Abstract
Background:
Escitalopram is an allosteric selective serotonin reuptake inhibitor (SSRI) with some indication of superior efficacy in the treatment of major depressive disorder. In this systematic review, we critically evaluate the evidence for comparative efficacy and tolerability of escitalopram, focusing on pooled and meta-analysis studies.
Methods:
A literature search was conducted for escitalopram studies that quantitatively synthesized data from comparative randomized controlled trials in MDD. Studies were excluded if they did not focus on efficacy, involved primarily subgroups of patients, or synthesized data included in subsequent studies. Outcomes extracted from the included studies were weighted mean difference or standard mean difference, response and remission rates, and withdrawal rate owing to adverse events.
Results:
The search initially identified 24 eligible studies, of which 12 (six pooled analysis and six meta-analysis studies) met the criteria for review. The pooled and meta-analysis studies with citalopram showed significant but modest differences in favor of escitalopram, with weighted mean differences ranging from 1.13 to 1.73 points on the Montgomery Asberg Depression Rating Scale, response rate differences of 7.0%–8.3%, and remission rate differences of 5.1%–17.6%. Pooled analysis studies showed efficacy differences compared with duloxetine and with serotonin noradrenaline reuptake inhibitors combined, but meta-analysis studies did not. The effect sizes of the efficacy differences increased in the severely depressed patient subgroups.
Conclusion:
Based on pooled and meta-analysis studies, escitalopram demonstrates superior efficacy compared with citalopram and with SSRIs combined. Escitalopram shows similar efficacy to serotonin noradrenaline reuptake inhibitors but the number of trials in these comparisons is limited. Efficacy differences are modest but clinically relevant, especially in more severely depressed patients.
Keywords: escitalopram, depressive disorders, meta-analysis, pooled analysis, efficacy, antidepressants
Introduction
Major depressive disorder (MDD) is a common and serious psychiatric condition with significant public health implications.1 The World Health Organization estimates that, by 2030, MDD will be second only to ischemic heart disease as an overall cause of disability and disease burden.2 The economic costs of depression and its treatment are estimated at C$6 billion in Canada,3 US$83 billion in the US,4 and €118 billion in Europe.5
There are many evidence-based psychotherapy and pharmacotherapy treatments for MDD. Antidepressant medications remain a mainstay of treatment for MDD, especially for those with moderate to severe depression. Newer antidepressants, including selective serotonin reuptake inhibitors (SSRIs), serotonin noradrenaline reuptake inhibitors (SNRIs), and novel mechanism agents offer fewer side effects and are safer in overdose compared with tricyclic antidepressants and monoamine oxidase inhibitors. Hence, most clinical guidelines consider the newer generation antidepressants to be first-line medications for MDD.6–8
Escitalopram, the S-enantiomer of racemic citalopram, is an SSRI that has an additional modulatory effect at an allosteric binding site on the serotonin transporter protein.9 Escitalopram has been demonstrated in many placebo-controlled, randomized, controlled trials to be an efficacious antidepressant for MDD.10,11 Moreover, some randomized controlled trials have shown evidence for the superior efficacy and tolerability of escitalopram compared with other SSRIs and other agents.12,13
Unfortunately, the evaluation of comparative efficacy of antidepressants is complex. Placebo-controlled, randomized, controlled trials remain the gold standard for demonstrating the efficacy of treatments. However, most randomized controlled trials in MDD are designed to detect differences between an active antidepressant and placebo, and hence are not adequately powered to detect smaller, but still clinically relevant, differences between two active antidepressants.
Because of the limitations of randomized controlled trials, meta-analysis to investigate the comparative effectiveness of antidepressants is being increasingly used.14 Meta-analysis is a statistical technique to synthesize results from many randomized controlled trials. It can be a powerful method to increase power to detect differences between agents even when individual randomized controlled trials cannot. There are two main types of meta-analysis, ie, those using pooled individual patient data (usually called pooled analysis studies) and those using summary data from individual trials (more typically known as meta-analyses).15 Pooled analysis studies have the advantages of considerable power and the ability to examine subgroups, because all individual patient data are available for analysis. However, randomized controlled trials can only be pooled if they have very similar study designs (eg, use the same outcome measure) and if investigators agree to release of individual patient data. The latter is very difficult to arrange, hence many pooled analysis studies report on trials from a single sponsor. In contrast, standard meta-analyses can synthesize data from very different types of randomized controlled trials, because a standardized effect size can be calculated for any outcome measure and only summary data from a trial are necessary.
Regardless of the type of meta-analysis, the details of meta-analysis methodology are as important for interpretation of results as they are for randomized controlled trials. Selection criteria for inclusion of studies is perhaps the most important aspect of meta-analysis. Results may differ widely depending on these criteria, including whether published or unpublished trials are included.15 Other important factors to consider include definitions of primary and secondary outcomes, duration of trials, dose comparability, and assessment of heterogeneity and publication bias.14
The objective of this systematic review is to examine critically the evidence for the comparative efficacy and tolerability of escitalopram, focusing on studies using pooled analysis and meta-analysis to synthesize randomized controlled trial data.
Methods
A literature search was performed using PubMed with keywords including “escitalopram”, “depression”, “meta-analysis”, “pooled analysis”, and “systematic review”. We also scanned reference lists of review papers on escitalopram. Studies were included if they conducted analyses that synthesized data on randomized controlled trials using pooled analysis and meta-analysis. Studies were excluded if they did not primarily examine efficacy or if they only examined patient subgroups.
All of the randomized controlled trials represented within these studies used the Montgomery-Asberg Depression Rating Scale (MADRS) or the Hamilton Depression Rating Scale (Ham-D) as primary outcomes. The results of included studies were tabulated for the following outcomes: weighted mean difference (WMD) or standardized mean difference (SMD) from MADRS or Ham-D scores, response rate, remission rate, and withdrawal rate owing to adverse events (if not available, then all-cause withdrawal rate was used). Unless otherwise indicated, response is defined as a 50% or greater reduction in scale scores from baseline, while remission is defined as either MADRS ≤ 12 or Ham-D ≤ 7, depending on the scale used.
