Abstract
The management of suicide risk in patients with schizophrenia poses many challenges for clinicians. Compared with the general population, these patients have an 8.5-fold greater risk of suicide. This article reviews the literature dealing with the treatment of at-risk patients with schizophrenia. An integrated psychosocial and pharmacological approach to managing this population of patients is recommended. Although there is at least modest evidence suggesting that antipsychotic medications protect against suicidal risk, the evidence appears to be most favourable for second-generation antipsychotics, particularly clozapine, which is the only medication approved by the US FDA for preventing suicide in patients with schizophrenia. In addition, treating depressive symptoms in patients with schizophrenia is an important component of suicide risk reduction. While selective serotonin receptor inhibitors (SSRIs) ameliorate depressive symptoms in patients with schizophrenia, they also appear to attenuate suicidal thoughts. Further research is needed to more effectively personalize the treatment of suicidal thoughts and behaviours and the prevention of suicide in patients with schizophrenia.
Suicide is one of the leading causes of premature death among people with schizophrenia.[1,2] Epidemiological investigation has established suicidal behaviour as more frequent in patients with schizophrenia than in the general population.[3] Compared with the general population, schizophrenia patients have an 8.5-fold greater risk of suicide,[4] a rate surpassed only by people with severe mood disorders.[5] Between 40% and 50% of people with schizophrenia report suicidal ideation at some point in their lives, 20–50% have a history of suicide attempts[6,7] and 4–13% eventually commit suicide.[3,8,9] Much of the literature has suggested that 9–13% of patients with schizophrenia have completed suicide.[4,9,10] However, in a recent review of the literature on suicide and schizophrenia, Palmer et al.[11] reported an overall prevalence estimate for completed suicide of 4.9%, which illustrates the differing ways of expressing this suicide rate.
Most completed suicides appear to occur early in the disease process. However, the risk of suicidal behaviours in patients with schizophrenia is lifelong.[12] Individuals with schizophrenia who attempt suicide appear to be more impulsive.[11,13]
The treatment of patients with schizophrenia and suicidal behaviour is challenging. This article reviews the literature related to the treatment of schizophrenia patients with suicidal behaviour, focusing on pharmacological treatments, with the purpose of assisting mental health professionals to better understand some of the treatment challenges.
1. Risk Factors
In order to diminish suicide among people with schizophrenia, researchers have frequently focused on risk factors. This involves identifying which patients are most at risk for suicide, so as to more effectively implement appropriate interventions.
Risk factors include the presence of previous attempts, greater lethality of attempts, hopelessness, psychotic symptoms and fewer provisions for being rescued.[12,14–22] In addition, individuals with highly severe illness – as evidenced by an early age of onset, long duration of index hospitalization, frequent hospitalizations and relapses, and the use of high doses of antipsychotic medications – also are at elevated suicide risk.[8,17,19,21,23,24] In addition, social support strongly mediates levels of suicidal behaviours.[15,22,24,25] Coexisting depressive symptoms in general have also been established as an important risk factor.[8,12,15,16,19,20,24,26]
The majority of suicides for patients with schizophrenia occur within the first 10 years after illness onset,[22,25,27] and 50% occur within the first 2 years.[20] Not only are patients at higher risk in the years directly following their initial diagnosis, but they are also more likely to commit suicide within the first few weeks or months after a hospital discharge.[16,24,28] For example, in one series, 80% of patients with schizophrenia who committed suicide did so while in the hospital or within 6 months of discharge.[18] This relationship between hospital discharge and suicidality may be the result of a ‘postpsychotic depression’.[24,29–31] Often in this scenario, it is believed that people with schizophrenia whose symptoms improve while in the hospital consequently gain a better awareness of their life circumstance, and experience a corresponding increase in despair, which then appears to increase the risk for suicide on discharge from hospital. If this occurs, increased monitoring with diligent clinical care from clinicians is needed.
The connection between suicide, schizophrenia and substance abuse is also important.[27,32,33] Substance abuse and alcoholism can worsen impulsiveness as well as social isolation.
Another important factor is the positive association found between the duration of psychosis and suicide risk in patients with schizophrenia.[34] This supports the notion that early treatment is needed not only for alleviating symptoms of the disease but also in preventing suicidal behaviour.
2. Demographic Factors
Men with schizophrenia commit suicide more frequently than women with schizophrenia.[8,18,25,35,36] It is not known whether this increased risk is related to a worsened course of illness or an earlier onset of disease – both of which are frequently observed among men.[5,37] This earlier onset of disease in combination with a more severe illness could lead to lower levels of social and occupational functioning, and increased rates of hospitalization.[20,21,25] Men with schizophrenia also commit suicide at a younger age than women with the disorder.[38,39]
The mean age of patients with schizophrenia who commit suicide is approximately 33 years,[7,40] with one study noting the greatest risk occurring between 20 and 39 years of age,[41] and a more general range cited between 22 and 40 years of age.[22] The higher rate of suicide seen among young people with schizophrenia is at odds with trends in the general population. However, this is not to say that elderly people with schizophrenia are not vulnerable, since they commit suicide as well.[12,42]
3. Assessment and Initial Management
Patients with schizophrenia require a thorough assessment of the nature of their suicidal ideation or behaviour, their suicide risk and what factors are contributing to the suicidal symptoms. Once this is accomplished, a clinical decision must be made as to the appropriate setting for treating the patient, i.e. either inpatient or outpatient. The goals of treatment are to (i) reduce psychotic symptoms; (ii) reduce depressive symptoms; (iii) alleviate the patient’s sense of demoralization and despair; (iv) instil hope; and (v) address any other issues such as substance abuse and anxiety disorders.[43] A thorough consideration should be made of the full range of treatments available in order to treat the problem, which includes restriction to the means of self-harm.[44] There are limited data supporting both psychosocial and pharmacological approaches,[45] so clinicians may need to base decisions on how to treat suicidality on data from studies directed at the management of affective disorders.[43] Clearly, upon discharge from hospitalization, it is important to set up psychosocial programmes as part of the after-care plan to augment the pharmacological treatment.
4. Staff Education in the Management of the Suicidal Patient with Schizophrenia
It is important to make medical staff well aware of how best to interact with a suicidal patient with schizophrenia. Risk factors for suicide include poor relationships with the staff and difficulty acclimatizing to the ward environment.[34,46] An important component of the treatment milieu is to have staff ready to deal with patients’ anxiety and despair. It is also important for staff to realize that a more withdrawn or paranoid patient should be regarded as one having an increased risk of suicide. Farberow et al.[47] demonstrated that suicidal patients made more demands on hospital personnel and criticized the treatment more than other patients. These suicidal individuals were also more likely to express ambivalence about leaving the security of the hospital and needed a great deal of reassurance and support. Morgan and Priest[48,49] described a state of “terminal malignant alienation”, resulting from the patient’s fluctuating suicidality and excessive demands, which led to distancing of the patient from the staff, eventually leading to rejection. It is important for staff to maintain good morale in these situations.[50–52]
5. Psychosocial Modalities
Psychosocial interventions have been shown to be beneficial, in general, in patients with schizophrenia. There are a variety of psychosocial approaches available for the treatment of suicidal patients with schizophrenia, and their degree of effectiveness is an area that requires further research.[53] An integrated approach using several psychosocial modalities is regarded as standard practice in treating patients with schizophrenia.[54–56] One 2-year trial, which compared an integrated biomedical/psychosocial treatment with standard pharmacotherapy and case management in patients with recent-onset schizophrenia, has also supported the use of integrated care as a way to improve outcomes, including positive and negative symptom outcomes.[57] Other approaches include supportive employment, family intervention, psychoeducation, assertive community treatment, social skills training and cognitive behavioural treatment; the latter appears to improve insight, positive symptoms and depressive symptoms and also suicidal behaviour.[58–62]
Patients with schizophrenia clearly need empathetic support when they exhibit suicidal behaviour.[63] Providers need to acknowledge the patient’s degree of despair, losses and troubles with daily life, and to engage the patient in establishing realistic goals.[8,26,62] Sensitivity addressing subjective distress and hopelessness is also important, since despair is known to be a risk factor for completed suicide in patients with schizophrenia.[36,45,64] Cotton et al.[21] stressed the importance of providing supportive psychotherapeutic interventions aimed at discussing daily difficulties, medications, adverse effects, social isolation, money and stigma. They also outlined the importance of psychotherapy in helping this group of patients better understand how hopelessness plays a part in their illness. In addition, Mueser and Berenbaum[65] reviewed controlled trials of psychotherapy in this group of patients and concluded that reality-orientated psychotherapy is the optimal approach. Harkavy-Friedman and Nelson[66] offered a comprehensive discussion of the ways in which clinicians can intervene in crisis situations. Their discussions included the use of mobile multidisciplinary outreach teams and crisis-oriented day treatment.
