Abstract
There has recently been a renewal of human research with classical hallucinogens (psychedelics). This paper first briefly discusses the unique history of human hallucinogen research, and then reviews the risks of hallucinogen administration and safeguards for minimizing these risks. Although hallucinogens are relatively safe physiologically and are not considered drugs of dependence, their administration involves unique psychological risks. The most likely risk is overwhelming distress during drug action (“bad trip”), which could lead to potentially dangerous behavior such as leaving the study site. Less common are prolonged psychoses triggered by hallucinogens. Safeguards against these risks include the exclusion of volunteers with personal or family history of psychotic disorders or other severe psychiatric disorders, establishing trust and rapport between session monitors and volunteer before the session, careful volunteer preparation, a safe physical session environment, and interpersonal support from at least two study monitors during the session. Investigators should probe for the relatively rare hallucinogen persisting perception disorder in follow up contact. Persisting adverse reactions are rare when research is conducted along these guidelines. Incautious research may jeopardize participant safety and future research. However, carefully conducted research may inform the treatment of psychiatric disorders, and may lead to advances in basic science.
Keywords: hallucinogens, psychedelics, entheogens, psilocybin, LSD, DMT, mescaline, 5-HT2A agonists, safety guidelines, adverse reactions, human research
Introduction
After several decades of dormancy, research involving the administration of classical hallucinogens to humans has been recently renewed (Frecska and Luna, 2006; Harvard Mental Health Letter, 2006; Lancet, 2006; Morris, 2006; Sessa, 2005; Winkelman and Roberts, 2007). Although animal research during the intervening decades has substantially advanced our understanding of underlying neuropharmacological mechanisms of the hallucinogens, the fact that human research with this historically important and widely used class of compounds remained inactive is remarkable (Nichols, 2004). Renewed human administration research began with the work of Rick Strassman, who initiated research on the effects of the N,N-dimethyltryptamine (DMT) at the University of New Mexico in the early 1990s (Strassman, 1991, 1996, 2001; Strassman and Qualls, 1994; Strassman et al., 1994, 1996). Subsequently, investigators both in the United States and in Europe have developed human research programs with hallucinogens. This new research has included basic-science studies that have administered hallucinogens as tools for investigating cognitive neuroscience and perception (Gouzoulis-Mayfrank, Heekeren et al., 1998; Gouzoulis-Mayfrank et al., 2002; Umbricht et al., 2003; Carter et al., 2004; Carter, Pettrigrew, Burr et al., 2005; Carter, Pettrigrew, Hasler, et al., 2005), time perception (Wittmann et al., 2007), hallucinogen pharmacokinetics and metabolism (Hasler et al., 1997, 2002), model psychosis (Gouzoulis-Mayfrank, Heekeren et al., 1998; Vollenweider et al., 1997, 1998, 1999, 2007; Vollenweider and Geyer, 2001; Gouzoulis-Mayfrank et al., 2005, 2006), and, recently in our laboratory, hallucinogens’ reported facilitation of experiences having enduring personal meaning and spiritual significance (Griffiths et al., 2006). Recent clinical studies have administered hallucinogens to evaluate their safety and efficacy in the treatment of psychiatric disorders: specifically, anxiety related to advanced-stage cancer (Grob, 2005) and obsessive-compulsive disorder (Moreno et al., 2006). In addition, several studies have examined the effects of ayahuasca (also known as hoasca or yagé; an admixture containing DMT) in human volunteers outside of the United States (e.g., Grob et al., 1996; Riba et al., 2001). Because the United States Supreme Court has recently ruled in favor of the União do Vegetal (UDV; a syncretic Brazilian church that uses ayahuasca in the context of religious ceremonies) in their claim that the UDV’s use of ayahuasca is protected under the Religious Freedom Restoration Act (Gonzales v. O Centro Espirita Beneficiente União do Vegetal, 2006), ayahuasca use within this church setting may receive increased scientific investigation within the United States.
We use the word “hallucinogen” herein to refer to the classical hallucinogens, sometimes called “psychedelics,” “psychotomimetics,” or “entheogens” (Ruck et al., 1979; Grinspoon and Bakalar, 1979; Ott, 1996; Metzner, 2004). Admittedly, the term “hallucinogen” is not ideal for these substances because perceptual changes are only one domain of their effects, and the typical perceptual changes engendered by hallucinogens at typical doses rarely include frank hallucinations (Grinspoon and Bakalar, 1979; Nichols, 2004; O’Brien, 2006). However, we use this term because it is the most widely used in the scientific literature. Although the term “psychedelic” is widely used, it has the disadvantage of carrying considerable cultural connotation (i.e., its use as a descriptor of a style of music or art associated with Western counter-culture of the 1960s). The terms “psychotomimetic” (emphasizing model psychosis) and “entheogen” (emphasizing mystical-type experiences, i.e., phenomenologically indistinguishable from classically described mystical experiences) highlight only a single aspect (which may not occur reliably) of the much broader range of hallucinogen effects.
Hallucinogens can be divided structurally into two classes of alkaloids: the tryptamines, including psilocybin (prodrug constituent of Psilocybe and several other mushroom genera), the semi-synthetic d-lysergic acid diethylamide (LSD), and DMT; and the phenethylamines, including mescaline (principle active constituent of peyote) and certain synthetic compounds (Grinspoon and Bakalar, 1979; Shulgin and Shulgin, 1991, 1997; Metzner, 2004, Nichols, 2004). The effects of these substances are primarily mediated by agonist action at 5-HT2A receptors (Glennon et al., 1984; Nichols, 2004; González-Maeso, 2007) and produce a generally similar profile of subjective effects (Hidalgo, 1960; Hollister, 1962; Wolbach, Isbell and Miner, 1962; Wolbach, Miner and Isbell, 1962; Shulgin and Shulgin, 1991, 1997). Other classes of substances have sometimes been identified as “hallucinogens,” including 3,4-methylenedioxymethamphetamine or MDMA (perhaps more appropriately labeled an entactogen [Nichols et al., 1986] or empathogen [Metzner, 1985]); dissociative anesthetics such as ketamine, phencyclidine, and dextromethorphan; and anticholinergic agents such as scopolamine and atropine (Nichols, 2004). However, this paper uses the term “hallucinogen” to refer specifically to classical hallucinogens.
The purpose of this paper is to provide guidance in the safe administration of high doses of hallucinogens (e.g., ≥ 25 mg psilocybin or 200 µg LSD). Some aspects of these recommendations may also apply to studies employing lower doses, although, as with other drug classes, the likelihood of potential adverse effects will be related to dose. Similarly, some aspects of these recommendations may also apply to studies administering the other drug classes mentioned in the preceding paragraph: entactogens, dissociative anesthetics, and anticholinergic agents. However, the clinical effects and mechanisms of action of these agents are sufficiently different from the classical hallucinogens that safety recommendations concerning their administration are beyond the scope of this manuscript.
First, so that the historical context in which current human hallucinogen studies are conducted will be clear, we will briefly discuss the history of sacramental hallucinogen use by indigenous cultures, and the history of human hallucinogen research before it became dormant in the 1970s. The decades-long virtual dormancy of human hallucinogen research stands as a unique case in the history of modern clinical pharmacology. It is important for researchers going forward to understand the role that safety factors, as well as sociological and political factors, played in the history and cessation of human hallucinogen research. Also, because of the historical legacy of sensationalism surrounding hallucinogens, researchers should appreciate the precarious position of current human hallucinogen research, and recognize that very high safety standards will help to ensure that human research continues into the decades to come. Next, we will provide a detailed description of the unique risks of hallucinogen administration. We will then present the proposed guidelines for conducting high-dose hallucinogen research in each of several domains including volunteer selection, study personnel, physical environment, preparation of volunteers, conduct of sessions, and post-session procedures.
Relevant history
Hallucinogen use by indigenous cultures
Hallucinogens have been used by indigenous cultures for millennia (Schultes, 1969; Lowy, 1971; Schultes et al., 2001). These cultures have restricted hallucinogen use to sacramental and healing contexts, with these two often being inseparably intertwined. Remarkably, apparently without exception, such cultures view hallucinogenic plants and fungi as being of divine origin (Schultes et al., 2001). Given this orientation, it is not surprising that their ingestion is often tightly restricted, with use controlled by ceremonial guidelines including taboos against improper use (Schultes et al., 2001; Weil, 2004). Indigenous cultures restrict use of hallucinogens to highly ritualized, sacred ceremonies such as those designed to serve as rites of passage, or to set the occasion for divination and spiritual or physical healing. Even in cases in which certain use extends beyond the shaman and may be more recreational in nature (e.g., use of the DMT-containing epená by the Waiká cultures of Brazil and Venezuela), the hallucinogen is prepared and taken in a highly ritualized context (Grinspoon and Bakalar, 1979; Schultes, 2001; Weil, 2004). Modern, urban syncretic religions, such as the UDV, which have developed in South America and have been influenced by indigenous use of ayahuasca, also incorporate a high degree of structure and guidance into their ayahuasca use, which may minimize adverse reactions (Gonzales v. O Centro Espirita Beneficiente União do Vegetal, 2006).
However, indigenous cultures should not be regarded as absolute role models in the clinical use of hallucinogens for at least two reasons. First, some of these cultures also engaged in practices considered unethical in our culture. For example, the Aztecs, who used psilocybin mushrooms and morning glory seeds (containing LSD-related agents), practiced human sacrifice, and even incorporated hallucinogen use into sacrificial rituals (Ott, 1996). As another example, the Jivaro in Ecuador who use ayahuasca practice sacramental headhunting, and ayahuasca may be used by the shaman in that society for malevolent intent (i.e., bewitching) as well as for healing (Harner, 1962, 1968; Grof, 1977). Second, risk/benefit tradeoffs that may be acceptable in various religious contexts may fall short of what is expected in the domain of contemporary scientific research with human participants.
