Abstract
Schizophrenia is a common disorder, affecting approximately 1 out of every 100 people, with a typical onset during adolescence and early adulthood. The personal and societal costs of schizophrenia are extremely high. Prevention of schizophrenia, would offer substantial benefits to patients, their family members, and the community at large. The prodromal phase of schizophrenia has been recognized since the 19th century. At-risk individuals for psychosis and schizophrenia are the subjects who can provide information for intervention prior to development of frank psychosis. This approach is currently being investigated. The question remains, however, whether it can be a diagnostic category by itself. The proposal for including the risk syndrome is one of the recommendations by the working group on schizophrenia and psychotic disorders for the forthcoming DSM-V. There are differing views in academia regarding this proposal. Prior to becoming fully psychotic, a consistent literature demonstrates that patients generally had suffered from accelerating attenuated symptoms and distress. It is important that the prodromal phase be accurately recognized in order to accomplish the goal of prevention. We can then purposefully engage in early intervention aiming toward prevention. A recent strong resurgent interest in this area stems largely from two developments: First, the identification of the neurobiological deficit processes associated with the severity and chronicity of schizophrenia, and second, the development of reliable criteria for diagnosis. Although the general at-risk construct appears to offer great potential to advance both the treatment and research dealing with psychotic illnesses, it seems premature to many researchers to include the syndrome as an established entity in the text of the new DSM-V. It would be far more appropriate to include this proposed syndrome in the appendix and evaluate the many contemporary issues in future studies. The main issues involved in this discussion are the clinical validity of the syndrome, concern about stigma and unnecessary treatment, and need for responding to patients′ distress in addition to the ethical dilemma. In this review we examine the issue of inclusion of the risk syndrome as a diagnosis.
INTRODUCTION
Psychiatric diagnosis has acquired the status of quasi-legal documentation for mental health services and agencies. Its utility has gone far beyond “clinical diagnosis for treatment.” The concept of risk syndrome for schizophrenia has been thoroughly researched in the last 10 years or so. Significant advancement has been made in phenomenology, diagnostic criteria, classification, and neurobiology. The research of prodromal or at-risk or ultra high-risk states for psychosis has significantly contributed to the understanding of schizophrenia.[1] The scientific data about the psychosis risk syndrome have apparently matured and their proponents are ready for its inclusion in DSM-V as a diagnosis. This has generated debate in academia, support groups, and advocacy groups.[2,3]The main concern most of these stakeholders have is related to stigma, unnecessary treatment, and misuse of medications and labeling of at-risk individuals. We need to be mindful, in the process, not to do anything in which the interest of the “patient” is left out.[4] Prevention of schizophrenia, would offer substantial benefits to the patients, families, and the community at large. Identification of individuals at prodromal stages would provide clinicians an opportunity for preventive intervention. However the question is whether it is necessary to be a diagnostic category by itself. The proposal for including the risk syndrome is one of the recommendations by the working group on schizophrenia and psychotic disorders for the forthcoming DSM-V.[5] In this review we examine the issue of inclusion of the risk syndrome as a diagnosis. We first review the current status of research, which has led to this proposal. Thereafter we discuss the arguments in for, against, and alternatives for inclusion as a diagnosis. Finally, we provide a critical synthesis of opinions on this topic. Clearly more research, discussion, and understanding are required to reach a consensus.
On the right track but not quite there
Despite the advent of operational criteria, diagnosis in psychiatry continues to struggle for validity. One strategy which may help to establish predictive validity of clinical syndromes and phenotypes is to develop a clinical staging model in which early stages of illness are defined with later stages evolving from these in several different possible directions. While a certain degree of predictive validity must exist for progression, remission may occur in many cases at each stage. Such cases can also be described as false positives. The key is to avoid overtreatment of such false positives. The key task is to define the boundary for initial caseness and “need for care.” Much of our thinking links this to symptom severity and we assume for example that intensity and frequency of psychotic symptoms are the best way to define onset for psychotic illnesses including schizophrenia. Long-term follow up data from the Melbourne cohort of over 400 ultra-high risk cases show that while a minority of patients (29%) made the transition by 5 years to psychotic disorder, many others had persistent mental disorders and disability. The ultra high risk criteria proposed as the basis for the psychosis risk syndrome in DSM-V therefore have a substantial predictive power and validity for not only psychosis but also persistent psychiatric disorders of other kinds, notably affective disorders. This initial stage of clinical disorder is therefore non-specific. A further twist is that there may be other pathways to both psychotic and affective exit syndromes or later stages of disorder.
Overview: risk syndrome, early intervention and prevention of schizophrenia
The general principles and concepts of early identification
There is universal agreement that early intervention in schizophrenia produces better outcomes than later intervention. Consequently, the development of effective early intervention strategies is among the most important goals of schizophrenia research. Early intervention efforts currently focus on prodromal symptoms and show promise to ameliorate them. The larger goal in these efforts is to alter and prevent the development of psychosis and chronic, debilitating treatment-resistant problems. Although the realization of this goal remains in the future, the foundation for its success is being laid in the present. One of the most important steps needed to progress toward prevention is to identify the individuals who are at greatest risk to develop schizophrenia.
