Abstract
This study evaluated the 10-year clinical performance of high-viscosity glass-ionomer cement placed in posterior permanent teeth by means of the Atraumatic Restorative Treatment (ART) approach. One operator placed 167 single- and 107 multiple-surface restorations in 43 high-risk caries pregnant women (mean decayed teeth = 9.8 ± 5.5). Examinations were performed at 1-, 2-, and 10-year intervals according to ART criteria. In the last evaluation, the US Public Health Service (USPHS) criteria were also used. After 10 years, 129 restorations (47.1%) were evaluated and achieved a cumulative survival rate of 49.0% (SE 7.2%). The 10-year survival of single- and multiple-surface ART restorations assessed using the ART criteria were 65.2% (SE 7.3%) and 30.6% (SE 9.9%), respectively. This difference was significant (jackknife SE of difference; p < 0.05). Using the USPHS criteria, the 10-year survival of single- and multiple-surface ART restorations were 86.5% and 57.6%, respectively. The primary causes of failure were total loss (9.3%) and marginal defects (5.4%). The survival rates observed, especially for the single-surface restorations, confirm the potential of the ART approach for restoring and saving posterior permanent teeth.
Keywords: Atraumatic restorative treatment, Clinical trial, Glass ionomer, Restorations, Cumulative survival
Introduction
The Atraumatic Restorative Treatment (ART) approach was introduced to provide dental preventive and restorative care to underserved populations in out-of-reach areas [1, 2]. Since its inception, this technique has been improved by the development of high-viscosity glass-ionomer cement (HVGIC), and its indication has expanded considerably [2, 3]. Clinical investigations conducted with children and adolescents assure reliable clinical performance of ART restorations for a 3-year period [4, 5]. However, long-term investigations are scarce and focused on one-surface cavities [6, 7]. Regarding the survival rates of multiple-surface ART restorations in permanent teeth, few studies have been carried out [8–11], and the information available is not sufficient. The survival of one-surface ART restorations in primary and permanent teeth does not vary much, only the survival of ART restorations in multiple surfaces in primary teeth varies [5]. In a randomized clinical trial conducted 10 years ago, 274 single- and multiple-surface glass-ionomer posterior restorations were performed using a modified ART approach as part of the restorative strategy of a prenatal oral healthcare program directed at 43 high-caries active pregnant patients of low social background. The impact of the program on the oral health status of the mother–child couple and the clinical behavior of the ART restorations were evaluated for 2 years [11, 12]. The aim of the present paper was to evaluate the 10-year survival rates of the single- and multiple-surface ART restorations placed in permanent posterior teeth of a high-risk caries group (DT = 9.8 ± 5.5).
Materials and methods
Study design
The materials and methods of the trial have been previously published [11, 12]. The study protocol was approved by the Bauru School of Dentistry Institutional Review Board. Informed consent was granted. Four hundred thirty patients attending eight public health centers of suburban areas of the city of Bauru were examined until 81 pregnant women (mean age 19 ± 3.7 years) could be selected. The inclusion criterion was the presence of three or more active carious lesions (cavities). The exclusion criteria were medical impairment and pulpal involvement. The subjects were randomly divided into two groups (in a non-blinded parallel design), namely the experimental group (n = 43) and the control group (n = 38). In both groups, the patients were submitted to a basic oral health program including restorative care, dietary counseling, oral hygiene instructions, professional prophylaxis, and fluoride topical applications. In the experimental group, all cavities were restored with the HVGIC Fuji IX (Fuji IX glass-ionomer cement, GC Dental Co., Tokyo, Japan) using the ART approach. In the control group, the posterior teeth were restored with reinforced ZOE cement (IRM-Dentsply/DeTrey, USA). As 90.8% of the ZOE restorations failed within 2 years, only the posterior ART restorations continued to be evaluated.