Nonetheless, some important themes have emerged in the use of hallucinogens by indigenous cultures that may have bearing on the appropriate use of hallucinogens in clinical research. Indeed, some of the safeguards developed for clinical hallucinogen research and expressed in the guidelines presented herein are similar to important aspects of hallucinogen use by indigenous cultures. These common themes are structured use (expressed as ritual in indigenous use), restrictions on use including the need for guidance, and appreciation of hallucinogens’ powerful psychological effects (expressed as reverence in indigenous use). We believe that these commonalities are more than coincidence. The unique pharmacology of classical hallucinogens may have shaped convergent practices across independent cultures. Likewise, the guidelines expressed herein for human clinical research with hallucinogens may also be viewed as having been developed in reaction to these same aspects of hallucinogen pharmacology. As an example, some of the unique effects and safety concerns for hallucinogens may be related to their ability to set the occasion for deeply meaningful, even spiritual experiences (Richards, 2003, 2005). Novak (1997) hypothesized that Western intellectuals in the mid 1950’s such as Aldous Huxley and Gerald Heard merely redefined the subjective effects resulting from hallucinogen administration as a spiritual experience, thereby popularizing such an association in western culture. However, the observation that indigenous cultures that ingest classical hallucinogens almost invariably do so under sacramental contexts (Schultes et al., 2001), along with the findings from double-blind clinical studies demonstrating that under supportive conditions hallucinogens occasion mystical-type experiences with high frequency (Pahnke, 1963; Griffiths et al., 2006), suggests that the association of hallucinogens with spiritual experience relates to the pharmacology of these agents rather than being based entirely on cultural suggestion.
Early clinical research
In the 1950s and 1960s, thousands of research participants were administered hallucinogens in the context of basic clinical research or therapeutic clinical research, resulting in hundreds of publications (Grinspoon and Bakalar, 1979; Grob et al., 1998; Strassman, 2001; Nichols, 2004). During this time the United States Army investigated classical hallucinogens as incapacitating agents in soldiers, and the United States Central Intelligence Agency conducted clandestine research investigating classical hallucinogens as interrogation agents in which civilians were administered hallucinogens without knowledge or consent. Eventually, both groups ceased to focus on classical hallucinogens in favor of non-classical “hallucinogens” such as the synthetic anticholinergic compound quinuclidinyl benzilate (BZ), which showed greater promise as a warfare agent than LSD because its effects were marked by greater immobility, delirium, amnesia, and duration (Lee and Shlain, 1992). Very early academic research on classical hallucinogens was designed without considering the powerful influences of set (psychological state) and setting (environment) (e.g., Malitz et al., 1960; Rinkel et al., 1960; Hollister, 1961; Rümmele and Gnirss, 1961; Leuner, 1962). Subsequent research, which included more preparation and interpersonal support during the period of drug action, found fewer adverse psychological reactions, such as panic reactions and paranoid episodes, and increased reports of positively-valued experiences (Chwelos et al., 1959; Leary, 1964; Leary et al., 1963, 1964; Metzner et al. 1965; Pahnke, 1969).
One major area of early research focused on the comparison of hallucinogen effects with the symptoms of psychosis (e.g., Stockings, 1940; Hoch et al., 1953; Hoffer and Callbeck, 1960; Leuner, 1962; Kuramochi and Takahashi, 1964). Although the study of hallucinogens as models for the psychosis observed in schizophrenia eventually fell out of favor in psychiatry (Grinspoon and Bakalar, 1979; Snyder, 1988; Strassman, 2001), a renewed interest in this area is emerging, in part due to modern brain imaging techniques and neuropharmacological findings that have supported hallucinogens as a model of at least certain aspects of acute psychosis (Gouzoulis-Mayfrank, Heekeren et al., 1998; Vollenweider et al., 1997; Vollenweider and Geyer, 2001; Gouzoulis-Mayfrank et al., 2005, 2006).
Other areas of early human research included investigations of therapeutic applications of hallucinogens in treatment of psychological suffering associated with cancer and in the treatment of substance dependence. Anecdotal observations and non-blind studies in cancer patients suffering from anxiety and depression suggested that LSD administration resulted in an ability to openly discuss existential fears and be at peace with approaching death, and that this reorientation often outlasted the acute drug effects (Kast and Collins, 1964; Cohen, 1965; Kast, 1967). Follow up investigations involved the administration of a high dose of a hallucinogen to carefully prepared patients under highly supportive interpersonal conditions, with the patient wearing eyeshades and listening to classical music through headphones during the course of pharmacological action, a model known as “psychedelic peak therapy” or “psychedelic therapy” (Kurland et al., 1969; Pahnke et al., 1969; Richards et al, 1972; Grof et al., 1973; Kurland et al., 1973; Grof and Halifax, 1977; Richards et al., 1977; Richards et al., 1979; Grof, 1980; Richards, 1980; Kurland, 1985). Unfortunately, these early studies did not include the stringent control conditions or groups that now have become standard in modern clinical psychopharmacology research. The results suggest, however, that these compounds may have improved psychological well-being in the face of anxiety and depression secondary to cancer.
Another focus of study was hallucinogen-facilitated therapy in the treatment of alcoholism and other forms of substance dependence (e.g., Smart et al., 1966; Holister et al., 1969; Ludwig et al., 1969; Kurland et al., 1971; Savage and McCabe, 1973). While some studies prepared patients and utilized supportive conditions (e.g., Kurland et al., 1971; Savage and McCabe, 1973), others drastically departed from the “psychedelic therapy” model (and from the guidelines herein), and involved the administration of high doses to unprepared, restrained patients (e.g., Smart et al., 1966). Results across studies were ultimately inconclusive due to such variations in methods and a lack of modern controls and experimental rigor (Abuzzahab and Anderson, 1971; McGlothlin and Arnold, 1971; Halpern, 1996; Mangini, 1998). Similarly, some therapists reported that hallucinogens administered under supportive contexts could accelerate psychotherapy for a variety of psychological disorders (e.g., Abramson, 1960, 1963; Crochet et al., 1963; Mogar and Aldrich, 1969; Rhead, 1977). However, these reports were largely based on anecdotal clinical accounts rather than controlled studies.
Escalation in recreational hallucinogen use, primarily LSD, in the 1960s, led to considerable sensationalism concerning these drugs in media coverage. Adding to the controversy was the publicized departure and termination of Timothy Leary and Richard Alpert from Harvard University in 1963 following charges of unorthodox methods in hallucinogen research (Grinspoon and Bakalar, 1979; Lee and Shlain, 1992; Novak, 1997; Strassman, 2001). Leary’s subsequent irresponsible advocacy of hallucinogen use by youth further undermined an objective scientific approach to studying these compounds. The growing controversy and sensationalism resulted in increasing restrictions on access to hallucinogens throughout the 1960s (ultimately resulting in the placement of the most popular hallucinogens into Schedule I of the 1970 Controlled Substances Act in the United States), creating substantially greater regulatory barriers for researchers to conduct human trials. The negative publicity also resulted in withdrawal of federal research funds, which had previously supported much of the human research, and in the professional marginalization of clinical investigators interested in pursuing research with hallucinogens. Human research with hallucinogens in the United States became virtually dormant when the last trials were published in the early 1970s. Commenting on the unusual evolution of psychiatric research with hallucinogens, Strassman (2001) mused, “They began as ‘wonder drugs,’ turned into ‘horror drugs,’ then became nothing” (p. 28).
Unique risks of human hallucinogen research
Hallucinogen administration in humans results in a unique profile of effects and potential adverse reactions that need to be appropriately addressed in order to maximize safety. Different risks are associated with different drug classes, and human research with each class requires procedures to be in place to address those particular risks. For example, because high doses of certain opioids and sedative/hypnotics can cause respiratory depression (Gutstein and Akil, 2006; Charney et al., 2006), when conducting research with high doses of these drugs, respiration rate and/or blood oxygen are monitored, and mechanical breathing assistance and appropriate rescue medications are readily available. As another example, administration of high doses of psychomotor stimulants such as cocaine can cause cardiac stress (O’Brien, 2006). Therefore electrocardiogram (ECG) readings taken at screening are scrutinized carefully, pulse and blood pressure are monitored during sessions, and rescue medication for acute hypertension is immediately available. Similarly, human hallucinogen administration entails its own unique risk profile. Unlike opioids, sedative/hypnotics, or psychomotor stimulants, the primary safety concerns with hallucinogens are largely psychological rather than physiological in nature.
Physiological toxicity
Hallucinogens generally possess relatively low physiological toxicity, and have not been shown to result in organ damage or neuropsychological deficits (Strassman, 1984; Gable, 1993, 2004; Halpern and Pope, 1999; Hasler et al., 2004; Nichols, 2004; Halpern et al., 2005). Nonhuman animal studies have shown MDMA (structurally similar to some classical hallucinogens, but with a substantially different pharmacological mechanism of action) to have neurotoxic effects at high doses, although MDMA has been judged to be safe for human administration in the context of several therapeutic and basic human research studies. In contrast, there is no evidence of such potential neurotoxic effects with the prototypical classical hallucinogens (i.e., LSD, mescaline, and psilocybin). Some physiological symptoms may occur during hallucinogen action, such as dizziness, weakness, tremors, nausea, drowsiness, paresthesia, blurred vision, dilated pupils, and increased tendon reflexes (Isbell, 1959; Hollister, 1961; Nichols, 2004). In addition, hallucinogens can moderately increase pulse and both systolic and diastolic blood pressure (Isbell, 1959; Wolbach, Miner and Isbell, 1962; Strassman and Qualls, 1994; Gouzoulis-Mayfrank et al., 1999; Passie et al., 2002; Griffiths et al., 2006). However, these somatic effects vary and are relatively unimpressive even at doses yielding powerful psychological effects (perceptual, cognitive, and affective) (Metzner et al., 1965; Passie et al., 2002; Metzner, 2004).
Although a full discussion of special physiological toxicity concerns for medical patient populations is beyond the scope of this manuscript, a few observations are worthy of note. The early literature examining hallucinogens in the treatment of anxiety and depression secondary to cancer indicated that the classical hallucinogens LSD and N,N-dipropyltryptamine (DPT) were physiologically well-tolerated. The physical adverse effects of these agents observed in cancer patients were manageable and similar to effects observed in physically healthy individuals. These researchers noted that any other symptoms experienced during sessions with cancer patients were symptoms already associated with their existing illness (Richards et al., 1972; Kurland et al., 1973; Kurland, 1985). Early clinical research also safely administered LSD to chronic alcoholics and cancer patients with “considerable liver damage,” suggesting hepatic concerns are “negligible unless the dysfunction is of a critical degree” (Grof, 1980, p. 164).
