Abstract
Background:
Studies on clinical features of catatonia in the Indian population are few in number.
Aim:
To study the phenomenology, clinical profile and treatment response of subjects admitted to the psychiatry inpatient with catatonia.
Materials and Methods:
Detailed treatment records of all the inpatients were scanned for the period January 2004 to December 2008. Patients with catatonia (diagnosed as two symptoms as per the Bush Francis Catatonia Rating scale) were included.
Results:
During the study period, 1056 subjects were admitted in the inpatient unit, of which 51 (4.8% of the total admissions) had catatonic features and had been rated on the Bush Francis Catatonia Rating scale. The mean age of the sample was 30.02 years (SD=14.6; range 13-69), with an almost equal gender ratio. Most of the patients presenting with catatonia were diagnosed as having psychotic disorders (40; 74.8%), of which the most common diagnosis was schizophrenia (27; 52.9%) of the catatonic subtype (20; 39.2%). Three subjects with primary diagnosis of a psychotic disorder had comorbid depression. Other diagnoses included mood disorders (7; 13.72%) and organic brain syndromes (04; 7.9%). According to the Bush Francis Rating scale, the common signs and symptoms exhibited by the subjects were mutism (94.1%), followed by immobility/stupor (78.5%), staring (78.4%), negativism (74.5%), rigidity (63%) and posturing/catalepsy (61.8%). All the patients were initially treated with lorazepam. Electroconvulsive therapy was required in most cases (42; 82.35%).
Conclusion:
The common symptoms of catatonia are mutism, immobility/stupor, staring, posturing, negativism and rigidity. The most common underlying psychiatric diagnosis was schizophrenia.
Keywords: Catatonia, ECT, lorazepam, phenomenology
INTRODUCTION
Karl Ludwig Kahlbaum first described catatonia as a “symptom complex,”[1] and it is currently viewed as a syndrome of motor abnormality associated with disorders of mood, behavior or thought. It is reported to occur as a presenting complaint in 7-15% of acute psychiatric inpatients.[2,3]
Over the years, more than 40 signs have been ascribed to catatonia, with an overlap of definitions. Patients with catatonia may be hypokinetic, stuporous or hyperkinetic; they may posture, exhibit stereotypies and mannerisms, stare or grimace. They may be mute, echo words or phrases or verbigerate. Their behavior may also be stimulus bound in negativism, automatic obedience, waxy flexibility, mitgehen, gegenhalten or echo phenomena.[1] The most common signs are mutism, posturing, negativism, staring, rigidity and echo phenomena. These signs occur in two principal forms: a retarded-stuporous variety and an excited-delirious variety.[4] According to the DSM-IV criteria, the presence of two prominent signs for at least 24 h is sufficient for the diagnosis of catatonia. The diagnosis may be confirmed by symptomatic improvement after the acute administration of a challenge dose of lorazepam or amobarbital. Confirmation after lorazepam is reported in approximately 80% of the patients with catatonia.[4,5]
There are very few studies that have assessed the phenomenology of catatonia in India. Most of the data is in the form of case reports, in which catatonia due to various causes has been reported,[6–21]and some have reported use of electroconvulsive therapy (ECT) and lorazepam.[11,22–27]Cases of periodic catatonia have also been reported from India.[6,10]
An earlier study from India showed that catatonic signs were present in nearly 40% inpatients diagnosed with mood and psychotic disorders, a significant proportion of which were schizophrenia and acute and transient psychotic disorders.[28] However, the recent studies are in concordance with the general belief that the incidence of catatonia is declining as they have reported a lower incidence of catatonia in an inpatient setting. This is highlighted by a study reporting catatonic syndrome in 11% patients, following screening of 138 inpatients with the Bush Francis Catatonia Rating scale (BFCRS).[29] Another cross-cultural study reported an incidence of 13.5% in consecutively admitted patients in India, which was higher than that seen in Wales (9.6%).[30] The only study from India that has evaluated the incidence of catatonia in children and adolescents has reported an incidence of 5.5% in the entire study sample and 17.7% in patients with affective and nonaffective psychotic disorders.[31]
0 Some of these studies have also reported the phenomenology of catatonia. Seethalaksmi et al,[29] reported mutism (87.5% incidence) to be the most common symptom of catatonic syndrome. In the cross-cultural study by Chalasani et al,[30] it was found that retarded catatonia (12.5%) and some classic signs like posturing, catalepsy, staring and stupor were more frequent among psychiatric admissions in India than in Wales. In the study on children and adolescents, it was reported that stupor/immobility, mutism, posturing/catalepsy, rigidity and negativism were present in affective as well as nonaffective psychoses, but signs such as excitation, echo phenomenon and verbigeration were seen only in affective disorders.[31] Atypical presentation like recurrent opisthotonus has also been reported.[20]
One of the recent Indian studies showed that patients with catatonic schizophrenia require fewer ECTs than those with noncatatonic schizophrenia.[32] In another study from India, it was reported that a significant proportion (93%) of patients with catatonia showed a marked immediate response to lorazepam, with 75% showing sustained improvement.[29]
As evident from the above review, few studies have been conducted in India with the aim to explore the phenomenology and treatment response in patients presenting with catatonia. However, there is no data from north India with respect to the phenomenology of catatonia. With these lacunae in mind, an exploratory retrospective chart review was undertaken of inpatients presenting with catatonia with the aim of studying the phenomenology, clinical profile and treatment response.