Schizophrenia in relation to genetic factors
There is no longer any doubt about the importance of genetic factors for influencing vulnerability for schizophrenia. Family studies have demonstrated that the biologic relatives of individuals with schizophrenia are at an increased risk for developing schizophrenia and related disorders, such as schizoaffective disorder, schizotypal personality disorder, and other non-affective psychoses,[6] Adoption and twin studies have allowed researchers to examine the extent to which this increased risk is due to genetic or common environmental factors. Adoption studies suggest a strong genetic influence, demonstrating that biologic but not adoptive relatives of schizophrenics are at an increased risk for the disorder. Biologic children of non-schizophrenics do not have a greater risk for developing schizophrenia when raised by schizophrenic adoptive parents. Twin studies have found that Monozygotic (MZ) twins have a greater concordance rate of schizophrenia (about 50%) compared with Dizygotic (DZ) twins (about 10%), reflecting genetic influence, and studies suggests that approximately 70% of the vulnerability to schizophrenia is due to genetic factors. Since the concordance rate of schizophrenia among identical twin pairs is not more than 50%, environmental factors must also influence risk of developing schizophrenia. Although family, twin, and adoption studies show that the etiology of schizophrenia is largely genetically driven, identifying susceptibility genes is challenging since many genes likely each contribute a small proportion of vulnerability.
Studies[7] identified eight putative susceptibility genes which contribute to the risk, with positive findings: catechol-O-methyltransferase (COMT), neuregulin (NRG1), dysbindin (DTNBP1), disrupted-in-schizophrenia 1 (DISC1), regulator of G-protein signaling (RGS4), metabotropic glutamate receptor-3 (GRM3; mGluR3), G72 (and DAAO), and KCNH2 (a human ether-a-go-go (ERG)-family potassium channel).[8]
Schizophrenia in relation to environmental factors
While evidence for genetic components in schizophrenia derives primarily from family, molecular and biological studies, evidence for environmental components originate from behavioral genetic studies as well as epidemiological analysis of risk factors. The percent risk for schizophrenia is correlated to the degree of relatedness of the individuals in a family. An identical twin of a patient with schizophrenia and a child with two schizophrenic parents have the highest risks. The environment in which a high-risk adoptee is brought up, including the environment of a child adopted away from a schizophrenic mother, has little effect on risk. This suggests strong evidence for the effect of genes, but one should also note that the morbid risk does not approach the theoretical predictions based on the percentage of shared genes alone. This phenomenon stresses the importance of environmental factors. Early environmental risk factors for schizophrenia include urban and winter birth, fetal malnutrition and hypoxia, and possibly prenatal viral infections; these early hazards have only a modest risk-increasing effect, and operate in the context of genetic risk. Preschizophrenic children are more likely to have minor psychomotor and cognitive problems; low IQ has a linear relationship with risk for schizophrenia. However, schizophrenia is not simply a neurodevelopmental disorder, because risk factors have been identified that have their effects proximal to the onset of psychosis: drug abuse, immigrant status, and social adversity and isolation,[9] though the risk of schizophrenia to the offspring of both the affected and unaffected twins in a discordant MZ pair is virtually identical.[10] The genetic predisposition is present in both twins but is expressed only in the twin who has undergone certain environmental experiences as well. Environmental components are either shared by individuals in the same household, (whether related or not) or unshared, in which case the latter can be unique even for MZ twins. The components of the environment include psychosocial, biological, and physical factors that the individual experiences from the moment of conception, through development, birth, and maturation.
MZ twins may experience different prenatal and perinatal factors, such as adequacy of the blood supply, position in the womb, and birth complications. Later, they may be subjected to different treatments by their parents or siblings and have different school environments and marital and occupational events or surroundings.[11,12]According to Cannon's statistical model[13] unique (unshared) environmental effects account for the entire non-genetic component of the variance in liability; there is no effect of shared experience. Environmental factors may have varied effects on individuals with different genotypes. Genotype-environment interactions may result from genetically mediated differences in sensitivity to environmental factors or environmentally mediated influences on gene expression.[14] A recent study shows familial clustering of increased stress-reactivity, suggesting common etiological influences, probably both genetic and environmental, underlying stress-reactivity in the siblings and patients[15] Gene-environment associations also suggest that individuals with particular genotypes may seek out or construct specific environments or, alternatively, that their parents with the same genetic lesion have sought out or created particular environments that are compatible with their genotype.
Prevention of schizophrenia
In the near future, progress toward the ultimate goal of prevention likely reflects progress in interim goals that include the following: (1) identify gene expression patterns of first-degree relatives. By analyzing the gene expression patterns of “normal” relatives of schizophrenia patients, we can circumvent the problems associated with the effects of the medications and identify areas of convergence and divergence with their affected relatives. (2) Apply bioinformatics methodologies. We need to incorporate the vast amounts of information being generated in the fields of bioinformatics, especially proteomics and the new fledgling field of metabolomics, to complement our genetic epidemiology studies; and (3) focus on early intervention. Increased genetic and epidemiologic information will allow us to move ever closer to our ultimate goal of preventing schizophrenia.
Characteristics of risk syndrome
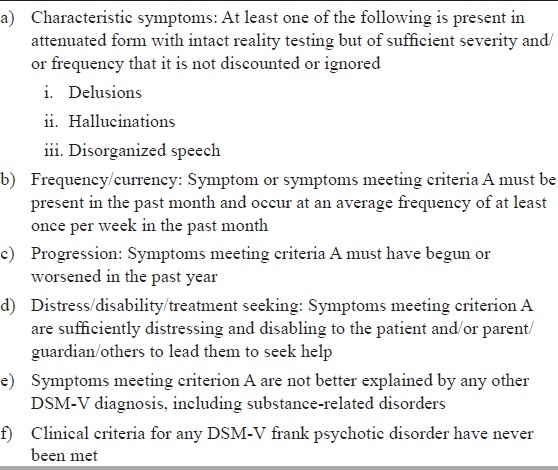
In order to prevent psychosis, the first step should be to identify the characteristics of risk syndrome for psychosis before its onset. Characteristic symptoms include delusions, hallucinations, and disorganized speech. We can then purposefully engage in early intervention aiming toward prevention. Currently, there are relatively reliable and valid research criteria for identifying risk syndrome for psychosis. By utilizing these criteria we can predict future occurrences of psychosis based on follow-up studies. These clinical criteria are given in Table 1.[16]
Table 1.