Participants and review committees may be concerned that LSD or other hallucinogens are associated with chromosomal damage. These concerns stem from an anti-LSD media campaign by the United States government in the late 1960s that was based on and followed soon after initial reports (Cohen, Hirschhorn and Frosch, 1967; Cohen, Marinello and Back, 1967; Irwin and Egozcue, 1967) suggesting LSD caused chromosomal damage in human leukocytes (Ott, 1996; Weil, 2004). This campaign included pictures of deformed children (Grinspoon and Bakalar, 1979) at a time when the thalidomide tragedies of a decade earlier were relatively fresh in the public’s memory (Ott, 1996). However, many follow up investigations soon squarely refuted the hypothesis that LSD use in humans was a significant risk for chromosomal damage or carcinogenic, mutagenic, or teratogenic effects (e.g., Bender and Siva Sankar, 1968; Tjio et al., 1969; Dishotsky et al., 1971; Long, 1972).
Abuse and dependence
Like many classes of psychoactive drugs, hallucinogens are sometimes used in a manner that jeopardizes the safety or well-being of the individual or others (e.g., driving while impaired; a pattern of use that interferes with work, school, or relationships). Under such circumstances hallucinogens are said to be abused. However, hallucinogens are not typically considered drugs of dependence in that they do not engender compulsive drug seeking (National Institute on Drug Abuse, 2001, 2006; O’Brien, 2006), consistent with the observation that they are not reliably self-administered in nonhuman animals (Poling and Bryceland, 1979; Griffiths et al., 1980; Fantegrossi et al., 2004). Further, they are not associated with a known withdrawal syndrome (O’Brien, 2006). Therefore, there is little risk that exposing human volunteers to hallucinogens will leave participants physically or psychologically dependent on these compounds. This low dependence potential allows for the possibility of administering these compounds to hallucinogen-naïve volunteers when blinding issues are critical (e.g., Griffiths et al., 2006). However, in certain situations it may be advantageous to study hallucinogen-experienced participants (e.g., brain imaging studies requiring the participant to remain immobile).
Acute psychological distress and dangerous behavior during hallucinogen action
Although hallucinogens have relatively low physiological toxicity and are not associated with compulsive drug seeking, there is still concern that they may pose other psychological risks. The most likely risk associated with hallucinogen administration is commonly known as a “bad trip” and is characterized by anxiety, fear/panic, dysphoria, and/or paranoia. Distressing effects may be experienced in a variety of modalities: sensory (e.g., frightening illusions), somatic (e.g., disturbing hyperawareness of physiological processes), personal psychological (e.g., troubling thoughts or feelings concerning one’s life) and metaphysical (e.g., troubling thoughts or feelings about ultimate evil forces) (McCabe, 1977; Grinspoon and Bakalar, 1979; Strassman, 1984). Because emotional experience is often intensified when under the influence of a hallucinogen, in unprepared individuals or uncontrolled situations any of these effects may potentially escalate to dangerous behavior. For example, fear and paranoid delusions may lead to erratic and potentially dangerous behavior, including aggression against self or others (Strassman, 1984). Although very rare, in hazardous and unsupervised conditions, individuals under the influence of hallucinogens have ended their lives by such acts as jumping from buildings (Keeler and Reifler, 1967; Reynolds and Jindrich, 1985; Reitman and Vasilakis, 2004; O’Brien, 2006). We recognize that even under unsupervised and unprepared conditions, reactions to hallucinogens involving violence and self-destructive behavior are rare, and our intention is not to create an unrealistic account of the dangers of hallucinogens. Nonetheless, even infrequent reports of such dangers require that investigators take seriously such risks and take steps to avoid their occurrence.
Prolonged psychosis
Another potential risk of hallucinogen administration is provoking the onset of prolonged psychosis, lasting days or even months (Strassman, 1984). Although determining causation is difficult, it appears that individuals who experience such reactions have premorbid mental illness before taking hallucinogens. However, it is unknown whether the precipitation of psychosis in such susceptible individuals represents a psychotic reaction that would have never occurred in the absence of hallucinogen use, or whether it represents an earlier onset of a psychotic break that would have inevitably occurred (Grinspoon and Bakalar, 1979; Strassman, 1984). Unlike acute psychological distress, these cases will be extremely rare in well-selected and well-prepared participants. In a survey of investigators who had administered LSD or mescaline, Sidney Cohen (1960) reported that only a single case of a psychotic reaction lasting more than 48 hours occurred in 1200 experimental (non-patient) research participants (a rate of 0.8 per 1000). Notably, the individual was an identical twin of a schizophrenic patient and thus would have been excluded under the proposed guidelines. Prolonged reactions over 48 hours were slightly more frequent in patients undergoing psychotherapy than in experimental non-patient participants, but still relatively rare, occurring at a rate of 1.8 prolonged reactions per 1000 patients. Cohen (1960) also reported that suicide attempts and completed suicides occurred at a rate of 1.2 and 0.4, respectively, per 1000 patients. The causal link between hallucinogen exposure and suicide or suicide attempt was only clear for a portion of these cases in patients, and no suicides or suicide attempts were noted for the 1200 non-patient, experimental participants. However, it is important when evaluating these data to consider that only 44 of the 62 researchers queried by Cohen returned survey results (Cohen, 1960; Novak, 1997). Although Cohen and Ditman (1962) subsequently expressed misgivings over the increased incidence of adverse effects due to the increasing recreational use of LSD and some questionable clinical practices, they maintained that when used under the proper guidelines, LSD was an important tool for use in human research (cf., Novak, 1997). McGlothin and Arnold (1971) reported 1 case out of 247 individuals who received LSD in either experimental or psychotherapeutic studies in which an LSD-related psychotic reaction lasting more than 48 hours occurred. That single case was a patient who received repeated LSD administrations in a psychotherapeutic context. Although very rare, care must be taken to minimize the risks of such an episode. The volunteer selection guidelines, addressed in a later section, will be the key factor in minimizing the risk of prolonged psychosis in human hallucinogen research studies.
Some clinical observations suggest the possibility that unconscious psychological material may be activated during hallucinogen sessions, and that such material, if not properly worked through and psychologically integrated, may lead to psychological difficulties of a non-psychotic nature, such as negative emotions and psychosomatic symptoms, lasting beyond the session (e.g., McCabe, 1977; Grof, 1980). Although these observations have not been examined experimentally, they deserve consideration. As suggested in our subsequent discussion of volunteer-monitor interactions, we believe that the strong interpersonal support from session monitors before, during, and following sessions will minimize any enduring untoward psychological effects.
Lasting perceptual abnormalities
Another potential risk of hallucinogen administration is hallucinogen persisting perception disorder (HPPD). In order to meet DSM-IV-TR criteria for this disorder, a hallucinogen user must re-experience perceptual effects similar to those experienced under acute hallucinogen action after cessation of hallucinogen use, these effects must be clinically distressing or impair functioning, and the effects must not be caused by a medical condition or be better explained by another psychiatric disorder or hypnopompic hallucinations (American Psychiatric Association, 2000). The incidence of HPPD is unknown, although it is thought to be very uncommon given the relatively few cases reported out of the millions of hallucinogen doses consumed since the 1960s (Halpern and Pope, 2003). Although the term “flashback” is sometimes used interchangeably with HPPD, the former term is often used to describe any brief perceptual effects reminiscent of acute hallucinogen effects but occurring beyond acute hallucinogen use, usually in the absence of clinical distress or impairment (Lerner et al., 2002). Indeed, many illicit hallucinogen users report some brief visual abnormalities occurring after acute hallucinogen effects, but only for a small minority of users are these effects troubling or impairing enough to be considered clinically significant or warrant the diagnosis of HPPD (Lerner et al., 2002; Baggott et al., 2006). Many illicit users regard such sub-clinical effects as benign and pleasurable (Strassman, 1984; Lerner et al., 2002; Frecska and Luna, 2006). Importantly, the incidence of HPPD or other perceptual abnormalities appears to be much lower in therapeutic or research contexts with careful screening and preparation than in the context of illicit recreational use which may include the confounds of polydrug use and unscreened psychiatric disorders (Cohen, 1960; McGlothlin and Arnold, 1971; Strassman, 1984; Halpern and Pope, 2003). Because such perceptual abnormalities are poorly understood, researchers administering hallucinogens to human volunteers should probe for perceptual disturbances in follow up contact.
Guidelines for safety
The guidelines that follow are intended to support the safe administration of high doses of hallucinogens to human volunteers while minimizing potential adverse reactions. Although a previous paper outlined methodological issues relevant to the study of hallucinogens in humans (Gouzoulis-Mayfrank, Schneider et al., 1998), safety issues were not the primary focus of that paper. The present paper substantially complements this previous work by providing a more detailed discussion of safety concerns. Issues relevant to the conduct of human research with drugs of abuse in general have been well described (Fischman and Johanson, 1998). The present guidelines extend and complement the recommendations of Fischman and Johanson (1998) for high-dose hallucinogen research. For some domains, such as volunteer selection, volunteer preparation, and the interactions between the volunteer and study personnel, the proposed criteria are substantially more extensive than those presented by Fischman and Johanson (1998) and those routinely used in human behavioral pharmacology because these domains appear to require even greater attention for hallucinogens than for other classes of psychoactive drugs. Although particular aspects of the proposed guidelines may be debatable, it is hoped that this paper will encourage such discussion while conveying the general themes and major domains of concern in human hallucinogen research. The proposed guidelines may serve as a helpful starting point for investigators planning to conduct human hallucinogen research.
Selection of volunteers
There are two main domains of consideration for volunteer selection. First, selection criteria may be methodological in nature and involve the specific research questions being explored. Second, which is the focus of this manuscript, is safety-related selection criteria. In our studies at Johns Hopkins, participants must be in good general health as assessed by detailed medical history, physical exam, 12-lead ECG, blood chemistry profile, hematology, and urinalysis. Pregnant women or those not practicing effective means of birth control are excluded. Relevant to general medical screening, classical hallucinogens moderately increase pulse and both systolic and diastolic blood pressure (Isbell, 1959; Wolbach, Miner and Isbell, 1962; Strassman and Qualls, 1994; Gouzoulis-Mayfrank et al., 1999; Passie et al., 2002; Griffiths et al., 2006). Therefore in our studies of psilocybin to date, volunteers have been excluded if resting blood pressure exceeded 140 systolic and 90 diastolic (mm Hg), averaged across four assessments on at least two separate days. Using these screening parameters with 54 participants to date, no psilocybin session has resulted in blood pressure increases considered medically dangerous, and we have never needed to administer an anti-hypertensive medication in response to psilocybin effects. Modification of these limits may be considered in future studies if safety continues to be observed under these parameters.