One common outcome in patients with schizophrenia is the development of the demoralization syndrome.[67] As patients become aware of their illness and its consequences they develop a state of hopelessness. This can lead to depression and suicidal behaviour. Restifo et al.[68] tested the validity of this model in 164 patients. They assessed depression, pre-morbid functioning, insight and suicidal behaviour, and determined that the interaction between good pre-morbid adjustment and insight predicted greater severity of depressive symptoms. Furthermore, psychological symptoms of depression were able to distinguish suicide attempters from non-attempters, while the somatic symptoms did not.[69]
Enhancing adherence to psychiatric follow-up and maintenance of social support are important components of caring for this group of patients.[70,71] In addition, maintaining adherence to antipsychotic drug treatment is a critical component of the treatment of patients with schizophrenia in general.[72] Improving poor adherence with treatment is important, since poor treatment adherence has been shown to be associated with suicidal risk.[73] For instance, one study that examined adherence to second-generation antipsychotic medications in two Canadian provinces demonstrated that good medication adherence was associated with a reduction in hospitalization.[74] In addition, there was a significant association of poor adherence with risk of suicide and with death in general; the adjusted hazard ratio (HR) for the risk of suicide was 0.68 for good versus poor compliance.[74]
Thus, psychosocial approaches appear to be important in stabilizing symptoms in suicidal patients with schizophrenia.[45,54,55,75] However, more research is clearly needed in this area.
6. Pharmacological Approaches
In this section, we initially discuss the use of antipsychotics to treat the suicidal patient with schizophrenia; we then discuss antidepressant augmentation of antipsychotic treatment. One set of agents not well studied are mood stabilizers. Mood stabilizers, including lithium, are frequently used by clinicians in this population of patients. There is much evidence supporting the efficacy of lithium in reducing suicidal behaviour in patients with bipolar disorder;[76] however, there is very little evidence available to support its use as being of benefit in treating patients with schizophrenia in general or in helping reduce suicidal behaviour in these patients.[77]
6.1 First-Generation Antipsychotics
Even though first-generation antipsychotics are successful in treating positive symptoms, this is not necessarily associated with a decreased suicide risk. The suicide rates determined in 1975 and in 1992 indicate that there was no appreciable change, despite the increasing use of antipsychotics during this time period.[78,79] In general, the literature on the effects of first-generation antipsychotic drugs is inconsistent in determining whether these agents are helpful with the suicidal patient.[43] These inconsistencies may be related to several methodological factors, including the retrospective design of most of these studies, failure to address confounding factors, co-morbidity, multiple medications and absence of randomization in treatment assignment.[80,81]
In general, no clear dose-effect relationship with suicidal behaviour has been found for first-generation antipsychotic medications. For instance, no differences in daily doses were found between patients with schizophrenia who completed suicide and those who did not compete suicide.[82] Also, with one exception, results of studies suggest that there is no greater likelihood that suicidal behaviours improve in patients with schizophrenia when treated with lower or, alternatively, higher doses of first-generation antipsychotics.[7,19,83–85] One review did investigate the effects of first-generation antipsychotics on suicide rates and demonstrated only a modest advantage in patients with schizophrenia.[86] With regard to dose, some of the retrospective studies reviewed utilized high doses of antipsychotic medication; however, a high dose may be indicative of disease severity or treatment resistance; both severe and refractory symptoms can lead to a higher risk of suicide among patients with schizophrenia. It has also been suggested that the inconsistencies observed may reflect an interaction of selection bias; for instance, more severely ill patients are receiving the higher doses and there may be more adverse effects (extrapyramidal symptoms) in patients receiving higher doses, which, in turn, contribute to an increased suicide risk. The higher rate of extrapyramidal adverse effects observable with higher doses can be associated with dysphoria, worsening subjective distress, agitation and suicidal behaviour.[87,88]
Some studies suggest a modest overall beneficial effect of first-generation antipsychotics on suicide risk.[86] Wilkinson and Bacon,[89] for example, found a lower likelihood of suicide attempts in patients receiving first-generation antipsychotic drugs. Furthermore, in a prospective case-control study, Johnson and colleagues[90] found more self-injurious behaviours following discontinuation of depot antipsychotics at 18 months when compared with patients who were maintained on the medication. This suggests that antipsychotics possess protective effects on suicidal behaviour in patients with schizophrenia.[90] Another study from Finland examining psychological autopsies in suicide victims who had schizophrenia supported the antisuicidal effects of first-generation antipsychotics.[91] In that study, most patients with schizophrenia who died by suicide either received inadequate doses of antipsychotic medication or were non-adherent with their prescribed medication.[91]
6.2 Second-Generation Antipsychotics
Compared with first-generation antipsychotic agents, the second-generation agents (and especially clozapine) appear to be more effective in reducing suicidal risk. Although there have been no prospective, randomized, controlled studies comparing the effect of first- and second-generation antipsychotic drugs on suicidal behaviour, one small retrospective study suggested that patients attempting suicide were more likely to be taking first-generation antipsychotic medication, while non-attempters were more likely to be taking second-generation antipsychotic agents.[34]
Studies examining various second-generation agents such as risperidone and olanzapine[92–96] have been mixed. One 5-year, retrospective, case-control study concluded that there was a decreased rate of suicide attempts with second-generation antipsychotic medications.[97] In this study, the index group consisted of patients who attempted suicide prior to admission; the control group comprised the next admission of a patient with schizophrenia (or schizoaffective disorder), matched for sex and age, who did not attempt suicide. Among 378 patients who attempted suicide (index group), 16.1% were exposed to second-generation antipsychotics while 37% of the control group were similarly exposed (p = 0.0001). This suggests a protective effect and yielded an odds ratio of 3.54 (95% CI 2.4, 5.3).
Two meta-analyses examined rates of suicide attempts or completed suicide from randomized, double-blind, placebo-controlled studies involving either risperidone, quetiapine or olanzapine treatment: no differences were noted.[98,99] At this point, there are no other systematic data available for the effects of second-generation antipsychotic agents, besides clozapine, on suicidal behaviours. Furthermore, all of these trials are limited by having a brief duration; in addition, patients with a high risk of suicidal behaviour were excluded from these trials.[98,99]
6.2.1 Clozapine
The best evidence supporting the use of second-generation agents to treat patients with schizophrenia and suicidal behaviour derives from studies focusing on clozapine. Clozapine was first reported to reduce rates of suicidality in a study among 88 treatment-refractory patients with schizophrenia or schizoaffective disorder.[100] In that trial, in the 2 years prior to initiation of clozapine therapy, 22 suicide attempts were reported, while in the 2 years after the start of clozapine treatment, the rate of suicide decreased by 88%.
Spivak et al.[101] conducted a 1-year study of treatment-refractory patients with schizophrenia, and noted that patients treated with clozapine rather than first-generation antipsychotics had fewer suicide attempts (p < 0.05) and decreased impulsivity (p < 0.05) and aggressiveness (p < 0.01). Walker et al.[102] performed a retrospective analysis of morbidity and mortality data for over 67 000 clozapine-treated patients using the Clozaril® National Registry (a database of all patients taking clozapine, which is maintained by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA), National Death Index and Social Security Administration databases. With this analysis, the authors demonstrated there was an 83% reduction in death by suicide among current clozapine users compared with those who were using clozapine and then stopped.[102]
It appears from this dataset[102] that the risk of death by suicide increased after clozapine discontinuation. Another study from the Clozaril® National Registry data indicated that there was a 0.0157% yearly incidence of completed suicides for clozapine-treated patients[103] versus a higher rate (0.4–0.8% per year) in other studies using antipsychotic agents.[40]
While most studies suggest that clozapine is important in reducing suicidal risk in patients with schizophrenia, one Veterans’ Administration study did not support a significant effect, although there was a trend favouring clozapine.[104] This investigation, however, did not match the comparison group on variables related to risk of suicide and follow-up. Furthermore, one-third of the sample received clozapine for <6 months, even though the follow-up period was 5–6 years.