Proposed revision in DSM-5 Criteria for identifying attenuated psychotic symptoms syndrome
It is imperative that well-designed field trials involving clinicians be undertaken utilizing clinical criteria for risk syndrome. These field trials should test reliability of the clinical criteria in order to identify risk syndrome for psychosis among heath seeking subjects. In addition, comparison groups with other well-established disorders should be selected to test the specificity of the clinical criteria. When the field trials are complete and have successfully demonstrated their reliability and specificity, DSM-V should include Risk syndrome for psychosis for further refinement. This rigorous approach will prevent over-diagnosis and unnecessary treatment.
Attenuated psychotic symptoms syndrome: A reliable and valid diagnosis
A prodrome for psychosis has been recognized retrospectively for 100 years. Prior to becoming fully psychotic, a consistent literature demonstrates that patients generally had suffered from an accelerating pattern of specific attenuated positive symptoms, other non-specific symptoms, distress, and functional and cognitive impairment.
When we look prospectively, many patients who appear to be prodromal for psychosis go on to become psychotic, but many do not. However, if anything is to be done to help these patients before they develop frank psychosis, we have no option other than to think prospectively. Several terms have been proposed to describe patients who appear to be prodromal but may or may not become psychotic, and recently the term “risk syndrome” has been suggested.[3,4,17–23] Like the retrospectively identified prodrome, risk syndrome patients are also symptomatic, distressed, and functionally and cognitively impaired—that is, they are currently ill[24] even if they do not progress to psychosis. The DSM-V Psychosis Work Group prefers a name that emphasizes the current illness: Attenuated Psychotic Symptoms Syndrome, or APS Syndrome.
One research study from North America and one from Australia have both demonstrated statistically significant predictive validity of a risk syndrome diagnosis compared to the optimal control group. The optimal control patients are those referred for risk syndrome research evaluation who did not meet criteria. In the North American study[16] and analysis adjusting for loss to follow-up estimated that 40% of 303 patients developed full psychosis over 2.5 years. Only an estimated 4% of 135 help-seeking controls converted. In the Australian study,[25] 16% of 119 patients developed frank psychosis over 2 years, compared to only 1% of 173 help-seeking controls. Other studies demonstrate construct validity[17,26] diagnostic inter-rater reliability across 11 sites[27–29] and inter-rater reliability for severity of the positive symptoms required for the diagnosis.[22,26,28,30]
The proportion of false positive identifications is partly a function of the criteria themselves. The attenuated positive symptom (APS) syndrome criteria currently proposed for DSM-V are substantially less inclusive than current research criteria. Characteristic attentuated positive symptoms must meet these requirements: present in the past month and accelerating within the past year, associated with distress and impairment and help-seeking, and not better explained by other DSM-V diagnoses. The requirement for functional impairment is not part of current research criteria, but has been suggested by six large studies.[18,31–35] The proposed DSM-V criteria should yield higher conversion rates than the broader research criteria.
The proportion of false positive identifications is also partly a function of the population to which the criteria are applied. When we essentially screen for attenuated positive symptoms among the general population of patients rather than respond to referrals for specific concern about psychosis, conversion rates fall. “Yung and colleagues reported on the 2-year outcomes of conducting risk syndrome structured interviews on all patients entering the youth mental health system in their catchment area[25]. In previous studies of specific referral populations, roughly 40% of patients meeting criteria transitioned to psychosis within 2 years. Screening for the same criteria in a broader population yielded only 16% conversion rate." At least two of the explanations proposed by Yung and colleagues (earlier detection and higher proportions of false positives) and possibly also the third (changed treatment patterns) could be consequences of the evolved ascertainment methods. Since clinicians in actual practice generally focus primarily on the chief complaint, it is likely that the patients for whom a DSM-V APS syndrome diagnosis would be considered in clinical practice would have a risk more similar to that for a specific referral population than to that for a screened population.
The benefits of inclusion of a new APS syndrome category in DSM-V are two: (1) widespread community education about who does and does not meet risk syndrome criteria, and (2) promotion of more rapid and larger-scale treatment research. In the past 15 years the world community has managed to publish only four controlled trials[36–40] with a combined sample size of only 260 (<20/year). The risks of inclusion are also two: (1) stigma and (2) overmedication of false positive patients. Stigma can be managed through provider education, similar to the way investigators minimize stigma associated with participation in risk syndrome research. Overmedication can also be managed by provider education, and if we have a DSM-V diagnosis we will be able to acquire far more information with which to educate. The DSM-V proposal is substantially more helpful for these patients than the DSM-IV diagnostic set, and the risks of a DSM-V diagnosis are not necessarily greater than those associated with the DSM-IV diagnoses these patients now receive, such as psychosis NOS.
It is premature to consider a diagnosis in DSM-V?
