Abstract
Many different chromosomal translocations occur in man at chromosome 11q23 in acute leukaemias. Molecular analyses revealed that the MLL gene (also called ALL–1, HRX or HTRX) is broken by the translocations, causing fusion with genes from other chromosomes. The diversity of MLL fusion partners poses a dilemma about the function of the fusion proteins in tumour development. The consequence of MLL truncation and fusion has been analysed by joining exon 8 of Mll with the bacterial lacZ gene using homologous recombination in mouse embryonic stem cells. We show that this fusion is sufficient to cause embryonic stem cell-derived acute leukaemias in chimeric mice, and these tumours occur with long latency compared with those found in MLL–Af9 chimeric mice. These findings indicate that an MLL fusion protein can contribute to tumorigenesis, even if the fusion partner has no known pathogenic role. Thus, truncation and fusion of MLL can be sufficient for tumorigenesis, regardless of the fusion partner.
Keywords: ALL-1/cancer/chromosomal translocations/leukaemia/trithorax
Introduction
Chromosomal translocations are involved in the development of tumours by activation of oncogenes (reviewed in Rabbitts, 1994). Chromosome 11q23 is important as translocations occur here in both acute myeloid and lymphoblastic leukaemias (Rowley, 1993; Bernard and Berger, 1995; Rubnitz et al., 1996; Look, 1997; Gilliland, 1998) as well as in therapy-related leukaemias (DeVore et al., 1989; Pui et al., 1989; Cimino et al., 1997; Nasr et al., 1997; Rowley et al., 1997; Sobulo et al., 1997; Atlas et al., 1998; Felix, 1998). Molecular cloning of various translocation breakpoints revealed a gene called MLL (also called ALL-1, HRX or HTRX) in which the translocations occur (Ziemin-van der Poel et al., 1991; Djabali et al., 1992; Gu et al., 1992; Morgan et al., 1992; Tkachuk et al., 1992; Thirman et al., 1993). The affected region of the MLL gene is fairly small, around exon 8, but the chromosomal translocations result in fusion with a range of genes from other chromosomes. The diversity of the MLL fusion partners is very broad, ranging from putative transcription factors, ABL-binding proteins to septins (reviewed in DiMartino and Cleary, 1999). There is no obvious common feature of these fusion partners apparent from sequences alone, and in addition, some would be expected to be in the nucleus and others in the cytoplasm of cells, at least in their normal context.
Thus, the diversity of MLL partners raises questions about any possible function of the fusion proteins in dictating tumour phenotype. It is possible that the chromosomal translocations occur in committed cells, which become a tumour of that lineage as a result of the chromosomal translocations, or that they occur in early progenitors and thus contribute to (i.e. help specify) the phenotype of the final tumour by virtue of the fusion partner. An alternative possibility is that the chromosomal translocations usually occur in non-committed cells and the default pathway is to the myeloid lineage, which is the most common phenotype for MLL-associated tumours (DiMartino and Cleary, 1999). The occurrence of a lymphoid tumour may require a specific fusion for specificity of the lineage, as may be the case with the MLL–AF4 fusion. Some model systems have been established to assess the biological role of various MLL gene fusions. The HRX–ENL (MLL–ENL) fusion encoded by a retrovirus caused myeloproliferation and myeloid tumours (Lavau et al., 1997; Slany et al., 1998) and similarly homologous recombination ‘knock-in’ of AF9 into Mll caused acute myeloid leukaemia (AML) (Corral et al., 1996) preceded by myeloproliferation (Dobson et al., 1999). These suggest gain-of-function features of MLL-mediated tumorigenesis. However, in the self-fusion of ALL1 (MLL) there is a duplication of MLL, suggesting that the phenotypic effect might be production of a dominant-negative protein in this case (Schichman et al., 1994, 1995). In addition, an artificially created truncation of Mll at exon 8 (Mll–myc tag) in mice failed to show any influence on haematopoietic differentiation nor on tumour propensity (Corral et al., 1996). This, and the self-fusion of MLL, suggested that addition of material to the N-terminal portion of MLL might be able to elicit a tumorigenic effect, perhaps by stabilizing a truncated MLL protein or via protein interactions. In an attempt to assess diversity of the Mll fusions, we have used β-galactosidase as an Mll fusion partner in vivo. This enzyme has been extensively used in transgenic mouse and gene targeting experiments and has no demonstrated role in tumour formation. Accordingly, we have fused exon 8 of Mll with the lacZ gene by homologous recombination in embryonic stem (ES) cells (herein called Mll–lacZ) and used these ES cells to create chimeric mice. We found that this Mll–lacZ fusion gene was sufficient to cause leukaemia in chimeric mice and that ES cell-derived acute leukaemias arose among Mll–lacZ chimeric mice with long latency, compared with Mll–AF9 chimeric mice.
Results
Fusion of lacZ with Mll exon 8 by homologous recombination
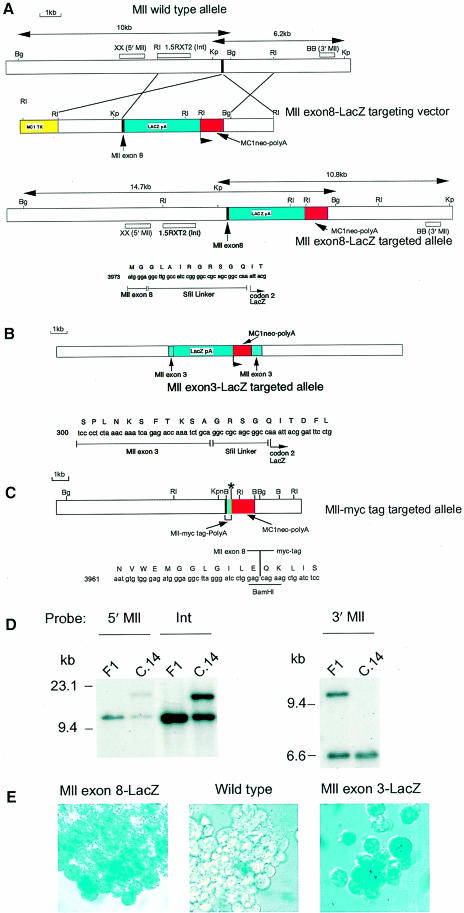
We constructed a knock-in ES cell targeting vector designed to fuse the lacZ gene into exon 8 of the endogenous Mll gene, which would result in the synthesis of an Mll–β-galactosidase fusion protein. Figure 1A–C shows the predicted organization of the targeted knock-in allele (Figure 1A, Mll–exon8–lacZ) compared with Mll–exon3–lacZ (previously called AT–lac; Corral et al., 1996) and Mll–myc tag. Homologous recombination of the Mll–lacZ targeting vector was carried out in ES cells and filter hybridization analysis of DNA from three clones (clone 14 is shown in Figure 1D as an example) confirmed the integrity of the targeting events using external probes on the 5′ and 3′ side of the targeting region and confirmation of a single insertion with an internal probe (Figure 1D).