Certain medications may alter the effects of a hallucinogen and therefore individuals taking these medications should be excluded from participation. Specifically, chronic administration of tricyclic antidepressants and lithium (Bonson and Murphy, 1996), and acute administration of serotonin reuptake inhibitors (Fiorella et al., 1996) and the antipsychotic medication haloperidol (Vollenweider et al., 1998) have been shown to potentiate hallucinogen effects, and therefore participants’ use of these represents a safety concern. Chronic administration of serotonin reuptake inhibitors (Stolz et al., 1983; Strassman, 1992; Bonson et al., 1996) and monoamine oxidase inhibitors (Bonson and Murphy, 1996) have been shown to decrease sensitivity to hallucinogens, and therefore participants’ use of these represents a scientific concern. We also advise investigators to include questions concerning over-the-counter dietary supplements in addition to prescription medications when probing medication history, and to exclude those taking potentially problematic substances (e.g., 5-hydroxytryptophan and St. John’s Wort may affect serotonergic function, and, therefore, it is appropriate to exclude individuals currently or recently taking these products). It should also be noted that administration of ayahuasa (which contains monoamine oxidase inhibitors in addition to DMT) to individuals taking serotonin reuptake inhibitors may lead to a severe serotonin syndrome reaction (Callaway and Grob, 1998).
Psychiatric screening criteria are important for minimizing the already low chances of precipitating a longer-term psychotic reaction by hallucinogen administration. Thorough psychiatric interviews (e.g., SCID; First et al., 2001) should be conducted in order to identify contraindicated psychological functioning or history. In our research, individuals are excluded who have a current or past history of meeting DSM-IV criteria for schizophrenia or other psychotic disorders (unless substance-induced or due to a medical condition), or bipolar I or II disorder, which are the most important conditions to exclude for ensuring safety. We also exclude those with a first or second-degree relative with these disorders. There is considerable evidence from family, twin, and adoptive studies that genetic factors make a robust contribution to the etiology of schizophrenia, with genetic factors established as relevant to some, perhaps all cases (Buchanan and Carpenter, 2005). In fact, data indicate there is approximately a six-fold greater chance of developing schizophrenia in second-degree relatives of individuals with schizophrenia (Patel et al., 2003). Other investigators have also excluded individuals scoring high on the personality traits of rigidity and emotional lability on the grounds that these have been significantly associated with negative experiences during hallucinogen action and during non-pharmacologically induced altered states of consciousness (Dittrich, 1993; Hasler et al., 2004).
Depending on the nature of the study, it may be appropriate to exclude those with other psychiatric disorders as well. Unless the research study is designed to specifically address a question relevant to a specific psychiatric disorder, our advice is to select a population that is psychiatrically healthy. This strategy is warranted because the effects of hallucinogens may potentially interact with various psychiatric disorders. Furthermore, including volunteers with psychiatric disorders may increase the chances that symptoms from such disorders may inadvertently be misattributed to hallucinogen action. For example, our recent studies with healthy volunteers have excluded volunteers with a current or a recent past history (e.g., within the last 5 years) of alcohol or drug dependence (excluding caffeine and nicotine) or major depression, and volunteers with current obsessive-compulsive disorder, dysthymic disorder, panic disorder, dissociative disorder, anorexia nervosa, or bulimia nervosa.
Recent and current studies have investigated therapeutic applications of psilocybin for psychiatric disorders (Grob, 2005; Moreno et al., 2006). Because preliminary reports have suggested safety, studies examining therapeutic indications are likely to continue. These studies target for participation volunteers with disorders that would normally be excluded from non-treatment studies. Therefore, additional considerations are appropriate for such studies. For example, in a study of hallucinogen-assisted therapy for depression or anxiety, individuals should be excluded whose symptoms of depression or anxiety are sufficiently severe to warrant immediate treatment with medication (e.g., due to suicidal ideation). In addition, clinical treatment studies may choose to lift restrictions on relatively minor non-target psychiatric disorders that would be excluded in studies with healthy volunteers. For example, a study of hallucinogens in the treatment of anxiety related to cancer might choose to allow the inclusion those with comorbid dysthymic disorder or mild obsessive-compulsive disorder. Investigators should examine the relevant evidence when considering lifting specific exclusions, proceed cautiously, and implement any supplemental safeguards that might be appropriate for such exceptions.
Study personnel
It is difficult to overemphasize the importance of the interpersonal atmosphere created by study staff in influencing a volunteer’s response to a hallucinogen. Most critically, this applies to the interpersonal environment created by the actual session monitors (Leary et al., 1964; Masters and Houston, 1966). We use the term “monitor” to refer to the staff members who will be with the participant in the session room during the course of hallucinogen action. The monitors should be knowledgeable about the medical and psychological markers of potential adverse reactions to the drug. Furthermore, monitors should have significant human relation skills and be familiar with descriptions of altered states of consciousness induced by hallucinogens. Personal experience with techniques such as meditation, yoga, or breathing exercises may also prove to be helpful in facilitating empathy for volunteers that experience altered states of consciousness during hallucinogen action. The lead monitor for each participant in the Johns Hopkins studies to date has been a clinical psychologist or a clinical social worker. However, we believe clinical sensitivity (e.g., empathy, respect) is likely more important than formal degrees when considering monitor qualifications.
We recommend the presence of at least two monitors during hallucinogen administration sessions so that the volunteer will never be alone should one monitor need to briefly leave the session room (e.g., to the restroom). For each participant in the Johns Hopkins studies, we have specified a primary monitor (who takes the lead in participant interactions) and an assistant monitor, with differing required levels of involvement for the two monitors during volunteer preparation (see Preparation of volunteers section below). In prior research into potential treatment applications of hallucinogens, the presence of both genders in the monitoring team has been recommended (Grof and Halifax, 1977; Grof, 1980; Kurland, 1985). Having both genders present may foster feelings of security. In the Johns Hopkins studies, we have followed this recommendation when possible, but also have conducted sessions in which the primary and assistant monitors were of the same gender as the volunteer. We would counsel against both members of the monitoring team being the opposite gender of a volunteer unless there is a staff member of volunteer’s gender who has established some rapport with the volunteer in advance, and who can quickly be summoned to assist should support be needed in the restroom. For studies that are intended to maximize the potential for mystical-type experience during hallucinogen administration, an additional valuable monitor characteristic may be her or his ability to interact with and relate to the participant concerning spiritual issues (e.g., Moss and Dobson, 2006; Council on Spiritual Practices, 2001).
Although the volunteer’s interactions with the monitors are of paramount importance, all individuals at the study site having contact with the volunteer on or before the session day may influence a volunteer’s reaction to a hallucinogen. Pre-session negative mood consisting of anxiety or depression has been shown to significantly predict anxious or other negative experiences during the session (Metzner et al., 1965). Strassman (2001) reported that a visiting medical student’s unexpected interaction with a volunteer before the session may have contributed to an adverse event resulting in the volunteer leaving the study site under the influence of psilocybin. To the degree possible, investigators should work with all personnel that the volunteer may encounter (e.g., receptionist, building security, nurses) to ensure that volunteers are treated with courtesy and respect. For example, in the Johns Hopkins studies, a research staff member other than the study monitors meets with the volunteer in the morning and administers a few pre-session questionnaires and manages other logistics. This staff member should be friendly, welcoming, and compassionate, as he or she inquires as to the volunteer’s current emotional and physical well being (e.g., recent sleeping history, interpersonal or work stressors, anticipation of session, adherence to study dietary and medication/drug restrictions). The staff member should maintain a positive social rapport with the volunteer to reduce the likelihood of adverse psychological reactions during the session and to gain accurate information on the volunteer’s condition so that other study staff may be notified if there is any potential reason to postpone or cancel the session (e.g., if the volunteer is experiencing a particularly stressful life event or is feeling ill). If any staff member treats the volunteer disrespectfully or coldly (i.e., “like a guinea pig”), this may negatively influence the volunteer’s psychological state and subsequent hallucinogen experience. We recognize that treating volunteers respectfully is an ethical imperative for all human research. However, with hallucinogen administration research, the importance of this mandate is even more compelling given the powerful influence of set and setting on hallucinogen effects. Therefore, we recommend providing additional attention to volunteer rapport beyond what is customary in general human behavioral pharmacology practice.
Physical environment
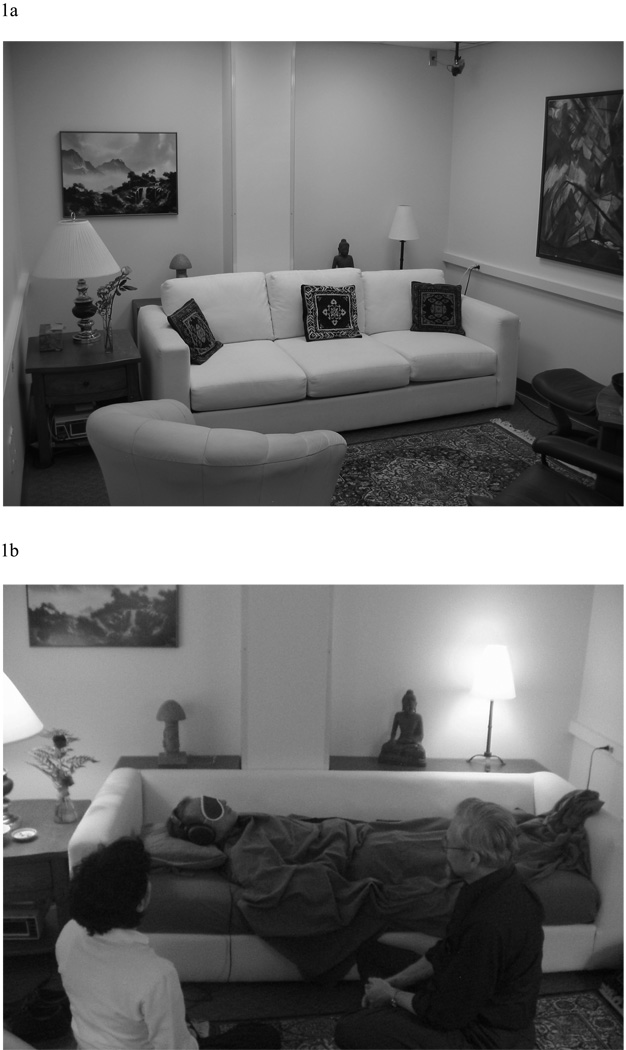
The physical environment during hallucinogen sessions is extremely important for ensuring safety for volunteers in two respects. First, an aesthetically pleasing environment may decrease the probability of acute psychological distress. The Johns Hopkins hallucinogen research projects use a living room-like setting (see Figure 1). The furniture is comfortable and is atypical for a research laboratory or medical office setting. An overly “clinical” environment with an “antiseptic” look (e.g., white walls, extraneous medical equipment, personnel in white lab coats) may increase anxious reactions. Strassman (2001) noted that the medically oriented environment in which his DMT studies were conducted may have contributed to volunteers having unpleasant subjective experiences. For example, some volunteers reported vivid and realistic experiences of being medically examined by extraterrestrials. It has also been noted that many of the potentially unpleasant physical reactions to hallucinogens (e.g., subjective changes in temperature, difficulty in breathing, various bodily sensations) might be in part psychosomatic in nature (Blewett and Chwelos, 1959), and therefore possibly more likely in settings evocative of medical conditions (Masters and Houston, 1966). Some protocols may require videotaping of sessions for scientific purposes. Although there might be concern that videotaping could increase self-consciousness or paranoia, we have no evidence that this has occurred in the Johns Hopkins studies, in which videotaping of sessions is routine.
