10.1128/jcm.32.1.176-186.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDonald HM, O’Loughlin JA, Jolley P, Vigneswaran R, McDonald PJ. Prenatal microbiological risk factors associated with preterm birth. Br J Obstet Gynaecol. 1992;99(3):190–196. doi: 10.1111/j.1471-0528.1992.tb14497.x. [DOI] [PubMed] [Google Scholar]
- 20.Wennerholm UB, Holm B, Mattsby-Baltzer I, Nielsen T, Platz-Christensen J, Sundell G, et al. Fetal fibronectin, endotoxin, bacterial vaginosis and cervical length as predictors of preterm birth and neonatal morbidity in twin pregnancies 1970. Br J Obstet Gynaecol. 1997;104(12):1398–1404. doi: 10.1111/j.1471-0528.1997.tb11010.x. [DOI] [PubMed] [Google Scholar]
- 21.Lamont RF. Bacterial Vaginosis. In: Critchley H, Bennett P, Thornton S, editors. Preterm Birth. London: RCOG Press; 2004. pp. 163–180. [Google Scholar]
- 22.McGregor JA, French JI, Jones W, Milligan K, McKinney PJ, Patterson E, et al. Bacterial vaginosis is associated with prematurity and vaginal fluid mucinase and sialidase: results of a controlled trial of topical clindamycin cream 1966. Am J Obstet Gynecol. 1994;170(4):1048–1059. doi: 10.1016/s0002-9378(94)70098-2. [DOI] [PubMed] [Google Scholar]
- 23.Kurki T, Sivonen A, Renkonen OV, Savia E, Ylikorkala O. Bacterial vaginosis in early pregnancy and pregnancy outcome. Obstet Gynecol. 1992;80(2):173–177. [PubMed] [Google Scholar]
- 24.Riduan JM, Hillier SL, Utomo B, Wiknjosastro G, Linnan M, Kandun N. Bacterial vaginosis and prematurity in Indonesia: association in early and late pregnancy. Am J Obstet Gynecol. 1993;169(1):175–178. doi: 10.1016/0002-9378(93)90157-e. [DOI] [PubMed] [Google Scholar]
- 25.Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995;333(26):1737–1742. doi: 10.1056/NEJM199512283332604. [DOI] [PubMed] [Google Scholar]
- 26.Meis PJ, Goldenberg RL, Mercer B, Moawad A, Das A, McNellis D, et al. The preterm prediction study: significance of vaginal infections. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1995;173(4):1231–1235. doi: 10.1016/0002-9378(95)91360-2. [DOI] [PubMed] [Google Scholar]
- 27.Gibbs RS. Chorioamnionitis and bacterial vaginosis 7. Am J Obstet Gynecol. 1993;169(2 Pt 2):460–462. doi: 10.1016/0002-9378(93)90341-f. [DOI] [PubMed] [Google Scholar]
- 28.Martius J, Eschenbach DA. The role of bacterial vaginosis as a cause of amniotic fluid infection, chorioamnionitis and prematurity--a review 8. Arch Gynecol Obstet. 1990;247(1):1–13. doi: 10.1007/BF02390649. [DOI] [PubMed] [Google Scholar]
- 29.Jacobsson B, Pernevi P, Chidekel L, Jorgen Platz-Christensen J. Bacterial vaginosis in early pregnancy may predispose for preterm birth and postpartum endometritis 5. Acta Obstet Gynecol Scand. 2002;81(11):1006–1010. doi: 10.1034/j.1600-0412.2002.811103.x. [DOI] [PubMed] [Google Scholar]
- 30.Watts DH, Krohn MA, Hillier SL, Eschenbach DA. Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstet Gynecol. 1990;75(1):52–58. [PubMed] [Google Scholar]
- 31.Romero R, Espinoza J, Mazor M, Chaiworapongsa T. The preterm parturition syndrome. In: Critchley H, Bennett P, Thornton S, editors. Preterm Birth. London: RCOG Press; 2004. pp. 28–60. [Google Scholar]
- 32.Gotsch F, Romero R, Kusanovic JP, Mazaki-Tovi S, Pineles BL, Erez O, et al. The fetal inflammatory response syndrome. Clin Obstet Gynecol. 2007;50(3):652–683. doi: 10.1097/GRF.0b013e31811ebef6. [DOI] [PubMed] [Google Scholar]
- 33.Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. The fetal inflammatory response syndrome. Am J Obstet Gynecol. 1998;179(1):194–202. doi: 10.1016/s0002-9378(98)70272-8. [DOI] [PubMed] [Google Scholar]
- 34.Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics. 2000;106(4):659–671. doi: 10.1542/peds.106.4.659. [DOI] [PubMed] [Google Scholar]
- 35.Fellman V, Hellstrom-Westas L, Norman M, Westgren M, Kallen K, Lagercrantz H, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA. 2009;301(21):2225–2233. doi: 10.1001/jama.2009.771. [DOI] [PubMed] [Google Scholar]
- 36.March of Dimes Foundation. March of Dimes White Paper on Preterm Birth: the Global and Regional Toll. Internet. 2009 Dec 16; [Google Scholar]
- 37.Petrou S, Abangma G, Johnson S, Wolke D, Marlow N. Costs and Health Utilities Associated with Extremely Preterm Birth: Evidence from the EPICure Study. Value Health. 2009 doi: 10.1111/j.1524-4733.2009.00580.x. [DOI] [PubMed] [Google Scholar]
- 38.Institute of Medicine. Preterm Birth: Causes, Consequences, and Prevention. Institute of Medicine of the National Academies. 2006. 2009 Dec 16; [Google Scholar]
- 39.Keirse MJ. New perspectives for the effective treatment of preterm labor 10. Am J Obstet Gynecol. 1995;173(2):618–628. doi: 10.1016/0002-9378(95)90292-9. [DOI] [PubMed] [Google Scholar]
- 40.Chow AW, Bartlett KH. Sequential assessment of vaginal microflora in healthy women randomly assigned to tampon or napkin use. Rev Infect Dis. 1989;11(Suppl 1):S68–S73. doi: 10.1093/clinids/11.supplement_1.s68. [DOI] [PubMed] [Google Scholar]
- 41.Johnson SR, Petzold CR, Galask RP. Qualitative and quantitative changes of the vaginal microbial flora during the menstrual cycle. Am J Reprod Immunol Microbiol. 1985;9(1):1–5. doi: 10.1111/j.1600-0897.1985.tb00331.x. [DOI] [PubMed] [Google Scholar]
- 42.Larsen B, Monif GR. Understanding the bacterial flora of the female genital tract. Clin Infect Dis. 2001;32(4):e69–e77. doi: 10.1086/318710. [DOI] [PubMed] [Google Scholar]
- 43.Marrazzo JM, Koutsky LA, Eschenbach DA, Agnew K, Stine K, Hillier SL. Characterization of vaginal flora and bacterial vaginosis in women who have sex with women. J Infect Dis. 2002;185(9):1307–1313. doi: 10.1086/339884. [DOI] [PubMed] [Google Scholar]
- 44.Stahl CE, Hill GB. The clinical perspectives in obstetrics and gynecology. In: Galask RP, editor. Infectious Diseases in the Female Patient. New York: Springer; 2009. pp. 16–42. [Google Scholar]
- 45.Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–1359. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sidhu H, Allison MJ, Chow JM, Clark A, Peck AB. Rapid reversal of hyperoxaluria in a rat model after probiotic administration of Oxalobacter formigenes. J Urol. 2001;166(4):1487–1491. [PubMed] [Google Scholar]