Fig. 1. Mll gene targeting lacZ fusion constructs and β–galactosidase expression. (A) The Mll–exon8–lacZ targeting construct. The top map represents the Mll wild-type allele, indicating the position of exon 8 (black box) and positions of probes used to evaluate the gene targeting. Below this is a map of the Mll–exon8–lacZ targeting construct indicating the location of the LacZ fusion (blue box) in Mll exon 8, together with the MC1-neo-pA resistance gene (red box) (located downstream of the Mll–lacZ fusion gene). The MC1-tk-pA cassette (Thomas and Capecchi, 1987) [encoding the HSV thymidine kinase gene (yellow box)] is upstream of the fusion gene to allow negative selection of non-homologous integrations. The regions of homology between the Mll–exon8–lacZ targeting construct and the germ-line Mll gene are indicated. The bottom map indicates the expected organization of the Mll locus in the targeted allele together with the junctional sequence between Mll exon 8 and the lacZ gene fusion, including the SfiI linker, which was incorporated at the BamHI site to facilitate insertion of the lacZ-MC1-neo-pA cassette. The positions of the three DNA probes used to assess the gene targeting are indicated [XX, 5′ Mll; 1.5RXT2, internal (Int); BB, 3′ Mll]. (B) Organization of the Mll–exon3–lacZ targeted allele (previously AT-lac; Corral et al., 1996) and the junctional sequence between Mll exon 3 and the lacZ gene fusion. (C) Organization of the Mll–myc tag targeted allele (previously Mll–myc; Corral et al., 1996) and the junctional sequence between Mll exon 8 and the myc epitope tag fusion. (D) Southern filter hybridization of DNA from ES cells with targeted Mll–exon8–lacZ alleles. Three independent targeted ES clones were derived, two made in E14 ES cells (clones 14 and 24) and one in CCB ES cells (clone 118). Filter hybridization of clone 14 is shown for representation, in comparison with wild-type (F1 mouse kidney) DNA. Genomic DNA was digested with either BglII or KpnI. BglII-digested DNA was hybridized with the probe XX (5′ Mll) from outside the targeting vector and with the probe p1.5RXT2 (Int), which is located internally in the targeting vector. KpnI-digested DNA was hybridized with the probe BB (3′ Mll) from outside the targeting vector. In each case, the lower band represents the germ-line band and the larger band the targeted allele). Confirmation that a single insertion had occurred in each cell line was obtained by re-probing with a neo probe (data not shown). (E) β-galactosidase staining of targeted ES cells. ES cells targeted with either Mll–exon8–lacZ clone 14, Mll–exon3–lacZ or wild-type E14 ES cells were prepared and fixed with 2% formaldehyde/0.2% glutaraldehyde before staining for 48 h with X-gal solution. Cells were transferred to glass slides for photography. Both Mll–exon8–lacZ- and Mll–exon3–lacZ-targeted ES cells stain blue with X-gal.
The integrity and function of the Mll–lacZ fusion gene were established by analysis of β–galactosidase enzyme activity in ES cell cultures. We compared the expression of the Mll–exon3–lacZ (Corral et al., 1996) and Mll–exon8–lacZ fusion genes in ES cells by histochemical analysis of β–galactosidase protein activity in comparison with wild-type ES cells. Both the Mll–exon8–lacZ and Mll–exon3–lacZ ES cells express β–galactosidase (Figure 1E). Mll–exon8–lacZ therefore represents a phenotypic truncation of the Mll gene in which functional Mll fusion protein is made. We used these Mll–lacZ-targeted ES cells to generate chimeric mice and these mice were monitored for the occurrence of tumours over a 20 month period. A cohort of 43 chimeras was established with the targeted Mll–lacZ clones. A full post-mortem examination was performed during a period of 20 months on all mice that developed symptoms. In those cases where leukaemia or lymphoma was found, histological analysis and fluorescent antibody cell sorter (FACS) analysis of surface antigen expression were conducted. At the designated end of the experiment, all surviving mice were examined to determine any pathological features. The control groups were of two different types: (i) a cohort of negative controls comprising C57/Bl6 mice or chimeric mice made by injecting E14 ES cells with a single Lmo2 null allele (C320 cells; Yamada et al., 1998); and (ii) a cohort of Mll–myc tag mice.
Mll–lacZ mice develop haematopoietic malignancies
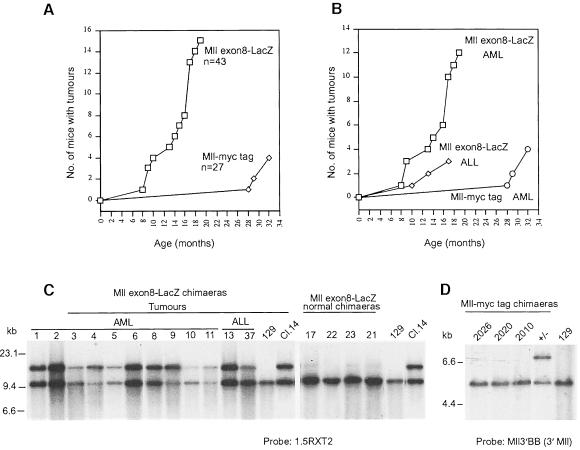
Mll–lacZ fusion mice were found to be prone to developing haematopoietic malignancies (Figure 2A). About one-third of the mice developed ES cell-derived leukaemias prior to 14 months. Fifteen Mll–lacZ mice developed leukaemia, of which 12 had AML and three had acute lymphoblastic leukaemia (ALL) or lymphoma (Figure 2B; see below). Filter hybridization of spleen tumour DNA was conducted to determine the presence of the Mll-targeted allele to determine whether the tumours were of ES cell or blastocyst origin. This analysis demonstrated that all the Mll–lacZ mouse tumours were of ES cell origin as the tumour DNA samples had the targeted Mll allele plus germ-line allele (Figure 2C). In contrast, the spleen DNA of four Mll–lacZ mice lacking detectable tumours showed predominantly germ-line Mll alleles (Figure 2C). The Mll–lacZ chimeric mice that did not develop leukaemia were not low chimeras, as most of these Mll–lacZ mice had high levels of coat chimerism (Figure 3D). Furthermore, the Mll–lacZ tumour DNAs had variable ratios of targeted to germ-line alleles due to the chimeric origin of these mice. Interestingly, in two samples the targeted allele seemed more intense than the germ-line allele (Figure 2C, numbers 4 and 9), indicative of loss of chromosomal material including the normal Mll allele from the non-targeted chromosome in these tumours. Unfortunately, no karyotype data are available for these tumours and we cannot therefore assess the extent of this putative loss.