Figure 1.
The living room-like session room used in the Johns Hopkins hallucinogen research studies. Aesthetically pleasing environments such as this, free of extraneous medical or research equipment, in combination with careful volunteer screening, volunteer preparation, and interpersonal support from two or more trained monitors, may help to minimize the probability of acute psychological distress during hallucinogen studies. For studies that investigate potential therapeutic effects or the phenomenology of introspective hallucinogen experiences, the use of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel.
Beyond the psychological importance of a comfortable, relaxing environment, attention must be paid to the physical safety of the environment. The environment should be designed keeping in mind the perceptual changes and disorientation that can occur under the influence of hallucinogens. Thus, any potentially dangerous objects (e.g., furniture with sharp corners; glass lamps) should be avoided. If there is a window in the room, the investigators need to be confident that the volunteer could not exit the window if in a delusional state. Additionally, the session room should not have a telephone, and the participant should surrender her or his cellular telephone before the session. Not only may an incoming telephone call be distracting or alarming while under the influence of a hallucinogen, but it may also represent a safety risk, as Strassman (2001) has reported a case in which a participant used a session room telephone to call a companion, which culminated in the two fleeing the study site. Having a private restroom located near the session room would be ideal for volunteer use during the session. A shared restroom may be used if the monitors ensure that the volunteer does not interact with non-study personnel while going to the restroom (more details under the section Conduct of hallucinogen administration sessions). Of course, most research laboratories do not provide the ideal physical environment. Thus, resourcefulness and ingenuity may be necessary to convert a less than ideal location into a relaxing and secure environment.
Preparation of volunteers
As with any human research with psychoactive drugs, volunteer preparation at the earliest stages must include a thorough review of the consent form, which should include in plain language the range of experiences that may result from hallucinogen administration, including changes in perception, sense of time and space, and emotion (possibly including anxiety, fear, panic, and paranoia). Relative to other drug classes, the subjective effects of hallucinogens are likely more difficult to describe to a naïve volunteer; therefore, additional time may be necessary to fully discuss these potential effects with volunteers. The consent form should also include the approximate timecourse of the drug, the state of knowledge concerning its toxicity profile, and its status as an experimental drug. In addition, the consent form should state that there is a relatively small risk of adverse effects that last for hours to days after the hallucinogen session. These include mood disorders (such as depression), psychotic disorders, and anxiety disorders. It should also state that there are rare reports in which hallucinogen exposure appears to cause, accelerate, or precipitate the onset of significant or lasting psychiatric illnesses such as psychoses and intermittent or persisting visual perceptual abnormalities (“flashbacks,” HPPD).
The next step in volunteer preparation is to conduct a series of meetings between the monitors and volunteer in order to build rapport and trust. The relationship between the monitors and the volunteers should be well established by the time of the first session (Masters and Houston, 1966). In the Johns Hopkins studies, there are at least eight contact hours over the course of at least four meetings, usually over a one-month period. One of these preparatory meetings should be conducted in the room in which the hallucinogen is to be administered, in order to familiarize the participant with the physical environment. The primary monitor meets with the volunteer during all of these meetings, while the assistant monitor is required to be present on at least one occasion. It is important that the assistant monitor, in addition to the primary monitor, has developed a trusting relationship with the volunteer because this assistant monitor will be the only person in the session room with the volunteer if the primary monitor needs to leave briefly.
During these preparatory meetings, the monitors discuss meaningful aspects of the volunteer’s life. The main purpose of the participant-monitor meetings is to develop rapport and trust, which we believe helps minimize the risk of fear or anxiety reactions during the hallucinogen session. This typically includes discussions of the volunteer’s childhood, romantic life, current relationships with family and friends, and the volunteer’s philosophical and/or spiritual beliefs. Reviewing personal history and feelings may be important for two reasons. First, this discussion helps establish a significant level of trust. The interaction should convey that all aspects of the person are welcome, from the petty to the noble, from embarrassments to achievements, and from sorrow to joy. By the time of the hallucinogen session day, the volunteer will ideally feel completely comfortable with the monitor, reducing the likelihood of paranoia (e.g., feeling that the monitors are trying to control her or his mind, or have deceived the volunteers about the nature of the study). Second, related personal material may “emerge” under the effects of the hallucinogen. That is, the volunteer may experience intense thoughts, feelings, and visions related to his or her personal history or world-view. Knowing about the volunteer’s life will allow the monitor to better understand her or his session experience and help the monitor in providing interpersonal support should strong emotions arise. If it is felt that sufficient rapport and trust have not developed during these monitor meetings, then either additional contact hours should be provided, or the volunteer’s participation should be cancelled. A high dose of a hallucinogen should not be administered to a volunteer if sufficient trust has not been established. As with other forms of human research involving the development of rapport and trust (e.g., clinical trials involving psychotherapy) investigators should be careful that this rapport and trust does not create a situation in which the volunteer feels obligated to remain in the study. Volunteers and monitors should be clear that participation is voluntary, and that the participant will be fully supported if her or his decision is to quit the study.
At some point during preparatory meetings, time must be devoted to explaining the study logistics. These should include the timing of the session (e.g., what time to arrive at the laboratory if an outpatient study, what time the session is likely to end), any restrictions on diet or contraindicated medicines, drugs, or nutritional supplements (e.g., if fasting or a low-fat diet is required the morning before session), and any requirements of other people (e.g., if a family member or friend is to pick up the participant at the end of the session).
This discussion should also include thorough descriptions of study procedures, to the degree allowable by blinding issues. For example, if cognitive or memory tests are to be performed, or questionnaires are to be answered, the participants should be aware of these requirements. If physiological measures such as blood pressure are to be taken during the time of drug action, this also should be explained. The activities during hallucinogen action will naturally depend on the scientific questions under investigation. Whatever the nature of the experiment after hallucinogen administration, the scenario should be thoroughly discussed with the volunteer in preparation. In some cases, such as with brain imaging research, it may be helpful for volunteers to be run through a preliminary research session in order to familiarize them with the equipment and procedures. Some studies have conducted an initial non-blind hallucinogen administration session, in which safety measures are assessed, before subsequent blinded sessions in order to, among other reasons, acquaint volunteers with the effects of the drug before the introduction of additional, potentially-anxiety provoking measures (e.g., blood draws) (Strassman and Qualls, 1994; Strassman et al., 1994; Strassman et al., 1996).
The preparation of the volunteer should involve a detailed discussion of the possible range of experiences that may be encountered after hallucinogen administration. This includes the typical onset and duration of the drug(s) under investigation. Preparation involves discussion of the various potential physical sensations, such as nausea, or heightened awareness of physiological processes such as breathing and heartbeat. Volunteers are encouraged to trust that their bodies will continue to function properly regardless of such sensations, and that these bodily processes will continue without the volunteers’ volitional control.
The major categories of potential psychological experiences during hallucinogen action should be discussed with the participant. The range of subjective experience under hallucinogens can be remarkably broad (Blewett and Chwelos, 1959; Richards, 1980; Masters and Houston, 1966; Strassman, 2001; Nichols, 2004; Stolaroff, 2004). This range of experiences includes perceptual changes such as visual illusions, intensification of colors, proprioceptive changes (e.g., one’s body may feel gigantic or tiny), and synesthesia (e.g., seeing sounds or hearing colors). Another type of possible experience is the alteration of emotions, such that emotions of either a positive or negative nature may be greatly intensified, yielding experiences that may range from euphoria to despair. Another category of possible effects involves changes in the sense of time and space. At the extremes, time and/or space may be experienced as infinite or nonexistent. Other experiences may include thoughts, feelings, or insights concerning one’s personal history (e.g., revisiting childhood memories) or current life circumstances (e.g., relations with loved ones), highly symbolic experiences (e.g., involving religious symbols, animals, etc.), and experiences described by some to be of a mystical or spiritual nature. Importantly, it should be emphasized that these experiences may consist of much more than the participant subjectively observing internal and external events. Rather, the effects may involve a profound change in one’s sense of self, such that one feels as if he or she is merging into the surrounding environment or the entire universe (Schultes et al., 2001). The individual may temporarily experience a complete loss of subjective self-identity, a phenomenon sometimes referred to as “ego loss” or “ego death” (e.g., Leary et al., 1964; Grof and Halifax, 1977; Grof, 1980). While a detailed discussion concerning the range of possible hallucinogen effects will enhance safety by psychologically preparing the participant for the unique and often intense effects of a hallucinogen, it may also serve to undermine the blind. That is, such preparation may train the participant on how to identify a hallucinogen by its effects. Nonetheless, the primary concern must be the participant’s safety. Therefore, researchers must minimize the potential for unblinding by manipulating other aspects of the experimental design, such using hallucinogen-naïve participants or the use of an active placebo (e.g., Griffiths et al., 2006).