Adding a new risk category to the DSM-V reflects a growing enthusiasm for the possibility that intervening prior to onset may impact the severity and course of psychosis. The prevention movement also brings mental illness more into line with the pre-emptive intervention strategies of many chronic physical illnesses, such as heart disease, diabetes, and cancer. This can be viewed as a major advance in the research and treatment of schizophrenia and related psychotic disorders. Nevertheless, caution about over-exuberance must be stressed. The field of prevention in psychosis is only about 15 years old, with dramatic research growth occurring mainly over the past 5 or so years. There are therefore many challenges and issues yet to be resolved before introducing this new clinical construct to a broad public, which will result from the inclusion of the proposed risk diagnosis into the main text of the DSM-V. Because information is so sparse about critical issues such as validity of the diagnostic criteria, long-term course of the syndrome, and the lack of an accepted treatment, inclusion in the DSM-V main text is controversial and many researchers, especially those who have conducted prodromal studies, maintain that it is premature to formalize the psychosis at-risk category as currently conceptualized by the DSM-V Psychosis Work Group.[3,18,19]
One problem is the lack of information about conversion rates. At the moment, conversion rates, which reflect the accuracy with which the diagnosis predicts future psychosis, appear to be changing quite substantially. This is indicated by the substantial range in conversion rates reported, which was close to 50% in the early studies[28,41] but, more recently, has fallen to about 20% in several long-running prospective programs.[3,18] As a result, the false positive rate (i.e., those individuals meeting risk criteria but who never become ill) steadily increases and is now considered to be about 80%[42] Furthermore, in one of the few studies addressing outcome for those individuals who do not convert, substantial clinical improvement was observed over time.[43] Therefore, for most of the individuals, it is likely that APSS criteria will not be clinically or functionally meaningful in the long run.
Two major negative consequences of false positive identifications are stigma and unnecessary treatment. With regard to the first of these, stigma remains a major difficulty associated with mental illness despite years of public education and advocacy attempting to reduce it. There is no reason to expect this to be remedied in the near future and informing an adolescent or young adult that they are at risk for a severe, chronic, often incurable, form of mental illness is likely to have life-altering consequences.
Unnecessary medication is a second major problem associated with widespread false positive identifications. Prodromal research and treatment is very difficult, and correct identifications require a great deal of training and constant quality control, procedures that are very time and resource consuming and typically not feasible for community clinicians. The handful of clinical trials studying the preventive potential resulting from the early use of anti-psychotics that have been conducted over the past 10 years have been suggestive, but none have been conclusive[37,38] illustrating the difficulty of this research. There are also preliminary hints that anti-depressives[44] and, possibly, omega-3 fatty acids[36] might be of some preventive benefit. However, there is as yet no recommended treatment. In the absence of clear guidance, the fall back is likely to be anti-psychotics. If the use of anti-psychotics becomes standard in the absence of clinical trial information, and patients improve, then the assumption will be that improvement is due to medication (not necessarily true) and this in itself will increase anti-psychotic medication use, in many cases unnecessarily.
It should be noted that in the latest iteration of the DSM-V proposal,[45] the name of the proposed prodromal clinical entity has been changed from “psychosis risk syndrome” to “attenuated positive symptom syndrome” (APSS). This emphasizes the current symptoms, already present, rather than their potential for predicting future psychosis. As a result, concern about false positives in the sense of converting to psychosis is diminished, because everyone identified is symptomatic, distressed, and may need some type of treatment. However, this new approach has raised several new issues. The criteria defining the newly proposed “APSS” are more limited than those applied to the more traditional “prodromal or risk syndrome.” There are no data available to assess the validity of this new set of criteria and certainly no information about the longitudinal course of the syndrome. It is thus unclear how clinically significant this new diagnostic entity will be. This concern is heightened by the fact that the entity now appears to be a mild form of psychosis (though there is little evidence to substantiate this assumption), which will only increase the tendency to use anti-psychotics as the preferred treatment. As mentioned above, there is little conclusive evidence to support the benefits of anti-psychotic interventions and no information about possible exit strategies. Moreover, while reduced, the false positive issue is not completely resolved, since diagnosis of the proposed APSS syndrome is of unestablished reliability and, as mentioned, requires substantial training and continual monitoring. Field trials will only address these issues if they are truly done in the community and do not involve academic or research sites already familiar with the APSS construct. In addition, it is likely that as the APSS criteria become widely accepted throughout the treatment community as part of the new DSM-V, individuals with quite moderate or even fleeting symptoms will be evaluated as meeting APSS status, in turn, greatly extending a concept that has yet to be validated. This will, in effect, tend to dilute the construct, impact validity, and lead to an even greater number of unnecessarily medicated false positives.
In summary, while the general APSS construct appears to offer great potential to advance both the treatment and research dealing with psychotic illnesses, it seems premature to many researchers to include the syndrome as an established entity in the text of the new DSM-V. It would appear far more appropriate to include this proposed syndrome in the appendix and evaluate the many issues discussed above in future studies.