- 47.Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449(7164):804–810. doi: 10.1038/nature06244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van HJ, Green DB. Relationship between the concentration of bacteria in saliva and the colonization of teeth in humans. Infect Immun. 1974;9(4):624–630. doi: 10.1128/iai.9.4.624-630.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim TK, Thomas SM, Ho M, Sharma S, Reich CI, Frank JA, et al. Heterogeneity of vaginal microbial communities within individuals. J Clin Microbiol. 2009;47(4):1181–1189. doi: 10.1128/JCM.00854-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of the human intestinal microbial flora. Science. 2005;308(5728):1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pavlova SI, Kilic AO, Kilic SS, So JS, Nader-Macias ME, Simoes JA, et al. Genetic diversity of vaginal lactobacilli from women in different countries based on 16S rRNA gene sequences. J Appl Microbiol. 2002;92(3):451–459. doi: 10.1046/j.1365-2672.2002.01547.x. [DOI] [PubMed] [Google Scholar]
- 52.Verhelst R, Verstraelen H, Claeys G, Verschraegen G, Delanghe J, Van SL, et al. Cloning of 16S rRNA genes amplified from normal and disturbed vaginal microflora suggests a strong association between Atopobium vaginae, Gardnerella vaginalis and bacterial vaginosis. BMC Microbiol. 2004;4:16. doi: 10.1186/1471-2180-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med. 2005;353(18):1899–1911. doi: 10.1056/NEJMoa043802. [DOI] [PubMed] [Google Scholar]
- 54.Oakley BB, Fiedler TL, Marrazzo JM, Fredricks DN. Diversity of human vaginal bacterial communities and associations with clinically defined bacterial vaginosis. Appl Environ Microbiol. 2008;74(15):4898–4909. doi: 10.1128/AEM.02884-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamamoto T, Zhou X, Williams CJ, Hochwalt A, Forney LJ. Bacterial populations in the vaginas of healthy adolescent women. J Pediatr Adolesc Gynecol. 2009;22(1):11–18. doi: 10.1016/j.jpag.2008.01.073. [DOI] [PubMed] [Google Scholar]
- 56.Zozaya-Hinchliffe M, Martin DH, Ferris MJ. Prevalence and abundance of uncultivated Megasphaera-like bacteria in the human vaginal environment. Appl Environ Microbiol. 2008;74(5):1656–1659. doi: 10.1128/AEM.02127-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hill JE, Goh SH, Money DM, Doyle M, Li A, Crosby WL, et al. Characterization of vaginal microflora of healthy, nonpregnant women by chaperonin-60 sequence-based methods. Am J Obstet Gynecol. 2005;193(3 Pt 1):682–692. doi: 10.1016/j.ajog.2005.02.094. [DOI] [PubMed] [Google Scholar]
- 58.Hyman RW, Fukushima M, Diamond L, Kumm J, Giudice LC, Davis RW. Microbes on the human vaginal epithelium. Proc Natl Acad Sci U S A. 2005;102(22):7952–7957. doi: 10.1073/pnas.0503236102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Trama JP, Pascal KE, Zimmerman J, Self MJ, Mordechai E, Adelson ME. Rapid detection of Atopobium vaginae and association with organisms implicated in bacterial vaginosis. Mol Cell Probes. 2008;22(2):96–102. doi: 10.1016/j.mcp.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 60.Schellenberg J, Links MG, Hill JE, Dumonceaux TJ, Peters GA, Tyler S, et al. Pyrosequencing of the chaperonin-60 universal target as a tool for determining microbial community composition. Appl Environ Microbiol. 2009;75(9):2889–2898. doi: 10.1128/AEM.01640-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yachi S, Loreau M. Biodiversity and ecosystem productivity in a fluctuating environment: the insurance hypothesis. Proc Natl Acad Sci U S A. 1999;96(4):1463–1468. doi: 10.1073/pnas.96.4.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhou X, Bent SJ, Schneider MG, Davis CC, Islam MR, Forney LJ. Characterization of vaginal microbial communities in adult healthy women using cultivation-independent methods. Microbiology. 2004;150(Pt 8):2565–2573. doi: 10.1099/mic.0.26905-0. [DOI] [PubMed] [Google Scholar]
- 63.Dethlefsen L, Fall-Ngai M, Relman DA. An ecological and evolutionary perspective on human-microbe mutualism and disease. Nature. 2007;449(7164):811–818. doi: 10.1038/nature06245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haruta S, Kato S, Yamamoto K, Igarashi Y. Intertwined interspecies relationships: approaches to untangle the microbial network. Environ Microbiol. 2009 doi: 10.1111/j.1462-2920.2009.01956.x. [DOI] [PubMed] [Google Scholar]
- 65.Burton JP, Reid G. Evaluation of the bacterial vaginal flora of 20 postmenopausal women by direct (Nugent score) and molecular (polymerase chain reaction and denaturing gradient gel electrophoresis) techniques. J Infect Dis. 2002;186(12):1770–1780. doi: 10.1086/345761. [DOI] [PubMed] [Google Scholar]
- 66.Hugenholtz P, Pace NR. Identifying microbial diversity in the natural environment: a molecular phylogenetic approach. Trends Biotechnol. 1996;14(6):190–197. doi: 10.1016/0167-7799(96)10025-1. [DOI] [PubMed] [Google Scholar]
- 67.Pace NR. A molecular view of microbial diversity and the biosphere. Science. 1997;276(5313):734–740. doi: 10.1126/science.276.5313.734. [DOI] [PubMed] [Google Scholar]
- 68.Hugenholtz P, Goebel BM, Pace NR. Impact of culture-independent studies on the emerging phylogenetic view of bacterial diversity. J Bacteriol. 1998;180(18):4765–4774. doi: 10.1128/jb.180.18.4765-4774.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baker GC, Smith JJ, Cowan DA. Review and re-analysis of domain-specific 16S primers. J Microbiol Methods. 2003;55(3):541–555. doi: 10.1016/j.mimet.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 70.Schmidt TM. The maturing of microbial ecology. Int Microbiol. 2006;9(3):217–223. [PubMed] [Google Scholar]
- 71.Weng L, Rubin EM, Bristow J. Application of sequence-based methods in human microbial ecology. Genome Res. 2006;16(3):316–322. doi: 10.1101/gr.3676406. [DOI] [PubMed] [Google Scholar]
- 72.Fredricks DN, Fiedler TL, Thomas KK, Oakley BB, Marrazzo JM. Targeted PCR for detection of vaginal bacteria associated with bacterial vaginosis. J Clin Microbiol. 2007;45(10):3270–3276. doi: 10.1128/JCM.01272-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hillier SL. The complexity of microbial diversity in bacterial vaginosis. N Engl J Med. 2005;353(18):1886–1887. doi: 10.1056/NEJMp058191. [DOI] [PubMed] [Google Scholar]