The volunteers should be given guidance on how to handle difficult hallucinogen experiences. Whether the disturbance consists of frightening illusions or internal imagery, difficult thoughts and feelings about some past or present personal issue, or anxiety related to a radical change in sense of self (e.g., temporary loss of self-identity), the volunteer is encouraged to mentally surrender to the experience, trusting that her or his usual state of consciousness will return when the drug effects resolve (Blewett and Chwelos, 1959; Masters and Houston, 1966; McCabe, 1977). For example, if the participant experiences disturbing internal imagery of a demon or monster, he or she is encouraged to mentally approach the figure and interact with it (e.g., imagine asking the figure why it has appeared), rather than attempt to flee from the disturbing imagery. The participant should be alerted that sometimes people experience extremely convincing sensations of dissolving, melting, exploding, and so forth, and that the best way to deal with all such situations is to surrender to the experience, subjectively allowing oneself to dissolve, melt, or explode. Similar advice applies to physical symptoms such as nausea; for example, participants may be encouraged to “dive in” to their stomachs, which may alleviate the nausea, as it has been suggested anecdotally that nausea and other somatic discomforts may in part be of a psychosomatic nature (Blewett and Chwelos, 1959; Masters and Houston, 1966).
The preparation of volunteers for hallucinogen administration will require balancing the ethical requirements to prepare the volunteer for the potentially powerful psychological effects of hallucinogens, with the scientific concern not to bias the volunteer with respect to the dependent variables. This is especially true because classical hallucinogens have been shown to increase suggestibility in an experimental model involving body sway (Sjoberg and Hollister, 1965; Middlefell, 1967), and suggestibility has been proposed as a potential mechanism of the possible therapeutic efficacy of hallucinogens (Dobkin de Rios et al., 2002; Barbosa et al., 2005). That is, one could argue that examples conveyed during preparation are then experienced during the session only due to an increased level of suggestibility during hallucinogen action. Increased suggestibility would seem to be of greatest concern as a confound when investigating the phenomenology of subjective hallucinogen occasioned experience (e.g., the study by Griffiths et al., 2006, demonstrating that psilocybin can occasion mystical-type experiences under supportive conditions). In the study by Griffiths and colleagues (2006), although experiences of a spiritual variety were included among the range of possible effects conveyed in preparation, the monitors emphasized that these experiences were not the only variety of interesting or valuable effects that might occur. Specific categories of mystical-type experience to be assessed in measures were not discussed. In the Johns Hopkins studies we have not encouraged participants to read the diverse and widely varying published accounts of hallucinogen effects as part of their preparation because this may introduce compelling idiosyncratic expectations. Our research has proceeded safely by delivering all such preparatory information to participants verbally during pre-session meetings with monitors. Researchers will need to design studies such that a maximum amount of preparation is provided for safety reasons while not confounding the particular hypotheses being studied. Furthermore, controlled studies should ensure that the unique preparation methods and research environment qualities described herein are in place, under double-blind conditions, for both hallucinogen and placebo groups (or conditions). For example, in the study by Griffiths and colleagues (2006), the use of identical procedures under double-blind conditions for psilocybin sessions and the active placebo (a high dose of methylphenidate) sessions permitted a reasonable degree of control over suggestibility.
Conduct of hallucinogen administration sessions
As with research with many other psychoactive drugs, a physician should be available during hallucinogen sessions should any untoward medical complications arise. Furthermore, medication for the treatment of acute hypertension (e.g., intravenous labetalol) should be immediately available in the event that blood pressure exceeds pre-determined safety parameters.
Adverse psychological reactions to hallucinogens will be minimized when studies are conducted under conditions that provide strong interpersonal support to the participants (Blewett and Chwelos, 1959; Chwelos et al., 1959; Pahnke, 1969; Masters and Houston, 1966). The monitors should carefully observe the participant and be vigilant for signs of psychological distress. If the volunteer needs to walk in order to complete study tasks or to go to the restroom, the monitors should stand close by in order to assist by gently holding an arm or shoulder. Even with high doses of hallucinogens, individuals do not typically show substantial motor impairment, and will likely be able to ambulate without considerable difficulty (with the exception of hallucinogens such as parenteral DMT with abrupt effects and short duration of action). However, perceptual and proprioceptive effects may make walking disorienting, which is why gentle guidance may be helpful. One of the monitors should always be present in the session room with the participant. Because the session monitors will have developed rapport and trust with the participant, they should be the only people to interact with the volunteer during the course of hallucinogen action, barring any non-routine event (e.g., fire alarm, medical intervention by a specialist). Individuals who are anticipated to have contact with the volunteer during the course of hallucinogen action (e.g., nurse, physician) should have at least met with the volunteer once prior to session to develop some degree of rapport and trust.
For all but the shortest acting hallucinogens (e.g., parenteral DMT), the participant is likely to need to use the restroom at some point while experiencing hallucinogen effects. If a private restroom is not available, then study staff should escort the volunteer to assure that no one is in the restroom. Either the restroom door needs to have no lock, or study staff should have a key readily available if needed. Cohen (1960) reported a case in which a depressed patient who had been administered LSD barricaded himself into a room in order to attempt suicide. In the Johns Hopkins studies, sessions are conducted in a room located on the third floor of a research facility. The session room itself has a private restroom just outside of the session room. During sessions, the volunteer is closely escorted to the restroom and a session monitor waits just outside the restroom to be available if the volunteer should encounter any difficulties. Furthermore, waiting in this area outside the restroom allows the monitors to ensure that the volunteer does not exit the research site. Any attempt by a disoriented volunteer to leave the session area would be met with compassionate but firm direction to return to the session room.
Serious attention must be devoted to the possibility of volunteers trying to leave the study site under the influence of a hallucinogen. Walter Pahnke’s (1963) dissertation study (known as the “Good Friday Experiment”) examined the ability of a high dose of psilocybin to occasion mystical experiences by administering either psilocybin or placebo (randomly assigned) to seminary students in a small, basement chapel into which a Good Friday service from the main sanctuary was broadcast. A retrospective investigation conducted over 25 years after the original experiment revealed that two volunteers left the chapel under the influence of psilocybin (Doblin, 1991). One of these volunteers reported feeling imprisoned in the chapel and left the chapel during a portion of the experiment. The other volunteer abruptly left the chapel believing that God had chosen him to immediately announce to the world the dawning of an age of peace (Roberts and Jesse, 1997; Smith, 2000). This volunteer was apprehended by the research staff and administered the antipsychotic agent chlorpromazine after efforts to calm him were unsuccessful (Doblin, 1991; Roberts and Jesse, 1997; Smith, 2000). Strassman (2001) also reported an incident in which a participant experiencing the full effects of a high dose of psilocybin evaded the research staff and left the research site. Fortunately the participant’s spouse monitored the participant and no one was injured.
The risks of allowing a research volunteer experiencing the effects of a hallucinogen to leave the study site are significant. For example, in a bewildered or delusional state, the person might walk into traffic or attempt to drive. Although many hallucinogen users maintain reasonable control while under the influence of hallucinogens, panic or delusional reactions to hallucinogens have in rare circumstances resulted in tragic consequences such as jumping out of windows (Keeler and Reifler, 1967; Reynolds and Jindrich, 1985; Reitman and Vasilakis, 2004; O’Brien, 2006). Interestingly, the volunteer who fled Strassman’s (2001) study site on psilocybin was a carefully screened, experienced LSD user. Therefore, it is imperative for safety reasons that the study site environment, session procedures, and participant preparation all minimize the chance of a volunteer leaving the study site.
Strategies for handling non-routine scenarios should be considered. For example, how are study monitors and the volunteer expected to respond in the event of a fire alarm or fire? On the single occasion at Johns Hopkins in which a fire alarm sounded during a session, the two study monitors closely escorted the volunteer outside, making sure to minimize contact with other individuals. The three of them walked to a nearby quiet area with an attractive landscape and enjoyed the scenery until the volunteer and monitors could return to the building. The monitors encouraged the participant to view the occasion as an opportunity to enjoy the natural world outdoors (something normally unavailable during sessions), rather than as an impediment to having a successful session. If any non-routine events occur, the monitors should maintain contact with the volunteer throughout.
If participants become anxious during the course of hallucinogen action, it is now widely recognized that the appropriate first response is to provide strong personal support and reassurance (O’Brien, 2006). This primarily includes interacting with the volunteer in a comforting and reassuring manner. If the volunteer is behaving anxiously and a negative psychological reaction seems to be escalating, the monitors should convey a solid sense of security and calm, while empathizing with what may be an incredibly intense and unpleasant experience. Attempts to “talk down” the participant (i.e., the use of reality-defining techniques in order to distract the participant from or attenuate the altered state of consciousness) may be counterproductive and aggravate a difficult reaction (McCabe, 1977). Instead, participants should be reminded to surrender to the experience. Appropriate forms of reassurance may include a supportive touch to the arm or shoulder with verbal reminders that the participant is in a research study, has taken the hallucinogen, and that he or she will return to normal consciousness in “a few minutes” or “a few hours” (or whatever the appropriate estimate may be, depending on the specific drug under study and when it was administered). During an intense hallucinogen-occasioned experience when verbal interactions may be of limited help, a powerful form of reassurance (sometimes called “interpersonal grounding”) is simply holding the hand of the participant (McCabe, 1977). Many volunteers report that during such experiences, a reassuring hand provides an incredible sense of stability and connection. Monitors should demonstrate this practice during preparation to normalize hand holding during sessions.