Restorative care
In both groups, all restorations were completed by one previously trained dentist, aided by a chair-side assistant, in a mobile dental unit. Cotton rolls and suction were used for moisture control. In the experimental group, the entrances of the cavities were widened with a dental hatchet, excavators were used to remove soft carious dentin based on tactile and optical criteria, and retentive grooves were prepared on the axiobucal and axiolingual line angles of Class II restorations using modified excavators specifically designed for this purpose n. 15–16 L and 17–18 L (SS WHITE, Rio de Janeiro, RJ, Brazil). In the control group, the cavities were cleaned with sharp excavators. In the profound cavities, a calcium hydroxide base (Hydro C, Dentsply/DeTrey, USA) was applied on the floor of the deepest part of these cavities.
In the experimental group, the prepared cavity and adjacent pits and fissures were conditioned with the liquid component of the cement. The HVGIC was hand-mixed according to the manufacturer’s instructions, and the “finger-press” technique was used [1]. Occlusion was checked with articulating paper (AccuFilm II, Parkell, Farmingdale, NY, USA) and adjusted with surgical scalpel blades n.11 (Free-Bac, Wuxi Xinda Medical Device Co., China). Surface protection was accomplished with Fuji Varnish (GC Dental Co., Tokyo, Japan). For proximal restorations, metal matrix strips and wood wedges (TDV Dental, Pomerode, SC, Brazil) were used before filling. The patients were instructed not to eat for at least 1 h after treatment.
The cavities were classified according to Black’s classification. Classes I and V restorations (n = 167) were recorded as single-surface restorations. Class II restorations (n = 107) were recorded as multiple-surface restorations.
Evaluations
Two calibrated dentists, not involved in the provision of restorative treatment, carried out the follow-up evaluations. The first evaluator participated in all three evaluations. The second evaluator was present at years 1 and 2 and then was replaced at year 10. In all examination periods, the criteria used were similar to those adopted in other ART studies (Table 1). Restorations scored as 0 or 1 for ART criteria were considered successful. Depth of marginal defects was measured using a CPI probe. At the 10-year examination, the US Public Health Service (USPHS) criteria [13] were also employed. Restorations scored as “alfa” or “bravo” for all USPHS categories were regarded as successful. At year 10, the examiners were calibrated under the supervision of an expert by means of duplicate examinations of 55 ART restorations on ten subjects with an interval of 2 weeks. Intra- and inter-examiner consistency was calculated for quality assessment of ART restorations. Considering ART criteria, inter-examiner consistency was excellent with a kappa-statistic value of 0.92. Intra-examiner kappa values were 0.96 for both examiners. For USPHS criteria, agreement was very high. The kappa-statistic values across the different categories ranged from 0.8 to 1.0 for intra-examiner reproducibility, and from 0.7 to 1.0 for inter-examiner reproducibility. In case of disagreement between evaluators, the subject was reexamined until a consensus was reached. The differences predominantly concerned scores 0 and 1 for ART criteria and scores “alpha” and “bravo” for USPHS criteria.
Table 1.
Criteria for evaluating ART restorations
| Code | Criterion | Definition |
|---|---|---|
| 0 | Present, satisfactory | Successful |
| 1 | Present, slight defect at the cavity margin of less than 0.5 mm; no repair is needed | Successful |
| 2 | Present, marginal defect deeper than 0.5 mm | Failed |
| 3 | Partially present, restoration and/or tooth breakdown | Failed |
| 4 | Not present, restoration missing | Failed |
| 5 | Not present, other restorative treatment has been performed | Failed |
| 6 | Not present, tooth has been extracted | Failed |
| 7 | Pulpal involvement | Failed |
| C | Caries present | Failed |
Adapted from [1]
The evaluation also assessed the presence of primary and secondary caries. Caries increment was evaluated using the Decayed, Missing, and Filling Surface index according to WHO criteria. The inter-examiner consistency for diagnosing dental caries was excellent, with kappa values of 0.92. Secondary caries is included as a category of the USPHS criteria. The ART criteria considered the physical condition of the restoration, but additionally, the presence of secondary caries was recorded. When secondary caries were present in combination with a mechanical failure, the latter was considered as the failure reason.