Fig. 2. Tumour incidence in Mll–lacZ mice. Tumour incidence was monitored in cohorts of mice and when signs of indolence or unhealthy coat appeared, animals were killed and post-mortems carried out. (A) Data showing incidence of Mll–lacZ mice with detectable tumours compared with a cohort of Mll–myc tag mice (plotted as numbers of mice with time in months). The cohort size of the Mll–lacZ mice was 43 and that of the Mll–myc tag mice was 27. (B) Data showing the incidence of AML versus ALL within cohorts of Mll–lacZ and Mll–myc tag mice. Distinct forms of disease were found to be AML or ALL and lymphoma in the groups of mice as indicated. (C) Southern filter hybridization of DNA from Mll–lacZ chimeric animals with acute leukaemia. DNA was prepared from the spleen of the chimeras indicated (1–6 and 8–11 diagnosed with AML and 13 and 37 diagnosed with ALL), or chimeras not afflicted with discernible disease (17, 22, 23 and 21). DNA was digested with BglII, separated on 0.8% agarose alongside 129 liver DNA and DNA from Mll–lacZ ES clone 14, both digested with BglII. After transfer to nylon membranes, hybridization was carried out with 32P-labelled probe 1.5RXT2. The upper band represents the targeted allele (found in clone 14) and the lower band represents the germ-line allele. (D) Southern filter hybridization of DNA from Mll–myc tag chimeric animals with acute leukaemia. DNA was prepared from the spleen of the chimeras indicated (2026, 2020, 2010 diagnosed with AML) digested with KpnI, separated on 0.8% agarose alongside 129 liver DNA and DNA from an Mll–myc tag heterozygous mouse. After transfer to nylon membranes, hybridization was carried out with 32P-labelled probe BB (3′ Mll probe). The upper band represents the targeted allele (found in clone 14) and the lower band represents the germ-line allele.
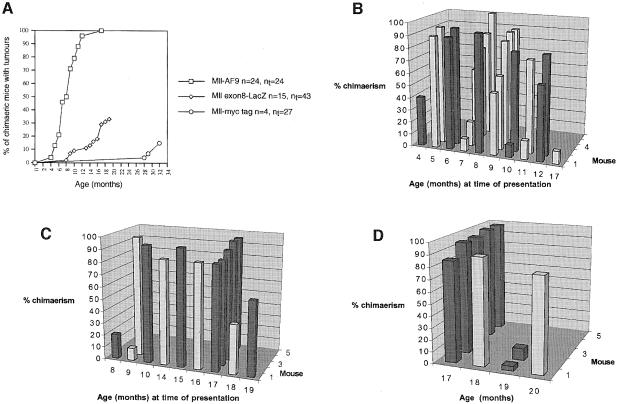
Fig. 3. Relationship between chimerism and tumour incidence in Mll–lacZ mice. Comparison of tumour incidence and coat colour chimerism in Mll–lacZ and Mll–AF9 mice. (A) Comparative tumour incidence in the cohort of chimeric mice made with the Mll–lacZ ES cells and cohorts of Mll–myc tag and Mll–AF9 chimeric mice. n, number of mice that developed tumours; nt, number of mice in the cohort. (B) Histograms showing the estimated coat colour chimerism in mice derived from injection of targeted ES cells with Mll–AF9 and time of leukaemia incidence. (C) Histograms showing the estimated coat colour chimerism in mice derived from injection of targeted ES cells with Mll–lacZ and time of leukaemia incidence. (D) Histograms showing the level of estimated coat colour chimerism in those Mll–lacZ mice that were culled for post-mortem examination without symptoms or pathology of leukaemia.
In confirmation of previous observations (Corral et al., 1996), we found no tumours arising in the Mll–myc tag mice during the 20 month experimental period (Figure 2A). However, four tumours did arise [all AML, Figure 2B] in 34 months. DNA filter hybridization analysis of these tumours failed to reveal targeted alleles in the tumour DNA, so we conclude that none of these tumours were of ES cell origin (Figure 2D) and these presumably represent the low, sporadic incidence of leukaemia in the C57/Bl6 strain over a 3-year period. It should be stressed that none of the Mll–myc chimeras developed leukaemia within the designated experimental period (20 months).
Longer latency of tumorigenesis in Mll–lacZ chimeras
We have compared the incidence and latency of tumours in Mll–lacZ chimeras with a cohort of chimeric mice developed from ES cells with an Mll–AF9 knock-in gene fusion (Corral et al., 1996). All the Mll–AF9 chimeras developed leukaemia (Figure 3A) with 50% having died by ∼8 months. The penetrance for the Mll–lacZ fusion mice is lower, with only 35% developing leukaemia, starting at 8 months and ending at 20 months (Figure 3A). The difference in tumour occurrence in Mll–AF9 and Mll–lacZ mice is apparently not attributable to different levels of chimerism. The ES cell contribution to chimerism was assessed by coat colour difference between 129 and C57/Bl6 strains. Figure 3B and C shows histograms of coat colour chimerism compared with age of leukaemia detection. These data show that there is no relationship between level of coat colour chimerism and tumour onset in either Mll–AF9 or Mll–exon8–lacZ groups.