If volunteers have been appropriately screened and the guidelines herein followed, reassurance should be sufficient to diffuse acute psychological distress in the vast majority of cases. For example, in recent studies in our laboratory, in which we have administered high doses of psilocybin to 54 volunteers, reassurance has been sufficient to handle all cases of acute psychological distress that have arisen. Although pharmacological intervention is a last resort and should rarely, if ever, be needed, medications should be readily available for use if the need arise. For cases in which acute psychological distress is insufficiently managed with reassurance alone, treatment with a benzodiazepine anxiolytic is the pharmacological intervention of choice (Abraham and Aldridge, 1993; Frecska and Luna, 2006; O’Brien, 2006). In these cases we recommend a 10 mg oral dose of diazepam (Grinspoon and Bakalar, 1979), although oral doses of 15–30 mg per hour or every few hours as needed have been recommended for pharmacological treatment of “bad trips” that do not respond to reassurance in emergency department settings (Ungerleider and Frank, 1976). Because of its high lipid solubility, diazepam has a more rapid onset, a shorter time until peak plasma concentration, and a shorter duration of therapeutic action than many other benzodiazepines including lorazepam, despite the fact that lorazepam has a shorter elimination half-life (Greenblatt and Shader, 1985; Funderburk et al., 1988). Although the intravenous route may be considered, the oral route is preferable because intravenous injection procedures may further exacerbate the participant’s anxiety. Also, antipsychotic medications (e.g., risperidone, olanzapine) should be available in the event that an adverse reaction escalates to unmanageable psychosis. However, experienced clinicians have suggested that although antipsychotic medications may reduce psychotic behavior through sedation, their use may be problematic because the effects may be abrupt, unpleasant, and intense and their use may result in subsequent psychological problems (McCabe, 1977; Grinspoon and Bakalar, 1979; Grof, 1980). Furthermore, pretreatment with the antipsychotic haloperidol has been shown to exacerbate the psychosis-like effects of psilocybin (Vollenweider, et al., 1998), suggesting that haloperidol should not be used as a rescue medication. Although not approved for use in the United States, ketanserin (a 5-HT2A antagonist) pretreatment has been shown to attenuate psilocybin effects (Vollenweider, et al., 1998), suggesting possible use as a rescue medication for hallucinogen administration. Ultimately the decision to medicate will depend on whether the monitors and responsible physician judge that they are capable of maintaining the safety of the volunteer and others without medical intervention. Bringing the participant to the emergency department represents an ultimate “last resort” in the treatment of a very difficult (i.e., psychotic) reaction. However, medical evaluation by well-meaning emergency department personnel who are inexperienced with hallucinogen effects can readily escalate and prolong an adverse reaction. Therefore, all possible efforts should be made to treat a difficult experience in the session context, even if pharmacological intervention is required.
The conduct of the session will largely be based on the particular research topics being studied. The research requirements of many types of studies will require the participants to adhere to regimented testing conditions (e.g., cognitive tests, memory tests, brain scans). In such investigations, interference with procedures may be minimized by judiciously selecting dose and the hallucinogen experience level required of volunteers. Adverse reactions will generally be more likely at higher hallucinogen doses; however, adverse reactions can potentially occur at any dose level. Experienced hallucinogen users may be particularly appropriate participants for studies involving challenging conditions, such as remaining immobile for long periods in a confining brain imaging scanner. Regardless of experience level and dose, however, the possibility of psychological adverse reactions exists whenever a hallucinogen is administered. To the degree possible, investigators should attempt to implement their scientific protocols as planned. However, monitors should always be vigilant for potential adverse psychological reactions. In the event of a significant adverse psychological reaction, interpersonal support should be provided even if it interferes with data collection. Clearly, volunteer safety must take priority over scientific procedures. In studies such as ours, in which participants are encouraged to focus their attention inward by wearing eyeshades and listening to music through headphones, our advice is for monitors to occasionally probe the volunteer’s psychological well-being (e.g., ask the volunteer, “Would you like to describe where you find yourself?”) to ensure that the volunteer is not experiencing significant anxiety and is in need of support.
For studies that investigate potential therapeutic effects or the phenomenology of hallucinogen experiences (i.e., studies that do not require participants to engage in research tasks during the session), the employment of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel. This may be especially important for volunteers who are experiencing the effects of a hallucinogen for the first time. Typically, we have kept eyeshades and headphones in place for most of the session. In the latter hours of the session some time is spent with the volunteer sitting on the couch, interacting without eyeshades and headphones, although music may still be played through speakers to provide nonverbal structure and continuity. As a whole, we encourage our participants to “collect experiences” to discuss after the drug effects have abated, and discourage attempts to analyze material or communicate excessively while the atypical states of consciousness are still occurring.
After the effects of the hallucinogen have resolved, the participant should either be released into the care of a friend or family member or required to stay overnight at the research site for monitoring. If participants are released from the study site after the session, they should be instructed not to drive an automobile or engage in any other potentially dangerous activity for the remainder of the day. At Johns Hopkins, volunteers are released into the care of a friend or family member, who has been appropriately oriented by our staff to be available to emotionally support the participant, but also to provide space (i.e., be in another room) if the participant feels the need to be alone. We have also given the participant the primary monitor’s pager number to call if he or she feels the need for support that evening. Of the 54 volunteers tested at a high psilocybin dose to date, no one has paged the monitor, although volunteers do seem to appreciate this opportunity for additional support.
Post-session procedures
After the session, safety monitoring should continue in the form of one or more post-session meetings (typically the next day) between the primary monitor and participant to ensure psychological stability and provide an opportunity for the volunteer to discuss thoughts or feelings from the session. As with any acute, intense positive or negative emotional experience, participants often feel the need for, and seem to benefit from, additional time for reflecting on the novel thoughts and feelings that may have arisen in the session. Given the potentially intense and unusual psychological nature of hallucinogen effects, the volunteer may have difficulty discussing the experience with others in her or his life. Because the monitors were present during the session when the hallucinogen effects were experienced and have knowledge of a broad range of reported phenomena during drug action, the volunteer may feel more comfortable discussing her or his experiences with the monitors than with others. This follow up contact also allows the assessment of any potentially persisting adverse effects, including perceptual abnormalities. More than one post-session meeting may be necessary if the volunteer is experiencing psychological difficulty concerning thoughts and feelings encountered during the session. Of the 54 volunteers tested with a high dose of psilocybin at Johns Hopkins to date, none has shown evidence of persisting psychosis or psychological problems related to their sessions, and all have returned to their normal daily activities. If the primary session monitor is not a clinically trained psychologist or psychiatrist, it is prudent for research teams to have available for consultation a clinically trained psychologist or psychiatrist familiar with altered states of consciousness, who can work with patients who appear to have developed psychological difficulties stemming from hallucinogen administration.
Concluding remarks
After a decades-long period of dormancy in response to the sensationalism surrounding the nonmedical use of hallucinogens during the 1960’s, human hallucinogen research has resumed in the United States and Europe, and is now beginning to address a variety of important basic research questions as well as potential therapeutic applications (Nichols, 2004). In light of the unusual history of restriction on human research with this class of compounds, it is critical for investigators to implement appropriate and conservative safeguards. With such safeguards this class of compounds can be studied safely in humans. Careless research that lacks attention to the unique risk profile of hallucinogens may not only endanger the safety and well-being of the research participants, but may also jeopardize future human research with these scientifically fascinating compounds. On the other hand, carefully conducted research that respects hallucinogens’ unique and often powerful psychological effects may potentially inform the treatment of various psychiatric disorders, as well as lead to significant advances in our understanding of perception, cognition, behavior, the psychology of religion, and the biological underpinnings of consciousness.
Acknowledgments
Support for preparation of this manuscript was provided by grants from NIH (R01 DA03889), the Council on Spiritual Practices, and the Heffter Research Institute. We thank George Greer, M.D., Charles Grob, M.D., Robert Jesse, Annie Umbricht, M.D., and Franz Vollenweider, M.D. for helpful comments on previous versions of this manuscript. We also thank the staff of the Johns Hopkins psilocybin research studies, whose insights have contributed to these guidelines, including Mary P. Cosimano, M.S.W. and Brian D. Richards, Psy.D. for their roles in screening volunteers and monitoring sessions, and Lawrence P. Carter, Ph.D., Ryan K. Lanier, Ph.D., Benjamin McKay, Chad J. Reissig, Ph.D., and Ryan G. Vandrey, Ph.D. for their assistance in monitoring sessions.