Statistical analysis
The actuarial method was applied for estimation of the survival percentages of ART restorations by using ART criteria and 95% confidence interval over time. The survival percentages were estimated in two ways: in the first analysis, including both re-restored and extracted teeth and, subsequently, in the second analysis, excluding both the categories of re-restored and extracted teeth. To deal with the dependency of the data (several restorations per patient), the jackknife method was used to calculate the standard error (SE) [14]. The difference between the survival percentages of single- and multiple-surface restorations was tested using the jackknife SE. Survival percentages of ART restorations assessed using ART and USPHS criteria at year 10 were compared using the McNemar test. Statistical significance was considered at p < 0.05.
Results
After 10 years, the examiners evaluated 129 posterior restorations, in that 67 were single- and 62 were multiple-surface restorations, in 20 patients. The lost-to-follow-up percentage of the restorations originally placed was 52.9% (145 out of 274 restorations). The mean number of posterior restoration per patient was 6.4 (SD = 3.5) at baseline. The mean number of restorations evaluated per patient after 10 years was 6.6 (SD = 3.6). The cumulative survival percentages according to ART code and the jackknife SE of the evaluated ART restorations are shown in Table 2. Figures 1 and 2 show successful Classes I and II restorations, respectively. There were no statistically significant differences between single- and multiple-surface restorations at 1-year (p = 0.137) and 2-year (p = 0.377) evaluations.
Table 2.
Cumulative survival and SE (%) of the ART restorations assessed using the ART criteria over a 10-year period
| Interval (year) | Single-surface ART restorations | Multiple-surface ART restorations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N rest at start | N rest lost | N rest fail | Survival (%) | ±SE (%) | N rest at start | N rest lost | N rest fail | Survival (%) | ±SE (%) | p value | |
| 0–1 | 167 | 21 | 2 | 98.7 | 1.2 | 107 | 9 | 9 | 91.2 | 4.8 | 0.137ns |
| 1–2 | 144 | 27 | 8 | 92.7 | 3.0 | 89 | 12 | 4 | 86.8 | 5.8 | 0.377ns |
| 2–10 | 109 | 42 | 19 | 65.2 | 7.3 | 73 | 11 | 35 | 30.6 | 9.9 | 0.009a |
N rest at start number of restorations at start of interval, N rest lost number of restorations lost-to-follow-up in the interval, N rest fail number of restorations failed in the interval
aSignificant
ns not significant
Fig. 1.
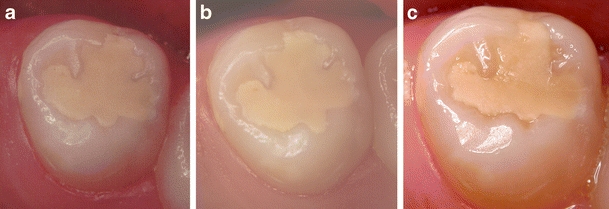
a–c One-surface ART restoration scored as successful at start and 2- and 10-year evaluations
Fig. 2.
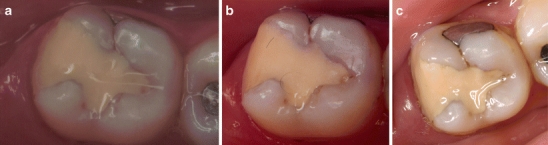
a–c Multiple-surface restoration scored as successful at start and 2- and 10-year evaluations
At the 10-year evaluation, considering ART codes 5 and 6 as failures, the survival rate for single-surface restorations (65.2%) was 2.1 times higher than that for the multiple-surface restorations (30.6%). This difference was statistically significant (p = 0.009). The survival rates observed when excluding the re-restored and extracted teeth (ART codes 5 and 6) from the statistical analysis showed survival rates of 86.5% and 57.6% for single- and multiple-surface restorations, respectively (Table 3). No significant difference in survival rates of ART restorations assessed using the ART and USPHS criteria was observed at 10 years (p = 1). The status of the restorations according to USPHS criteria are shown in Table 4. The reasons for failure of ART restorations assessed using ART criteria at the 10-year evaluation are provided in Table 5.
Table 3.