- 74.Donachie SP, Foster JS, Brown MV. Culture clash: challenging the dogma of microbial diversity. ISME J. 2007;1(2):97–99. doi: 10.1038/ismej.2007.22. [DOI] [PubMed] [Google Scholar]
- 75.Margulies M, Egholm M, Altman WE, Attiya S, Bader JS, Bemben LA, et al. Genome sequencing in microfabricated high-density picolitre reactors. Nature. 2005;437(7057):376–380. doi: 10.1038/nature03959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Petrosino JF, Highlander S, Luna RA, Gibbs RA, Versalovic J. Metagenomic pyrosequencing and microbial identification. Clin Chem. 2009;55(5):856–866. doi: 10.1373/clinchem.2008.107565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Forney LJ, Zhou X, Brown CJ. Molecular microbial ecology: land of the one-eyed king. Curr Opin Microbiol. 2004;7(3):210–220. doi: 10.1016/j.mib.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 78.Kalra A, Palcu CT, Sobel JD, Akins RA. Bacterial Vaginosis: Culture- and PCR-based Characterizations of a Complex Polymicrobial Disease’s Pathobiology. Curr Infect Dis Rep. 2007;9(6):485–500. doi: 10.1007/s11908-007-0074-4. [DOI] [PubMed] [Google Scholar]
- 79.Srinivasan S, Fredricks DN. The human vaginal bacterial biota and bacterial vaginosis. Interdiscip Perspect Infect Dis. 2008;2008:750479. doi: 10.1155/2008/750479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Skarin A, Sylwan J. Vaginal lactobacilli inhibiting growth of Gardnerella vaginalis, Mobiluncus and other bacterial species cultured from vaginal content of women with bacterial vaginosis. Acta Pathol Microbiol Immunol Scand B. 1986;94(6):399–403. doi: 10.1111/j.1699-0463.1986.tb03074.x. [DOI] [PubMed] [Google Scholar]
- 81.Hawes SE, Hillier SL, Benedetti J, Stevens CE, Koutsky LA, Wolner-Hanssen P, et al. Hydrogen peroxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis. 1996;174(5):1058–1063. doi: 10.1093/infdis/174.5.1058. [DOI] [PubMed] [Google Scholar]
- 82.Aroutcheva AA, Simoes JA, Faro S. Antimicrobial protein produced by vaginal Lactobacillus acidophilus that inhibits Gardnerella vaginalis. Infect Dis Obstet Gynecol. 2001;9(1):33–39. doi: 10.1155/S1064744901000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ng SC, Hart AL, Kamm MA, Stagg AJ, Knight SC. Mechanisms of action of probiotics: recent advances. Inflamm Bowel Dis. 2009;15(2):300–310. doi: 10.1002/ibd.20602. [DOI] [PubMed] [Google Scholar]
- 84.Doderlein A. Das scheidensekret und seine bedeutung fur puerperalfieber. Zbl Bakteriol. 1892;11:699. [Google Scholar]
- 85.Thomas S. Doderlein’s Bacillus: Lactobacillus Acidpohilus. J Infect Dis. 1928;43:218–227. [Google Scholar]
- 86.Lauer E, Helming C, Kandler O. Heterogeneity of the species Lactobacillus acidophilus (Moro) Hansen and Mocquot as revealed by biochemical characteristics and DNA-DNA hybridization. Zentbl Bakteriol Microbiol Hyg Abt. 1980;1:150–168. [Google Scholar]
- 87.Johnson JL, PHELPS CF, CUMMINS CS, LONDON J, GASSER F. Taxonomy of the Lactobacillus acidophilus Group. Int J Syst Bacteriol. 1980;30(1):53–68. [Google Scholar]
- 88.Schleifer KH, Ludwig W. Phylogeny of the genus Lactobacillus and related genera. Syst Appl Microbiol. 1995;18:461–467. [Google Scholar]
- 89.Du Plessis EM, Dicks LM. Evaluation of random amplified polymorphic DNA (RAPD)-PCR as a method to differentiate Lactobacillus acidophilus, Lactobacillus crispatus, Lactobacillus amylovorus, Lactobacillus gallinarum, Lactobacillus gasseri, and Lactobacillus johnsonii. Curr Microbiol. 1995;31(2):114–118. doi: 10.1007/BF00294286. [DOI] [PubMed] [Google Scholar]
- 90.Falsen E, Pascual C, Sjoden B, Ohlen M, Collins MD. Phenotypic and phylogenetic characterization of a novel Lactobacillus species from human sources: description of Lactobacillus iners sp. nov. Int J Syst Bacteriol. 1999;49(Pt 1):217–221. doi: 10.1099/00207713-49-1-217. [DOI] [PubMed] [Google Scholar]
- 91.Klein G, Pack A, Bonaparte C, Reuter G. Taxonomy and physiology of probiotic lactic acid bacteria. Int J Food Microbiol. 1998;41(2):103–125. doi: 10.1016/s0168-1605(98)00049-x. [DOI] [PubMed] [Google Scholar]
- 92.Redondo-Lopez V, Cook RL, Sobel JD. Emerging role of lactobacilli in the control and maintenance of the vaginal bacterial microflora. Rev Infect Dis. 1990;12(5):856–872. doi: 10.1093/clinids/12.5.856. [DOI] [PubMed] [Google Scholar]
- 93.Zhong W, Millsap H, Bialkowska-Hobrzanska H, Reid G. Differentiation of Lactobacillus species by molecular typing. Appl Environ Microbiol. 1998;64:2418–2423. doi: 10.1128/aem.64.7.2418-2423.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dimitonova SP, Bakalov BV, eksandrova-Georgieva RN, Danova ST. Phenotypic and molecular identification of lactobacilli isolated from vaginal secretions. J Microbiol Immunol Infect. 2008;41(6):469–477. [PubMed] [Google Scholar]
- 95.Antonio MA, Hawes SE, Hillier SL. The identification of vaginal Lactobacillus species and the demographic and microbiologic characteristics of women colonized by these species. J Infect Dis. 1999;180(6):1950–1956. doi: 10.1086/315109. [DOI] [PubMed] [Google Scholar]
- 96.Reid G, McGroarty JA, Tomeczek L, Bruce AW. Identification and plasmid profiles of Lactobacillus species from the vagina of 100 healthy women. FEMS Immunol Med Microbiol. 1996;15(1):23–26. doi: 10.1111/j.1574-695X.1996.tb00354.x. [DOI] [PubMed] [Google Scholar]
- 97.Vasquez A, Jakobsson T, Ahrne S, Forsum U, Molin G. Vaginal lactobacillus flora of healthy Swedish women. J Clin Microbiol. 2002;40(8):2746–2749. doi: 10.1128/JCM.40.8.2746-2749.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tarnberg M, Jakobsson T, Jonasson J, Forsum U. Identification of randomly selected colonies of lactobacilli from normal vaginal fluid by pyrosequencing of the 16S rDNA variable V1 and V3 regions. APMIS. 2002;110(11):802–810. doi: 10.1034/j.1600-0463.2002.1101106.x. [DOI] [PubMed] [Google Scholar]
- 99.Giorgi A, Torriani S, Dellaglio F, Bo G, Stola E, Bernuzzi L. Identification of vaginal lactobacilli from asymptomatic women. Microbiologica. 1987;10(4):377–384. [PubMed] [Google Scholar]