Although we could not assess bone marrow chimerism in the live animals, the difference in coat colour chimerism indicates that the difference in leukaemia latency in the two groups is due to the targeted alleles, rather than merely different chimeric levels in the bone marrow. In addition, this conclusion is supported by the finding that the majority of Mll–Af9 chimeras develop tumours before 12 months, irrespective of chimerism. Finally, examination of chimerism in Mll–lacZ mice with no signs of leukaemia showed that the survivors at 17 months of age or more were, with two exceptions, high chimeras (Figure 3D). As every tumour in the Mll–lacZ group had a high ES cell contribution (Figure 2C), a direct effect of the Mll–lacZ allele is therefore implicated in tumorigenesis.
Mll–lacZ chimeric mice develop acute leukaemias
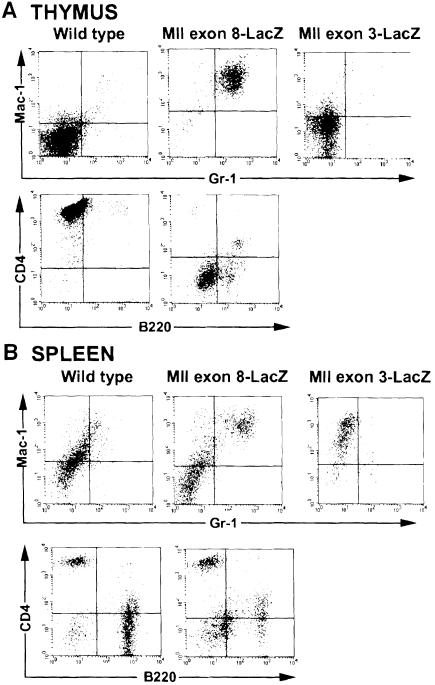
Mll–lacZ mice with haematological disease generally had an enlarged thymus, splenomegaly, hepatomegaly and pale kidneys. Twelve mice developed AML (Figure 2B). Three mice developed lymphoid disease, of which two were lymphoblastic lymphomas and one was ALL. In the control groups, the Mll–myc tag mice with late onset non-ES-derived tumours had AML (Figure 2B). The majority of Mll–lacZ tumours were Gr-1/Mac-1 double-positive cell type, indicating a myeloid lineage origin. FACS analyses were carried out with spleen and thymus cells of Mll–lacZ tumour-bearing mice and compared with phenotypically normal Mll–exon3–lacZ and wild-type mice (Figure 4). In the case shown, the Mll–lacZ mouse thymus is almost completely populated by Mac-1/Gr-1 double-positive tumour cells compared with the control thymi, which have few Mac-1/Gr-1 double-positive cells (Figure 4A). Similarly, the spleen of the Mll–lacZ mouse is infiltrated with Mac-1+/Gr-1+ cells (Figure 4B). From 10 Mll–lacZ tumour-bearing mice examined in detail, all but one had thymus cells expressing the Mac-1 antigen. We conclude, therefore, that the majority of tumours are in the myeloid lineage.
Fig. 4. FACS analysis of tumours from Mll–lacZ mice. Single-cell suspensions were made from spleen and thymus of an Mll–lacZ mouse (mouse number 6) with symptoms of disease and from Mll–exon3–lacZ or wild-type mice. Cells were stained with an anti-Mac–1 antibody coupled with PE together with an anti-Gr–1 antibody coupled with FITC or with an anti-CD4 antibody coupled with PE together with an anti-B220 antibody coupled with FITC. The markers were Gr–1, Mac–1 (alone or together) to detect myeloid populations, and CD4 or B220 to detect T- or B-cell populations, respectively. (A) Thymus cell populations; (B) spleen cell populations.
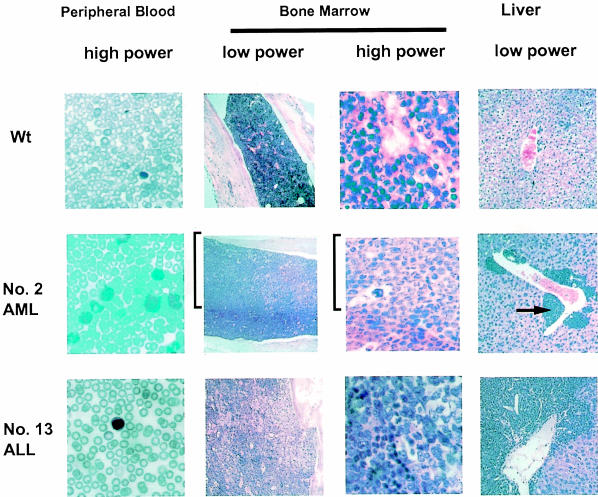
This classification of the malignancies was consolidated by histological analysis of the bone marrow, liver, spleen and peripheral blood. The bone marrow was typically found to have layers of malignant myeloid cells with increased numbers of circulating myeloblasts in blood (Figure 5). Most of the afflicted Mll–lacZ mice also had extensive perivascular infiltration of the abnormal myeloblasts in liver (e.g. Figure 5, mouse 2) and similar extensive infiltrates in the spleen. In all cases, we observed marked leukaemic cell infiltration in the bone marrow, liver and peripheral blood and, to a lesser extent, in the spleen (data not shown).
Fig. 5. Histology of haematological tumours arising in Mll–lacZ mice. Tissues were dissected and fixed in 10% formalin. Paraffin sections were prepared and stained with H&E. Blood films were stained with MGG. Comparison of tissues from Mll–lacZ mice with those from a normal C57/Bl6 wild-type mouse. Mll–lacZ mouse number 2 had AML and number 13 had ALL. The tissues from the Mll–lacZ mouse 2 show infiltration with myeloblastic tumour cells, e.g. the arrow indicates the location of the myeloblasts around a blood vessel in the liver of the Mll–lacZ mouse. These myeloid tumour cells are located next to and within the centrilobular vein. A band of myeloblasts (bracketed region) is seen adjacent to a layer of darker normal cells in the bone marrow. Mll–lacZ mouse number 13 had a lymphoblastic lymphoma with few lymphoid cells in peripheral blood, with patches of tumour cells in the bone marrow but large amounts of tumour cells surrounding the veins in liver. Low or high power magnifications are indicated.