Cumulative survival and SE (%) of ART restorations assessed using the ART criteria over a 10-year period, excluding the re-restored and extracted teeth
| Interval (year) | Single-surface ART Restorations | Multiple-surface ART restorations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N rest at start | N rest lost | N rest fail | Survival (%) | ±SE (%) | N rest at start | N rest lost | N rest fail | Survival (%) | ±SE (%) | p value | |
| 0–1 | 167 | 21 | 2 | 98.7 | 1.2 | 107 | 9 | 9 | 91.2 | 4.8 | 0.137ns |
| 1–2 | 144 | 27 | 8 | 93.6 | 3.0 | 89 | 12 | 4 | 94.5 | 5.8 | 0.890ns |
| 2–10 | 97 | 54 | 7 | 86.5 | 4.9 | 52 | 32 | 14 | 57.6 | 10.0 | 0.014a |
N rest at start number of restorations at start of interval, N rest lost number of restorations lost-to-follow-up in the interval, N rest fail number of restorations failed in the interval
aSignificant
ns not significant
Table 4.
Status of the ART restorations (n and %) according to USPHS criteria at the 10-year evaluation
| Category | Rating | Type of restoration | Total | |
|---|---|---|---|---|
| Single-surface (Classes I and V) | Multiple-surface (Class II) | |||
| Marginal discoloration | Alfa | 37 (45.7) | 18 (22.3) | 55 (67.9) |
| Bravo | 13 (16) | 13 (16) | 26 (32.1) | |
| Charlie | – | – | – | |
| Marginal adaptation | Alfa | 30 (31.2) | 17 (17.7) | 47 (49) |
| Bravo | 18 (18.8) | 11 (11.5) | 29 (30.2) | |
| Charlie | 2 (2.1) | 3 (3.1) | 5 (5.2) | |
| Delta | 5 (5.2) | 10 (10.4) | 15 (15.6) | |
| Caries | Alfa | 52 (54.2) | 31 (32.3) | 83 (86.5) |
| Charlie | 3 (3.1) | 10 (10.4) | 13 (13.5) | |
| Anatomic form | Alfa | 38 (46.9) | 25 (30.9) | 63 (77.8) |
| Bravo | 9 (11.1) | 6 (7.4) | 15 (18.5) | |
| Charlie | 1 (1.2) | 2 (2.5) | 3 (3.7) | |
| Surface texture | Alfa | 1 (1.2) | 1 (1.2) | 2 (2.5) |
| Bravo | 49 (60.5) | 28 (34.6) | 77 (95) | |
| Charlie | – | 2 (2.5) | 2 (2.5) | |
| Color match | Alfa | 8 (9.9) | 1 (1.2) | 9 (11.1) |
| Bravo | 42 (51.9) | 27 (33.3) | 69 (85.2) | |
| Charlie | – | 3 (3.7) | 3 (3.7) | |
The restorations replaced for another treatment (n = 28) and the teeth extracted (n = 5) were excluded (scored as Oscar). The percentages given for caries and marginal adaptation relate to all restorations evaluated (n = 96). For other USPHS categories, percentages relate to restorations present without fractures (n = 81)
Table 5.
Reasons for failure of ART restorations assessed by using ART criteria at a 10-year evaluation (n and %)
| Code | Single surface | Multiple surface | Total |
|---|---|---|---|
| 2 | 2 | 4 | 6 |
| 3 | 2 | 1 | 3 |
| 4 | 3 | 9 | 12 |
| 5 | 10 | 18 | 28 |
| 6 | 2 | 3 | 5 |
| 7 | 0 | 0 | 0 |
| Total | 19 | 35 | 54 |
Secondary caries were detected in 13 ART-restored teeth and were always related to mechanical failures. Therefore, secondary caries were not regarded as the primary cause of failure. Caries increment was diagnosed in 33 dental surfaces (new lesions).