- 100.Song YL, Kato N, Matsumiya Y, Liu CX, Kato H, Watanabe K. Identification of and hydrogen peroxide production by fecal and vaginal lactobacilli isolated from Japanese women and newborn infants. J Clin Microbiol. 1999;37(9):3062–3064. doi: 10.1128/jcm.37.9.3062-3064.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wilks M, Wiggins R, Whiley A, Hennessy E, Warwick S, Porter H, et al. Identification and H(2)O(2) production of vaginal lactobacilli from pregnant women at high risk of preterm birth and relation with outcome. J Clin Microbiol. 2004;42(2):713–717. doi: 10.1128/JCM.42.2.713-717.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Anukam KC, Osazuwa EO, Ahonkhai I, Reid G. Lactobacillus vaginal microbiota of women attending a reproductive health care service in Benin city, Nigeria. Sex Transm Dis. 2006;33(1):59–62. doi: 10.1097/01.olq.0000175367.15559.c4. [DOI] [PubMed] [Google Scholar]
- 103.Zhou X, Brown CJ, Abdo Z, Davis CC, Hansmann MA, Joyce P, et al. Differences in the composition of vaginal microbial communities found in healthy Caucasian and black women. ISME J. 2007;1(2):121–133. doi: 10.1038/ismej.2007.12. [DOI] [PubMed] [Google Scholar]
- 104.Burton JP, Cadieux PA, Reid G. Improved understanding of the bacterial vaginal microbiota of women before and after probiotic instillation. Appl Environ Microbiol. 2003;69(1):97–101. doi: 10.1128/AEM.69.1.97-101.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wertz J, Isaacs-Cosgrove N, Holzman C, Marsh TL. Temporal Shifts in Microbial Communities in Nonpregnant African-American Women with and without Bacterial Vaginosis. Interdiscip Perspect Infect Dis. 2008;2008:181253. doi: 10.1155/2008/181253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Thies FL, Konig W, Konig B. Rapid characterization of the normal and disturbed vaginal microbiota by application of 16S rRNA gene terminal RFLP fingerprinting. J Med Microbiol. 2007;56(Pt 6):755–761. doi: 10.1099/jmm.0.46562-0. [DOI] [PubMed] [Google Scholar]
- 107.Biagi E, Vitali B, Pugliese C, Candela M, Donders GG, Brigidi P. Quantitative variations in the vaginal bacterial population associated with asymptomatic infections: a real-time polymerase chain reaction study. Eur J Clin Microbiol Infect Dis. 2009;28(3):281–285. doi: 10.1007/s10096-008-0617-0. [DOI] [PubMed] [Google Scholar]
- 108.Shi Y, Chen L, Tong J, Xu C. Preliminary characterization of vaginal microbiota in healthy Chinese women using cultivation-independent methods. J Obstet Gynaecol Res. 2009;35(3):525–532. doi: 10.1111/j.1447-0756.2008.00971.x. [DOI] [PubMed] [Google Scholar]
- 109.Vitali B, Pugliese C, Biagi E, Candela M, Turroni S, Bellen G, et al. Dynamics of vaginal bacterial communities in women developing bacterial vaginosis, candidiasis, or no infection, analyzed by PCR-denaturing gradient gel electrophoresis and real-time PCR. Appl Environ Microbiol. 2007;73(18):5731–5741. doi: 10.1128/AEM.01251-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29(2):297–301. doi: 10.1128/jcm.29.2.297-301.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Morse SA, Butel JS. Jawetz, Melnick & Adelberg’s Medical Microbiology. 23. New York: McGraw Hill; 1995. [Google Scholar]
- 112.Burton JP, Devillard E, Cadieux PA, Hammond JA, Reid G. Detection of Atopobium vaginae in postmenopausal women by cultivation-independent methods warrants further investigation. J Clin Microbiol. 2004;42(4):1829–1831. doi: 10.1128/JCM.42.4.1829-1831.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Martinez RC, Franceschini SA, Patta MC, Quintana SM, Nunes AC, Moreira JL, et al. Analysis of vaginal lactobacilli from healthy and infected Brazilian women. Appl Environ Microbiol. 2008;74(14):4539–4542. doi: 10.1128/AEM.00284-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Coolen MJ, Post E, Davis CC, Forney LJ. Characterization of microbial communities found in the human vagina by analysis of terminal restriction fragment length polymorphisms of 16S rRNA genes. Appl Environ Microbiol. 2005;71(12):8729–8737. doi: 10.1128/AEM.71.12.8729-8737.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Garg KB, Ganguli I, Das R, Talwar GP. Spectrum of Lactobacillus species present in healthy vagina of Indian women. Indian J Med Res. 2009;129(6):652–657. [PubMed] [Google Scholar]
- 116.Tamrakar R, Yamada T, Furuta I, Cho K, Morikawa M, Yamada H, et al. Association between Lactobacillus species and bacterial vaginosis-related bacteria, and bacterial vaginosis scores in pregnant Japanese women. BMC Infect Dis. 2007;7:128. doi: 10.1186/1471-2334-7-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Anukam KC, Reid G. Organisms associated with bacterial vaginosis in Nigerian women as determined by PCR-DGGE and 16S rRNA gene sequence. Afr Health Sci. 2007;7(2):68–72. doi: 10.5555/afhs.2007.7.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kilic AO, Pavlova SI, Alpay S, Kilic SS, Tao L. Comparative study of vaginal Lactobacillus phages isolated from women in the United States and Turkey: prevalence, morphology, host range, and DNA homology. Clin Diagn Lab Immunol. 2001;8(1):31–39. doi: 10.1128/CDLI.8.1.31-39.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ahrne S, Nobaek S, Jeppsson B, Adlerberth I, Wold AE, Molin G. The normal Lactobacillus flora of healthy human rectal and oral mucosa. J Appl Microbiol. 1998;85(1):88–94. doi: 10.1046/j.1365-2672.1998.00480.x. [DOI] [PubMed] [Google Scholar]
- 120.Benno Y, Endo K, Mizutani T, Namba Y, Komori T, Mitsuoka T. Comparison of fecal microflora of elderly persons in rural and urban areas of Japan. Appl Environ Microbiol. 1989;55(5):1100–1105. doi: 10.1128/aem.55.5.1100-1105.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cooperstock MS, Zedd AJ. Intestinal flora of infants. In: Hentges DJ, editor. Human intestinal microflora in health and disease. New York: Academic Press; 1983. pp. 79–99. [Google Scholar]