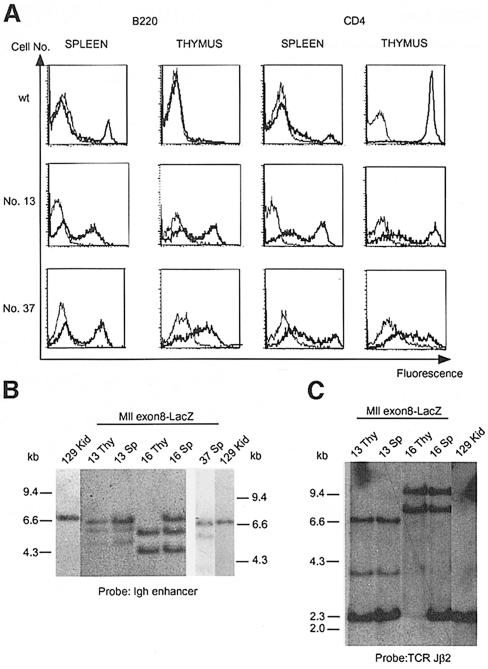
A small number of Mll–lacZ knock-in mice developed lymphoid tumours. Histology of these tumours revealed few circulating lymphoblasts in blood but pronounced swathes of abnormal cells in bone marrow and extensive perivascular deposits in liver (Figure 5, mouse 13). FACS analysis of tumours from two ALL-bearing mice (mice 13 and 37) showed that these expressed the B–cell marker antigen B220 in both spleen and thymus (Figure 6A). Unexpectedly, tumour cells in these mice also expressed the T–cell marker CD4 (Figure 6A) suggesting a mixed lineage cell type. This was further examined by clonality filter hybridization assays of immunoglobulin (Ig) and T–cell receptor (TCR) gene rearrangement. Figure 6B shows the hybridization patterns of DNA from spleen and thymus from mice 13, 16 and 37, each of which had a diagnosed lymphoid tumour. All three tumour DNA samples exhibited clonal rearrangements of the Ig heavy chain gene on one (Figure 6B, mouse 37) or both alleles (mice 13 and 16). When these same DNA samples were examined with a TCR β–chain probe, mice 13 and 16 showed clonal TCR gene rearrangements, in addition to Ig rearrangements (Figure 6C). Mouse 37 did not exhibit rearranged TCR alleles (data not shown). Thus, all three of these Mll–lacZ tumours are clonal lymphoid tumours and two of the three samples have two attributes of mixed lymphocyte lineage. While we have no experimental evidence of clonality of the AML tumours, it is reasonable to assume that they are clonal as there is a long latency before their occurrence. It thus seems very likely that in both Mll–AF9 and Mll–lacZ, secondary mutations in other genes (e.g. undetermined tumour suppressor genes) are necessary for overt tumours to occur.
Fig. 6. Clonality of ALL tumours arising in Mll–lacZ chimeras. Three animals from the Mll–lacZ cohort developed ALL according to post-mortem examination and histological analysis. The spleen and thymus cells from these mice were isolated for FACS analysis of lymphoid surface marker analysis (A), and DNA prepared for hybridization analysis of the rearrangement status of Ig heavy chain genes (B) and TCR genes (C). (A) Spleen and thymus cells were prepared from a C57/Bl6 mouse (control) and Mll–lacZ tumour mice numbers 13 and 37. The cells were incubated with antibodies recognizing B220 and CD4 antigens. The stained cells were analysed on a FACSCALIBUR instrument. The thinner line represents the signal obtained with an isotype control for B220 or CD4, respectively. The thick line represents the signal obtained with stained mouse cells. (B) Autoradiograph of a filter hybridization using an IgH-chain enhancer probe (Neuberger et al., 1989). Spleen and thymus DNA from Mll–lacZ mice numbers 13, 16 and 37 (ALL tumours) were digested with EcoRI (compared with 129 kidney DNA) prior to gel separation, transfer to nylon and hybridization. The DNA shows similar rearrangement patterns between spleen and thymus in each mouse. Each of these ALL-bearing Mll–lacZ has clonal IgH rearrangements. (C) Autoradiograph of a filter hybridization using a TCR Jβ2 probe (Malissen et al., 1984). Spleen and thymus DNA from Mll–lacZ mice numbers 13 and 16 were digested with EcoRI (compared with 129 kidney DNA) prior to gel separation, transfer to nylon and hybridization. The DNA shows similar rearrangement patterns between spleen and thymus in each Mll–lacZ mouse. Mll–lacZ mouse 37 had no evidence of TCR rearrangement (data not shown). Autoradiography was for 16 h.
Discussion
Mll fusion protein variability and possible functions in leukaemogenesis
Our results show that the stable expression of a truncated Mll (truncated where many chromosomal translocations occur in man) contributes to the development of leukaemia in mice, regardless of the fusion partner. The latency period prior to tumour appearance in the Mll–lacZ fusion mice appears longer than that observed with the Mll–AF9 fusions (Corral et al., 1996; Dobson et al., 1999). These data argue that there are at least two constituents to MLL-mediated tumorigenesis. One is the effect of the removal of MLL sequences after the truncation of the gene, which may create a dominant-negative form (Prasad et al., 1994; Schichman et al., 1994, 1995). The second is the positive contribution of gaining specific fusion partners. The faster rate at which tumours develop in mice with Mll–AF9 fusion genes points to a further biological role for the Mll–AF9 protein fusion in tumorigenesis. These data are consistent with in vitro transfection studies with a construct encoding a truncated MLL protein (Joh et al., 1996), which produced an inhibition of differentiation and responsiveness to GCSF in 32Dc13 cells as well as gain-of-function features proposed for the ENL (chromosome 19) fusion partner of MLL (Lavau et al., 1997; Slany et al., 1998).
Clonality and latency of mouse tumours with Mll fusions
The mouse models of Mll-mediated tumorigenesis are characterized by long latency. In addition, the lymphoid tumours are clonal in origin, as presumably are the myeloid tumours, and thus may require secondary mutations to express the overt tumour phenotype. This may point to a difference in the situation with the human paediatric tumours, which arise early and may not require any somatically acquired mutation other than the chromosomal translocation. It is possible, however, that inherited predisposition gene products may synergize with the chromosomal translocation in these cases. In mice, the additional mutation(s) that seems to be required could be loss of heterozygosity of tumour suppressor genes or gain-of-function mutations in other oncogenes.