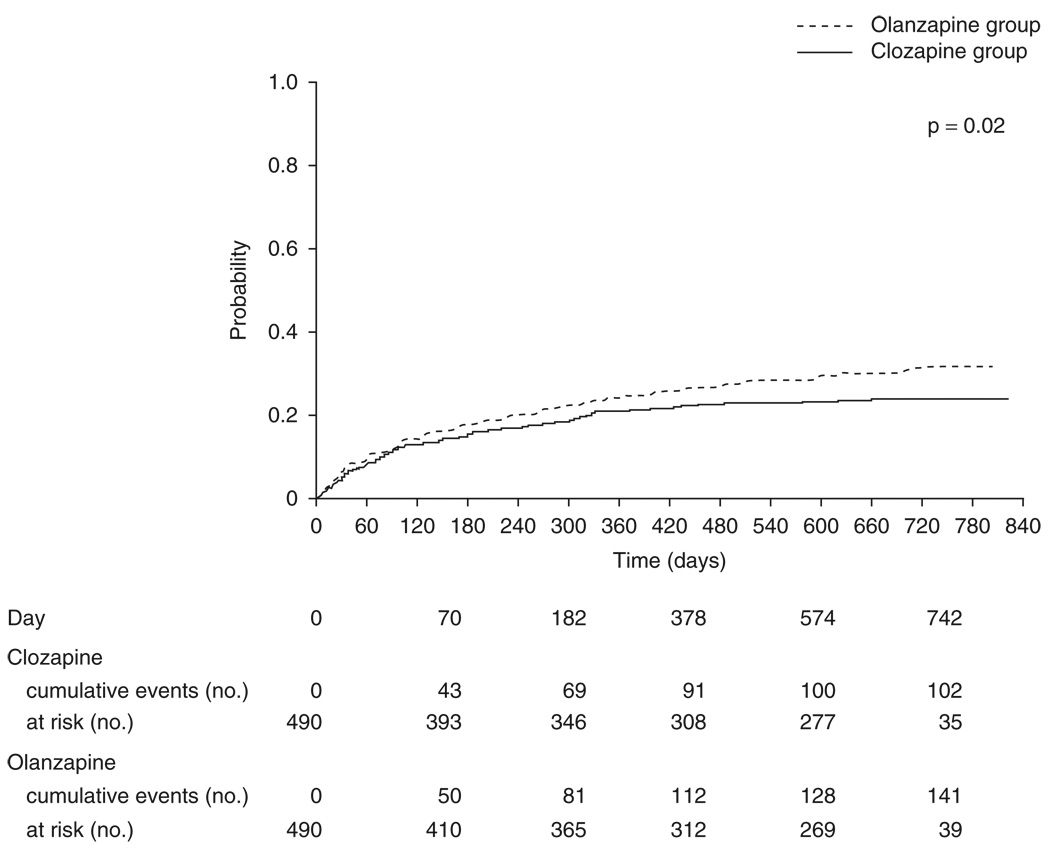
The InterSePT (International Suicide Prevention Trial) was an international, prospective, multicentre study that compared the effects of olanzapine with clozapine on suicidal behaviour over 2 years.[95] Using an open-label design, this trial recruited patients with schizophrenia or schizoaffective disorder at high risk for suicidal behaviour (having previous suicide attempts or current suicidal ideation). They were randomized to either clozapine (300–900 mg/day; n = 479) or olanzapine (10–20mg/day; n = 477). Subjects were followed at the same intervals in both groups; clinical ratings were performed by blinded raters. The outcomes of interest included any suicidal behaviour (suicide attempts or completions) or hospitalizations to prevent suicide, which were labelled type 1 events. Type 2 events included patients exhibiting worsening of suicidality from baseline, using the suicide severity subscale of the Clinical Global Impression (CGI) scale. The study also involved an independent suicide monitoring board comprising an international panel of experts in managing suicidal patients. The panel was blinded to treatment group assignment.[95]
Improved outcomes were observed with clozapine compared with olanzapine (figure 1). This included improvements in suicidal behaviour (HR 0.76; 95% CI 0.58, 0.97; p = 0.03), suicide attempts (p = 0.03), numbers of required hospitalizations (p = 0.05), interventions needed to prevent suicide (p = 0.01) and use of adjunctive antidepressants (p = 0.01), as well as anxiolytics (p = 0.03). Thus, the results of the study indicated that clozapine was associated with significantly fewer type 1 and type 2 events. Even though the olanzapine group received significantly more concurrent antidepressant and anxiolytic medications, treatment with clozapine reduced serious suicide attempts and hospitalizations to prevent suicide by 26%. The number needed to treat was 12 in favour of clozapine. InterSePT also demonstrated that the severity of accompanying parkinsonian symptoms was one of the four major factors accounting for most of the suicidal behaviour in this cohort.[105]
Fig. 1.
Results from the InterSePT (International Suicide Prevention Trial)[95] with Kaplan-Meier estimates of the probability of a suicide attempt or hospitalization to prevent suicide. The p-value refers to the Cox proportional hazards regression model. The model included treatment, number of previous suicide attempts, active substance or alcohol abuse, country, sex and age group at baseline. The model showed that there was a 26% reduction in risk for suicide attempt or hospitalization to prevent suicide for those randomized to clozapine vs those randomized to olanzapine. The hazard ratio was 0.74 (95% CI 0.57, 0.96) [reproduced from Meltzer et al.,[95] with permission from the Archives of General Psychiatry].
After InterSePT there were additional studies that focused on the use of clozapine to treat suicidal patients with schizophrenia. Modestin et al.[106] used a mirror-image, retrospective design with hospitalized patients and found an 88% decrease in the risk of suicide and a 12-fold decrease in the risk of suicidal behaviours during the period of continuous clozapine treatment. In patients who discontinued clozapine, the rate of suicidal behaviour increased to the baseline rate. This study also controlled for clinical contact. In 2005, Hennen and Baldessarini[107] examined studies that exhibited contrasting rates of suicides or attempts by psychotic patients treated with clozapine versus other agents. Among six studies, a random-effects meta-analysis determined that there was a lower risk of suicidal behaviours with clozapine relative to other treatments (risk ratio 3.3; 95% CI 1.7, 6.3; p < 0.0001). For completed suicides, the risk ratio was 2.9 (95% CI 1.5, 5.7; p = 0.002). The authors also concluded that the findings were not consistent quantitatively; furthermore, they commented that the only randomized trial available did not find a reduced risk of completed suicide and that additional randomized studies are needed.
Tiihonen et al.[108] performed an 11-year follow-up of mortality in patients with schizophrenia in Finland, called the FIN11 study. Cause-specific mortality in 66 881 patients was compared with the total population (5.2 million) from 1996 to 2006. This dataset was linked to the use of antipsychotic drugs and compared all-cause mortality of patients with schizophrenia in outpatient care with current or cumulative exposure to any antipsychotic drug versus no antipsychotic drugs. Also, the authors compared exposure to the six most frequently used antipsychotic drugs (including haloperidol, risperidone and quetiapine) with exposure to perphenazine. The gap in life expectancy between patients with schizophrenia and the general population did not widen between 1996 and 2006 (25 vs 22.5 years) despite an increase in the use of second-generation antipsychotics over this period. Compared with perphenazine, the highest risk for overall mortality was with quetiapine (adjusted HR 1.41; 95% CI 1.09, 1.82). The lowest risk was for clozapine (HR 0.74; 95% CI 0.60, 0.91; p = 0.0045 for clozapine vs perphenazine and p < 0.0001 for all other antipsychotic drugs).
Long-term cumulative exposure (i.e. 7–11 years) to any antipsychotic treatment was associated with lower mortality compared with no drug use (HR 0.81; 95% CI 0.77, 0.84). In patients who filled one or more prescriptions for an antipsychotic drug, there was an inverse relationship between mortality and duration of cumulative use (HR 0.991; 95% CI 0.985, 0.997). Thus, long-term treatment with antipsychotic drugs was associated with lower mortality compared with no antipsychotic use. Furthermore, second-generation drugs appear to be a heterogeneous group with regard to mortality: clozapine appears to be associated with lower mortality than any other antipsychotic.
De Hert et al.[109] commented on the Tiihonen et al.[108] study and noted a number of methodological problems: (i) incomplete reporting of data; (ii) questionable selection of drug groups and comparisons; (iii) lack of control for potential confounders; and (iv) exclusion of deaths occurring during hospitalization, which excluded 64% of the deaths. De Hert et al.[109] concluded that more well designed, prospective, mortality studies are clearly needed that involve a direct measurement of known relevant risk factors.
It appears that the use of clozapine in patients at high risk for suicide is beneficial.[110] The US FDA has now included suicidal behaviour in schizophrenia as an indication for clozapine treatment.[110,111] In addition, the American Psychiatric Association has now incorporated into their practice guidelines for the treatment of patients with schizophrenia[55] the recommendation that first-generation antipsychotics be used only in suicidal individuals who need depot antipsychotic medications. The Texas Medication Algorithm Project[112] recommends the use of clozapine in the suicidal patient.