MATERIALS AND METHODS
Setting
The Department of Psychiatry at the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, is a general hospital psychiatric unit with inpatient and outpatient facilities in a tertiary care, multi-disciplinary teaching hospital. All patients admitted in the inpatient are routinely assessed through a detailed semistructured interview. Brief data (patients name, age, gender, psychiatry number, diagnosis, duration of stay, treatment given, outcome, etc.) of all the patients admitted to the inpatient unit are also entered in an admission register.
Psychiatric diagnosis, primary and comorbid, is based on the International Classification of Diseases and Related Health Problems -tenth revision (ICD-10).[33] Depending on the diagnosis, all subjects are routinely rated on various instruments (e.g., Positive and Negative Symptom scale, Hamilton Depression Rating scale, Young Mania Rating scale, BFCRS, Abnormal Involuntary Movement scale, etc.) to assess the severity of psychopathology at baseline and progress of the same during the inpatient stay. All the ratings are carried out by a trainee psychiatrist (Junior Resident) under the supervision of a qualified psychiatrist (Senior Resident) and are reviewed by the consultant in-charge of the case and, if required, necessary modifications are made in the ratings before being finally accepted for the clinical monitoring of the patients. In general, all patients presenting with catatonia are initially given a trial of parental/oral lorazepam for 3-4 days at doses ranging from 4 to 12 mg/day along with other psychotropics as per the requirement. Patients who do not respond to lorazepam trial or relapse even after receiving adequate trial of lorazepam are given ECT.
The present study is a retrospective chart review of all patients who were admitted to the psychiatry inpatient unit with catatonic symptoms between January 2004 and December 2008, all of whom had been rated on the BFCRS. During the study period, 1056 subjects were admitted in the inpatient unit, of which 51 (4.8% of the total admissions) had catatonic features and had been rated on the BFCRS. For the current study, the treatment records of these patients were screened for their sociodemographic profile, diagnosis, scores on the BRCRS at admission and treatment given during admission.
Bush Francis Catatonia Rating scale
This is a 23-item clinician rated scale. The initial 14 items are used for screening and include most of the common signs like immobility/stupor, mutism, posturing and staring as well as several classical signs (e.g., waxy flexibility, mannerisms, echophenomena). It has a high reliability.[34] The diagnosis of catatonia is made when two or more features are present for more than 24 h. Each item is scored on a 0-4-point scale to rate the severity of catatonia.
Statistical analyses
Categorical variables were analyzed using frequency and percentages. Continuous variables were analyzed by mean and standard deviation.
Ethical considerations
The study was approved by the Departmental Research Committee.
RESULTS
Sociodemographic profile
The mean age of the study population was 30.02±14.6 years (13-69 years), with an almost equal gender distribution (male-26; female-25). The majority of the patients were single (n=30, 58.8%), studied till matric or less (n=35; 68.6%), unemployed (n=15; 29.4%) or homemakers (n=15; 29.4%) or students (n=10; 19.6%), belonging to Hindu (n=37; 72.5%), nuclear (n=25; 49%) or joint (n=16; 31.4%) families. Patients from urban (n=27; 52.9%) and rural (n=24; 47.1%) backgrounds were almost equally represented.