It is noteworthy that the spectrum of leukaemias found in the Mll–lacZ fusion mice is similar in phenotype to that of Mll–AF9 fusion mice (Corral et al., 1996; Dobson et al., 1999). It is possible, therefore, that the default pathway for Mll-mediated tumorigenesis is in the myeloid lineage. Thus, the development of a lymphoid phenotype may be due to other specific secondary mutations or, perhaps more likely, a specific Mll fusion partner that may normally have a specific role in the lymphoid pathway, such as AF4, since the MLL–AF4 fusion predominates in B-lymphoid tumours. In support of this is the fact that the mouse Af4 gene is required for aspects of lymphopoiesis (Dr M.Djabali, personal communication). In vivo experiments to test the specificity of Mll–Af4 gene fusion should help to resolve these questions.
A model of the Mll–β–galactosidase fusion protein in leukaemia
Our data on the Mll–lacZ fusion indicate that it may be possible to dissect different elements of MLL function in tumorigenesis. A possible explanation of some distinct components might be that the MLL fusion protein must be stable after chromosomal translocation and that the various fusion partners confer this stabilization. Thus, the β–galactosidase moiety may confer stability of the Mll truncation, yielding effectively a functional Mll-half protein. In the case of the Mll–lacZ fusion, the truncated Mll may function as a dominant-negative molecule, operating in the absence of C–terminal sequences, as suggested for the self-fusion of MLL (Schichman et al., 1994, 1995).
Alternatively, complementary functions of truncation and protein fusion of MLL may be important such that Mll–lacZ fusion exhibits the loss of function (i.e. C–terminal sequences) and gain of function. In the case of the Mll–lacZ gene some potentially important characteristics are shared between this fusion and some naturally occurring fusions that arise somatically in man by chromosomal translocations. Potentially the most pertinent is the protein–protein interaction feature of β–galactosidase. The crystal structure of the active enzyme shows a tetrameric structure, with the enzyme active site located around a pocket in the tetramer (Jacobson et al., 1994). For the Mll–β–galactosidase fusion to function as an enzyme, it is therefore presumably also necessary for the fusion molecule to assemble into a tetrameric form. In the structural model of β–galactosidase (Jacobson et al., 1994), the N-termini of the four β–galactosidase molecules are central in the tetramer and thus the Mll moieties would be located there in a putative Mll–β–galactosidase tetramer. Thus, the contacts in β–galactosidase, which allow the formation of the tetrameric active enzyme, might create a dimer of Mll dimers, potentially with the two Mll ‘dimers’ facing away from each other. A possible Mll dimerization effect has interesting parallels with possible dimerization of MLL fusion genes made by chromosomal translocations. In particular, two translocations have been described in which related genes are fused to MLL, namely AF10 and AF17, which are fused to MLL after the chromosomal translocations t(10;11)(p12;23) and t(11;17)(q23;q21), respectively (Prasad et al., 1994; Chaplin et al., 1995a,b; Saha et al., 1995). A prominent feature of the AF10 and AF17 proteins is the presence of a leucine zipper protein dimerization domain in the part retained by the MLL–AF10 and MLL–AF17 fusions, suggesting that a dimer of MLL–AF10 or MLL–AF17 could occur in the leukaemic cells after the chromosomal translocations, thereby eliciting the function of the MLL fusion protein (Prasad et al., 1994; Chaplin et al., 1995b). Thus, there is a potential similarity between the Mll–β–galactosidase and MLL–AF10 or MLL–AF17 fusions in terms of dimerization.
Materials and methods
Construction of targeting vectors and analysis of targeted ES cells
The Mll–exon8–lacZ plasmid for gene targeting was constructed from a λ phage genomic clone containing Mll exon 8, isolated from a library of Sau3A partial fragments made in λ 2001. A 5.5 kb EcoRI genomic fragment containing exon 8 was subcloned in pBlueScript and an SfiI site added at the BamHI site within exon 8. An SfiI cassette carrying the bacterial β–galactosidase gene coding region upstream of the SV40 poly(A) site plus the MC1-neo-polyA (Thomas and Capecchi, 1987) was inserted into the modified SfiI site yielding an open reading frame fusion with Mll exon 8 (Figure 1A). This fusion was confirmed by DNA sequencing. An MC1-tk cassette was cloned at the 5′ end of the EcoRI fragment and the final targeting construct was linearized at the 3′ end by SalI digestion. The Mll–exon3–lacZ targeting construct was the AT–lac clone and Mll–myc tag was the Mll–myc clone previously described (Corral et al., 1996).
E14 cells were grown and transfected with DNA as described (Warren et al., 1994). Homologous recombination with the Mll–exon8–lacZ vector was assessed by filter hybridization (LeFranc et al., 1986) of BglII-digested genomic DNA using a 5′ end 1 kb XbaI fragment probe pXX (E.Collins and T.H.Rabbitts, unpublished data) or the EcoRI–XhoI fragment from p1.5RXT2 (Corral et al., 1996). Confirmation of correct targeting was obtained by hybridization of KpnI-digested DNA with the 3′ Mll probe BB (derived from a BstXI–BglII subclone) and the presence of a single insertion site was confirmed using the MC1-neo-pA fragment as a probe. Targeted ES clones were injected into C57/Bl6 blastocysts, which were transferred into recipient females. Chimeric mice thereby generated were estimated by coat colour compared with the black colour of the recipient strain.
β-galactosidase assay
Single-cell suspensions of ES cells were prepared and fixed with 2% formaldehyde/0.2% glutaraldehyde before staining for 48 h at 37°C with X-gal solution [0.2% X-gal, 2 mM MgCl2, 5 mM K4Fe(CN)6⋅3H2O] and 5 mM K3Fe(CN)6. The cells were then fixed again with 2% formaldehyde/0.2% glutaraldehyde and washed with phosphate-buffered saline (PBS). Slides were prepared for photography on Kodak Tungsten 160 film.