An argument for placing it in the appendix
With each iteration and revision of the Diagnostic and Statistical Manual for Mental Disorders, new disorders are proposed for inclusion within its text. For each of these proposals, a careful analysis of the risks and benefits of inclusion is warranted. Typically, the potential main benefit of inclusion of a diagnosis within the DSM is that suffering can be identified and treated. The psychosis risk syndrome additionally offers the promise of prevention beyond treatment. That is, the potential inclusion of the “psychosis risk syndrome” or “attenuated positive symptom syndrome” could lead not only to reducing current morbidity in young people who are grappling with disturbing changes in their thinking and behavior, but that there may additionally be the prospect of forestalling or preventing the onset of psychotic disorder, in particular schizophrenia, a worthy cause, as psychotic illness is the ninth leading cause of disability worldwide and causes much suffering for patients and families. The prevention of schizophrenia would be remarkable as it cannot be cured. Although a proportion of patients with schizophrenia do have successful remission of psychotic symptoms with treatment with primarily antidopaminergic agents, these medications have potentially serious side effects, lifelong treatment is typically indicated, and most patients have residual psychotic symptoms and relapses. Furthermore, many of the core deficits of schizophrenia, including its cognitive deficits, negative symptoms, and functional impairment, are very entrenched and difficult to treat. The real tragedy of schizophrenia for so many individuals with this illness is such that the impetus to understand its potential risk states is strong. Research into the putative prodrome is essential for understanding the pathophysiological mechanisms which underlie the development of serious psychotic illness. The promotion of research in this area would be greatly enhanced by including the syndrome and its operationalized criteria in the appendix of the DSM under “Criteria sets and axes provided for further study.” Its inclusion in the DSM would reflect the progress that has been made thus far in prodromal research worldwide in the past few decades, with the identification of putative biomarkers, the evaluation of potential treatments, and the descriptive phenomenology of the clinical risk state.
However, it may be premature to include the psychosis risk syndrome within the main text of the DSM because so much work remains to be done to understand this clinical state, and there remains insufficient understanding of the psychosis risk state, as knowledge is still incomplete as to the validity of the diagnosis.[19] To return to the construct of the risk--benefit analysis, which must be undertaken for consideration of any diagnosis within the DSM historically, there are significant risks in inclusion of the psychosis risk syndrome in the main text of the DSM, primarily related to the problem of “false positives,” rates of which are agreed upon to be certainly more than 50% and potentially as high as 90%.[19,36] High false positive rates in and of themselves are not necessarily problematic if the risks are small. For example, although most individuals with mild hypertension or elevated cholesterol do not develop coronary heart disease,[45] screening for these risk factors is widely accepted given that the potential benefits of early intervention are high and there is little risk associated with the recommended interventions, i.e. instituting lifestyle changes and taking statins and/or antihypertensive agents. However, with a psychosis risk syndrome, the main risks include stigma[22] and unnecessary medication exposure.[41] As for stigma, it is known that the label of serious mental illness, even accounting for concurrent symptoms, is associated with significant stigma, including internalized stigma (individuals see themselves as bad, defective, or unworthy), identity engulfment (individuals see the illness as a defining aspect of who they are, instead of as something they have), shame (the label is kept secret and concealed from others), and discrimination on the part of others, expressed as devaluation or unfair treatment.[46] It is an empirical question whether the label of psychosis risk would also have as much associated stigma, though it may be expected to, as teens and young adults are more sensitive to these stigmatizing effects than older adults.[3] As for antipsychotic exposure, prescribing patterns of psychiatrists worldwide suggest that antipsychotics will be used to treat the psychosis risk syndrome, despite the absence of a clear evidence base to do so and the prevalent adverse effects of weight gain (up to 8.8 kg)[37] and motor abnormalities (i.e. treatment-emergent akathisia in 8/15 patients receiving aripiprazole)[47] documented in clinical trials of putatively prodromal cohorts. Furthermore, as little or nothing is known about the long-term outcomes in individuals identified as at risk for psychosis, these young people may be prescribed antipsychotics indefinitely. This is particularly concerning, given that antipsychotic medications can pose significant risk to cardiovascular and general health.
In summary therefore, a cogent argument can be made for placing the psychosis risk syndrome within appendices of the DSM dedicated to research on criteria sets. There is precedent for the success of this strategy, as premenstrual dysphoric disorder (PMDD) was proposed for inclusion in the DSM-III-R[48] and then again for DSM-IV[49] with purported benefits including that recurrent premenstrual mood symptoms would be recognized by clinicians in women as psychiatric symptoms are appropriately treated, and not dismissed as “moodiness.” However, there were concerns raised as to the risk of stigmatizing women especially in the workplace, where they have been historically discriminated against. In weighing these benefits and risks, the DSM-IV Task Force decided that on balance it would be premature to add PMDD to the main body of DSM-IV, and instead included it in the appendix for “criteria sets and axes provided for future study” to encourage future research.[50] There is now a better understanding of PMDD with a range of treatments available, as it was included in the appendix of the DSM, and its diagnosis has not been indiscriminate and there has not been much adverse effect in terms of stigma.
DISCUSSION
Response to debate by William Carpenter: Chair, DSM-V, psychosis work group
As discussant, I should first point out that I chair the DSM-V Psychosis Work Group. A decision as to whether to recommend a diagnostic class for the attenuated psychotic symptom syndrome will not be made until 2012. Comments here are my own. The following may be considered established facts
Persons who develop psychotic illnesses usually manifest attenuated symptoms before full expression;
Behaviors similar to attenuated psychotic symptoms are not uncommon in the general population;
Early detection to treat what is wrong and prevent worsening is a time-honored principle in medicine.
Clinical criteria can be used to identify persons with attenuated psychotic symptoms who are at substantially elevated risk for progression to a psychotic illness. Validation data have been published.[17] Initial consideration for DSM-V has been presented[4] and the concept of a risk syndrome was considered[20] The subsequent debate as to the wisdom of including this construct in DSM-V has been spirited[51] including the 2010 presentations at the 163rd Annual meeting of the American psychiatric Association summarized above by the participants. Here I will note key issues of concern and how they might be addressed.
-
Concern: Extending pathology connotation to normal behavior with failure to distinguish disorder from normative behavior.