Clinical profile
Psychotic disorder (n=40; 74.8%) was the most common diagnosis in the study population, with schizophrenia (n=27; 52.9%) of the catatonic subtype (n=20; 39.2%) being the most common followed by undifferentiated (n=7; 13.72%) schizophrenia. Other psychotic disorders included subjects with acute and transient psychosis (n=7; 13.72%), delusional disorder (n=1; 1.96%), schizoaffective disorder (n=1; 1.96%) and psychosis NOS (n=1; 1.96%). Three subjects with primary diagnosis of a psychotic disorder (two diagnosed as schizophrenia and one diagnosed as delusional disorder) had comorbid severe depressive episodes. Other common psychiatric diagnosis included first episode depression (n=2; 3.9%), recurrent depressive disorder (n=1; 1.96%) and bipolar depression (n=4; 7.84%). In only four patients (7.9%) was catatonic syndrome attributed to organic disorders like febrile encephalitis (n=1; 1.96%), Wilson's disease (n=2; 3.98%) and other medical conditions (n=1; 1.96%).
Rating on the Bush Francis Catatonia Rating scale
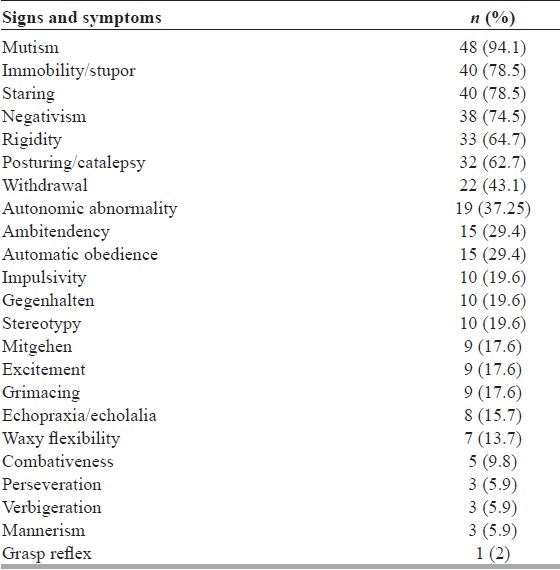
At the initial assessment, the mean BFCRS score was 15.33±5.33 (range, 4-31). The commonly seen catatonic symptoms included mutism, immobility/stupor, staring, negativism, rigidity, posturing/catalepsy and withdrawal. The less commonly seen catatonic symptoms included autonomic abnormality, ambitendency, automatic obedience, impulsivity, gegenhalten, stereotypy, mitgehen, excitement, grimacing, echopraxia/echolalia, waxy flexibility, combativeness, perseveration, verbigeration, mannerism and grasp reflex [Table 1].
Table 1.
Phenomenology of catatonia as assessed on the Bush Francis Catatonia Rating scale at baseline
Treatment
Although no fixed regiment was followed, all patients were initially given lorazepam at the dose of, usually, 4-12 mg/day either in the form of intravenous/intramuscular injections or a combination of intravenous/intramuscular and oral medication, with the dose per day not exceeding 12 mg/day. Depending on the response, lorazepam was gradually tapered off over the period of 2-3 weeks. Those subjects who relapsed when lorazepam was being tapered off, who partially responded to the above described lorazepam trial or who did not respond to the lorazepam trial were given ECT for catatonia. Except for nine (17.65%) patients who responded to lorazepam, ECT (n=42; 82.35%) was required in most cases. During the study period, overall, 260 subjects received ECT, of which catatonia was an indication for ECT in 16.21% of the subjects. There was no significant difference in number of ECT received in the index episode in subjects who had catatonia (10.76±4.43) and those who did not have catatonia (9.17±5.12). In all patients, catatonic symptoms resolved with ECT (post-ECT catatonia scores, 0.14±0.52; range 0-3).
Additionally, most of the patients (96.1%) were treated with antipsychotics. Among the various antipsychotic, atypical antipsychotics (n=40; 78.4%) were more commonly used. Olanzapine (n=17; 33.3%) was the most commonly used antipsychotic medication followed by risperidone (n=12; 23.5%), quetiapine (n=5; 9.8%), clozapine (n=3; 5.9%), amisulpiride (n=2; 3.9%) and aripiprazole (n=1; 2%). Antidepressants were used in nine patients (17.6%), with venlafaxine (n=4; 7.8%) being the most commonly used agent, whereas tricyclic antidepressants and selective serotonin reuptake inhibitors were used in two subjects each and mirtazapine was used in one subject. Four patients (7.8%) received mood stabilizers, with an equal distribution of lithium and sodium valproate.