Despite much of the indirect and direct evidence supporting the use of clozapine to treat suicidal patients with schizophrenia, clozapine remains under-utilized. In addition to the direct clinical benefits, it is also associated with fewer extrapyramidal symptoms and a lower risk of tar-dive dyskinesia than other antipsychotics. When looking solely at haematological adverse effects, it is estimated that one in 10 000 people treated with clozapine will die from agranulocytosis;[80] among patients at high risk for suicide, approximately 1 in 10–20 will die from suicide. Thus, the relative risk favours clozapine when comparing only the suicide risk with risk from agranulocytosis.[113] On the other hand, the need for long-term haematological monitoring clearly places a burden on both patient and caregiver. Although the frequency of monitoring has been decreased in the US to every other week after 6 months, this is still a burden. Clozapine also has the potential for other serious adverse effects such as seizures, weight gain, metabolic disturbances and sedation.[100] When making clinical decisions, providers need to take these risks into consideration.
Two other issues to consider when using clozapine are that it may take several months for the effects to become apparent and that a high dose may be required. The use of a high dose is associated with a higher risk of developing adverse effects.[114] In 2003, a panel of experts in suicide prevention held a consensus conference regarding the use of clozapine. They constructed an algorithm for the effective treatment of suicidal schizophrenic and schizoaffective patients.[115] However, this algorithm did not consider whether akathisia was present. This is important to consider, since it may lead not only to reduced quality of life but can also increase the suicide risk.[116]
6.3 Treating Depressive Symptoms in Patients with Schizophrenia
Treating depression in the suicidal patient with schizophrenia is important, since depressive symptoms are risk factors for suicidal behaviour in patients with schizophrenia.[73,117] Of course, when evaluating depression in patients with schizophrenia, consideration needs to be given to reversible causes of depressive symptoms, such as abuse of and withdrawal from illicit drugs or the dysphoria and akathisia secondary to antipsychotic drugs.[43] In addition, pharmacological approaches for the patient with schizophrenia and depressive symptoms are not the only options available; although there has been little research examining this, psychosocial interventions are also considered to be important ways to augment pharmacological treatments.[118]
Siris et al.[30] conducted an international survey of depression in schizophrenia, which used a 48-item questionnaire, comprising fixed-response questions and questions stimulated by case scenarios. They reported that practitioners prescribed antidepressants to 30% of inpatients and 43% of outpatients with schizophrenia as a way to augment antipsychotic treatment when treating depressive symptoms. Furthermore, selective serotonin reuptake inhibitors (SSRIs) were the most frequently prescribed antidepressants, and the preferred combination was a second-generation antipsychotic plus an SSRI. Interestingly, one-fourth of practicing psychiatrists rarely or never prescribed antidepressant medications in patients with schizophrenia, perhaps wary of the possibility of increasing psychotic symptoms or being otherwise uncertain about whether the benefits outweighed the risks.
American Psychiatric Association guidelines for the treatment of depression in patients with schizophrenia[55,110] recommend that clinicians use antidepressant medications for co-morbid syndromal major depressive disorder; this also applies to patients with schizoaffective disorder. The guidelines state that an antidepressant should be used when the major depressive disorder is severe, when it causes significant distress or if it interferes with functioning. In treating depressive symptoms in patients with schizophrenia, clinicians should maximize the dose and duration of antipsychotic medications first, especially if patients are taking second-generation antipsychotic medications, since second-generation agents may have antidepressant properties.[119] The clinician should also be alert to the possibility of pharmacokinetic interactions. As an example, clozapine and fluvoxamine can exhibit significant interactions.[43]
The 1999 Expert Treatment Guidelines for schizophrenia[120,121] recommended that, in patients with schizophrenia and postpsychotic depression, SSRIs should be first-line agents; if these are not helpful, it is recommended that clinicians try venlafaxine initially and then buproprion if venlafaxine is not helpful. These guidelines state that if an antidepressant is started then clinicians should try these agents for a duration of at least 6 months. Tricyclic antidepressants (TCAs) are other possible options. There are two randomized, placebo-controlled studies with imipramine as an agent to augment antipsychotics and these trials suggest that imipramine might be useful in the acute and maintenance treatment of postpsychotic depression.[122,123]
6.3.1 Use of Selective Serotonin Reuptake Inhibitors (SSRIs)
The evidence base supporting the use of antidepressants in treating depressive symptoms in patients with schizophrenia is strongest for SSRIs, and only very recently has there been evidence supporting the use of SSRIs as potential agents that can help treat suicidal symptoms. The published, peer-reviewed, double-blind, placebo-controlled trials examining SSRIs for the treatment of depressive symptoms in patients with schizophrenia are summarized in table I.
Table I.
Double-blind, placebo-controlled trials examining selective serotonin reuptake inhibitor (SSRI) augmentation of antipsychotic agents in patients with schizophreniaa (adapted from Kasckow and Zisook,[118] with permission from Adis, a Wolters Kluwer business [© Adis Data Information BV 2008. All rights reserved])
| Study | No. of patients |
Baseline depression | Medication | Duration (wk) |
Results vs placebo |
|---|---|---|---|---|---|
| Silver and Nassar[124] (1992) | 30 | Mean HAM-D score 7.7 | Fluvoxamine | 7 | No differences in HAM-D scores |
| Addington et al.[125] (2002) | 48 | Schizophrenia with major depression; HAM-D score 20.6; CDRS score 14.0 | Sertraline | 6 | No difference in CDRS or HAM-D scores |
| Buchanan et al.[126] (1996) | 33 | Mild to moderate depression; HAM-D score 12.6–13.3 | Fluoxetine augmentation of clozapine | 8 | No difference in HAM-D scores |
| Goff et al.[127] (1995) | 41 | Mild to moderate depressive symptoms; major depression excluded; HAM-D score 12.8–13.9 | Fluoxetine augmentation of depot antipsychotic | 6 | No difference in HAM-D scores |
| Spina et al.[128] (1994) | 30 | Mild to moderate depressive symptoms; HAM-D score 11.5–12.2 | Fluoxetine | 12 | HAM-D scores better in fluoxetine group |
| Salokangas et al.[129] (1996) | 90 | Not specified except that scores ≥4 on PANSS P7 (hostility), N4 (passive-apathetic withdrawal), G2 (anxiety) or G6 (depression) required for inclusion | Citalopram | 12 | No depression outcomes assessed; improvement in CGI and subjective well-being with citalopram based on a visual analogue scale |
| Vartiainen et al.[130] (1995) | 19 | Not specified | Citalopram | 24 | No depression outcomes assessed; lower frequency of aggressive incidents with citalopram |
| Zisook et al.[131,132] (2010, 2009) | 198 | HAM-D score >7 | Citalopram | 12 | Citalopram superior to placebo for depressive and suicidal symptoms |
All studies were double-blind and placebo-controlled except Vartiainen et al.[130] (1995), which was a double-blind, placebo, crossover design.
CDRS = Calgary Depression Rating Scale; CGI = Clinical Global Impression; HAM-D = Hamilton Rating Scale for Depression; PANSS = Positive and Negative Syndrome Scale.
Sertraline was used to treat patients with remitted schizophrenia and major depression; however, no benefit over placebo was demonstrated.[125] With fluoxetine, two studies also showed no benefit over placebo in the treatment of depressive symptoms.[126,127] However, another study with fluoxetine showed a slight and statistically significant decrease in depressive symptoms.[128] In addition, a study with fluvoxamine showed a positive effect on negative symptoms only.[124] One study found citalopram to have a salutary effect on severity of illness and subjective sense of wellbeing.[129] An additional citalopram trial with a crossover design[130] determined that citalopram decreased the frequency of aggressive incidents in 19 chronically violent patients with schizophrenia. All of these trials of SSRIs were limited by a small sample size, making interpretation of the results less clear. Furthermore, suicidal behaviour was not directly assessed in these trials.
The third trial of citalopram was a randomized controlled trial that examined the effects of citalopram in a much larger sample of patients with schizophrenia or schizoaffective disorder and sub-syndromal depressive symptoms.[131,132] 198 participants aged ≥40 years were randomized to receive citalopram or placebo. Augmentation with citalopram was significantly more effective than placebo in improving depression. The number needed to treat for improvement of depressive symptoms was six based on both the Hamilton Rating Scale for Depression (HAM-D) and Calgary Depression Rating Scale (CDRS) scores. No adverse events were more frequent in participants receiving citalopram.
In the same trial that examined patients with sub-syndromal depressive symptoms,[132] the investigators examined the response of suicidal behaviours to citalopram treatment.[131] Forty-seven percent of participants had made previous suicide attempts and 21% expressed suicidal ideation at baseline based on the CGI-Severity of Suicide (CGI-SS) scale. At 12 weeks, citalopram augmentation was associated with participants having significantly lower scores on the Beck Hopelessness Scale compared with placebo augmentation (4.21 vs 4.98; p < 0.05), and lower scores on the InterSePT Scale for Suicidal Ideation (ISST; 17.7% vs 38.7%; p < 0.005) and item 3 of the HAM-D, which assesses suicidality (14.4% vs 22.6%; p < 0.05).