Discussion
In the present study and in other studies [9, 15], ART and USPHS criteria were applied to the same ART restorations in permanent teeth, with no significant differences in survival outcomes. Some authors [9, 15] have suggested that ART criteria are more stringent than USPHS criteria. We considered ART criteria adequate and comparable to those of USPHS and even easier to be reproduced. In spite of the limited sensitivity of the USPHS criteria in short-term clinical investigations [16], they are largely used and appraise properties such as marginal discoloration, color match, and surface texture, which are not taken into account by ART criteria. However, most restorations were scored as acceptable for these properties and, thus, did not impact the results.
The effectiveness of single-surface ART restorations in permanent dentition for a period of 3 years has been verified [4, 10]. Survival rates similar or superior to those achieved with amalgam restorations were reported after 6 years [5, 6, 10, 14]. In the present investigation, the cumulative survival rate of ART single-surface restorations remained high throughout the study—92.7% (SE 3.0%) over 2 years and 65.2% (SE 7.3%) up to 10 years. These rates are in line with the results of other investigations, which reported survival rates ranging from 66% [7, 14] to 76% [9] at 6 years for single-surface restorations. The cumulative success of 65.2% observed in this study could be considered even better due to the longer period of clinical service.
The survival rates of multiple-surface restorations (Class II) decreased significantly from 2 to 10 years. After 2 years, the survival rates between single- and multiple-surface restorations were similar (92.7 × 86.8%, respectively). These results are consistent with those of Cefaly [8] and Farag [17] which observed similar survival rates for Classes I and II restorations after 1 and 5 years, respectively. However, a statistical difference was apparent over the 10-year evaluation period (65.2 × 30.6% success rate for single- and multiple-surface restorations, respectively).
Caution is recommended when extending the indication of the ART approach to larger restorations. This does not necessarily mean that these restorations should not be performed if no conventional approach is available to control advanced carious lesions. Large untreated cavities are frequently observed in high-caries underserved populations even in permanent dentition. This study intended to provide an alternative treatment to limit this problem, but more studies are needed.
After 10 years, the replacement rates observed were 16% and 29% for single- and multiple-surface restorations, respectively. It is important to note that when an ART restoration was replaced by another restoration, according to the ART criteria, it was classified as a failure. Replaced restorations do not count as failures using the USPHS criteria. It is, therefore, justified to compare the survival results of ART restorations using the ART criteria with and without codes 5 and 6. When the re-restored teeth were excluded from the statistical analysis, the success rates observed were high for both types of restorations. This confirms the potential of the ART approach for saving posterior permanent decayed teeth. Indeed, we consider that the replacement of ART restorations should not be regarded as a failure inasmuch as ART was effective as to this primary purpose, or be it, to control caries damage and improve oral health of underserved populations until a conventional treatment is affordable. Only five teeth were extracted due to caries, and we considered this clinical observation as a failure.
The main cause of failure for both types of restorations was total loss (9.3%), followed by gross marginal defect (5.4%). The same pattern of failure was observed in other investigations [9]. Carious lesions adjacent to the restoration were observed in four teeth (1.2%) at 2 years and in 13 teeth (13.5%) at 10 years. No ART restoration failed because of carious lesion development only. All these 13 restorations failed because of a combination of dentine carious lesions and mechanical defects. This pattern of failure was also observed by Frencken et al. [6] but contrasts with the study of Prakki et al. [18] which observed no caries even in those teeth whose ART restorations were missing.
At the start of the study, the mean decayed surface index of the group was 15.9 and thus was considered as a high-caries risk group (Fig. 3). After 2 years, a mean increase of 2.0 tooth surfaces with new cavitated lesions was observed. At the 10-year evaluation, the mean increase of new caries lesion was 1.7, pointing out that the caries risk of these women had been reduced, thus emphasizing the preventive potential of the ART approach.
Fig. 3.