Results
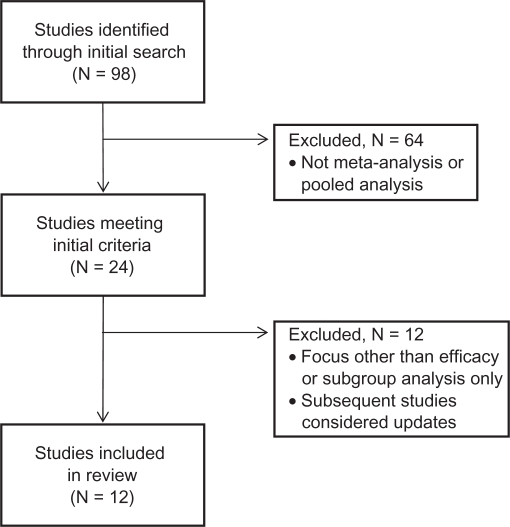
The initial electronic search yielded 98 articles, of which 24 met the inclusion criteria as a pooled analysis or meta-analysis study (see Figure 1). Sixteen pooled analysis studies and six meta-analysis studies were identified. Two additional meta-analysis studies were “hybrid” studies, but were classified as pooled studies because they primarily reported pooled analyses of individual patient data, with only limited analyses of summary data.16,17
Figure 1.
Flow diagram for identification of pooled and meta-analysis studies of comparative efficacy of escitalopram.
Of the 18 pooled analysis studies, we excluded five studies18–22 primarily focusing on topics (symptom clusters, onset of action, predictors of response) other than efficacy, two studies17,23 which were considered subsets of subsequent larger pooled studies, and five studies24–28 focusing on severity analyses only. This left six pooled analysis studies for review (Table 1). Several of the pooled studies also analyzed outcomes for a severely depressed patient subgroup, defined as baseline MADRS ≥ 30 (Table 2). All studies except one29 used data from randomized controlled trials sponsored by the manufacturer or distributor of escitalopram (Lundbeck or Forest).
Table 1.
Pooled analysis studies of comparative efficacy of escitalopram in all patients
| Author | Number of trials (patients, n) | Comparator | Primary outcome | Mean treatment difference | Response rates | Remission rates | Withdrawals (for adverse events) | Comments |
|---|---|---|---|---|---|---|---|---|
| Kennedy et al16 | 16 trials with all agents (n = 4549) | Citalopram, fluoxetine, paroxetine, sertraline, duloxetine, venlafaxine | MADRS | ESC > Comp, 1.1 points, P < 0.0001 | ESC > Comp, 63.7% vs 58.3%, P < 0.0001 | ESC > Comp, 53.1% vs 49.4%, P < 0.0059 | ESC < Comp, 5.4% vs 7.9%, P < 0.0007 | Also conducted subgroup analysis of four SNRI trials, but used the same data and had the same results as Kornstein et al 2009 |
| 12 trials with SSRIs (n = 2964) | Citalopram, fluoxetine, paroxetine, sertraline | MADRS | ESC > SSRIs, 0.9 points, P = 0.0023 | ESC > SSRIs, 62.1% vs 58.3%, P = 0.0089 | ESC = SSRIs, 51.6% vs 49.0%, P = 0.0958 | ESC = SSRIs, 5.4% vs 6.3%, P = ns | Pooled data from 12 of 15 identified randomized controlled trials with SSRIs | |
| 5 trials with citalopram (n = 1583) | Citalopram | MADRS | ESC > CIT, 1.2 points, P = 0.0094 | ESC > CIT, 59.7% vs 52.3%, P = 0.0043 | ESC = CIT, 47.8% vs 42.7%, P = 0.0517 | Not reported | Pooled data from 5 of 8 identified randomized controlled trials with citalopram | |
| Kasper et al32 | 2 trials (n = 777) | Paroxetine | MADRS | ESC > PAR, 2.0 points, P < 0.01 | ESC > PAR, 83% vs 76.8%, P < 0.05 | ESC > PAR, 76.4% vs 70.0%, P < 0.05 | ESC < PAR, 6.6% vs 11.7%, P < 0.01 | Pooled data from 2 of 2 identified randomized controlled trials with paroxetine |
| Lam et al34 | 2 trials (n = 569) | Duloxetine | MADRS | ESC > DUL, 2.6 points, P < 0.01 | ESC > DUL, 67.1% vs 53.2%, P < 0.001 | ESC > DUL, 54.3% vs 44.4%, P < 0.05 | ESC < DUL, 12.9% vs 24.3%, P < 0.001 | Pooled data from 2 of 3 identified randomized controlled trials with duloxetine |
| Montgomery and Andersen33 | 2 trials (n = 483) | Venlafaxine XR | MADRS | ESC = VEN, 2.1 points, P = ns | ESC = VEN, 70% vs 67%, P = ns | ESC = VEN, 62% vs 58%, P = ns | ESC < VEN, 6.2% vs 13.3%, P < 0.01 | Pooled data from 2 of 2 identified randomized controlled trials with venlafaxine XR |
| Kornstein et al35 | 4 trials (n = 1051) | Duloxetine, venlafaxine XR | MADRS | ESC > SNRIs 1.7 points, P < 0.01 | ESC > SNRIs, 68.3% vs 59.0%, P < 0.01 | ESC > SNRIs, 57.8% vs 50.5%, P < 0.05 | ESC < SNRIs, 5.3% vs 12.0%, P < 0.0001 | Pooled data from 4 of 5 identified randomized controlled trials with SNRIs |
| Clayton et al29 | 2 trials (n = 830) | Bupropion XL | Ham-D | ESC = BUP 0.4 points, P = ns | ESC = BUP, 65% vs 62%, P = ns | ESC = BUP, 45% vs 43%, P = ns | ESC = BUP, 4.3% vs 6.2%, P = ns | Pooled data from 2 of 2 identified randomized controlled trials with bupropion. ESC > BUP in worsened sexual functioning, 36% vs 20%, P < 0.001 |
Abbreviations: BUP, bupropion XL; ESC, escitalopram; CIT, citalopram; Comp, comparator; DUL, duloxetine; Ham-D, Hamilton Depression Rating Scale; MADRS, Montgomery Asberg Depression Rating Scale; ns, not significant; PAR, paroxetine; SNRI, serotonin noradrenaline reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; VEN, venlafaxine XR.
Table 2.