When comparing the subset of participants who exhibited no suicidal ideation at baseline (n = 114) with those who did have such ideation at baseline (n = 55), there were no significant differences between the two groups with regard to ‘emergent’ ideation at the end of treatment. However, among the participants with suicidal ideation at baseline, fewer participants treated with citalopram augmentation had endpoint suicidal ideation on the ISST (28.6% vs 66.7%; p < 0.05). In addition, 75% of depression responders who exhibited baseline suicidal ideation exhibited no suicidal ideation at the final visit on the ISST compared with 31.4% of non-responders (p < 0.05). Using the CGI-SS, 84% of depression responders had no endpoint suicidal ideation compared with 31.3% of the non-responders (p < 0.05). In those participants with baseline suicidal ideation, antidepressant treatment reduced suicidal ideation, especially in those whose depressive symptoms responded to treatment. The study suggests there may be a possible anti-suicidal role for antidepressant medication in this population of patients.[131]
7. Conclusions
The treatment of suicidal patients with a diagnosis of schizophrenia involves careful assessment of risk factors and formulation of a comprehensive safety plan involving biopsychosocial interventions. This includes building patients’ social support networks and teaching positive coping skills. Furthermore, both psychosocial and pharmacological approaches applied in the long term should help minimize the risk of suicide. There is some suggestion that first-generation antipsychotics may be protective, but perhaps not to the extent of some second-generation antipsychotics, especially clozapine. However, the use of clozapine must be carefully considered in light of its potential adverse event burden. Finally, given that depressive symptoms appear to be a risk factor for suicide, antidepressant augmentation in patients with syndromal or sub-syndromal depression is another promising strategy.
Acknowledgements
Supported by MH6398 (SZ, JK), a VISN 4 CPPF grant (JK) and a grant from the American Foundation for Suicide Prevention (JK), the VISN 4 and VISN 22 MIRECC and the University of California, San Diego Center for Community-Based Research in Older People with Psychoses. The contents do not represent the views of the Department of Veterans Affairs of the US government.
Sidney Zisook, MD, has received research support from Aspect Medical and PamLab and speaker’s honoraria from Forest Pharmaceuticals, Inc. and GlaxoSmithKline. John Kasckow, MD, PhD, has received grant support as well as honoraria for speaking and consultation from Forest, AstraZeneca, Bristol Meyers Squibb, Pfizer, Johnson & Johnson, Solvay and Eli Lilly.
Footnotes
Ms Felmet has no conflicts of interest to declare.
References
- 1.Allebeck P, Wistedt B. Mortality in schizophrenia: a ten-year follow-up based on the Stockholm County inpatient register. Arch Gen Psychiatry. 1986;43:650–653. doi: 10.1001/archpsyc.1986.01800070036005. [DOI] [PubMed] [Google Scholar]
- 2.Montross L, Zisook S, Kasckow JW. Suicide among patients with schizophrenia: a consideration of risk and protective factors. Ann Clin Psychiatry. 2005;17:173–182. doi: 10.1080/10401230591002156. [DOI] [PubMed] [Google Scholar]
- 3.Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry. 1998;172:35–37. doi: 10.1192/bjp.172.1.35. [DOI] [PubMed] [Google Scholar]
- 4.Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 5.Nasrallah HA, Smeltzer DJ. Contemporary diagnosis and management of the patient with schizophrenia. Newton (PA): Handbooks in Health Care; 2002. [Google Scholar]
- 6.Breier A, Schreiber JL, Dyer J, et al. National Institute of Mental Health longitudinal study of chronic schizophrenia: prognosis and predictors of outcome. Arch Gen Psychiatry. 1991;48:239–246. doi: 10.1001/archpsyc.1991.01810270051007. [DOI] [PubMed] [Google Scholar]
- 7.Roy A. Depression, attempted suicide, and suicide in patients with chronic schizophrenia. Psychiatr Clin North Am. 1986;9:193–206. [PubMed] [Google Scholar]
- 8.Drake RE, Gates C, Whitaker A, et al. Suicide among schizophrenics: a review. Compr Psychiatry. 1985;26:90–100. doi: 10.1016/0010-440x(85)90053-7. [DOI] [PubMed] [Google Scholar]
- 9.Miles CP. Conditions predisposing to suicide: a review. J Nerv Ment Dis. 1977;164:231–246. doi: 10.1097/00005053-197704000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Meltzer HY. Suicide and schizophrenia: clozapine and the InterSePT study. J Clin Psychiatry. 1999;60:47–50. [PubMed] [Google Scholar]
- 11.Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005;62:247–253. doi: 10.1001/archpsyc.62.3.247. [DOI] [PubMed] [Google Scholar]
- 12.Heila H, Isometsa ET, Henriksson MM, et al. Suicide and schizophrenia: a nationwide psychological autopsy study on age- and sex-specific clinical characteristics of 92 suicide victims with schizophrenia. Am J Psychiatry. 1997;154:1235–1242. doi: 10.1176/ajp.154.9.1235. [DOI] [PubMed] [Google Scholar]
- 13.Kreyenbuhl JA, Kelly DL, Conley RR. Circumstances of suicide among individuals with schizophrenia. Schizophr Res. 2002;58:253–261. doi: 10.1016/s0920-9964(01)00379-6. [DOI] [PubMed] [Google Scholar]
- 14.Allebeck P, Varla A, Kristjansson E, et al. Risk factors for suicide among patients with schizophrenia. Acta Psychiatr Scand. 1987;76:414–419. doi: 10.1111/j.1600-0447.1987.tb05626.x. [DOI] [PubMed] [Google Scholar]
- 15.Caldwell CB, Gottesman II. Schizophrenia: a high risk factor for suicide: clues to risk reduction. Suicide Life Threat Behav. 1992;22:479–493. [PubMed] [Google Scholar]
- 16.Roy A. Suicide in schizophrenia. Int Rev Psychiatry. 1992;4:205–209. [Google Scholar]
- 17.Modestin J, Zarro I, Waldvogel D. A study of suicide in schizophrenic in-patients. Br J Psychiatry. 1992;160:398–401. doi: 10.1192/bjp.160.3.398. [DOI] [PubMed] [Google Scholar]
- 18.Cannon M, Buckley P, Larkin C. Suicide in schizophrenia. Irish J Psychol Med. 1991;8:19–21. [Google Scholar]
- 19.Cheng KK, Leung CM, Lo W, et al. Risk factors of suicide among schizophrenics. Acta Psychiatr Scand. 1990;81:220–224. doi: 10.1111/j.1600-0447.1990.tb06484.x. [DOI] [PubMed] [Google Scholar]
- 20.Tandon R, Jibson MD. Suicidal behavior in schizophrenia: diagnosis, neurobiology, and treatment implications. Curr Opin Psychiatry. 2003;16:193–197. [Google Scholar]
- 21.Cotton PG, Drake RE, Gates C. Critical treatment issues in suicide among schizophrenics. Hosp Community Psychiatry. 1985;36:534–536. doi: 10.1176/ps.36.5.534. [DOI] [PubMed] [Google Scholar]
- 22.Pinikahana J, Happell B, Keks NA. Suicide and schizophrenia: a review of literature for the decade (1990–1999) and implications for mental health nursing. Issues Ment Health Nurs. 2003;24:27–43. doi: 10.1080/01612840305305. [DOI] [PubMed] [Google Scholar]
- 23.De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res. 2001;47:127–134. doi: 10.1016/s0920-9964(00)00003-7. [DOI] [PubMed] [Google Scholar]
- 24.Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15:127–135. doi: 10.1177/026988110101500209. [DOI] [PubMed] [Google Scholar]
- 25.Raymont V. Suicide in schizophrenia: how can research influence training and clinical practice? Psychiatr Bull. 2001;25:46–50. [Google Scholar]
- 26.Roy A. Suicide in chronic schizophrenia. Br J Psychiatry. 1982;141:171–177. doi: 10.1192/bjp.141.2.171. [DOI] [PubMed] [Google Scholar]
- 27.Gut-Fayand A, Dervaux A, Olie JP, et al. Substance abuse and suicidality in schizophrenia: a common risk factor linked to impulsivity. Psychiatry Res. 2001;102:65–72. doi: 10.1016/s0165-1781(01)00250-5. [DOI] [PubMed] [Google Scholar]