Seventeen-year-old pregnant women—oral condition at the start of the study
Especially regarding multiple-surface restorations, it is worth mentioning that it is not standard practice to use HVGIC for restoring large multiple-surface caries lesions due to the weakness of the material in stress-bearing situations, such as Class II posterior restorations [19]. Surprising, therefore, are the cumulative success rates of 86.8% (SE = 5.8) and 30.6% (SE = 9.9) observed after 2 and 10 years, respectively (Fig. 2), and the results are even better if the re-restored teeth were not considered as failures (survival rate of 57.6% at the 10-year evaluation). Initially, fracture resistance and retention may have been increased due to the inclusion of retentive grooves [20]. Over time, intrinsic alterations observed in the HVGIC structure can be related to the long-term survival of the restorations [21–23]. The findings of a correlated study (http://iadr.confex.com/iadr/2009miami/webprogram/Paper117559.html) which, by observing MEV-EDX and Knoop microhardness, analyzed seven samples of the same restorations that were clinically evaluated here, showed significant hardness improvement and chemical alterations of the glass ionomer after 10 years in vivo.
Every effort was made to appraise the patients’ restorations. The main reason for dropouts was the impossibility, over time, to find some of the patients, since they had moved to other areas or even cities. A high subject dropout rate has been reported for ART trials ranging from 25% to 70% at 6-year evaluations [7, 9, 14, 18]. In the present study, although the dropout rate was of 53.5% after 10 years, still, a significant number of restorations could be reevaluated. Nevertheless, the need for specific professional support directed to dental assistance for volunteers (research subjects) should be established at research centers and universities, independently of the recall periods. An identification card and financial support should also be offered to patients to guarantee their presence at the recalls thus minimizing the dropout rate frequently observed in cohort studies and the loss of re-restored teeth with no previous evaluation by the research team.
The present results are an important source of information about ART clinical behavior in permanent teeth and report on the longest examination period to be published.
Conclusion
The survival rates observed, especially for single-surface restorations, confirm the potential of the ART approach for restoring and saving posterior permanent teeth. The technique was effective after 10 years of clinical service.
Acknowledgments
The authors would like to thank the volunteers for their attendance in performing this study.
The authors would like to thank Angela Christine Charity for the English revision.
This investigation was supported by São Paulo State Foundation for Research Support (FAPESP), Grant 2007/04276-0.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P. Atraumatic restorative treatment (ART): rationale, technique, and development. J Public Health Dent. 1996;56:135–140. doi: 10.1111/j.1752-7325.1996.tb02423.x. [DOI] [PubMed] [Google Scholar]
- 2.Holmgren CJ. The state of ART (Atraumatic Restorative Treatment)—a scientific perspective. Community Dent Oral Epidemiol. 1999;27:419–460. doi: 10.1111/j.1600-0528.1999.tb02041.x. [DOI] [PubMed] [Google Scholar]
- 3.Zanata RL. Research proposal: evaluation of ART in adult patients. J Appl Oral Sci. 2006;14:25–29. doi: 10.1590/s1678-77572006000700006. [DOI] [PubMed] [Google Scholar]
- 4.Frencken JE, van’t Hof MA, Van Amerogen WE, Holmgren CJ. Effectiveness of single-surface ART restorations in the permanent dentition: a meta-analysis. J Dent Res. 2004;83:120–123. doi: 10.1177/154405910408300207. [DOI] [PubMed] [Google Scholar]