Pooled analysis studies of comparative efficacy of escitalopram: subgroups of severely depressed patients
| Author | Number of trials (patients, n) | Comparator | Primary outcome | Mean treatment difference | Response rates | Remission rates |
|---|---|---|---|---|---|---|
| Kennedy et al16 | 16 trials with all agents (n = 2345) | Citalopram, fluoxetine, paroxetine, sertraline, duloxetine, venlafaxine | MADRS | ESC > Comp, 1.8 points, P < 0.0001 | ESC > Comp, 64.4% vs 55.8%, P < 0.0001 | ESC > Comp, 47.7% vs 41.6%, P = 0.0017 |
| 12 trials with SSRIs (n = 869) | Citalopram, fluoxetine, paroxetine, sertraline | MADRS | ESC > SSRIs, 1.4 points, P = 0.0004 | ESC > SSRIs, 62.9% vs 56.3%, P = 0.0015 | ESC = SSRIs, 45.8% vs 42.0%, P = 0.0811 | |
| 5 trials with citalopram (n = 742) | Citalopram | MADRS | ESC > CIT, 2.0 points, P = 0.0013 | ESC > CIT, 61.2% vs 49.9%, P = 0.0012 | ESC = CIT, 41.8% vs 35.5%, P = 0.0640 | |
| Kasper et al32 | 2 trials (n = 606) | Paroxetine | MADRS | ESC > PAR, 2.6 points, P < 0.01 | ESC > PAR 82.6% vs 75.7%, P < 0.05 | ESC > PAR 69.0% vs 60.1%, P < 0.05 |
| Lam et al34 | 2 trials (n = 371) | Duloxetine | MADRS | ESC > DUL, 3.7 points, P < 0.01 | ESC > DUL, 68.8% vs 49.7%, P < 0.001 | ESC > DUL, 51.7% vs 37.4%, P < 0.01 |
| Montgomery and Andersen33 | 2 trials (n = 121) | Venlafaxine XR | MADRS | ESC > VEN, 3.8 points, P < 0.05 | Not reported | Not reported |
| Kornstein et al35 | 4 trials (n = 622) | Duloxetine, venlafaxine XR | MADRS | ESC > SNRIs 2.9 points, P < 0.001 | ESC > SNRIs 68.7% vs 54.3%, P < 0.001 | ESC > SNRIs 53.0% vs 40.4%, P < 0.001 |
Abbreviations: Comp, comparator; ESC, escitalopram; CIT, citalopram; DUL, duloxetine; MADRS, Montgomery Asberg Depression Rating Scale; PAR, paroxetine; SNRI, serotonin noradrenaline reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; VEN, venlafaxine XR.
Of the six meta-analysis (and two hybrid) studies, two studies17,30 were excluded because subsequent studies were considered updates, but one16 of the hybrid studies included a direct meta-analysis, hence six meta-analysis studies were eligible for review (Table 3).
Table 3.
Meta-analysis studies of comparative efficacy of escitalopram
| Author | Number of trials (patients, n) | Comparator | Mean difference | Response rates | Remission rates | Withdrawals (for adverse events) | Comments |
|---|---|---|---|---|---|---|---|
| Gartlehner et al37 | 114 trials with all agents (n = 26,349) | Bupropion, duloxetine, fluoxetine, fluvoxamine mirtazapine, nefazodone paroxetine, sertraline, trazodone, venlafaxine | Not reported | No differences in any comparisons | Not reported | No individual comparisons reported | Used indirect comparisons (including placebo-controlled randomized controlled trials) with modified network meta-analysis and meta-regression techniques. |
| 5 trials (n = 1359) | Citalopram | ESC > CIT, WMD = 1.13 MADRS points (CI 0.18–2.09) | ESC > CIT, RR = 1.14 (CI 1.04–1.26) | Not reported | Not reported | Direct meta-analysis | |
| Cipriani et al36 | 14 trials with all agents (n = 5921) | Bupropion, duloxetine, paroxetine, sertraline, venlafaxine | No differences in any comparisons | No differences in any comparisons | No differences in any comparisons | No differences in any comparisons | Cochrane systematic review – includes comprehensive search of all available randomized controlled trials to July 2008 |
| 3 trials (n = 783) | Fluoxetine | ESC > FLU, SMD = 0.17, P < 0.02 | ESC = FLU, OR = 0.81, P = ns | ESC = FLU OR = 0.86, P = ns | No differences | ||
| 6 trials (n = 1823) | Citalopram | ESC > CIT, SMD = 0.17, P = 0.009 | ESC > CIT, OR = 0.67 (CI 0.50–0.87) | ESC > CIT OR = 0.53 (CI 0.30–0.93) | No differences | ||
| Trkulja38 | 7 trials (n = 2476) | Citalopram | ESC > CIT, WMD = 1.232 points (CI 0.27–2.195) SMD = 0.131 (CI 0.027–0.322) | ESC > CIT, RR = 1.144 (CI 1.037–1.262) | Not reported | ESC = CIT 4.4% vs 4.7%, P = ns | Analyzed based on week to week outcomes. Figures in this table based on 8-week outcomes (5 trials) |
| Montgomery et al39 | 9 trials (n = 2009) | Citalopram | ESC > CIT, WMD = 1.7 MADRS points, P = 0.0002 | ESC > CIT, OR = 1.44, P = 0.0003 | ESC > CIT, OR = 1.86 P < 0.0001 | Not reported | Included one nonrandomized trial55 |
| Kennedy et al16 | 3 trials (n = 1111) | Duloxetine | ESC = DUL, WMD = 0.22 Ham-D points, P = ns | Not reported | Not reported | Not reported | Used results from mixed model repeated measures analyses of Ham-D data from primary randomized controlled trials |
| 5 trials (n = 1598) | Duloxetine, venlafaxine | ESC = SNRIs, WMD = 0.18 Ham-D points, P = ns | Not reported | Not reported | Not reported | Used results from mixed model repeated measures analyses of Ham-D data from primary randomized controlled trials | |
| Cipriani et al42 | 117 trials with all agents (n = 25,928) | Bupropion, citalopram, duloxetine, fluoxetine, fluvoxamine, milnacipran, mirtazapine, paroxetine, reboxetine, sertraline, venlafaxine | Not reported | ESC > CIT OR = 1.47 (CI 1.15–1.90) Superior response for escitalopram, mirtazapine, sertraline, and venlafaxine | Not reported | Superior acceptability (all-cause withdrawals) for bupropion, citalopram, escitalopram, and sertraline | Multiple treatments (network) meta-analysis using direct and indirect comparisons |
Abbreviations: ESC, escitalopram; CI, 95% confidence interval; CIT, citalopram; DUL, duloxetine; FLU, fluoxetine; Ham-D, Hamilton Depression Rating Scale; MADRS, Montgomery Asberg Depression Rating Scale; ns, not significant; OR, odds ratio; PAR, paroxetine; SMD, standardized mean difference; RR, relative risk; SNRI, serotonin noradrenaline reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; WMD, weighted mean difference.