- 122.Eschenbach DA, Davick PR, Williams BL, Klebanoff SJ, Young-Smith K, Critchlow CM, et al. Prevalence of hydrogen peroxide-producing Lactobacillus species in normal women and women with bacterial vaginosis. J Clin Microbiol. 1989;27(2):251–256. doi: 10.1128/jcm.27.2.251-256.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Marrazzo JM, Antonio M, Agnew K, Hillier SL. Distribution of genital Lactobacillus strains shared by female sex partners. J Infect Dis. 2009;199(5):680–683. doi: 10.1086/596632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cherpes TL, Hillier SL, Meyn LA, Busch JL, Krohn MA. A delicate balance: risk factors for acquisition of bacterial vaginosis include sexual activity, absence of hydrogen peroxide-producing lactobacilli, black race, and positive herpes simplex virus type 2 serology. Sex Transm Dis. 2008;35(1):78–83. doi: 10.1097/OLQ.0b013e318156a5d0. [DOI] [PubMed] [Google Scholar]
- 125.McGroarty JA, Tomeczek L, Pond DG, Reid G, Bruce AW. Hydrogen peroxide production by Lactobacillus species: correlation with susceptibility to the spermicidal compound nonoxynol-9. J Infect Dis. 1992;165(6):1142–1144. doi: 10.1093/infdis/165.6.1142. [DOI] [PubMed] [Google Scholar]
- 126.Nagy E, Petterson M, Mardh PA. Antibiosis between bacteria isolated from the vagina of women with and without signs of bacterial vaginosis. APMIS. 1991;99(8):739–744. doi: 10.1111/j.1699-0463.1991.tb01253.x. [DOI] [PubMed] [Google Scholar]
- 127.Srinivasan S, Liu C, Mitchell CM, Fiedler TL, Thomas KK, Agnew KJ, et al. Temporal variability of human vaginal bacteria and relationship with bacterial vaginosis. PLoS One. 2010;5(4):e10197. doi: 10.1371/journal.pone.0010197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gardiner GE, Heinemann C, Bruce AW, Beuerman D, Reid G. Persistence of Lactobacillus fermentum RC-14 and Lactobacillus rhamnosus GR-1 but not L. rhamnosus GG in the human vagina as demonstrated by randomly amplified polymorphic DNA. Clin Diagn Lab Immunol. 2002;9(1):92–96. doi: 10.1128/CDLI.9.1.92-96.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Reid G, Charbonneau D, Erb J, Kochanowski B, Beuerman D, Poehner R, et al. Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women. FEMS Immunol Med Microbiol. 2003;35(2):131–134. doi: 10.1016/S0928-8244(02)00465-0. [DOI] [PubMed] [Google Scholar]
- 130.Vallor AC, Antonio MA, Hawes SE, Hillier SL. Factors associated with acquisition of, or persistent colonization by, vaginal lactobacilli: role of hydrogen peroxide production. J Infect Dis. 2001;184(11):1431–1436. doi: 10.1086/324445. [DOI] [PubMed] [Google Scholar]
- 131.Antonio MA, Rabe LK, Hillier SL. Colonization of the rectum by Lactobacillus species and decreased risk of bacterial vaginosis. J Infect Dis. 2005;192(3):394–398. doi: 10.1086/430926. [DOI] [PubMed] [Google Scholar]
- 132.Antonio MA, Hillier SL. DNA fingerprinting of Lactobacillus crispatus strain CTV-05 by repetitive element sequence-based PCR analysis in a pilot study of vaginal colonization. J Clin Microbiol. 2003;41(5):1881–1887. doi: 10.1128/JCM.41.5.1881-1887.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Antonio MA, Meyn LA, Murray PJ, Busse B, Hillier SL. Vaginal colonization by probiotic Lactobacillus crispatus CTV-05 is decreased by sexual activity and endogenous Lactobacilli. J Infect Dis. 2009;199(10):1506–1513. doi: 10.1086/598686. [DOI] [PubMed] [Google Scholar]
- 134.Smith T. Parasitism and Disease. Princeton: Princeton University Press; 1934. [Google Scholar]
- 135.Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006;55(RR-11):1–94. [PubMed] [Google Scholar]
- 136.Hay PE, Lamont RF, Taylor-Robinson D, Morgan DJ, Ison C, Pearson J. Abnormal bacterial colonisation of the genital tract and subsequent preterm delivery and late miscarriage. BMJ. 1994;308(6924):295–298. doi: 10.1136/bmj.308.6924.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Oleen-Burkey MA, Hillier SL. Pregnancy complications associated with bacterial vaginosis and their estimated costs. Infect Dis Obstet Gynecol. 1995;3(4):149–157. doi: 10.1155/S1064744995000500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hillier SL, Nugent RP, Eschenbach DA, Krohn MA, Gibbs RS, Martin DH, et al. Association between bacterial vaginosis and preterm delivery of a low-birth-weight infant. The Vaginal Infections and Prematurity Study Group. N Engl J Med. 1995;333(26):1737–1742. doi: 10.1056/NEJM199512283332604. [DOI] [PubMed] [Google Scholar]
- 139.Hillier SL. The vaginal microbial ecosystem and resistance to HIV. AIDS Res Hum Retroviruses. 1998;14(Suppl 1):S17–S21. [PubMed] [Google Scholar]
- 140.Schwebke JR. Role of Vaginal Flora As a Barrier to HIV Acquisition. Curr Infect Dis Rep. 2001;3(2):152–155. doi: 10.1007/s11908-996-0040-6. [DOI] [PubMed] [Google Scholar]
- 141.Coleman JS, Hitti J, Bukusi EA, Mwachari C, Muliro A, Nguti R, et al. Infectious correlates of HIV-1 shedding in the female upper and lower genital tracts. AIDS. 2007;21(6):755–759. doi: 10.1097/QAD.0b013e328012b838. [DOI] [PubMed] [Google Scholar]
- 142.Sha BE, Zariffard MR, Wang QJ, Chen HY, Bremer J, Cohen MH, et al. Female genital-tract HIV load correlates inversely with Lactobacillus species but positively with bacterial vaginosis and Mycoplasma hominis. J Infect Dis. 2005;191(1):25–32. doi: 10.1086/426394. [DOI] [PubMed] [Google Scholar]
- 143.Cherpes TL, Meyn LA, Krohn MA, Lurie JG, Hillier SL. Association between acquisition of herpes simplex virus type 2 in women and bacterial vaginosis. Clin Infect Dis. 2003;37(3):319–325. doi: 10.1086/375819. [DOI] [PubMed] [Google Scholar]
- 144.Kaul R, Nagelkerke NJ, Kimani J, Ngugi E, Bwayo JJ, Macdonald KS, et al. Prevalent herpes simplex virus type 2 infection is associated with altered vaginal flora and an increased susceptibility to multiple sexually transmitted infections. J Infect Dis. 2007;196(11):1692–1697. doi: 10.1086/522006. [DOI] [PubMed] [Google Scholar]
- 145.Wiesenfeld HC, Hillier SL, Krohn MA, Landers DV, Sweet RL. Bacterial vaginosis is a strong predictor of Neisseria gonorrhoeae and Chlamydia trachomatis infection. Clin Infect Dis. 2003;36(5):663–668. doi: 10.1086/367658. [DOI] [PubMed] [Google Scholar]
- 146.Spear GT, Sikaroodi M, Zariffard MR, Landay AL, French AL, Gillevet PM. Comparison of the diversity of the vaginal microbiota in HIV-infected and HIV-uninfected women with or without bacterial vaginosis. J Infect Dis. 2008;198(8):1131–1140. doi: 10.1086/591942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gardner HL, Dukes CD. Haemophilus vaginalis vaginitis: a newly defined specific infection previously classified non-specific vaginitis. Am J Obstet Gynecol. 1955;69(5):962–976. [PubMed] [Google Scholar]