This concern is vitally important. Criteria for identifying a case must include disability, distress, and/or dysfunction. This is true for many mental disorders where symptoms are behaviors that may represent the extremes of normal and it is essential to judge the presence of disorder based on consequences of the behavior. Consider any of the anxiety or mood disorders for example.
In addition, help seeking is being considered as a criterion for diagnosis. Together with the distress/disability criteria, this is intended to extend an attenuated psychotic symptom syndrome diagnosis only to help seeking persons who will come into clinical care regardless of whether a new category exists.
-
Concern: The false positive rate is too high leading to unjustified clinical care.
The risk syndrome concept with parallels to hyperlipidemia is probably the wrong construct. A parallel with angina is more appropriate. Diagnosis and clinical care is warranted based on the attenuated symptoms and accompanying distress/disability. The risk reduction for a full psychotic outcome is highly desirable secondary prevention. In principle, this eliminated the false positive problem. All cases have the disorder, although only some are also on a path to more fully expressed psychosis. It is diagnosis and treatment of what is actually wrong, not risk detection and primary prevention.
-
Concern: The presence of an attenuated psychotic symptom syndrome in DSM-V will lead to excessive prescription of anti-psychotic medications with more harm than good.
Anti-psychotic drugs have very substantial adverse effects, and are not established as a treatment for attenuated psychotic symptoms nor are they established as a prevention of subsequent conversion to full psychosis. These drugs are already used in excess and the majority of young people receiving these medications at present do not have a psychotic diagnosis. The issue is whether establishing this diagnostic class will lead to better education and evidence-based clinical care or add to the ill-informed use of anti-psychotic drugs. This point is debatable and the outcome is unknown. Nonetheless, it seems likely that evidence for optimal clinical care will accrue more rapidly with focused attention to the problem.
Concern: Psychiatrists will label young people with this diagnosis with resultant harmful stigma.
This concern, often expressed by critics, is poorly presented. First of all, doctors do not label—they diagnose and provide care. It is inflammatory and misdirected to assert that mental disorder diagnoses are for the purpose of labeling. Stigma may be associated with receiving clinical care, but this is a very partial picture. Imagine a young person who becomes very suspicious, begins to withdraw from others, expresses odd ideas and has perceptual aberrations, and deteriorates in role performance. Self-esteem and identity are already challenged, and peers and family become concerned and relationships become strained. Stigma is already present before help seeking leads to a clinical contact. If clinical care begins, diagnosis and treatment plans are essential. If this increases stigma, the issue is whether a valid diagnosis or an [by definition] invalid diagnosis is more harmful. It is also hoped that clinical care will decrease the behaviors that lead to stigma.
As indicated above, the major concerns can be addressed with, at least, partial success. Highlighting the attenuated psychotic symptom syndrome as a diagnostic class in DSM-V may have other unintended negative consequences. On the other hand, the potential for substantially changing the longer term illness trajectory of individuals vulnerable to psychotic illness is of prime importance from a public health and humanitarian perspective. It is already established that treatment early in psychosis is more effective than later treatment. It has become clear that progression of cognitive impairments and structural brain changes occurs in the developmental phase of schizophrenia[52–55] and there may be a critical time point where intervention can alter the trajectory of chronic forms of psychotic disorders.
Finally, an intervention with efficacy for attenuated symptoms and secondary prevention of conversion to psychosis will dramatically alter the politics of this debate. The placebo controlled study of 3-omega fatty acid administered for 12 weeks in a cohort of high risk subjects[30] is illustrative. Over a 1 year period, the 12 weeks experimental compound reduced attenuated symptoms and was associated with a conversion to psychosis in 4.7% compared to placebo where the conversion rate was 27%. If this finding is replicated, few would argue that psychiatry should not identify cases and provide evidence-based treatment.
CONCLUSION
Identification of individuals at the prodromal stage of illness (i.e. prior to the onset of schizophrenia-level symptoms) would offer clinicians the opportunity to provide preventive interventions. Research in this area has been encouraging. Valid clinical criteria for diagnosis have been developed and search for biomarkers is expected to aid the diagnostic specificity. A recent strong resurgent interest in this area stems largely from two developments, first the neurobiological deficit processes associated with the severity and chronicity of schizophrenia and the second, development of reliable criteria for diagnosis.[32] It has also been shown that symptoms can be minimized by administration of atypical antipsychotic medication and Omega fatty acid during the prodromal period.[56] These findings show that individuals at high risk for psychosis can be identified with some reliability which provides hope for prevention.[25,35,57]