Histological and pathological analysis of mouse tissues
Mice were culled as soon as signs of ill health appeared. Mice were killed and a post-mortem carried out. Acute leukaemia was characterized by at least 30% of the nucleated cells in the bone marrow being blasts and this disease was mainly AML. The peripheral blood in AML was characterized by circulating myeloblasts. Appropriate tissue samples were taken for FACS analysis and for histology. For the latter, tissue specimens were fixed in a large volume of 10% formalin at room temperature for at least 24 h and embedded in paraffin wax. The wax blocks were sectioned and stained with haematoxylin–eosin (H&E) by routine techniques. Blood films on glass slides were stained with May–Giemsa–Grünwald (MGG). Slides were photographed using Kodak Tungsten 160 film.
Clonality analysis was carried out using filter hybridization as described previously (LeFranc et al., 1986) using an Ig heavy chain enhancer probe (Neuberger et al., 1989) or TCR β–chain Jβ2 and Cβ1 probes (Malissen et al., 1984).
Flow cytometric analysis (FACS) of cell surface marker expression
Single-cell suspensions were prepared from the thymus, spleen and bone marrow of Mll–exon8–lacZ or control mice as appropriate. Cells (100 ml; 5 × 107/ml) were incubated at 4°C for 20 min in PBS with 5% fetal calf serum (FCS) with a 1 in 1000 dilution of the following antibodies: anti-Gr–1 and anti-Mac–1 (granulocytes), anti-B220 (B cells), anti-CD3 and anti-CD4 (T cells). Antibodies (Pharmingen, San Diego, CA) were conjugated with either fluorescein isothiocyanate (FITC) or phycoerythrin (PE). Isotype-matched fluoresceinated antibodies were used as controls for non-specific immunofluorescence. After antibody labelling, cells were washed once with PBS plus 5% FCS and resuspended in 1 ml of PBS plus 5% FCS. Flow cytometric analysis was performed using a FACSCALIBUR and data analysis was performed with Cell Quest (Becton Dickinson, San Jose, CA). Each phenotype was generated by analysis of 10 000 cells.
Acknowledgments
Acknowledgements
We thank Drs Michael Neuberger and Gareth Williams for the IgH probe and Dr M.Malissen for the TCR probes. The assistance of Andrew Riddell in the FACS analysis is gratefully acknowledged. This work was supported by the MRC and partly by a grant from the Kay Kendall Leukaemia Research Fund. A.J.W. is the recipient of an MRC Clinician Scientist Fellowship held within the University of Cambridge, Department of Haematology, Hills Road, Cambridge. C.L.D. was the recipient of an MRC Studentship.
References
- Atlas M., Head, D., Behm, F., Schmidt, E., Zeleznik-Le, N.J., Roe, B.A., Burian, D. and Domer, P.H. (1998) Cloning and sequence analysis of four t(9;11) therapy-related leukemia breakpoints. Leukemia, 12, 1895–1902. [DOI] [PubMed] [Google Scholar]
- Bernard O. and Berger, R. (1995) Molecular basis of 11q23 rearrangements in hematopoietic malignant proliferations. Genes Chromosomes Cancer, 13, 75–85. [DOI] [PubMed] [Google Scholar]
- Chaplin T., et al. (1995a) A novel class of zinc finger/leucine zipper genes identified from the molecular cloning of the t(10;11) translocation in acute leukemia. Blood, 85, 1435–1441. [PubMed] [Google Scholar]
- Chaplin T., Bernard, O., Beverloo, H.B., Saha, V., Hagemeijer, A., Berger, R. and Young, B.D. (1995b) The t(10;11) translocation in acute myeloid leukemia (M5) consistently fuses the leucine zipper motif of AF10 onto the HRX gene. Blood, 86, 2073–2076. [PubMed] [Google Scholar]
- Cimino C., et al. (1997) Infant acute leukemias show the same biased distribution of ALL1 gene breaks as topoisomerase II related secondary acute leukemias. Cancer Res., 57, 2879–2883. [PubMed] [Google Scholar]
- Corral J., et al. (1996) An Mll–Af9 fusion gene made by homologous recombination causes acute leukemia in chimeric mice: A method to create fusion oncogenes. Cell, 85, 853–861. [DOI] [PubMed] [Google Scholar]
- DeVore R., Whitlock, J., Hainsworth, J.D. and Johnson, D.H. (1989) Therapy-related acute nonlymphocytic leukemia with monocytic features and rearrangement of chromosome 11q. Ann. Intern. Med., 10, 740–742. [DOI] [PubMed] [Google Scholar]
- DiMartino J.F. and Cleary, M.L. (1999) MLL rearrangements in haematological malignancies: lessons from clinical and biological studies. Br. J. Haematol., 106, 614–626. [DOI] [PubMed] [Google Scholar]
- Djabali M., Selleri,L., Parry,P., Bower,M., Young,B.D. and Evans,G.A. (1992) A trithorax-like gene is interrupted by chromosome 11q23 translocations in acute leukaemias Nature Genet., 2, 113–118. [DOI] [PubMed] [Google Scholar]
- Dobson C.L., Warren, A.J., Pannell, R., Forster, A., Lavenir, I., Corral, J., Smith, A.J.H. and Rabbitts, T.H. (1999) The Mll–AF9 gene fusion in mice controls myeloproliferation and specifies acute myeloid leukaemogenesis. EMBO J., 18, 3564–3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix C.A. (1998) Secondary leukemias induced by topoisomerase-targeted drugs. Biochim. Biophys. Acta, 1400, 233–255. [DOI] [PubMed] [Google Scholar]
- Gilliland D.G. (1998) Molecular genetics of human leukemia. Leukemia, 12, S7–S12. [PubMed] [Google Scholar]
- Gu Y., Nakamura, T., Alder, H., Prasad, R., Canaani, O., Cimino, G., Croce, C.M. and Canaani, E. (1992) The t(4;11) chromosome translocation of human acute leukemias fuses the ALL–1 gene, related to Drosophila trithorax, to the AF–4 gene. Cell, 71, 701–708. [DOI] [PubMed] [Google Scholar]