An important consideration for systematic reviews and meta-analyses is the “universe” of randomized controlled trials from which trials are selected. Inspection of the included trials from these meta-analysis studies revealed a total of 22 comparative randomized controlled trials of escitalopram with citalopram (eight trials), fluoxetine (three trials), paroxetine (two trials), sertraline (two trials), bupropion XL (two trials), duloxetine (three trials), and venlafaxine XR (two trials). An updated electronic search of PubMed through to November 2010 found one additional trial with desvenlafaxine in postmenopausal women.31
Pooled analysis studies
Two pooled analysis studies examined escitalopram compared with other SSRIs. Kennedy et al16 pooled five trials with citalopram and found superiority for escitalopram in mean MADRS difference (1.2 points, P = 0.00094) and response rate difference (7.4%, P = 0.0043), but remission rate difference missed significance (5.1%, P = 0.0517). In addition, Kennedy et al also reported superiority for escitalopram over combined SSRIs (12 trials of citalopram, fluoxetine, paroxetine, sertraline), although this was largely explained by differences between escitalopram and citalopram. There was no difference in withdrawal rate owing to adverse events between escitalopram and SSRIs. Another study pooled data from two trials with paroxetine and found superiority for escitalopram in mean MADRS difference (2 points, P < 0.01), response difference (6.2%, P < 0.05), remission difference (6.4%, P < 0.05) and withdrawal rate difference (5.1%, P < 0.01).32
Three pooled studies examined escitalopram compared with SNRIs. In the first, data from two randomized controlled trials with venlafaxine XR were pooled.33 No significant differences were found in MADRS difference, response, or remission rates. However, the withdrawal rate for adverse events was lower for escitalopram (7.5% versus 11.2%, P < 0.05). The second study pooled data from two trials with duloxetine.34 Escitalopram was superior in MADRS difference (2.6 points, P < 0.01), response difference (13.9%, P < 0.001) and remission difference (9.9%, P < 0.05). The withdrawal rate for adverse events also favored escitalopram (12.9% versus 24.3%, P < 0.001). The third study pooled results from the four randomized controlled trials of duloxetine and venlafaxine XR included in the previously described studies.35 (Note that Kennedy et al16 also reported a pooled analysis of these same four SNRI trials, but the results were identical.) At week 8, escitalopram was superior to the two SNRIs in MADRS difference (1.7 points, P < 0.01), and response and remission differences (9.3%, P < 0.01, and 7.2%, P < 0.05, respectively). The withdrawal rate for adverse events was also lower for escitalopram than the SNRIs (5.3% versus 12.0%, P < 0.0001).
A comprehensive pooled analysis compared 16 randomized controlled trials of escitalopram and six comparator antidepressants (citalopram, fluoxetine, paroxetine, sertraline, duloxetine, venlafaxine), which included all the trials in the previously described pooled studies.16 Trials less than 8 weeks (two trials) and trials that did not include the MADRS (four trials) were excluded from this analysis. At week 8, escitalopram was superior to all comparators, with an estimated MADRS difference of 1.1 points (P < 0.0001), response difference of 5.4% (P < 0.0001), remission difference of 3.7% (P < 0.006), and withdrawal rate difference of 2.5% (P < 0.0007).
One final pooled analysis29 involved two randomized controlled trials with bupropion XL, both sponsored by the manufacturer of bupropion (GlaxoSmithKline). No significant differences were found between escitalopram and bupropion XL in the efficacy outcomes or withdrawal rates.
Several of the pooled analysis studies also examined outcomes for a subgroup of patients who were severely depressed at baseline (Table 2). In these studies, when compared with the total group, the severely depressed subgroup showed increased differences between escitalopram and the comparator. In the Kennedy et al16 pooled analysis of five citalopram trials, the MADRS difference at week 8 in patients with baseline MADRS ≥ 30 favored escitalopram by 2.0 points (P = 0.0013), as did the response rate difference (11.3%, P = 0.0012), although the remission rate difference of 6.3% was not statistically significant. Similarly, Kornstein et al35 also found that the differences between escitalopram and SNRIs in the severely ill subgroup were greater than those overall, with a significant MADRS difference of 2.9 points and response/remission differences of 14.4%/13.4% (P < 0.001). Finally, the Kennedy et al16 comprehensive pooled analysis of 16 trials found that the MADRS difference between escitalopram and all comparators in the severely depressed subgroup was 1.8 points, with a response difference of 8.6% and a remission difference of 6.1%, all of which were statistically significant.
Meta-analysis studies
A Cochrane systematic review of escitalopram was conducted as one of a series systematically evaluating the newer generation antidepressants. Cipriani et al36 compared the efficacy and acceptability of escitalopram with other antidepressants in 20 published and unpublished trials, searched through to July 2008. In acute-phase treatment (6–12 weeks), escitalopram was shown to be significantly superior to citalopram (based on six trials) in SMD at endpoint (−0.17, P < 0.009) and in achieving response (60.7% versus 53.8%, P < 0.006) and remission (47.7% versus 38.5%, P < 0.02), and superior to fluoxetine (based on three trials) in SMD (−0.17, P < 0.02). There were no other significant differences in efficacy between escitalopram and paroxetine, sertraline, bupropion, duloxetine, and venlafaxine, but these analyses were limited to 2–3 trials per comparison.
Three other meta-analyses specifically focused on comparison of escitalopram versus citalopram. Although the included studies were similar for all three, each study used different analyses and reached different clinical conclusions. Gartlehner et al37 included five randomized controlled trials, of which one was unpublished, all using the MADRS as primary outcome. At week 8, escitalopram was superior in WMD (1.13 MADRS points, P = 0.02) and response rate difference (about 7%, P < 0.05). Trkulja38 included seven randomized controlled trials (including all those in Gartlehner et al37), but outcomes were analyzed for each weekly time point separately, and only those trials that reported data for that time point were included. At the week 8 time point, based on five trials, escitalopram was significantly superior, with a WMD of 1.23 (P = 0.012) and a response difference of 7% (P = 0.007). The week 6 time point results, based on four trials, showed a WMD of 1.73 (P = 0.004). Despite the statistically significant findings, the authors of these two studies concluded that the differences were not clinically relevant.