- 28.Rossau CD, Mortensen PB. Risk factors for suicide in patients with schizophrenia: nested case-control study. Br J Psychiatry. 1997;171:355–359. doi: 10.1192/bjp.171.4.355. [DOI] [PubMed] [Google Scholar]
- 29.McGlashan TH, Carpenter WT. Postpsychotic depression in schizophrenia. Arch Gen Psychiatry. 1976;3:231–239. doi: 10.1001/archpsyc.1976.01770020065011. [DOI] [PubMed] [Google Scholar]
- 30.Siris SG, Addington D, Azorin JM, et al. Depression in schizophrenia: recognition and management in the USA. Schizophr Res. 2001;47:185–197. doi: 10.1016/s0920-9964(00)00135-3. [DOI] [PubMed] [Google Scholar]
- 31.Pompili M, Mancinelli I, Tatarelli R. Suicide and schizophrenia. Psychiatr Serv. 2003;54:747–748. doi: 10.1176/appi.ps.54.5.747. [DOI] [PubMed] [Google Scholar]
- 32.Henriksson MM, Marttunen MJ, Isometsa ET, et al. Mental disorders in elderly suicide. Int Psychogeriatr. 1995;7:275–286. doi: 10.1017/s1041610295002031. [DOI] [PubMed] [Google Scholar]
- 33.Conwell Y, Duberstein PR, Cox C, et al. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153:1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 34.Altamura AC, Bassetti R, Bignotti S, et al. Clinical variables related to suicide attempts in schizophrenic patients: a retrospective study. Schizophr Res. 2003;60:47–55. doi: 10.1016/s0920-9964(02)00164-0. [DOI] [PubMed] [Google Scholar]
- 35.Breier A, Astrachan BM. Characterization of schizophrenic patients who commit suicide. Am J Psychiatry. 1984;141:206–209. doi: 10.1176/ajp.141.2.206. [DOI] [PubMed] [Google Scholar]
- 36.Cohen LJ, Test MA, Brown RL. Suicide and schizophrenia: data from a prospective community treatment study. Am J Psychiatry. 1990;147:602–607. doi: 10.1176/ajp.147.5.602. [DOI] [PubMed] [Google Scholar]
- 37.Andia AM, Zisook S, Heaton RK, et al. Gender differences in schizophrenia. J Nerv Ment Dis. 1995;183:522–528. doi: 10.1097/00005053-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Copas JB, Robin A. Suicide in psychiatric in-patients. Br J Psychiatry. 1982;141:503–511. doi: 10.1192/bjp.141.5.503. [DOI] [PubMed] [Google Scholar]
- 39.Black D, Winokur G, Warrach G. Suicide in schizophrenia: the Iowa Linkage Study. J Clin Psychiatry. 1985;46:14–17. [PubMed] [Google Scholar]
- 40.Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull. 1990;16:571–589. doi: 10.1093/schbul/16.4.571. [DOI] [PubMed] [Google Scholar]
- 41.Evenson RC, Wood JB, Nuttall EA, et al. Suicide rates among public mental health patients. Acta Psychiatr Scand. 1982;66:254–264. doi: 10.1111/j.1600-0447.1982.tb00933.x. [DOI] [PubMed] [Google Scholar]
- 42.Waern M, Runeson BS, Allebeck P, et al. Mental disorder in elderly suicides: a case-control study. Am J Psychiatry. 2002;159:450–455. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- 43.Mamo D. Caring for the suicidal patient: an evidence-based approach. Can J Psychiatry. 2007;52 Suppl. 1:59S–70S. [Google Scholar]
- 44.Nordentoft M. Prevention of suicide and attempted suicide in Denmark: epidemiological studies of suicide and intervention studies in selected risk groups. Dan Med Bull. 2007;54:306–369. [PubMed] [Google Scholar]
- 45.Nordentoft M, Jeppesen P, Abel M, et al. OPUS study: suicidal behaviour, suicidal ideation and hopelessness among patients with first-episode psychosis: one-year follow-up of a randomised controlled trial. Br J Psychiatry. 2002;43 Suppl.:s98–s106. doi: 10.1192/bjp.181.43.s98. [DOI] [PubMed] [Google Scholar]
- 46.Pompili M, Mancinelli I, Girardi P, et al. Nursing schizophrenic patients who are at risk of suicide. J Psychiatr Ment Health Nurs. 2003;10:622–624. doi: 10.1046/j.1365-2850.2003.00658.x. [DOI] [PubMed] [Google Scholar]
- 47.Farberow N, Shneidman E, Neuringer C. Case history and hospitalization factors in suicides of neuropsychiatric hospital patients. J Nerv Ment Dis. 1966;142:32–44. doi: 10.1097/00005053-196601000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Morgan HG, Priest P. Assessment of suicide risk in psychiatric in-patients. Br J Psychiatry. 1984;145:467–469. doi: 10.1192/bjp.145.5.467. [DOI] [PubMed] [Google Scholar]
- 49.Morgan HG, Priest P. Suicide and other unexpected deaths among psychiatric in-patients: the Bristol confidential inquiry. Br J Psychiatry. 1991;158:368–374. doi: 10.1192/bjp.158.3.368. [DOI] [PubMed] [Google Scholar]
- 50.Crammer JL. The special characteristics of suicide in hospital in-patients. Br J Psychiatry. 1984;145:460–463. doi: 10.1192/bjp.145.5.460. [DOI] [PubMed] [Google Scholar]
- 51.Goh SE, Salmons PH, Whittington RM. Hospital suicides: are there preventable factors? Profile of psychiatric hospital suicide. Br J Psychiatry. 1989;154:247–249. doi: 10.1192/bjp.154.2.247. [DOI] [PubMed] [Google Scholar]
- 52.Saarinen PI, Lehtonen J, Lonnqvist J. Suicide risk in schizophrenia: an analysis of 17 consecutive suicides. Schizophr Bull. 1999;25:533–542. doi: 10.1093/oxfordjournals.schbul.a033399. [DOI] [PubMed] [Google Scholar]
- 53.De Leo D, Spathonis K. Do psychosocial and pharmacological interventions reduce suicide in schizophrenia and schizophrenia spectrum disorders? Arch Suicide Res. 2003;7:353–374. [Google Scholar]
- 54.Lauriello J, Lenroot R, Bustillo JR. Maximizing the synergy between pharmacotherapy and psychosocial therapies for schizophrenia. Psychiatr Clin North Am. 2003;26:191–211. doi: 10.1016/s0193-953x(02)00017-5. [DOI] [PubMed] [Google Scholar]
- 55.Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl.):1–56. [PubMed] [Google Scholar]
- 56.Lenroot R, Bustillo JR, Lauriello J, et al. Integrated treatment of schizophrenia. Psychiatr Serv. 2003;54:1499–1507. doi: 10.1176/appi.ps.54.11.1499. [DOI] [PubMed] [Google Scholar]
- 57.Grawe RW, Falloon IR, Widen JH, et al. Two years of continued early treatment for recent-onset schizophrenia: a randomised controlled study. Acta Psychiatr Scand. 2006;114:328–336. doi: 10.1111/j.1600-0447.2006.00799.x. [DOI] [PubMed] [Google Scholar]
- 58.Turkington D, Kingdon D, Turner T. Effectiveness of a brief cognitive-behavioural therapy intervention in the treatment of schizophrenia. Br J Psychiatry. 2002;180:523–527. doi: 10.1192/bjp.180.6.523. [DOI] [PubMed] [Google Scholar]
- 59.Tarrier N, Haddock G, Lewis S, et al. Suicide behaviour over 18 months in recent onset schizophrenic patients: the effects of CBT. Schizophr Res. 2006;83:15–27. doi: 10.1016/j.schres.2005.12.846. [DOI] [PubMed] [Google Scholar]
- 60.Bateman K, Hansen L, Turkington D, et al. Cognitive behavioral therapy reduces suicidal ideation in schizophrenia: results from a randomized controlled trial. Suicide Life Threat Behav. 2007;37:284–290. doi: 10.1521/suli.2007.37.3.284. [DOI] [PubMed] [Google Scholar]
- 61.Ponizovsky AM, Grinshpoon A, Levav I, et al. Life satisfaction and suicidal attempts among persons with schizophrenia. Compr Psychiatry. 2003;44:442–447. doi: 10.1016/S0010-440X(03)00146-9. [DOI] [PubMed] [Google Scholar]
- 62.Nyman AK, Jonsson H. Patterns of self-destructive behaviour in schizophrenia. Acta Psychiatr Scand. 1986;73:252–262. doi: 10.1111/j.1600-0447.1986.tb02682.x. [DOI] [PubMed] [Google Scholar]
- 63.Drake RE, Bartels SJ, Torrey WC. Suicide in schizophrenia: clinical approaches. In: Williams R, Dalby JT, editors. Depression in schizophrenia. New York: Plenum Press; 1989. pp. 153–169. [Google Scholar]
- 64.Beck AT, Steer RA, Kovacs M, et al. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–563. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 65.Mueser KT, Berenbaum H. Psychodynamic treatment of schizophrenia: is there a future? Psychol Med. 1990;20:253–262. doi: 10.1017/s003329170001758x. [DOI] [PubMed] [Google Scholar]