DISCUSSION
The present study was a chart review of inpatients presenting with catatonia with the aim to study the phenomenology, clinical profile and treatment response. Frequency of catatonic signs as found in the present study is similar to previous studies that have shown that the retarded symptoms of catatonia, such as withdrawal, stupor, mutism, posturing and negativism, are more common than other signs and symptoms.[30,35]Our findings also support the previous finding of Chalasani et al,[30] who found that retarded catatonia was more frequently seen in India, in contrast to Wales.
In our study, most of the subjects were young and the mean age of the sample was about 30 years; the most common diagnosis being schizophrenia followed by acute and transient psychotic disorders. Only four cases had catatonia of organic origin. All these findings are consistent with that reported by Chalasani et al,[30] for subjects from India.
Studies including those from India have shown that lorazepam is useful in the management of catatonia.[5,36–38] However, some studies refute the benefit of lorazepam in the acute management of catatonia.[39] In our study, lorazepam was used for the management of catatonia. However, the results were not as gratifying as those reported in some other studies.[5,29]Although lorazepam was initially given to all the patients, only nine patients responded completely to this treatment regime. This apparently lower response rate to lorazepam in our study could be due to various reasons. Most studies that have described the effectiveness of lorazepam in the management of catatonia have considered lorazepam as effective in the treatment of catatonia when it resolved the catatonic signs to one or zero on BFCRS.[5,39]In the current study, when lorazepam did not lead to complete resolution of catatonic features, patients were started on ECT. Second, no standard protocol was followed for the use of lorazepam and, hence, it is quite possible that lack of standardization can lead to poor results. Thus, it is possible that the response to lorazepam in Indian patients requiring hospitalization might be poorer compared with that in other parts of the world due to a difference in their genetic makeup. Hence, prospective studies using standardized protocols to evaluate the efficacy of lorazepam in catatonia in an Indian setting might clarify these issues.
The use of ECT for the treatment of catatonia, irrespective of diagnosis, is supported by the literature, demonstrating the effectiveness of ECT in catatonia due to various psychiatric disorders and organic causes.[39–41]In our study, ECT was used in more than 80% of the subjects to treat catatonia, and all the subjects improved with ECT. In one study, it was shown that patients with catatonic schizophrenia require a lesser number of ECTs compared with those without catatonia.[32] However, we did not find any significant difference in the number of ECTs required by those with and without catatonia.
Our study has some limitations. We included only those subjects whose clinical picture was dominated by catatonic signs and symptoms. This may have led to the exclusion of psychotic patients having symptoms of more than one type (paranoid, heberphrenic schizophrenia and catatonia), with others symptoms being more dominant in the clinical picture as a result of which they had not been rated on the BFCRS. This limitation also possibly explains the low prevalence of subjects with affective disorders in this study. Another limitation of the study is the retrospective nature and also that we did not test the inter-rater reliability. Hence, the findings should be interpreted in this background. To conclude, our findings suggest that mutism, immobility/stupor, staring, negativism, rigidity, posturing/catalepsy and withdrawal are the common catatonic signs and symptoms seen in patients from India that respond to ECT.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Johnson J. Catatonia: The tension insanity. Br J Psychiatry. 1993;162:733–8. doi: 10.1192/bjp.162.6.733. [DOI] [PubMed] [Google Scholar]