In contrast, Montgomery et al39 meta-analyzed eight randomized controlled citalopram trials, including all those in the Trkulja38 review plus an additional small (n = 56) randomized controlled trial reported in a Chinese language journal. The outcomes included WMD (based on the six trials using the MADRS), response rates (based on all eight trials), and remission rates (based on the MADRS, reported in only four trials). The primary results showed superiority for escitalopram, with a WMD of 1.7 (P = 0.0002), a response difference of 8.3%, and a remission difference of 17.6%. These differences were regarded by the study authors as clinically significant.
Finally, Kennedy et al16 included a limited meta-analysis of the five randomized controlled trials with the SNRIs, duloxetine and venlafaxine XR. In contrast with the pooled analysis results, this was conducted using Ham-D scores and mixed model repeated measures analyses of the primary trials. With these parameters, there were no significant differences in the Ham-D WMD between escitalopram and duloxetine (three trials) or between escitalopram and the combined SNRIs (five trials).
Multiple treatments meta-analysis studies
Two of the escitalopram meta-analyses used a newer statistical approach, multiple-treatments meta-analysis, also called network meta-analysis, to compare the efficacy and acceptability of 12 new-generation antidepressants. In contrast with a usual meta-analysis, where direct comparisons of two agents are analyzed, a multiple-treatments meta-analysis allows for the integration of data from both direct comparisons (when two agents are compared within one randomized controlled trial) and indirect comparisons (when two agents are compared by combining results based on randomized controlled trials with a common third agent).40,41
Gartlehner et al37 included 114 randomized controlled trials (with 12 comparative escitalopram trials) searched through to April 2007, including unpublished trials. The primary efficacy outcomes were WMD and response rate. Direct comparison using meta-analysis was conducted if there were three or more trials, otherwise indirect comparisons of response rates were conducted using metaregression and modified network analysis. Only the direct meta-analyses found significant results in response rates: escitalopram superior to citalopram (described in the previous meta-analysis section), sertraline superior to fluoxetine, and venlafaxine superior to fluoxetine. However, the study authors questioned the clinical relevance of the small differences found.
Cipriani et al42 conducted a multiple treatments meta-analysis that included 117 randomized controlled trials (with 19 escitalopram trials) from 1991 to November 2007, including 15 unpublished trials obtained from pharmaceutical company websites. The primary outcomes were efficacy, defined as the response rate, and acceptability, defined as the proportion of patients who withdrew from the study for all causes. Compared with the other antidepressants, the main efficacy results found superiority in response rates for escitalopram, mirtazapine, sertraline, and venlafaxine; inferiority was found only for reboxetine. A series of sensitivity analyses (examining dosing, imputation strategy, sponsorship, etc) did not change the results. Four antidepressants were also found to be superior in acceptability, ie, bupropion, citalopram, escitalopram, and sertraline. The authors concluded that these were clinically relevant differences in efficacy and acceptability.
Discussion
This systematic review identified a number of studies using pooled analyses of individual patient data and meta-analyses of summary trial data evaluating the comparative efficacy of escitalopram, but differences in criteria for inclusion of trials and statistical methodologies of these studies make direct comparisons difficult. In addition, the “universe” of known trials available for meta-analysis is a moving target, as new randomized controlled trials are added to the clinical trials database. For example, there were 22 comparative randomized controlled trials of escitalopram available for review, but none of the meta-analysis studies included all of them.
Overall, a comprehensive pooled analysis16 and a network meta-analysis42 both found evidence for superiority of escitalopram over other comparators, although one modified network meta-analysis37 did not. However, there is consistent evidence that escitalopram is superior in efficacy to other SSRIs, especially citalopram. The pooled and meta-analysis studies with citalopram (with 3–8 trials included in each study) show consistent statistically significant findings in favor of escitalopram in WMD (1.13–1.73 MADRS points), response rate difference (7.0%–8.3%), and remission rate difference (5.1%–17.6%). A pooled analysis of two paroxetine trials also found superiority of escitalopram in these outcomes. Similarly, a pooled comparison of escitalopram with all SSRIs combined together (12 trials) also found significant differences in favor of escitalopram, although the effect sizes were smaller.16
The comparative efficacy of escitalopram with SNRIs and other agents is less clear. Pooled analyses found significant superiority over duloxetine,34 but no differences with venlafaxine XR,33 while meta-analyses found no differences with either.36,37 A pooled analysis35 (using MADRS scores) of the two SNRIs combined also favored escitalopram, while a meta-analysis16 (using Ham-D scores) did not. The reason for the discrepancy between the pooled and meta-analysis studies of SNRIs may be owing to the small number of randomized controlled trials available, in that pooled analysis of individual patient data has greater power to detect differences than meta-analysis. The one comparison with bupropion (a pooled analysis of two trials) found no comparative differences, but in that analysis the bupropion group did not significantly differentiate from placebo in the primary outcome (WMD), whereas the escitalopram group did.29
Despite the consistent evidence for superiority of escitalopram over SSRIs, there is still contention about the clinical importance of the differences. For example, very similar results were found in the pooled and meta-analysis studies with citalopram, but some authors interpreted their results as clinically relevant, while others did not. A major issue is that there is still no consensus about the definition for a minimal clinically important difference (MCID) for drug-placebo comparisons. Some suggested criteria for drug-placebo MCID with antidepressants include a MADRS difference of 2 points or a response rate difference of 10% (corresponding to a number needed to treat of 10).43 Moreover, it is unclear whether active drug comparisons should use the same MCID as drug-placebo comparisons. If so, to be considered superior, an antidepressant would need to show an additional 2-point MADRS difference against a comparator, or 4 points relative to placebo; this seems to be an unreasonably difficult threshold to achieve. Hence, some investigators have suggested that the MCID between two active agents should be half the drug-placebo MCID, corresponding to at least 1 point MADRS difference, or 5% response rate difference (number needed to treat = 20).44 Using these MCID criteria, the superiority of escitalopram over citalopram and other SSRIs would be considered clinically relevant.