- 66.Harkavy-Friedman JM, Nelson EA. Assessment and intervention for the suicidal patient with schizophrenia. Psychiatr Q. 1997;68:361–375. doi: 10.1023/a:1025447115067. [DOI] [PubMed] [Google Scholar]
- 67.Drake RE, Cotton PG. Depression, hopelessness and suicide in chronic schizophrenia. Br J Psychiatry. 1986;148:554–559. doi: 10.1192/bjp.148.5.554. [DOI] [PubMed] [Google Scholar]
- 68.Restifo K, Harkavy-Friedman JM, Shrout PE. Suicidal behavior in schizophrenia: a test of the demoralization hypothesis. J Nerv Ment Dis. 2009;197:147–153. doi: 10.1097/NMD.0b013e318199f452. [DOI] [PubMed] [Google Scholar]
- 69.Haghighat R. A discourse for hope: on defenses against suicide in people with schizophrenia. New York: Nova Science Publishers; 2007. pp. 189–213. [Google Scholar]
- 70.Lee PW, Lieh-Mak F, Wong MC, et al. The 15-year outcome of Chinese patients with schizophrenia in Hong Kong. Can J Psychiatry. 1998;43:706–713. doi: 10.1177/070674379804300705. [DOI] [PubMed] [Google Scholar]
- 71.Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J. 1999;318:1235–1239. doi: 10.1136/bmj.318.7193.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schooler NR. Relapse prevention and recovery in the treatment of schizophrenia. J Clin Psychiatry. 2006;67 Suppl. 5:19–23. [PubMed] [Google Scholar]
- 73.Hawton K, Sutton L, Haw C, et al. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9–20. doi: 10.1192/bjp.187.1.9. [DOI] [PubMed] [Google Scholar]
- 74.Ward A, Ishak K, Proskorovsky I, et al. Compliance with refilling prescriptions for atypical antipsychotic agents and its association with the risks for hospitalization, suicide, and death in patients with schizophrenia in Quebec and Saskatchewan: a retrospective database study. Clin Ther. 2006;28:1912–1921. doi: 10.1016/j.clinthera.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 75.Bustillo J, Lauriello J, Horan W, et al. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158:163–175. doi: 10.1176/appi.ajp.158.2.163. [DOI] [PubMed] [Google Scholar]
- 76.Cipriani A, Pretty H, Hawton K, et al. Lithium in the prevention of suicidal behaviour and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. Am J Psychiatry. 2005;162:1805–1819. doi: 10.1176/appi.ajp.162.10.1805. [DOI] [PubMed] [Google Scholar]
- 77.Leucht S, Kissling W, McGrath J. Lithium for schizophrenia. Cochrane Database Syst Rev. 2007;(3):CD003834. doi: 10.1002/14651858.CD003834.pub2. [DOI] [PubMed] [Google Scholar]
- 78.Winokur G, Tsuang M. The Iowa 500: suicide in mania, depression, and schizophrenia. Am J Psychiatry. 1975 Jun;132:650–651. doi: 10.1176/ajp.132.6.650. [DOI] [PubMed] [Google Scholar]
- 79.Axelsson R, Lagerkvist-Briggs M. Factors predicting suicide in psychotic patients. Eur Arch Psychiatry Clin Neurosci. 1992;241:259–266. doi: 10.1007/BF02195974. [DOI] [PubMed] [Google Scholar]
- 80.Meltzer HY. Treatment of suicidality in schizophrenia. Ann N Y Acad Sci. 2001;932:44–58. doi: 10.1111/j.1749-6632.2001.tb05797.x. discussion 58–60. [DOI] [PubMed] [Google Scholar]
- 81.Ernst CL, Goldberg JF. Antisuicide properties of psychotropic drugs: a critical review. Harv Rev Psychiatry. 2004;12:14–41. doi: 10.1080/10673220490425924. [DOI] [PubMed] [Google Scholar]
- 82.Cohen S, Leonard CV, Farberow NL, et al. Tranquilizers and suicide in the schizophrenic patient. Arch Gen Psychiatry. 1964;11:312–321. doi: 10.1001/archpsyc.1964.01720270084010. [DOI] [PubMed] [Google Scholar]
- 83.Warnes H. Suicide in schizophrenics. Dis Nerv Syst. 1968;29 Suppl.:35–40. [PubMed] [Google Scholar]
- 84.Taiminen TJ, Kujari H. Antipsychotic medication and suicide risk among schizophrenic and paranoid inpatients: a controlled retrospective study. Acta Psychiatr Scand. 1994;90:247–251. doi: 10.1111/j.1600-0447.1994.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 85.Taiminen TJ. Effect of psychopharmacotherapy on suicide risk in psychiatric inpatients. Acta Psychiatr Scand. 1993;87:45–47. doi: 10.1111/j.1600-0447.1993.tb03328.x. [DOI] [PubMed] [Google Scholar]
- 86.Palmer DD, Henter ID, Wyatt RJ. Do antipsychotic medications decrease the risk of suicide in patients with schizophrenia? J Clin Psychiatry. 1999;60 Suppl. 2:100–103. discussion 111–6. [PubMed] [Google Scholar]
- 87.Van Putten T, May RP. Akinetic depression in schizophrenia. Arch Gen Psychiatry. 1978;35:1101–1107. doi: 10.1001/archpsyc.1978.01770330075006. [DOI] [PubMed] [Google Scholar]
- 88.Cem Atbaşoglu E, Schultz SK, Andreasen NC. The relationship of akathisia with suicidality and depersonalization among patients with schizophrenia. J Neuropsychiatry Clin Neurosci. 2001;13:336–341. doi: 10.1176/jnp.13.3.336. [DOI] [PubMed] [Google Scholar]
- 89.Wilkinson G, Bacon NA. A clinical and epidemiological survey of parasuicide and suicide in Edinburgh schizophrenics. Psychol Med. 1984;14:899–912. doi: 10.1017/s0033291700019863. [DOI] [PubMed] [Google Scholar]
- 90.Johnson DA, Pasterski G, Ludlow JM, et al. The discontinuance of maintenance neuroleptic therapy in chronic schizophrenic patients: drug and social consequences. Acta Psychiatr Scand. 1983;67:339–352. doi: 10.1111/j.1600-0447.1983.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 91.Heila H, Isometsa ET, Henriksson MM, et al. Suicide victims with schizophrenia in different treatment phases and adequacy of antipsychotic medication. J Clin Psychiatry. 1999;60:200–208. doi: 10.4088/jcp.v60n0311. [DOI] [PubMed] [Google Scholar]
- 92.Tran PV, Hamilton SH, Kuntz AJ, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol. 1997;17:407–418. doi: 10.1097/00004714-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 93.Müller-Siecheneder F, Müller MJ, Hillert A, et al. Risperidone versus haloperidol and amitriptyline in the treatment of patients with a combined psychotic and depressive syndrome. J Clin Psychopharmacol. 1998;18:111–120. doi: 10.1097/00004714-199804000-00003. [DOI] [PubMed] [Google Scholar]
- 94.Beasley CM, Jr, Hamilton SH, Crawford AM, et al. Olanzapine versus haloperidol: acute phase results of the international double-blind olanzapine trial. Eur Neuropsychopharmacol. 1997;7:125–137. doi: 10.1016/s0924-977x(96)00392-6. [DOI] [PubMed] [Google Scholar]
- 95.Meltzer HY, Alphs L, Green AI, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT) Arch Gen Psychiatry. 2003 Jan;60(1):82–91. doi: 10.1001/archpsyc.60.1.82. [DOI] [PubMed] [Google Scholar]
- 96.Meltzer HY, Baldessarini RJ. Reducing the risk for suicide in schizophrenia and affective disorders. J Clin Psychiatry. 2003;64:1122–1129. doi: 10.4088/jcp.v64n0920. [DOI] [PubMed] [Google Scholar]
- 97.Barak Y, Mirecki I, Knobler HY, et al. Suicidality and second generation antipsychotics in schizophrenia patients: a case-controlled retrospective study during a 5-year period. Psychopharmacology (Berl) 2004;175:215–219. doi: 10.1007/s00213-004-1801-2. [DOI] [PubMed] [Google Scholar]
- 98.Khan A, Khan SR, Leventhal RM, et al. Symptom reduction and suicide risk among patients treated with placebo in antipsychotic clinical trials: an analysis of the Food and Drug Administration database. Am J Psychiatry. 2001;158:1449–1454. doi: 10.1176/appi.ajp.158.9.1449. [DOI] [PubMed] [Google Scholar]
- 99.Storosum JG, van Zwieten BJ, Wohlfarth T, et al. Suicide risk in placebo vs active treatment in placebo-controlled trials for schizophrenia. Arch Gen Psychiatry. 2003;60:365–368. doi: 10.1001/archpsyc.60.4.365. [DOI] [PubMed] [Google Scholar]