- 2.Fink M, Taylor MA. Catatonia: Subtype of syndrome DSM (editorial) Am J Psychiatry. 2006;163:1875–6. doi: 10.1176/ajp.2006.163.11.1875. [DOI] [PubMed] [Google Scholar]
- 3.Takata T, Takaoka K, Fujigaki M. Catatonia in the elderly: A review. Int J Psychiatry Clin Prac. 2005;9:230–7. doi: 10.1080/13651500500240670. [DOI] [PubMed] [Google Scholar]
- 4.Fink M, Taylor MA. New York: Cambridge University Press; 2003. Catatonia: A clinician's guide to diagnosis and treatment; pp. 147–69. [Google Scholar]
- 5.Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia, II: Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137–43. doi: 10.1111/j.1600-0447.1996.tb09815.x. [DOI] [PubMed] [Google Scholar]
- 6.Jha BK, Reddy GC. Catatonia associated with uraemic encephalopathy. Indian J Psychiatry. 1968;10:95–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Gangadhar BN, Keshavan MS, Goswami U, Rao JV. Cortical venous thrombosis presenting as catatonia: A clinicopathological report. J Clin Psychiatry. 1983;4:109–10. [PubMed] [Google Scholar]
- 8.Desai NG, Patil NM, Gangadhar N, Pradhan N, Channabasavanna SM. Catatonia associated with uraemic encephalopathy. Indian J Psychiatry. 1984;26:95–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Daradkeh JK, Nasrallah NS. Lupus catatonia a case report. Pharmatherapeutica. 1987;5:142–4. [PubMed] [Google Scholar]
- 10.Singh G, Bhaduri AS. Periodic catatonia: A case report. Indian J Psychiatry. 1988;30:197–200. [PMC free article] [PubMed] [Google Scholar]
- 11.Nizamie SH, Khanna R, Sharma LN. Catatonia and hyponatremia: A case report. Indian J Pyschiatry. 1991;33:153–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Prabhakar S, Malhotra RM, Goel DS. Rabies presenting as catatonic stupor. J Assoc Physicians India. 1992;40:272–3. [PubMed] [Google Scholar]
- 13.Jain A, Sharma AK, Kar P. Subdural hematoma presenting as catatonia. J Assoc Physicians India. 1993;41:615. [PubMed] [Google Scholar]
- 14.Chalela J, Kattah J. Catatonia due to central pontine and extrapontine myelinolysis: Case report. J Neurol Neurosurg Psychiatry. 1999;67:692–3. doi: 10.1136/jnnp.67.5.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jagadheesan K, Nizamie SH, Thakur A. Catatonia in obsessive compulsive disorder. Indian J Psychiatry. 2002;44:179–82. [PMC free article] [PubMed] [Google Scholar]
- 16.Berry N, Sagar R, Tripathi BM. Catatonia and other psychiatric symptoms with vitamin B12 deficiency. Acta Psychiatr Scand. 2003;108:156–9. doi: 10.1034/j.1600-0447.2003.00089.x. [DOI] [PubMed] [Google Scholar]
- 17.Kumar P, Jain MK. Progressive multifocal leucoencephalopathy in AIDS camouflaged with catatonia: A wolf in sheep's clothing. Indian J Psychiatry. 2006;48:69–71. doi: 10.4103/0019-5545.31625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muralidharan K, Rajkumar RP, Rao SA, Benegal V. Catatonia as a presenting feature of alcohol withdrawal: A Case Report. Prim Care Companion J Clin Psychiatry. 2007;9:465. doi: 10.4088/pcc.v09n0611a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arora M, Praharaj SK. Butterfly glioma of corpus callosum presenting as catatonia. World J Biol Psychiatry. 2007;8:54–5. doi: 10.1080/15622970600960116. [DOI] [PubMed] [Google Scholar]
- 20.Manjunatha N, Mehta UM, John P. Recurrent opisthotonus in catatonia: An atypical presentation. Indian J Med Sci. 2009;63:512–6. [PubMed] [Google Scholar]
- 21.Srivastava A, Gupta A, Murthy P, Murali T. Catatonia and multiple pressure ulcers: A rare complication in psychiatric setting. Indian J Psychiatry. 2009;51:206–8. doi: 10.4103/0019-5545.55091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dabholkar PD. Use of ECT in hysterical catatonia.A case report and discussion. Br J Psychiatry. 1988;153:246–7. doi: 10.1192/bjp.153.2.246. [DOI] [PubMed] [Google Scholar]