Because of the high placebo response in clinical trials, some investigators have also suggested using methods to increase assay sensitivity for detecting clinically relevant differences between antidepressants. One such method is to examine subgroups of patients with higher baseline severity of symptoms. The more severely depressed subgroup, usually defined as MADRS ≥ 30 or Ham-D ≥ 25, may have better responses to medication and/or lower responses to placebo, either of which make it easier to detect specific effects of the active medications. In this review, the pooled analysis studies that examined severely depressed subgroups found larger efficacy differences for escitalopram, with WMDs ranging from 1.4 to 3.8 MADRS points and response rate differences ranging from 6.6% to 19.1%. These differences are well within any definition for clinical importance. The results are consistent with evidence from pooled analyses that the comparative effect sizes in favor of escitalopram increase with increasing baseline severity.16,24,25 They are also consistent with those from head-to-head randomized controlled trials that prospectively enrolled patients with severe depression.45,46 Together, these studies provide some validation that the modest efficacy differences with escitalopram are clinically significant.
An important question is why should escitalopram have superior efficacy compared with racemic citalopram and other SSRIs? Biochemical studies have demonstrated that there are two distinct binding sites on the serotonin transporter protein, ie, a high-affinity, primary binding site that mediates the inhibition of serotonin reuptake, and a low affinity site that allosterically modulates the affinity of ligands at the primary site.9,47 Escitalopram uniquely binds to both the primary and allosteric sites,48 leading to enhanced serotonergic neurotransmission and subsequent downstream effects on synaptic plasticity and neurogenesis.49–51 The R-enantiomer in racemic citalopram binds only to the allosteric site, which interferes with the effects of escitalopram and counteracts its allosteric modulatory action.9,52 The additional allosteric mechanism of escitalopram, which appears to be unique among SSRI antidepressants,53 may explain its efficacy advantages in patients with MDD.
This systematic review also found evidence from the pooled analysis studies that escitalopram had lower withdrawal rates owing to adverse events compared with SNRIs, but not with citalopram or other SSRIs. Similarly, a multiple treatments meta-analysis found that escitalopram was one of four newer-generation antidepressants (along with bupropion, citalopram, and sertraline) that showed superior acceptability (based on all-cause withdrawals).42 These results are also consistent with a pooled analysis from a clinical trial database of over 4000 patients showing that escitalopram demonstrated very good safety and tolerability for treatment of MDD and anxiety disorders.13 Like other SSRIs, escitalopram is associated with sexual side effects, with pooled studies showing higher rates compared with bupropion.29 However, a meta-analysis of studies using specific sexual functioning questionnaires suggested that escitalopram may have lower rates than other SSRIs.54
The limitations of this systematic review must be considered. The meta-analysis and pooled studies were based on randomized controlled trials which mostly were eight weeks or less in duration. It is possible that any efficacy differences between escitalopram and comparators decrease over time. Similarly, doses may not have been optimized in the trials and results of randomized controlled trials may not be generalizable to more real-world conditions. Combining agents within a class (eg, all SSRIs, all SNRIs) as comparators may not be valid, especially because there is evidence that some agents within a class have greater efficacy than others. Finally, the total number of comparative randomized controlled trials of escitalopram (23 trials to November 2010) in MDD is still relatively low.
Conclusion
This systematic review of pooled analysis and meta-analysis studies found that escitalopram has superior efficacy compared with citalopram and SSRIs combined, and that the efficacy differences are modest but clinically relevant, especially in more severely depressed patients. Escitalopram also has at least similar efficacy to SNRIs and bupropion. In multiple-treatments (network) meta-analysis studies, escitalopram was one of four newer-generation antidepressants with evidence for superiority compared with the others. The efficacy differences of escitalopram may be related to its dual mechanism of action on the primary and allosteric binding sites on the serotonin transporter.
Many clinical factors, including efficacy, side effect profile, drug interactions, relapse prevention, simplicity of use, and cost-effectiveness must be considered together when making a clinical decision for a first-choice antidepressant.7 This systematic review of the efficacy of escitalopram should add to the evidence database to help guide clinicians on the choice of an appropriate medication.
Footnotes
Disclosure
Dr Ali reports no disclosures. Dr Lam is on Speaker/Advisory Boards for, or has received research funds from, Advanced Neuromodulation Systems Inc (St Jude Medical), AstraZeneca, BrainCells Inc, Biovail, Canadian Institutes of Health Research, Canadian Network for Mood and Anxiety Treatments, Canadian Psychiatric Research Foundation, Eli Lilly, Janssen, Litebook Company Ltd., Lundbeck, Lundbeck Institute, Mathematics of Information Technology and Advanced Computing Systems, Michael Smith Foundation for Health Research, Servier, Takeda, UBC Institute of Mental Health/Coast Capital Savings, and Wyeth.