- 5.van't Hof MA, Frencken JE, van Palenstein Helderman WH, Holmgren CJ. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis. Int Dent J. 2006;56:345–351. doi: 10.1111/j.1875-595x.2006.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 6.Frencken JE, van’t Hof MA, Taifour D, Al-Zaher I. Effectiveness of ART and traditional amalgam approach in restoring single-surface cavities in posterior teeth of permanent dentitions in school children after 6.3 years. Community Dent Oral Epidemiol. 2007;35:207–214. doi: 10.1111/j.1600-0528.2006.00322.x. [DOI] [PubMed] [Google Scholar]
- 7.Mandari GJ, Frencken JE, van't Hof MA. Six-year success rates of occlusal amalgam and glass-ionomer restorations placed using three minimal intervention approaches. Caries Res. 2003;37:246–253. doi: 10.1159/000070866. [DOI] [PubMed] [Google Scholar]
- 8.Cefaly DFG, Barata TJE, Bresciani E, Fagundes TC, Lauris JRP, Navarro MFL. Clinical evaluation of multiple-surface ART restorations: 12 month follow-up. J Dent Child. 2007;74:203–208. [PubMed] [Google Scholar]
- 9.Lo EC, Holmgren CJ, Hu D, van Palenstein HW. Six-year follow up of atraumatic restorative treatment restorations placed in Chinese school children. Community Dent Oral Epidemiol. 2007;35:387–392. doi: 10.1111/j.1600-0528.2006.00342.x. [DOI] [PubMed] [Google Scholar]
- 10.Mickenautsch S, Yengopal V, Banerjee A. Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review. Clin Oral Invest. 2009 doi: 10.1007/s00784-009-0335-8. [DOI] [PubMed] [Google Scholar]
- 11.Zanata RL, Navarro MF, Barbosa SH, Lauris JR, Franco EB. Clinical evaluation of three restorative materials applied in a minimal intervention caries treatment approach. J Public Health Dent. 2003;63:221–226. doi: 10.1111/j.1752-7325.2003.tb03503.x. [DOI] [PubMed] [Google Scholar]
- 12.Zanata RL, Navarro MF, Pereira JC, Franco EB, Lauris JR, Barbosa SH. Effect of caries preventive measures directed to expectant mothers on caries experience in their children. Braz Dent J. 2003;14:75–81. doi: 10.1590/S0103-64402003000200001. [DOI] [PubMed] [Google Scholar]
- 13.Ryge G. Clinical criteria. Int Dent J. 1980;30:347–358. [PubMed] [Google Scholar]
- 14.Frencken JE, Taifour D, van't Hof MA. Survival of ART and amalgam restorations in permanent teeth of children after 6.3 years. J Dent Res. 2006;85:622–626. doi: 10.1177/154405910608500708. [DOI] [PubMed] [Google Scholar]
- 15.Lo EC, Luo Y, Fan MW, Wei SH. Clinical investigation of two glass-ionomer restoratives used with the atraumatic restorative treatment approach in China: two-year results. Caries Res. 2001;35:458–463. doi: 10.1159/000047490. [DOI] [PubMed] [Google Scholar]
- 16.Hickel R, Roulet JF, Bayne S, Heintze SD, Mjor IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Invest. 2007;11:5–33. doi: 10.1007/s00784-006-0095-7. [DOI] [PubMed] [Google Scholar]
- 17.Farag A, van der Sanden WJM, Abdelwahab H, Mulder J, Frencken JE. 5-year survival of ART restorations with and without cavity disinfection. J Dent. 2009;37:468–474. doi: 10.1016/j.jdent.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Prakki A, Nunes MC, Cefaly DF, Lauris JR, Navarro MF. Six-year evaluation of the atraumatic restorative treatment approach in permanent-tooth Class III restorations. J Adhes Dent. 2008;10:233–237. [PubMed] [Google Scholar]
- 19.Mickenautsch S, Grossman E. Atraumatic Restorative Treatment (ART): factors affecting success. J Appl Oral Sci. 2006;14:34–36. doi: 10.1590/S1678-77572006000700008. [DOI] [PubMed] [Google Scholar]
- 20.Barata TJE, Bresciane E, Fagundes TC, Cefaly DFG, Lauris JRP, Navarro MFL. Fracture resistance of Class II glass-ionomer cement restorations. Am J Dent. 2008;21:163–167. [PubMed] [Google Scholar]
- 21.Okada K, Tosaki S, Hirota K, Hume WR. Surface hardness change of restorative filling materials stored in saliva. Dent Mater. 2001;17:34–39. doi: 10.1016/S0109-5641(00)00053-1. [DOI] [PubMed] [Google Scholar]
- 22.Van Duinen NB, Davidson CL, De Gee AJ, Feilzer AJ. In situ transformation of glass-ionomer into an enamel-like material. Am J Dent. 2004;17:223–227. [PubMed] [Google Scholar]
- 23.Wang XY, Ayu J, Ngo HC. Influence of enviromental calcium/phosphate and pH on glass ionomers. Eur J Oral Sci. 2007;115:224–229. doi: 10.1111/j.1600-0722.2007.00443.x. [DOI] [PubMed] [Google Scholar]