- 148.Totten PA, Amsel R, Hale J, Piot P, Holmes KK. Selective differential human blood bilayer media for isolation of Gardnerella (Haemophilus) vaginalis. J Clin Microbiol. 1982;15(1):141–147. doi: 10.1128/jcm.15.1.141-147.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Stackebrandt E, Ludwig W. The importance of using outgroup reference organisms in phylogenetic studies: the Atopobium case. Syst Appl Microbiol. 1994;17:39–43. [Google Scholar]
- 150.Hauduroy P, Ehringer G, Urbain A, Guillot G, Magrou J. Dictionnaire des Bacteries Pathogenes. Paris: Masson; 1937. [Google Scholar]
- 151.Olsen I, Johnson JL, Moore LV, Moore WE. Lactobacillus uli sp. nov. and Lactobacillus rimae sp. nov. from the human gingival crevice and emended descriptions of lactobacillus minutus and Streptococcus parvulus. Int J Syst Bacteriol. 1991;41(2):261–266. doi: 10.1099/00207713-41-2-261. [DOI] [PubMed] [Google Scholar]
- 152.Weinberg M, Nativelle R, Prevot AR. Les Microbes Anaerobies. Paris: Masson; 1937. [Google Scholar]
- 153.Collins MD, Wallbanks S. Comparative sequence analyses of the 16S rRNA genes of Lactobacillus minutus, Lactobacillus rimae and Streptococcus parvulus: proposal for the creation of a new genus Atopobium. FEMS Microbiol Lett. 1992;74(2-3):235–240. doi: 10.1016/0378-1097(92)90435-q. [DOI] [PubMed] [Google Scholar]
- 154.Rodriguez JM, Collins MD, Sjoden B, Falsen E. Characterization of a novel Atopobium isolate from the human vagina: description of Atopobium vaginae sp. nov. Int J Syst Bacteriol. 1999;49(Pt 4):1573–1576. doi: 10.1099/00207713-49-4-1573. [DOI] [PubMed] [Google Scholar]
- 155.Bradshaw CS, Tabrizi SN, Fairley CK, Morton AN, Rudland E, Garland SM. The association of Atopobium vaginae and Gardnerella vaginalis with bacterial vaginosis and recurrence after oral metronidazole therapy. J Infect Dis. 2006;194(6):828–836. doi: 10.1086/506621. [DOI] [PubMed] [Google Scholar]
- 156.De Backer E, Dubreuil L, Brauman M, Acar J, Vaneechoutte M. In vitro activity of secnidazole against Atopobium vaginae, an anaerobic pathogen involved in bacterial vaginosis. Clin Microbiol Infect. 2009 doi: 10.1111/j.1469-0691.2009.02852.x. [DOI] [PubMed] [Google Scholar]
- 157.Ferris MJ, Masztal A, Aldridge KE, Fortenberry JD, Fidel PL, Jr, Martin DH. Association of Atopobium vaginae, a recently described metronidazole resistant anaerobe, with bacterial vaginosis. BMC Infect Dis. 2004;4:5. doi: 10.1186/1471-2334-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ferris MJ, Masztal A, Martin DH. Use of species-directed 16S rRNA gene PCR primers for detection of Atopobium vaginae in patients with bacterial vaginosis. J Clin Microbiol. 2004;42(12):5892–5894. doi: 10.1128/JCM.42.12.5892-5894.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Menard JP, Fenollar F, Henry M, Bretelle F, Raoult D. Molecular quantification of Gardnerella vaginalis and Atopobium vaginae loads to predict bacterial vaginosis. Clin Infect Dis. 2008;47(1):33–43. doi: 10.1086/588661. [DOI] [PubMed] [Google Scholar]
- 160.Verstraelen H, Verhelst R, Claeys G, Temmerman M, Vaneechoutte M. Culture-independent analysis of vaginal microflora: the unrecognized association of Atopobium vaginae with bacterial vaginosis. Am J Obstet Gynecol. 2004;191(4):1130–1132. doi: 10.1016/j.ajog.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 161.Dewhirst FE, Paster BJ, Tzellas N, Coleman B, Downes J, Spratt DA, et al. Characterization of novel human oral isolates and cloned 16S rDNA sequences that fall in the family Coriobacteriaceae: description of olsenella gen. nov., reclassification of Lactobacillus uli as Olsenella uli comb. nov. and description of Olsenella profusa sp. nov. Int J Syst Evol Microbiol. 2001;51(Pt 5):1797–1804. doi: 10.1099/00207713-51-5-1797. [DOI] [PubMed] [Google Scholar]
- 162.Downes J, Munson MA, Spratt DA, Kononen E, Tarkka E, Jousimies-Somer H, et al. Characterisation of Eubacterium-like strains isolated from oral infections. J Med Microbiol. 2001;50(11):947–951. doi: 10.1099/0022-1317-50-11-947. [DOI] [PubMed] [Google Scholar]
- 163.Eschenlauer SC, McKain N, Walker ND, McEwan NR, Newbold CJ, Wallace RJ. Ammonia production by ruminal microorganisms and enumeration, isolation, and characterization of bacteria capable of growth on peptides and amino acids from the sheep rumen. Appl Environ Microbiol. 2002;68(10):4925–4931. doi: 10.1128/AEM.68.10.4925-4931.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kazor CE, Mitchell PM, Lee AM, Stokes LN, Loesche WJ, Dewhirst FE, et al. Diversity of bacterial populations on the tongue dorsa of patients with halitosis and healthy patients. J Clin Microbiol. 2003;41(2):558–563. doi: 10.1128/JCM.41.2.558-563.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kumar PS, Griffen AL, Barton JA, Paster BJ, Moeschberger ML, Leys EJ. New bacterial species associated with chronic periodontitis. J Dent Res. 2003;82(5):338–344. doi: 10.1177/154405910308200503. [DOI] [PubMed] [Google Scholar]
- 166.Pybus V, Onderdonk AB. Evidence for a commensal, symbiotic relationship between Gardnerella vaginalis and Prevotella bivia involving ammonia: potential significance for bacterial vaginosis. J Infect Dis. 1997;175(2):406–413. doi: 10.1093/infdis/175.2.406. [DOI] [PubMed] [Google Scholar]
- 167.Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983;74(1):14–22. doi: 10.1016/0002-9343(83)91112-9. [DOI] [PubMed] [Google Scholar]
- 168.Taylor-Robinson D, Morgan DJ, Sheehan M, Rosenstein IJ, Lamont RF. Relation between Gram-stain and clinical criteria for diagnosing bacterial vaginosis with special reference to Gram grade II evaluation. Int J STD AIDS. 2003;14(1):6–10. doi: 10.1258/095646203321043183. [DOI] [PubMed] [Google Scholar]
- 169.Rosenstein IJ, Morgan DJ, Sheehan M, Lamont RF, Taylor-Robinson D. Bacterial vaginosis in pregnancy: distribution of bacterial species in different gram-stain categories of the vaginal flora. J Med Microbiol. 1996;45(2):120–126. doi: 10.1099/00222615-45-2-120. [DOI] [PubMed] [Google Scholar]