References
- 1.Patten SB, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) Clinical Guidelines for the Management of Major Depressive Disorder in Adults. I. Classification, burden and principles of management. J Affect Disord. 2009;117(Suppl 1):S5–S14. doi: 10.1016/j.jad.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stephens T, Joubert N. The economic burden of mental health problems in Canada. Chronic Dis Can. 2001;22:18–23. [PubMed] [Google Scholar]
- 4.Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: How did it change between 1990 and 2000? J Clin Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 5.Sobocki P, Jonsson B, Angst J, Rehnberg C. Cost of depression in Europe. J Ment Health Policy Econ. 2006;9:87–98. [PubMed] [Google Scholar]
- 6.Davidson JR. Major depressive disorder treatment guidelines in America and Europe. J Clin Psychiatry. 2010;71(Suppl E1):e04. doi: 10.4088/JCP.9058se1c.04gry. [DOI] [PubMed] [Google Scholar]
- 7.Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord. 2009;117(Suppl 1):S26–S43. doi: 10.1016/j.jad.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 8.Anderson IM, Ferrier IN, Baldwin RC, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2000 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2008;22:343–396. doi: 10.1177/0269881107088441. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez C. The pharmacology of citalopram enantiomers: The antagonism by R-citalopram on the effect of S-citalopram. Basic Clin Pharmacol Toxicol. 2006;99:91–95. doi: 10.1111/j.1742-7843.2006.pto_295.x. [DOI] [PubMed] [Google Scholar]
- 10.Thase ME. Managing depressive and anxiety disorders with escitalopram. Expert Opin Pharmacother. 2006;7:429–440. doi: 10.1517/14656566.7.4.429. [DOI] [PubMed] [Google Scholar]
- 11.Waugh J, Goa KL. Escitalopram: A review of its use in the management of major depressive and anxiety disorders. CNS Drugs. 2003;17:343–362. doi: 10.2165/00023210-200317050-00004. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery SA, Baldwin DS, Blier P, et al. Which antidepressants have demonstrated superior efficacy? A review of the evidence. Int Clin Psychopharmacol. 2007;22:323–329. doi: 10.1097/YIC.0b013e3282eff7e0. [DOI] [PubMed] [Google Scholar]
- 13.Baldwin DS, Reines EH, Guiton C, Weiller E. Escitalopram therapy for major depression and anxiety disorders. Ann Pharmacother. 2007;41:1583–1592. doi: 10.1345/aph.1K089. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman JA, Greenhouse J, Hamer RM, et al. Comparing the effects of antidepressants: Consensus guidelines for evaluating quantitative reviews of antidepressant efficacy. Neuropsychopharmacology. 2005;30:445–460. doi: 10.1038/sj.npp.1300571. [DOI] [PubMed] [Google Scholar]
- 15.Lam RW, Kennedy SH. Using metaanalysis to evaluate evidence: Practical tips and traps. Can J Psychiatry. 2005;50:167–174. doi: 10.1177/070674370505000306. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy SH, Andersen HF, Thase ME. Escitalopram in the treatment of major depressive disorder: A meta-analysis. Curr Med Res Opin. 2009;25:161–175. doi: 10.1185/03007990802622726. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy SH, Andersen HF, Lam RW. Efficacy of escitalopram in the treatment of major depressive disorder compared with conventional selective serotonin reuptake inhibitors and venlafaxine XR: A meta-analysis. J Psychiatry Neurosci. 2006;31:122–131. [PMC free article] [PubMed] [Google Scholar]
- 18.Lam RW, Lonn SL, Despiegel N. Escitalopram versus serotonin noradrenaline reuptake inhibitors as second step treatment for patients with major depressive disorder: A pooled analysis. Int Clin Psychopharmacol. 2010;25:199–203. doi: 10.1097/YIC.0b013e32833948d8. [DOI] [PubMed] [Google Scholar]
- 19.Wade AG, Schlaepfer TE, Andersen HF, Kilts CD. Clinical milestones predict symptom remission over 6-month and choice of treatment of patients with major depressive disorder (MDD) J Psychiatr Res. 2009;43:568–575. doi: 10.1016/j.jpsychires.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Kasper S, Spadone C, Verpillat P, Angst J. Onset of action of escitalopram compared with other antidepressants: Results of a pooled analysis. Int Clin Psychopharmacol. 2006;21:105–110. doi: 10.1097/01.yic.0000194375.42589.c3. [DOI] [PubMed] [Google Scholar]
- 21.Papakostas GI, Larsen K. Testing anxious depression as a predictor and moderator of symptom improvement in major depressive disorder during treatment with escitalopram. Eur Arch Psychiatry Clin Neurosci. 2010 Sep 22; doi: 10.1007/s00406-010-0149-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Wade A, Friis AH. The onset of effect for escitalopram and its relevance for the clinical management of depression. Curr Med Res Opin. 2006;22:2101–2110. doi: 10.1185/030079906X148319. [DOI] [PubMed] [Google Scholar]
- 23.Gorman JM, Korotzer A, Su G. Efficacy comparison of escitalopram and citalopram in the treatment of major depressive disorder: Pooled analysis of placebo-controlled trials. CNS Spectr. 2002;7:40–44. doi: 10.1017/s1092852900028595. [DOI] [PubMed] [Google Scholar]
- 24.Kilts CD, Wade AG, Andersen HF, Schlaepfer TE. Baseline severity of depression predicts antidepressant drug response relative to escitalopram. Expert Opin Pharmacother. 2009;10:927–936. doi: 10.1517/14656560902849258. [DOI] [PubMed] [Google Scholar]
- 25.Lam RW, Andersen HF. The influence of baseline severity on efficacy of escitalopram and citalopram in the treatment of major depressive disorder: An extended analysis. Pharmacopsychiatry. 2006;39:180–184. doi: 10.1055/s-2006-949148. [DOI] [PubMed] [Google Scholar]
- 26.Bech P, Andersen HF, Wade A. Effective dose of escitalopram in moderate versus severe DSM-IV major depression. Pharmacopsychiatry. 2006;39:128–134. doi: 10.1055/s-2006-946702. [DOI] [PubMed] [Google Scholar]
- 27.Llorca PM, Azorin JM, Despiegel N, Verpillat P. Efficacy of escitalopram in patients with severe depression: A pooled analysis. Int J Clin Pract. 2005;59:268–275. doi: 10.1111/j.1742-1241.2005.00440.x. [DOI] [PubMed] [Google Scholar]
- 28.Lepola U, Wade A, Andersen HF. Do equivalent doses of escitalopram and citalopram have similar efficacy? A pooled analysis of two positive placebo-controlled studies in major depressive disorder. Int Clin Psychopharmacol. 2004;19:149–155. doi: 10.1097/00004850-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Clayton AH, Croft HA, Horrigan JP, et al. Bupropion extended release compared with escitalopram: Effects on sexual functioning and antidepressant efficacy in 2 randomized, double-blind, placebo-controlled studies. J Clin Psychiatry. 2006;67:736–746. doi: 10.4088/jcp.v67n0507. [DOI] [PubMed] [Google Scholar]