- 23.Thomas N, Suresh TR, Srinivasan TN. Electroconvulsive therapy in catatonia associated with pneumothorax. Indian J Psychiatry. 1994;36:91–2. [PMC free article] [PubMed] [Google Scholar]
- 24.Ahuja N. Organic catatonia: A review. Indian J Psychiatry. 2000;42:327–46. [PMC free article] [PubMed] [Google Scholar]
- 25.Thakur A, Dutta S, Jagadheesan K, Sinha VK. Electro convulsive therapy in pre-pubertal catatonia: A case study. Indian J Psychiatry. 2001;43:354–6. [PMC free article] [PubMed] [Google Scholar]
- 26.Manjunatha N, Saddichha S, Khess CR. Idiopathic recurrent catatonia needs maintenance lorazepam: Case report and review. Aust N Z J Psychiatry. 2007;41:625–7. doi: 10.1080/00048670701400032. [DOI] [PubMed] [Google Scholar]
- 27.Rao NP, Loganathan S, Prakash O, Varghese M. Use of electroconvulsive therapy for schizophrenia with comorbid Marfan syndrome. J ECT. 2009;25:276–7. doi: 10.1097/YCT.0b013e3181a09d69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banerjee A, Sharma LN. Catatonia incidence in acute psychiatric admissions. Indian J Psychiatry. 1995;37:35–40. [PMC free article] [PubMed] [Google Scholar]
- 29.Seethalakshmi R, Dhavale S, Suggu K, Dewan M. Catatonic syndrome: Importance of detection and treatment with lorazepam. Ann Clin Psychiatry. 2008;20:5–8. doi: 10.1080/10401230701844786. [DOI] [PubMed] [Google Scholar]
- 30.Chalasani P, Healy D, Morriss R. Presentation and frequency of catatonia in new admissions to two acute psychiatric admission units in India and Wales. Psychol Med. 2005;35:1667–75. doi: 10.1017/S0033291705005453. [DOI] [PubMed] [Google Scholar]
- 31.Thakur A, Jagadheesan K, Dutta S, Sinha VK. Incidence of catatonia in children and adolescents in a paediatric psychiatric clinic. Aust N Z J Psychiatry. 2003;37:200–3. doi: 10.1046/j.1440-1614.2003.01125.x. [DOI] [PubMed] [Google Scholar]
- 32.Thirthalli J, Phutane VH, Muralidharan K, Kumar CN, Munishwar B, Baspure P, et al. Does catatonic schizophrenia improve faster with electroconvulsive therapy than other subtypes of schizophrenia? World J Biol Psychiatry. 2009;10:772–7. doi: 10.1080/15622970902718782. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization. International Classification of Diseases. 10th revision. 1992. revision Geneva: World Health Organization;
- 34.Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93:129–36. doi: 10.1111/j.1600-0447.1996.tb09814.x. [DOI] [PubMed] [Google Scholar]
- 35.First MB, Spitzer RL, Gibbon M, Gibbon M, Williams , Janet BW. Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version. 2002 Patient edition (SCID-I/P) New York (NY): New York State Psychiatric Institute. [Google Scholar]
- 36.Schmider J, Standhart H, Deuschle M, Drancoli J, Heuser J. A double-blind comparison of lorazepam and oxazepam in psychomotor retardation and mutism. Biol Psychiatry. 1999;46:437–41. doi: 10.1016/s0006-3223(98)00312-6. [DOI] [PubMed] [Google Scholar]
- 37.Payee H, Chandrasekharan R, Raju GV. Catatonic Syndrome: Treatment response to Lorazepam. Indian J Psychiatry. 1999;41:49–53. [PMC free article] [PubMed] [Google Scholar]
- 38.Ungvari GS, Kau LS, Wai-Kwong T, Shing NF. The pharmacological treatment of catatonia: An overview. Eur Arch Psychiatry Clin Neurosci. 2001;251:s31–4. doi: 10.1007/pl00014198. [DOI] [PubMed] [Google Scholar]
- 39.Girish K, Gill NS. Electroconvulsive therapy in Lorazepam nonresponsive catatonia. Indian J Psychiatry. 2003;45:21–5. [PMC free article] [PubMed] [Google Scholar]
- 40.Rohland BM, Carroll BT, Jacob RG. ECT in the treatment of the catatonic syndrome. J Affect Disord. 1993;29:255–61. doi: 10.1016/0165-0327(93)90015-c. [DOI] [PubMed] [Google Scholar]
- 41.Benegal V, Hingorani S, Khanna S. Idiopathic catatonia: Validity of the concept. Psychopathology. 1993;26:41–6. doi: 10.1159/000284798. [DOI] [PubMed] [Google Scholar]