- 170.Paster BJ, Boches SK, Galvin JL, Ericson RE, Lau CN, Levanos VA, et al. Bacterial diversity in human subgingival plaque. J Bacteriol. 2001;183(12):3770–3783. doi: 10.1128/JB.183.12.3770-3783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Poco SE, Jr, Nakazawa F, Ikeda T, Sato M, Sato T, Hoshino E. Eubacterium exiguum sp. nov., isolated from human oral lesions. Int J Syst Bacteriol. 1996;46(4):1120–1124. doi: 10.1099/00207713-46-4-1120. [DOI] [PubMed] [Google Scholar]
- 172.Geissdorfer W, Bohmer C, Pelz K, Schoerner C, Frobenius W, Bogdan C. Tuboovarian abscess caused by Atopobium vaginae following transvaginal oocyte recovery. J Clin Microbiol. 2003;41(6):2788–2790. doi: 10.1128/JCM.41.6.2788-2790.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gundi VA, Desbriere R, La SB. Leptotrichia amnionii and the female reproductive tract. Emerg Infect Dis. 2004;10(11):2056–2057. doi: 10.3201/eid1011.031019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hanff PA, Rosol-Donoghue JA, Spiegel CA, Wilson KH, Moore LH. Leptotrichia sanguinegens sp. nov., a new agent of postpartum and neonatal bacteremia. Clin Infect Dis. 1995;20(Suppl 2):S237–S239. doi: 10.1093/clinids/20.supplement_2.s237. [DOI] [PubMed] [Google Scholar]
- 175.Shukla SK, Meier PR, Mitchell PD, Frank DN, Reed KD. Leptotrichia amnionii sp. nov., a novel bacterium isolated from the amniotic fluid of a woman after intrauterine fetal demise. J Clin Microbiol. 2002;40(9):3346–3349. doi: 10.1128/JCM.40.9.3346-3349.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.DiGiulio DB, Romero R, Amogan HP, Kusanovic JP, Bik EM, Gotsch F, et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One. 2008;3(8):e3056. doi: 10.1371/journal.pone.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.DiGiulio DB, Gervasi M, Romero R, Mazaki-Tovi S, Vaisbuch E, Kusanovic JP, et al. Microbial invasion of the amniotic cavity in preeclampsia as assessed by cultivation and sequence-based methods. J Perinat Med. 2010 doi: 10.1515/JPM.2010.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.DiGiulio DB, Romero R, Kusanovic JP, Gomez R, Kim CJ, Seok KS, et al. Prevalence and Diversity of Microbes in the Amniotic Fluid, the Fetal Inflammatory Response, and Pregnancy Outcome in Women with Preterm Pre-Labor Rupture of Membranes. Am J Reprod Immunol. 2010 doi: 10.1111/j.1600-0897.2010.00830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hebb JK, Cohen CR, Astete SG, Bukusi EA, Totten PA. Detection of novel organisms associated with salpingitis, by use of 16S rDNA polymerase chain reaction. J Infect Dis. 2004;190(12):2109–2120. doi: 10.1086/425929. [DOI] [PubMed] [Google Scholar]
- 180.Lepargneur JP, Dubreuil L, Levy J. Isolation of Dialister pneumosintes isolated from a bacteremia of vaginal origin. Anaerobe. 2006;12(5-6):274–275. doi: 10.1016/j.anaerobe.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 181.Donders GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salembier G, Spitz B. Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. BJOG. 2002;109(1):34–43. doi: 10.1111/j.1471-0528.2002.00432.x. [DOI] [PubMed] [Google Scholar]
- 182.Lamont RF, Hudson EA, Hay PE, Morgan DJ, Modi V, Ison CA, et al. A comparison of the use of Papanicolaou-stained cervical cytological smears with Gram-stained vaginal smears for the diagnosis of bacterial vaginosis in early pregnancy. Int J STD AIDS. 1999;10(2):93–97. doi: 10.1258/0956462991913709. [DOI] [PubMed] [Google Scholar]
- 183.Spiegel CA, Amsel R, Holmes KK. Diagnosis of bacterial vaginosis by direct gram stain of vaginal fluid. J Clin Microbiol. 1983;18(1):170–177. doi: 10.1128/jcm.18.1.170-177.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hay PE, Taylor-Robinson D, Lamont RF. Diagnosis of bacterial vaginosis in a gynaecology clinic. Br J Obstet Gynaecol. 1992;99(1):63–66. doi: 10.1111/j.1471-0528.1992.tb14395.x. [DOI] [PubMed] [Google Scholar]
- 185.Ison CA, Hay PE. Validation of a simplified grading of Gram stained vaginal smears for use in genitourinary medicine clinics. Sex Transm Infect. 2002;78(6):413–415. doi: 10.1136/sti.78.6.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Schmidt H, Hansen JG. Diagnosis of bacterial vaginosis by wet mount identification of bacterial morphotypes in vaginal fluid. Int J STD AIDS. 2000;11(3):150–155. doi: 10.1258/0956462001915589. [DOI] [PubMed] [Google Scholar]
- 187.Cauci S, Driussi S, Monte R, Lanzafame P, Pitzus E, Quadrifoglio F. Immunoglobulin A response against Gardnerella vaginalis hemolysin and sialidase activity in bacterial vaginosis. Am J Obstet Gynecol. 1998;178(3):511–515. doi: 10.1016/s0002-9378(98)70430-2. [DOI] [PubMed] [Google Scholar]
- 188.Myziuk L, Romanowski B, Johnson SC. BVBlue test for diagnosis of bacterial vaginosis. J Clin Microbiol. 2003;41(5):1925–1928. doi: 10.1128/JCM.41.5.1925-1928.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.O’Dowd TC, West RR, Winterburn PJ, Hewlins MJ. Evaluation of a rapid diagnostic test for bacterial vaginosis. Br J Obstet Gynaecol. 1996;103(4):366–370. doi: 10.1111/j.1471-0528.1996.tb09743.x. [DOI] [PubMed] [Google Scholar]
- 190.Thomason JL, Gelbart SM, Wilcoski LM, Peterson AK, Jilly BJ, Hamilton PR. Proline aminopeptidase activity as a rapid diagnostic test to confirm bacterial vaginosis. Obstet Gynecol. 1988;71(4):607–611. [PubMed] [Google Scholar]
- 191.Thomason JL, Gelbart SM, James JA, Edwards JM, Hamilton PR. Is analysis of vaginal secretions for volatile organic acids to detect bacterial vaginosis of any diagnostic value? Am J Obstet Gynecol. 1988;159(6):1509–1511. doi: 10.1016/0002-9378(88)90585-6. [DOI] [PubMed] [Google Scholar]
- 192.Wolrath H, Forsum U, Larsson PG, Boren H. Analysis of bacterial vaginosis-related amines in vaginal fluid by gas chromatography and mass spectrometry. J Clin Microbiol. 2001;39(11):4026–4031. doi: 10.1128/JCM.39.11.4026-4031.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Fredricks DN, Marrazzo JM. Molecular methodology in determining vaginal flora in health and disease: its time has come. Curr Infect Dis Rep. 2005;7(6):463–470. doi: 10.1007/s11908-005-0049-2. [DOI] [PubMed] [Google Scholar]
- 194.Doyle LM, McInerney JO, Mooney J, Powell R, Haikara A, Moran AP. Sequence of the gene encoding the 16S rRNA of the beer spoilage organism Megasphaera cerevisiae. J Ind Microbiol. 1995;15(2):67–70. doi: 10.1007/BF01569801. [DOI] [PubMed] [Google Scholar]