- 30.Auquier P, Robitail S, Llorca PM, Rive B. Comparison of escitalopram and citalopram efficacy: A meta-analysis. Int J Psychiatry Clin Pract. 2003;7:259–268. doi: 10.1080/13651500310003408. [DOI] [PubMed] [Google Scholar]
- 31.Soares CN, Thase ME, Clayton A, et al. Desvenlafaxine and escitalopram for the treatment of postmenopausal women with major depressive disorder. Menopause. 2010;17:700–711. doi: 10.1097/gme.0b013e3181d88962. [DOI] [PubMed] [Google Scholar]
- 32.Kasper S, Baldwin DS, Larsson LS, Boulenger JP. Superiority of escitalopram to paroxetine in the treatment of depression. Eur Neuropsychopharmacol. 2009;19:229–237. doi: 10.1016/j.euroneuro.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 33.Montgomery SA, Andersen HF. Escitalopram versus venlafaxine XR in the treatment of depression. Int Clin Psychopharmacol. 2006;21:297–309. doi: 10.1097/00004850-200609000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Lam RW, Andersen HF, Wade AG. Escitalopram and duloxetine in the treatment of major depressive disorder: A pooled analysis of two trials. Int Clin Psychopharmacol. 2008;23:181–187. doi: 10.1097/YIC.0b013e3282ffdedc. [DOI] [PubMed] [Google Scholar]
- 35.Kornstein SG, Li D, Mao Y, Larsson S, Andersen HF, Papakostas GI. Escitalopram versus SNRI antidepressants in the acute treatment of major depressive disorder: Integrative analysis of four double-blind, randomized clinical trials. CNS Spectr. 2009;14:326–333. doi: 10.1017/s1092852900020320. [DOI] [PubMed] [Google Scholar]
- 36.Cipriani A, Santilli C, Furukawa TA, et al. Escitalopram versus other antidepressive agents for depression. Cochrane Database Syst Rev. 2009:CD006532. doi: 10.1002/14651858.CD006532.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gartlehner G, Gaynes BN, Hansen RA, et al. Comparative benefits and harms of second-generation antidepressants: Background paper for the American College of Physicians. Ann Intern Med. 2008;149:734–750. doi: 10.7326/0003-4819-149-10-200811180-00008. [DOI] [PubMed] [Google Scholar]
- 38.Trkulja V. Is escitalopram really relevantly superior to citalopram in treatment of major depressive disorder? A meta-analysis of head-to-head randomized trials. Croat Med J. 2010;51:61–73. doi: 10.3325/cmj.2010.51.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Montgomery S, Hansen T, Kasper S. Efficacy of escitalopram compared with citalopram: A meta-analysis. Int J Neuropsychopharmacol. 2010:1–8. doi: 10.1017/S146114571000115X. [DOI] [PubMed] [Google Scholar]
- 40.Salanti G, Higgins JP, Ades AE, Ioannidis JP. Evaluation of networks of randomized trials. Stat Methods Med Res. 2008;17:279–301. doi: 10.1177/0962280207080643. [DOI] [PubMed] [Google Scholar]
- 41.Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med. 2002;21:2313–2324. doi: 10.1002/sim.1201. [DOI] [PubMed] [Google Scholar]
- 42.Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: A multiple-treatments meta-analysis. Lancet. 2009;373:746–758. doi: 10.1016/S0140-6736(09)60046-5. [DOI] [PubMed] [Google Scholar]
- 43.Duru G, Fantino B. The clinical relevance of changes in the Montgomery-Asberg Depression Rating Scale using the minimum clinically important difference approach. Curr Med Res Opin. 2008;24:1329–1335. doi: 10.1185/030079908x291958. [DOI] [PubMed] [Google Scholar]
- 44.Montgomery SA, Moller HJ. Is the significant superiority of escitalopram compared with other antidepressants clinically relevant. Int Clin Psychopharmacol. 2009;24:111–118. doi: 10.1097/YIC.0b013e32832a8eb2. [DOI] [PubMed] [Google Scholar]
- 45.Boulenger JP, Huusom AK, Florea I, Baekdal T, Sarchiapone M. A comparative study of the efficacy of long-term treatment with escitalopram and paroxetine in severely depressed patients. Curr Med Res Opin. 2006;22:1331–1341. doi: 10.1185/030079906X115513. [DOI] [PubMed] [Google Scholar]
- 46.Moore N, Verdoux H, Fantino B. Prospective, multicentre, randomized, double-blind study of the efficacy of escitalopram versus citalopram in outpatient treatment of major depressive disorder. Int Clin Psychopharmacol. 2005;20:131–137. doi: 10.1097/00004850-200505000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Chen F, Larsen MB, Neubauer HA, Sanchez C, Plenge P, Wiborg O. Characterization of an allosteric citalopram-binding site at the serotonin transporter. J Neurochem. 2005;92:21–28. doi: 10.1111/j.1471-4159.2004.02835.x. [DOI] [PubMed] [Google Scholar]
- 48.Sanchez C, Bogeso KP, Ebert B, Reines EH, Braestrup C. Escitalopram versus citalopram: The surprising role of the R-enantiomer. Psychopharmacology (Berl) 2004;174:163–176. doi: 10.1007/s00213-004-1865-z. [DOI] [PubMed] [Google Scholar]
- 49.El Mansari M, Sanchez C, Chouvet G, Renaud B, Haddjeri N. Effects of acute and long-term administration of escitalopram and citalopram on serotonin neurotransmission: An in vivo electrophysiological study in rat brain. Neuropsychopharmacology. 2005;30:1269–1277. doi: 10.1038/sj.npp.1300686. [DOI] [PubMed] [Google Scholar]
- 50.Mnie-Filali O, El Mansari M, Espana A, Sanchez C, Haddjeri N. Allosteric modulation of the effects of the 5-HT reuptake inhibitor escitalopram on the rat hippocampal synaptic plasticity. Neurosci Lett. 2006;395:23–27. doi: 10.1016/j.neulet.2005.10.044. [DOI] [PubMed] [Google Scholar]
- 51.Mnie-Filali O, Faure C, Mansari ME, et al. R-citalopram prevents the neuronal adaptive changes induced by escitalopram. Neuroreport. 2007;18:1553–1556. doi: 10.1097/WNR.0b013e3282f04047. [DOI] [PubMed] [Google Scholar]
- 52.Storustovu S, Sanchez C, Porzgen P, et al. R-citalopram functionally antagonises escitalopram in vivo and in vitro: Evidence for kinetic interaction at the serotonin transporter. Br J Pharmacol. 2004;142:172–180. doi: 10.1038/sj.bjp.0705738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen F, Larsen MB, Sanchez C, Wiborg O. The S-enantiomer of R, S-citalopram, increases inhibitor binding to the human serotonin transporter by an allosteric mechanism. Comparison with other serotonin transporter inhibitors. Eur Neuropsychopharmacol. 2005;15:193–198. doi: 10.1016/j.euroneuro.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 54.Serretti A, Chiesa A. Treatment-emergent sexual dysfunction related to antidepressants: A meta-analysis. J Clin Psychopharmacol. 2009;29:259–266. doi: 10.1097/JCP.0b013e3181a5233f. [DOI] [PubMed] [Google Scholar]
- 55.Lancon C, Sapin C, Note I, Farisse J. Comparison of escitalopram and citalopram in outpatients with severe major depressive disorder: A prospective, naturalistic 8-week study. Int J Psychiatry Clin Pract. 2006;10:131–137. doi: 10.1080/13651500600579290. [DOI] [PubMed] [Google Scholar]