The evidence for efficacy of pharmacological and psychosocial intervention for both, to prevent conversion to psychosis and to minimize the severity of psychosis, needs to be strengthened. A consensus among the public and the professionals can only emerge with more research findings. There is enough ground to start navigating the presence of “ARS” in the diagnostic category however to decide its exact position within the rubric of diagnosis remains a challenge. Merely the presence of ARS as a diagnosis may not be helpful if it is not well received and acceptable to clinicians, researchers, and care-givers. It is yet to be seen how clinicians receive it. It is expected that the results of field trial shall be of great significance to help reach a decision. New changes are difficult to be accepted at the very onset. With the passage of time, experience, and constructive discussion, opinions change. We hope the change would be for benefit of people suffering from schizophrenia and psychotic disorders.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Correll CU, Hauser M, Auther AM, Cornblatt BA. Research in people with psychosis risk syndrome: A review of the current evidence and future directions. J Child Psychol Psychiatry. 2010;51:390–431. doi: 10.1111/j.1469-7610.2010.02235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrivastava A. Should “risk syndrome for psychosis” be included as a diagnosis in DSM-V? World Psychiatry. 2010;9:123. doi: 10.1002/j.2051-5545.2010.tb00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yung AR, Nelson B, Thompson AD, Wood SJ. Should a “Risk Syndrome for Psychosis” be included in the DSMV? Schizophr Res. 2010;120:7–15. doi: 10.1016/j.schres.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Carpenter WT. “Editorial: Anticipating DSM-V: Should psychosis risk become a diagnostic class?”. Schizophr Bull. 2009;35:841–3. doi: 10.1093/schbul/sbp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oosthuizen P, Emsley R, Niehaus D, Koen L. The multidimensional assessment of psychopathology in mood and psychotic disorders. A proposal for Axis II in DSM-V/ICD-11. Afr J Psychiatry (Johannesbg) 2008;11:260–3. [PubMed] [Google Scholar]
- 6.Tsuang MT, Stone WS, Faraone SV. Schizophrenia: A review of genetic studies. Harv Rev Psychiatry. 1999;7:185–207. [PubMed] [Google Scholar]
- 7.Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: On the matter of their convergence. Mol Psychiatry. 2005;10:40–68. doi: 10.1038/sj.mp.4001558. [DOI] [PubMed] [Google Scholar]
- 8.Huffaker SJ, Chen J, Nicodemus KK, Sambataro F, Yang F, Mattay V, et al. A primate-specific, brain isoform of KCNH2 affects cortical physiology, cognition, neuronal repolarization and risk of schizophrenia. Nat Med. 2009;15:509–18. doi: 10.1038/nm.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly J, Murray RM. What risk factors tell us about the causes of schizophrenia and related psychoses. Curr Psychiatry Rep. 2000;2:378–85. doi: 10.1007/s11920-000-0019-1. [DOI] [PubMed] [Google Scholar]
- 10.Kringlen E, Cramer G. Offspring of monozygotic twins discordant for schizophrenia. Arch Gen Psychiatry. 1989;46:873–7. doi: 10.1001/archpsyc.1989.01810100015003. [DOI] [PubMed] [Google Scholar]
- 11.Pike A, Plomin R. Importance of nonshared environmental factors for childhood and adolescent psychopathology. J Am Acad Child Adolesc Psychiatry. 1996;35:560–70. doi: 10.1097/00004583-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Reiss D, Plomin R, Hetherington EM. Genetics and psychiatry: An unheralded window on the environment. Am J Psychiatry. 1991;148:283–91. doi: 10.1176/ajp.148.3.283. [DOI] [PubMed] [Google Scholar]
- 13.Cannon TD, Kaprio J, Lonnqvist J, Huttunen M, Koskenvuo M. The genetic epidemiology of schizophrenia in a Finnish twin cohort: A population-based modeling study. Arch Gen Psychiatry. 1998;55:67–74. doi: 10.1001/archpsyc.55.1.67. [DOI] [PubMed] [Google Scholar]
- 14.Van Os J, Marcelis M. The ecogenetics of schizophrenia: A review. Schizophr Res. 1998;32:127–35. doi: 10.1016/s0920-9964(98)00049-8. [DOI] [PubMed] [Google Scholar]
- 15.Lataster T, Collip D, Lardinois M, van Os J, Myin-Germeys I. Evidence for a familial correlation between increased reactivity to stress and positive psychotic symptoms. Acta Psychiatr Scand [In Press] 2010 doi: 10.1111/j.1600-0447.2010.01566.x. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association; DSM-5 proposal. [last accessed on 2010 Aug 19]. Available from: http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=412 .
- 17.Woods SW, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Validity of the prodromal risk syndrome for first psychosis: Findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009;35:894–908. doi: 10.1093/schbul/sbp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruhrmann S, Schultze-Lutter F, Klosterkotter J. Probably at-risk, but certainly ill - Advocating the introduction of a psychosis spectrum disorder in DSM-V. Schizophr Res. 2010;120:23–37. doi: 10.1016/j.schres.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 19.Corcoran C, First M, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: A risk-benefit analysis. Schizophr Res. 2010;120:16–22. doi: 10.1016/j.schres.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heckers S. Who is at risk for a psychotic disorder? Schizophr Bull. 2009;35:847–50. doi: 10.1093/schbul/sbp078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woods SW, Walsh BC, Saksa JR, McGlashan TH. The case for including Attenuated Psychotic Symptoms Syndrome in DSM-5 as a psychosis risk syndrome. Schizophr Res [In Press] 2010 doi: 10.1016/j.schres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang LH, Wonpat-Borja AJ, Opler MG, Corcoran CM. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: An empirical question. Schizophr Res. 2010;120:42–8. doi: 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGorry PD. Risk syndromes, clinical staging and DSM V: New diagnostic infrastructure for early intervention in psychiatry. Schizophr Res. 2010;120:49–53. doi: 10.1016/j.schres.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 24.Woods SW, Miller TJ, McGlashan TH. The “prodromal” patient: Both symptomatic and at-risk. CNS Spectr. 2001;6:223–32. doi: 10.1017/s1092852900008609. [DOI] [PubMed] [Google Scholar]