- 195.Ziola B, Gee L, Berg NN, Lee SY. Serogroups of the beer spoilage bacterium Megasphaera cerevisiae correlate with the molecular weight of the major EDTA-extractable surface protein. Can J Microbiol. 2000;46(2):95–100. doi: 10.1139/w99-123. [DOI] [PubMed] [Google Scholar]
- 196.Haggerty CL, Totten PA, Ferris M, Martin DH, Hoferka S, Astete SG, et al. Clinical characteristics of bacterial vaginosis among women testing positive for fastidious bacteria. Sex Transm Infect. 2009;85(4):242–248. doi: 10.1136/sti.2008.032821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ness RB, Hillier SL, Richter HE, Soper DE, Stamm C, McGregor J, et al. Douching in relation to bacterial vaginosis, lactobacilli, and facultative bacteria in the vagina. Obstet Gynecol. 2002;100(4):765. doi: 10.1016/s0029-7844(02)02184-1. [DOI] [PubMed] [Google Scholar]
- 198.Hanson JM, McGregor JA, Hillier SL, Eschenbach DA, Kreutner AK, Galask RP, et al. Metronidazole for bacterial vaginosis. A comparison of vaginal gel vs. oral therapy. J Reprod Med. 2000;45(11):889–896. [PubMed] [Google Scholar]
- 199.Livengood CH, III, Soper DE, Sheehan KL, Fenner DE, Martens MG, Nelson AL, et al. Comparison of once-daily and twice-daily dosing of 0.75% metronidazole gel in the treatment of bacterial vaginosis. Sex Transm Dis. 1999;26(3):137–142. doi: 10.1097/00007435-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 200.Livengood CH, III, McGregor JA, Soper DE, Newton E, Thomason JL. Bacterial vaginosis: efficacy and safety of intravaginal metronidazole treatment. Am J Obstet Gynecol. 1994;170(3):759–764. doi: 10.1016/s0002-9378(94)70278-0. [DOI] [PubMed] [Google Scholar]
- 201.Nyirjesy P, McIntosh MJ, Steinmetz JI, Schumacher RJ, Joffrion JL. The effects of intravaginal clindamycin and metronidazole therapy on vaginal mobiluncus morphotypes in patients with bacterial vaginosis. Sex Transm Dis. 2007;34(4):197–202. doi: 10.1097/01.olq.0000235152.98601.d7. [DOI] [PubMed] [Google Scholar]
- 202.Bradshaw CS, Morton AN, Hocking J, Garland SM, Morris MB, Moss LM, et al. High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. J Infect Dis. 2006;193(11):1478–1486. doi: 10.1086/503780. [DOI] [PubMed] [Google Scholar]
- 203.Sanchez S, Garcia PJ, Thomas KK, Catlin M, Holmes KK. Intravaginal metronidazole gel versus metronidazole plus nystatin ovules for bacterial vaginosis: a randomized controlled trial. Am J Obstet Gynecol. 2004;191(6):1898–1906. doi: 10.1016/j.ajog.2004.06.089. [DOI] [PubMed] [Google Scholar]
- 204.Sobel JD, Ferris D, Schwebke J, Nyirjesy P, Wiesenfeld HC, Peipert J, et al. Suppressive antibacterial therapy with 0.75% metronidazole vaginal gel to prevent recurrent bacterial vaginosis. Am J Obstet Gynecol. 2006;194(5):1283–1289. doi: 10.1016/j.ajog.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 205.Agnew KJ, Hillier SL. The effect of treatment regimens for vaginitis and cervicitis on vaginal colonization by lactobacilli. Sex Transm Dis. 1995;22(5):269–273. doi: 10.1097/00007435-199509000-00001. [DOI] [PubMed] [Google Scholar]
- 206.Devillard E, Burton JP, Reid G. Complexity of vaginal microflora as analyzed by PCR denaturing gradient gel electrophoresis in a patient with recurrent bacterial vaginosis. Infect Dis Obstet Gynecol. 2005;13(1):25–31. doi: 10.1080/10647440400025504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Marrazzo JM, Thomas KK, Fiedler TL, Ringwood K, Fredricks DN. Relationship of specific vaginal bacteria and bacterial vaginosis treatment failure in women who have sex with women. Ann Intern Med. 2008;149(1):20–28. doi: 10.7326/0003-4819-149-1-200807010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hale LP, Swidsinski A, Mendling W. Bacteria associated with bacterial vaginosis. N Engl J Med. 2006;354(2):202–203. doi: 10.1056/NEJMc053336. [DOI] [PubMed] [Google Scholar]
- 209.Swidsinski A, Mendling W, Loening-Baucke V, Swidsinski S, Dorffel Y, Scholze J, et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol. 2008;198(1):97–6. doi: 10.1016/j.ajog.2007.06.039. [DOI] [PubMed] [Google Scholar]
- 210.Kim M, Kim G, Romero R, Shim SS, Kim EC, Yoon BH. Biovar diversity of Ureaplasma urealyticum in amniotic fluid: distribution, intrauterine inflammatory response and pregnancy outcomes. J Perinat Med. 2003;31(2):146–152. doi: 10.1515/JPM.2003.020. [DOI] [PubMed] [Google Scholar]
- 211.Bujold E, Morency AM, Rallu F, Ferland S, Tetu A, Duperron L, et al. Bacteriology of amniotic fluid in women with suspected cervical insufficiency. J Obstet Gynaecol Can. 2008;30(10):882–887. doi: 10.1016/S1701-2163(16)32967-X. [DOI] [PubMed] [Google Scholar]
- 212.Yoon BH, Romero R, Lim JH, Shim SS, Hong JS, Shim JY, et al. The clinical significance of detecting Ureaplasma urealyticum by the polymerase chain reaction in the amniotic fluid of patients with preterm labor. Am J Obstet Gynecol. 2003;189(4):919–924. doi: 10.1067/s0002-9378(03)00839-1. [DOI] [PubMed] [Google Scholar]
- 213.Yoon BH, Romero R, Kim M, Kim EC, Kim T, Park JS, et al. Clinical implications of detection of Ureaplasma urealyticum in the amniotic cavity with the polymerase chain reaction. Am J Obstet Gynecol. 2000;183(5):1130–1137. doi: 10.1067/mob.2000.109036. [DOI] [PubMed] [Google Scholar]
- 214.DiGiulio DB, Gervasi M, Romero R, Vaisbuch E, Mazaki-Tovi S, Kusanovic JP, et al. Microbial invasion of the amniotic cavity in pregnancies with small-for-gestational-age fetuses. J Perinat Med. 2010 doi: 10.1515/JPM.2010.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Bearfield C, Davenport ES, Sivapathasundaram V, Allaker RP. Possible association between amniotic fluid micro-organism infection and microflora in the mouth. BJOG. 2002;109(5):527–533. doi: 10.1111/j.1471-0528.2002.01349.x. [DOI] [PubMed] [Google Scholar]
- 216.Creasy RK, Gummer BA, Liggins GC. System for predicting spontaneous preterm birth. Obstet Gynecol. 1980;55(6):692–695. [PubMed] [Google Scholar]
- 217.Verstraelen H, Verhelst R, Claeys G, De BE, Temmerman M, Vaneechoutte M. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 2009;9:116. doi: 10.1186/1471-2180-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]