- Jacobson R.H., Zhang, X.-J., DuBose, R.F. and Matthews, B.W. (1994) Three-dimensional structure of β-galactosidase from E.coli. Nature, 369, 761–766. [DOI] [PubMed] [Google Scholar]
- Joh T., Kagami, Y., Yamamoto, K., Segawa, T., Takizawa, J., Takahashi, T., Ueda, R. and Seto, M. (1996) Identification of MLL and chimeric MLL gene products involved in 11q23 translocation and possible mechanisms of leukemogenesis by MLL. Oncogene, 13, 1945–1953. [PubMed] [Google Scholar]
- Lavau C., Szilvassy, S.J., Slany, R. and Cleary, M.L. (1997) Immortalization and leukemic transformation of a myelomonocytic precursor by retrovirally transduced HRX-ENL. EMBO J., 16, 4226–4237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeFranc M.-P., Forster, A., Baer, R., Stinson, M.A. and Rabbitts, T.H. (1986) Diversity and rearrangement of the human T cell rearranging γ genes: Nine germ-line variable genes belonging to two subgroups. Cell, 45, 237–246. [DOI] [PubMed] [Google Scholar]
- Look A.T. (1997) Oncogenic transcription factors in the human acute leukemias. Science, 278, 1059–1065. [DOI] [PubMed] [Google Scholar]
- Malissen M., et al. (1984) Mouse T cell antigen receptor: structure and organization of constant and joining gene segments encoding the β polypeptide. Cell, 37, 1101–1110. [DOI] [PubMed] [Google Scholar]
- Morgan G.J., Cotter, F., Katz, F.E., Ridge, S.A., Domer, P., Korsmeyer, S. and Wiedemann, L.M. (1992) Breakpoints at 11q23 in infant leukemias with the t(11;19)(q23;p13) are clustered. Blood, 80, 2172–2175. [PubMed] [Google Scholar]
- Nasr F., Macintyre, E., Venuat, A.M., Bayle, C., Carde, P. and Ribrag, V. (1997) Translocation t(4;11)(q21;q23) and MLL gene rearrangement in acute lymphoblastic leukemia secondary to anti topoisomerase II anticancer agents. Leuk. Lymphoma, 25, 399–401. [DOI] [PubMed] [Google Scholar]
- Neuberger M.S., Caskey, H.M., Pettersson, S., Williams, G.T. and Surani, M.A. (1989) Isotype exclusion and transgene down-regulation in immunoglobulin-λ transgenic mice. Nature, 338, 350–352. [DOI] [PubMed] [Google Scholar]
- Prasad R., et al. (1994) Leucine-zipper dimerization motif encoded by the AF17 gene fused to ALL–1 (MLL) in acute leukemia. Proc. Natl Acad. Sci. USA, 91, 8107–8111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pui C.-H., et al. (1989) Secondary acute myeloid leukemia in children treated for acute lymphoid leukemia. N. Engl. J. Med., 321, 136–142. [DOI] [PubMed] [Google Scholar]
- Rabbitts T.H. (1994) Chromosomal translocations in human cancer. Nature, 372, 143–149. [DOI] [PubMed] [Google Scholar]
- Rowley J.D. (1993) Rearrangements involving chromosome 11Q23 in acute leukaemia. Semin. Cancer Biol., 4, 377–385. [PubMed] [Google Scholar]
- Rowley J.D., et al. (1997) All patients with the t(11;16)(q23;p13.3) that involves MLL and CBP have treatment-related hematologic disorders. Blood, 90, 535–541. [PubMed] [Google Scholar]
- Rubnitz J.E., Behm, F.G. and Downing, J.R. (1996) 11q23 rearrangements in acute leukemia. Leukemia, 10, 74–82. [PubMed] [Google Scholar]
- Saha V., Chaplin, T., Gregorini, A., Ayton, P. and Young, B.Y. (1995) The leukemia-associated-protein (LAP) domain, a cysteine-rich motif, is present in a wide range of proteins, including MLL, AF10 and MLLT6 proteins. Proc. Natl Acad. Sci. USA, 92, 9737–9741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schichman S.A., Caligiuri, M.A., Gu, Y., Strout, M.P., Canaani, E., Bloomfield, C.D. and Croce, C.M. (1994) ALL–1 partial duplication in acute leukemia. Proc. Natl Acad. Sci. USA, 91, 6236–6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schichman S.A., Canaani, E. and Croce, C. (1995) Self-fusion of the ALL1 gene. J. Am. Med. Assoc., 273, 571–576. [PubMed] [Google Scholar]
- Slany R.K., Lavau, C. and Cleary, M.L. (1998) The oncogenic capacity of HRX-ENL requires the transcriptional transactivation activity of ENL and the DNA binding motifs of HRX. Mol. Cell. Biol., 18, 122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobulo O.M., et al. (1997) MLL is fused to CBP, a histone acetyltransferase, in therapy-related acute myeloid leukemia with a t(11;16)(q23;p13.3). Proc. Natl Acad. Sci. USA, 94, 8732–8737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirman M.J., et al. (1993) Rearrangement of the MLL gene in acute lymphoblastic and acute myeloid leukemias with 11q23 chromosomal translocations. N. Engl. J. Med., 329, 909–914. [DOI] [PubMed] [Google Scholar]
- Thomas K.R. and Capecchi, M.R. (1987) Site-directed mutagenesis by gene targeting in mouse embryo-derived stem cells. Cell, 51, 503–512. [DOI] [PubMed] [Google Scholar]
- Tkachuk D.C., Kohler, S. and Cleary, M.L. (1992) Involvement of a homolog of Drosophila Trithorax by 11q23 chromosomal translocations in acute leukemias. Cell, 71, 691–700. [DOI] [PubMed] [Google Scholar]
- Warren A.J., Colledge, W.H., Carlton, M.B.L., Evans, M.J., Smith, A.J.H. and Rabbitts, T.H. (1994) The oncogenic cysteine-rich LIM domain protein rbtn2 is essential for erythroid development. Cell, 78, 45–58. [DOI] [PubMed] [Google Scholar]
- Yamada Y., Warren, A.W., Dobson, C., Forster, A., Pannell, R. and Rabbitts, T.H. (1998) The T cell leukaemia LIM protein Lmo2 is necessary for adult mouse haematopoiesis. Proc. Natl Acad. Sci. USA, 95, 3890–3895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziemin-van der Poel S., et al. (1991) Identification of a gene, MLL, that spans the breakpoint in 11q23 translocations associated with human leukemias. Proc. Natl Acad. Sci. USA, 88, 10735–10739. [DOI] [PMC free article] [PubMed] [Google Scholar]