- 25.Yung AR, Nelson B, Stanford C, Simmons MB, Cosgrave EM, Killackey E, et al. Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr Res. 2008;105:10–7. doi: 10.1016/j.schres.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: The Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–71. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- 27.Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, et al. North American Prodrome Longitudinal Study: A collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–72. doi: 10.1093/schbul/sbl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–15. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- 29.Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: Preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–5. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 30.Lencz T, Smith CW, Auther AM, Correll CU, Cornblatt BA. The assessment of “prodromal schizophrenia”: Unresolved issues and future directions. Schizophr Bull. 2003;29:717–28. doi: 10.1093/oxfordjournals.schbul.a007041. [DOI] [PubMed] [Google Scholar]
- 31.Addington J, Perkins DO, Woods SW. The PREDICT study. 2010 [Google Scholar]
- 32.Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: A multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with ‘at-risk mental states’. Schizophr Res. 2004;71:227–37. doi: 10.1016/j.schres.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: Psychopathology and clinical features. Schizophr Res. 2004;67:131–42. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- 35.Yung AR, Stanford C, Cosgrave E, Killackey E, Phillips L, Nelson B, et al. Testing the ultra high risk (prodromal) criteria for the prediction of psychosis in a clinical sample of young people. Schizophr Res. 2006;84:57–66. doi: 10.1016/j.schres.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 36.Amminger GP, Schafer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: A randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67:146–54. doi: 10.1001/archgenpsychiatry.2009.192. [DOI] [PubMed] [Google Scholar]
- 37.McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;163:790–9. doi: 10.1176/ajp.2006.163.5.790. [DOI] [PubMed] [Google Scholar]
- 38.McGorry PD, Yung AF, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, et al. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002;59:921–8. doi: 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]
- 39.Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, et al. Cognitive therapy for the prevention of psychosis in people at ultra-high risk.Randomized controlled trial. Br J Psychiatry. 2004;185:291–7. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- 40.Drake RJ, Lewis SW. Valuing prodromal psychosis: What do we get and what is the price? Schizophr Res. 2010;120:38–41. doi: 10.1016/j.schres.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 41.Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr Res. 2003;60:21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- 42.Simon AE, Umbricht D. High remission rates from an initial ultra-high risk state for psychosis. Schizophr Res. 2010;116:168–72. doi: 10.1016/j.schres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 43.Cornblatt BA, Lencz T, Smith CW, Olsen R, Auther AM, Nakayama E, et al. Can antidepressants be used to treat the schizophrenia prodrome.Results of a prospective, naturalistic treatment study of adolescents? J Clin Psychiatry. 2007;68:546–57. doi: 10.4088/jcp.v68n0410. [DOI] [PubMed] [Google Scholar]
- 44.DSM-5. [last accessed on 2010 Aug 16]. Available from: http://www.dsm5.org/Pages/Default.aspx .
- 45.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 46.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–85. [Google Scholar]
- 47.Woods SW, Tully EM, Walsh BC, Hawkins KA, Callahan JL, Cohen SJ, et al. Aripiprazole in the treatment of the psychosis prodrome: An open-label pilot study. Br J Psychiatry. 2007;51:96–101. doi: 10.1192/bjp.191.51.s96. [DOI] [PubMed] [Google Scholar]
- 48.Spitzer R, Severino S, Williams B, Parry B. Late luteal phase dysphoric disorder and DSM-III-R. Am J Psychiatry. 1989;146:892–7. doi: 10.1176/ajp.146.7.892. [DOI] [PubMed] [Google Scholar]
- 49.Severino S. Premenstrual dysphoric disorder: Controversies surrounding the diagnosis. Harv Rev Psychiatry. 1996;3:293–5. doi: 10.3109/10673229609017198. [DOI] [PubMed] [Google Scholar]
- 50.Gold J. Late luteal phase dysphoric disorder: A final overview. In: Widiger T, Frances A, Pincus H, Ross R, First M, editors. DSM-IV Sourcebook. Washington: DC: American Psychiatric Association; 1998. pp. 1035–46. [Google Scholar]
- 51.Live Discussion: Is the Risk Syndrome for Psychosis Risky Business? Schizophrenia Research forum. [last accessed on 2010 Aug 19]. Available from: http://www.schizophreniaforum.org/for/live/transcript.asp?liveID=68 .
- 52.Seidman LJ, Giuliano AJ, Meyer EC, Addington J, Cadenhead KS, Cannon TD, et al. Neuropsychology of the prodrome to psychosis in the NAPLS consortium: Relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010;67:578–88. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arango C, Kahn R. Progressive brain changes in schizophrenia. Schizophr Bull. 2008;34:310–1. doi: 10.1093/schbul/sbm166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lawrie SM, McIntosh AM, Hall J, Owens DG, Johnstone EC. Brain structure and function changes during the development of schizophrenia: The evidence from studies of subjects at increased genetic risk. Schizophr Bull. 2008;34:330–40. doi: 10.1093/schbul/sbm158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wood SJ, Pantelis C, Velakoulis D, Yücel M, Fornito A, McGorry PD. Progressive changes in the development toward schizophrenia: Studies in subjects at increased symptomatic risk. Schizophr Bull. 2008;34:322–9. doi: 10.1093/schbul/sbm149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walker EF, Cornblatt BA, Addington J, Cadenhead KS, Cannon TD, McGlashan TH, et al. The relation of antipsychotic and antidepressant medication with baseline symptoms and symptom progression: A naturalistic study of the North American Prodrome Longitudinal Sample. Schizophr Res. 2009;115:50–7. doi: 10.1016/j.schres.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Riecher-Rössler A, Gschwandtner U, Aston J, Borgwardt S, Drewe M, Fuhr P, et al. The Basel early-detection-of-psychosis (FEPSY)-study: Design and preliminary results. Acta Psychiatr Scand. 2007;115:114–25. doi: 10.1111/j.1600-0447.2006.00854.x. [DOI] [PubMed] [Google Scholar]