- 100.Meltzer HY, Okayli G. Reduction of suicidality during clozapine treatment of neuroleptic-resistant schizophrenia: impact on risk-benefit assessment. Am J Psychiatry. 1995;152:183–190. doi: 10.1176/ajp.152.2.183. [DOI] [PubMed] [Google Scholar]
- 101.Spivak B, Roitman S, Vered Y, et al. Diminished suicidal and aggressive behavior, high plasma norepinephrine levels, and serum triglyceride levels in chronic neuroleptic-resistant schizophrenic patients maintained on clozapine. Clin Neuropharmacol. 1998;21:245–250. [PubMed] [Google Scholar]
- 102.Walker AM, Lanza LL, Arellano F, et al. Mortality in current and former users of clozapine. Epidemiology. 1997;8:671–677. doi: 10.1097/00001648-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 103.Reid WH, Mason M, Hogan T. Suicide prevention effects associated with clozapine therapy in schizophrenia and schizoaffective disorder. Psychiatr Serv. 1998;49:1029–1033. doi: 10.1176/ps.49.8.1029. [DOI] [PubMed] [Google Scholar]
- 104.Sernyak M, Desai R, Stolar M, et al. Impact of clozapine on completed suicide. Am J Psychiatry. 2001;158:931–937. doi: 10.1176/appi.ajp.158.6.931. [DOI] [PubMed] [Google Scholar]
- 105.Potkin SG, Alphs L, Hsu C, et al. Predicting suicidal risk in schizophrenic and schizoaffective patients in a prospective two-year trial. Biol Psychiatry. 2003;54:444–452. doi: 10.1016/s0006-3223(03)00178-1. [DOI] [PubMed] [Google Scholar]
- 106.Modestin J, Dal Pian D, Agarwalla P. Clozapine diminishes suicidal behavior: a retrospective evaluation of clinical records. J Clin Psychiatry. 2005;66:534–538. doi: 10.4088/jcp.v66n0418. [DOI] [PubMed] [Google Scholar]
- 107.Hennen J, Baldessarini RJ. Suicidal risk during treatment with clozapine: a meta-analysis. Schizophr Res. 2005;73:139–145. doi: 10.1016/j.schres.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 108.Tiihonen T, Lönnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study) Lancet. 2009;374:620–627. doi: 10.1016/S0140-6736(09)60742-X. [DOI] [PubMed] [Google Scholar]
- 109.De Hert M, Correll C, Cohen D. Do antipsychotic medications reduce or increase mortality in schizophrenia? A critical appraisal of the FIN-11 study. Schizophr Res. 2010;117:68–74. doi: 10.1016/j.schres.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 110.American Psychiatric Association practice guidelines for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160 Suppl. 11:1–60. [PubMed] [Google Scholar]
- 111.Kerwin R. Preventing suicide [letter] Br J Psychiatry. 2003 Apr;182:366. doi: 10.1192/bjp.182.4.366. [DOI] [PubMed] [Google Scholar]
- 112.Miller AL, Hall CS, Buchanan RW, et al. The Texas medication algorithm project antipsychotic algorithm for schizophrenia: 2003 update. J Clin Psychiatry. 2004;65:500–508. doi: 10.4088/jcp.v65n0408. [DOI] [PubMed] [Google Scholar]
- 113.Meltzer H. Suicide in schizophrenia: clozapine, the adoption of evidence-based medicine [commentary] J Clin Psychiatry. 2005;66:4. doi: 10.4088/jcp.v66n0417. [DOI] [PubMed] [Google Scholar]
- 114.Meltzer HY. Treatment-resistant schizophrenia: the role of clozapine. Curr Med Res Opin. 1997;14:1–20. doi: 10.1185/03007999709113338. [DOI] [PubMed] [Google Scholar]
- 115.Meltzer HY, Conley RR, De Leo D, et al. Intervention strategies for suicidality [audiograph] J Clin Psychiatry. 2003;6:1–16. [Google Scholar]
- 116.Roy A, Pompili M. Management of schizophrenia with suicide risk. Psychiatr Clin N Am. 2009;32:863–883. doi: 10.1016/j.psc.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 117.Kasckow J, Fellows I, Golshan S, et al. Treatment of sub-syndromal depressive symptoms in middle-age and older patients with schizophrenia: effect of age on response. Am J Geriatr Psychiatry. 2010;18:853–857. doi: 10.1097/JGP.0b013e3181dba12f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kasckow JW, Zisook S. Co-occurring depressive symptoms in the older patient with schizophrenia. Drugs Aging. 2008;25:631–647. doi: 10.2165/00002512-200825080-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Furtado VA, Srihari V, Kumar A. Atypical antipsychotics for people with both schizophrenia and depression. Schizophr Bull. 2009;35:297–298. doi: 10.1093/schbul/sbn188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Treatment of schizophrenia 1999: the expert consensus guideline series. J Clin Psychiatry. 1999;60 Suppl. 11:3–80. [PubMed] [Google Scholar]
- 121.Kane J, Leucht S, Carpenter D. The expert consensus guideline series: optimizing pharmacologic treatment of psychotic disorders. Introduction: methods, commentary, and summary. J Clin Psychiatry. 2003;64 Suppl. 12:5–19. [PubMed] [Google Scholar]
- 122.Siris SG, Morgan V, Fagerstrom R, et al. Adjunctive imipramine in the treatment of postpsychotic depression: a controlled trial. Arch Gen Psychiatry. 1987;44:533–539. doi: 10.1001/archpsyc.1987.01800180043008. [DOI] [PubMed] [Google Scholar]
- 123.Siris SG, Bermanzohn P, Mason SE, et al. Maintenance imipramine therapy for secondary depression in schizophrenia: a controlled trial. Arch Gen Psychiatry. 1994;51:109–115. doi: 10.1001/archpsyc.1994.03950020033003. [DOI] [PubMed] [Google Scholar]
- 124.Silver H, Nassar A. Fluvoxamine improves negative symptoms in treated chronic schizophrenia: an add-on double-blind, placebo-controlled study. Biol Psychiatry. 1992 Apr 1;31(7):698–704. doi: 10.1016/0006-3223(92)90279-9. [DOI] [PubMed] [Google Scholar]
- 125.Addington D, Addington J, Patten S, et al. Double-blind, placebo-controlled comparison of the efficacy of sertraline as treatment for a major depressive episode in patients with remitted schizophrenia. Clin Psychopharmacol. 2002;22:20–25. doi: 10.1097/00004714-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 126.Buchanan RW, Kirkpatrick B, Bryant N, et al. Fluoxetine augmentation of clozapine treatment in patients with schizophrenia. Am J Psychiatry. 1996;153:1625–1627. doi: 10.1176/ajp.153.12.1625. [DOI] [PubMed] [Google Scholar]
- 127.Goff DC, Midha KK, Sarid-Segal O, et al. A placebo-controlled trial of fluoxetine added to neuroleptic in patients with schizophrenia. Psychopharmacology. 1995;117:417–423. doi: 10.1007/BF02246213. [DOI] [PubMed] [Google Scholar]
- 128.Spina E, De Domenico P, Ruello C, et al. Adjunctive fluoxetine in the treatment of negative symptoms in chronic schizophrenia patients. Int Clin Psychopharmacol. 1994;9:281–285. doi: 10.1097/00004850-199400940-00007. [DOI] [PubMed] [Google Scholar]
- 129.Salokangas RK, Saarijarvi S, Taiminen T, et al. Citalopram as an adjuvant in chronic schizophrenia: a double-blind placebo-controlled study. Acta Psychiatr Scand. 1996;94:175–180. doi: 10.1111/j.1600-0447.1996.tb09844.x. [DOI] [PubMed] [Google Scholar]
- 130.Vartiainen H, Tiihonen J, Putkonen A, et al. Citalopram, a selective serotonin reuptake inhibitor, in the treatment of aggression in schizophrenia. Acta Psychiatr Scand. 1995;91:348–351. doi: 10.1111/j.1600-0447.1995.tb09793.x. [DOI] [PubMed] [Google Scholar]
- 131.Zisook S, Kasckow JW, Lanouette NM, et al. Augmentation with citalopram for suicidal ideation in middle-aged and older outpatients with schizophrenia and schizoaffective disorder who have subthreshold depressive symptoms: a randomized controlled trial. J Clin Psychiatry. 2010;71:915–922. doi: 10.4088/JCP.09m05699gre. [DOI] [PubMed] [Google Scholar]
- 132.Zisook S, Kasckow JW, Golshan S, et al. Citalopram augmentation for sub-syndromal symptoms of depression in middle-aged and older outpatients with schizophrenia and schizoaffective disorder: a randomized controlled trial. J Clin Psychiatry. 2009;70:562–571. doi: 10.4088/jcp.08m04261. [DOI] [PubMed] [Google Scholar]