References
- Abraham HD, Aldridge AM. Adverse consequences of lysergic acid diethylamide. Addiction. 1993;88:1327–1334. doi: 10.1111/j.1360-0443.1993.tb02018.x. [DOI] [PubMed] [Google Scholar]
- Abramson HA, editor. The Use of LSD in Psychotherapy. New York: Josiah Macy Jr. Foundation Publications; 1960. [Google Scholar]
- Abramson HA, editor. The Use of LSD in Psychotherapy and Alcoholism. New York: Bobbs-Merrill; 1963. [Google Scholar]
- Abuzzahab FS, Anderson BJ. A review of LSD treatment in alcoholism. Int Pharmacopsychiat. 1971;6:223–235. doi: 10.1159/000468273. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Baggott MJ, Erowid E, Erowid F, Robertson LC. Chronic visual changes in hallucinogen users: a web-based questionnaire. Poster presented at the 2006 meeting of the College on Problems of Drug Dependence; Scottsdale, AZ. 2006. [Google Scholar]
- Barbosa PC, Giglio JS, Dalgalarrondo P. Altered states of consciousness and short-term psychological after-effects induced by the first time ritual use of ayahuasca in an urban context in Brazil. J Psychoactive Drugs. 2005;37:193–201. doi: 10.1080/02791072.2005.10399801. [DOI] [PubMed] [Google Scholar]
- Bender L, Siva Sankar DV. Chromosome damage not found in leukocytes of children treated with LSD-25. Science. 1968;159:749. doi: 10.1126/science.159.3816.749. [DOI] [PubMed] [Google Scholar]
- Blewett DB, Chwelos N. Handbook for the Therapeutic Use of Lysergic Acid Diethylamide-25: Individual and Group Procedures. 1959. [Accessed October 9, 2007]. http://www.erowid.org/psychoactives/guides/handbook_lsd25.shtml. [Google Scholar]
- Bonson KR, Buckholtz JW, Murphy DL. Chronic administration of serotonergic antidepressants attenuates the subjective effects of LSD in humans. Neuropsychopharmacology. 1996;14:425–436. doi: 10.1016/0893-133X(95)00145-4. [DOI] [PubMed] [Google Scholar]
- Bonson KR, Murphy DL. Alterations in responses to LSD in humans associated with chronic administration of tricyclic antidepressants, monoamine oxidase inhibitors or lithium. Behav Brain Res. 1996;73:229–233. doi: 10.1016/0166-4328(96)00102-7. [DOI] [PubMed] [Google Scholar]
- Buchanan RW, Carpenter WT. Concept of Schizophrenia. In: Sadock RJ, Sadock VA, editors. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 8th ed. Volume 1. Philadelphia: Lippincott, William, Wilkins; 2005. pp. 1329–1345. [Google Scholar]
- Callaway JC, Grob CS. Ayahuasca preparations and serotonin reuptake inhibitors: a potential combination for severe adverse interactions. J Psychoactive Drugs. 1998;30:367–369. doi: 10.1080/02791072.1998.10399712. [DOI] [PubMed] [Google Scholar]
- Carter OL, Burr DC, Pettigrew JD, Wallis GM, Hasler F, Vollenweider FX. Using psilocybin to investigate the relationship between attention, working memory, and the serotonin 1A and 2A receptors. J Cogn Neurosci. 2005;17:1497–1508. doi: 10.1162/089892905774597191. [DOI] [PubMed] [Google Scholar]
- Carter OL, Pettigrew JD, Hasler F, Wallis GM, Liu GB, Hell D, Vollenweider FX. Modulating the rate and rhythmicity of perceptual rivalry alternations with the mixed 5-HT2A and 5-HT1A agonist psilocybin. Neuropsychopharmacology. 2005;30:1154–1162. doi: 10.1038/sj.npp.1300621. [DOI] [PubMed] [Google Scholar]
- Carter OL, Pettigrew JD, Burr DC, Alais D, Hasler F, Vollenweider FX. Psilocybin impairs high-level but not low-level motion perception. Neuroreport. 2004;15:1947–1951. doi: 10.1097/00001756-200408260-00023. [DOI] [PubMed] [Google Scholar]
- Charney DS, Mihic SJ, Harris RA. Hypnotics and sedatives. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th edition. New York: McGraw-Hill; 2006. pp. 401–427. [Google Scholar]
- Chwelos N, Blewett DB, Smith CM, Hoffer A. Use of d-lysergic acid diethylamide in the treatment of alcoholism. Quart J Stud Alcohol. 1959;20:577–590. [PubMed] [Google Scholar]
- Cohen S. Lysergic acid diethylamide: side effects and complications. Journal of Nervous and Mental Disease. 1960;130:30–40. doi: 10.1097/00005053-196001000-00005. [DOI] [PubMed] [Google Scholar]
- Cohen S, Ditman KS. Complications associated with lysergic acid diethylamid (LSD-25) JAMA. 1962;181:161–162. doi: 10.1001/jama.1962.03050280091013b. [DOI] [PubMed] [Google Scholar]
- Cohen MM, Marinello MJ, Back N. Chromosomal damage in human leukocytes induced by lysergic acid diethylamide. Science. 1967;155:1417–1419. doi: 10.1126/science.155.3768.1417. [DOI] [PubMed] [Google Scholar]
- Cohen MM, Hirschhorn K, Frosch WA. In vivo in vitro chromosomal damage induced by LSD-25. New Engl J Med. 1967;277:1043–1049. doi: 10.1056/NEJM196711162772001. [DOI] [PubMed] [Google Scholar]
- Crochet R, Sandison R, Walk A, editors. Hallucinogenic Drugs and Their Psychotherapeutic Use. Springfield, IL: Thomas; 1963. [Google Scholar]
- Cohen S. LSD and the anguish of dying. Harper’s Magazine. 1965;231:69–78. [Google Scholar]
- Council on Spiritual Practices. Code of ethics for spiritual guides. In: Roberts TB, editor. Psychoactive Sacramentals: Essays on Entheogens and Religion. Council on Spiritual Practices; San Francisco: 2001. pp. 250–251. (appendix B) [Google Scholar]
- Dishotsky NI, Loughman WD, Mogar RE, Lipscomb WR. LSD and genetic damage. Is LSD chromosome damaging, carcinogenic, mutagenic, or teratogenic? Science. 1971;172:431–440. doi: 10.1126/science.172.3982.431. [DOI] [PubMed] [Google Scholar]
- Dittrich A. Psychological aspects of altered states of consciousness of the LSD type: measurement of their basic dimensions and prediction of individual differences. In: Pletscher A, Ladewig D, editors. Fifty years of LSD Concurrent status and perspectives of hallucinogens. New York: Parthenon; 1993. pp. 101–118. [Google Scholar]
- Dobkin de Rios M, Grob CS, Baker JR. Hallucinogens and redemption. J Psychoactive Drugs. 2002;34:239–248. doi: 10.1080/02791072.2002.10399960. [DOI] [PubMed] [Google Scholar]
- Doblin R. Pahnke's "Good Friday Experiment": a long-term follow-up and methodological critique. Journal of Transpersonal Psychology. 1991;23:1–28. [Google Scholar]
- Fantegrossi WE, Woods JH, Winger G. Transient reinforcing effects of phenylisopropylamine and indolealkylamine hallucinogens in rhesus monkeys. Behav Pharmacol. 2004;15:149–157. doi: 10.1097/00008877-200403000-00007. [DOI] [PubMed] [Google Scholar]
- Fiorella D, Helsley S, Rabin RA, Winter JC. Potentiation of LSD-induced stimulus control by fluoxetine in the rat. Life Sci. 1996;59:PL283–PL287. doi: 10.1016/0024-3205(96)00490-0. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis 1 Disorders Research Version Patient Edition (SCID-I/P) Biometrics Research. New York: New York State Psychiatric Institute; 2001. [Google Scholar]
- Fischman MW, Johanson CE. Ethical and practical issues involved in behavioral pharmacology research that administers drugs of abuse to human volunteers. Behav Pharmacol. 1998;9:479–498. doi: 10.1097/00008877-199811000-00002. [DOI] [PubMed] [Google Scholar]
- Frecska E, Luna LE. The adverse effects of hallucinogens from intramural perspective. Neuropsychopharmacol Hung. 2006;8:189–200. [PubMed] [Google Scholar]
- Funderburk FR, Griffiths RR, McLeod DR, Bigelow GE, Mackenzie A, Liebson IA, Nemeth-Coslett R. Relative abuse liability of lorazepam and diazepam: an evaluation in 'recreational' drug users. Drug Alcohol Depend. 1988;22:215–222. doi: 10.1016/0376-8716(88)90021-x. [DOI] [PubMed] [Google Scholar]
- Gable RS. Toward a comparative overview of dependence potential and acute toxicity of psychoactive substances used nonmedically. Am J Drug Alcohol Abuse. 1993;19:263–281. doi: 10.3109/00952999309001618. [DOI] [PubMed] [Google Scholar]
- Gable RS. Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction. 2004;99:686–696. doi: 10.1111/j.1360-0443.2004.00744.x. [DOI] [PubMed] [Google Scholar]
- Glennon RA, Titeler M, McKenney JD. Evidence for 5-HT2 involvement in the mechanism of action of hallucinogenic agents. Life Sci. 1984;35:2505–2511. doi: 10.1016/0024-3205(84)90436-3. [DOI] [PubMed] [Google Scholar]
- Gonzales VO Centro Espirita Beneficiente União do Vegetal 546 US. US Supreme Court. 2006. no 04-1084, decided 21 February 2006. [Google Scholar]
- González-Maeso J, Weisstaub NV, Zhou M, Chan P, Ivic L, Ang R, Lira A, Bradley-Moore M, Ge Y, Zhou Q, Sealfon SC, Gingrich JA. Hallucinogens recruit specific cortical 5-HT(2A) receptor-mediated signaling pathways to affect behavior. Neuron. 2007;53:439–452. doi: 10.1016/j.neuron.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Heekeren K, Thelen B, Lindenblatt H, Kovar KA, Sass H, Geyer MA. Effects of the hallucinogen psilocybin on habituation and prepulse inhibition of the startle reflex in humans. Behav Pharmacol. 1998;9:561–566. doi: 10.1097/00008877-199811000-00011. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Heekeren K, Neukirch A, Stoll M, Stock C, Daumann J, Obradovic M, Kovar KA. Inhibition of return in the human 5HT2A agonist and NMDA antagonist model of psychosis. Neuropsychopharmacology. 2006;31:431–441. doi: 10.1038/sj.npp.1300882. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Heekeren K, Neukirch A, Stoll M, Stock C, Obradovic M, Kovar KA. Psychological effects of (S)-ketamine and N,N-dimethyltryptamine (DMT): a double-blind, cross-over study in healthy volunteers. Pharmacopsychiatry. 2005;38:301–311. doi: 10.1055/s-2005-916185. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Schneider F, Friedrich J, Spitzer M, Thelen B, Sass H. Methodological issues of human experimental research with hallucinogens. Pharmacopsychiat. 1998;31:114–118. doi: 10.1055/s-2007-979356. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Thelen B, Habermeyer E, Kunert HJ, Kovar KA, Lindenblatt H, Hermle L, Spitzer M, Sass H. Psychopathological, neuroendocrine and autonomic effects of 3,4-methylenedioxyethylamphetamine (MDE), psilocybin and d-methamphetamine in healthy volunteers Results of an experimental double-blind placebo-controlled study. Psychopharmacology (Berl) 1999;142:41–50. doi: 10.1007/s002130050860. [DOI] [PubMed] [Google Scholar]
- Gouzoulis-Mayfrank E, Thelen B, Maier S, Heekeren K, Kovar KA, Sass H, Spitzer M. Effects of the hallucinogen psilocybin on covert orienting of visual attention in humans. Neuropsychobiology. 2002;45:205–212. doi: 10.1159/000063672. [DOI] [PubMed] [Google Scholar]
- Greenblatt DJ, Shader RI. Clinical pharmacokinetics of the benzodiazepines. In: Smith DE, Wesson DR, editors. The Benzodiazepines: Current Standards for Medical Practice. Lancaster, PA: MTP Press; 1985. pp. 43–58. [Google Scholar]
- Griffiths RR, Bigelow GE, Henningfield JE. Similarities in animal and human drug-taking behavior. Advances in Substance Abuse. 1980;1:1–90. [Google Scholar]
- Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology. 2006;187:268–283. doi: 10.1007/s00213-006-0457-5. [DOI] [PubMed] [Google Scholar]
- Grinspoon L, Bakalar JB. Psychedelic Drugs Reconsidered. New York: Basic Books; 1979. [Google Scholar]
- Grob CS. Psilocybin research with advanced-stage cancer patients. Multidisciplinary Association for Psychedelic Studies (MAPS) Bulletin. 2005;15:8. [Google Scholar]
- Grob CS, Greer GR, Mangini M. Hallucinogens at the turn of the century: an introduction. J Psychoactive Drugs. 1998;30:315–319. doi: 10.1080/02791072.1998.10399707. [DOI] [PubMed] [Google Scholar]
- Grob CS, McKenna DJ, Callaway JC, Brito GS, Neves ES, Oberlaender G, Saide OL, Labigalini E, Tacla C, Miranda CT, Strassman RJ, Boone KB. Human psychopharmacology of hoasca, a plant hallucinogen used in ritual context in Brazil. J Nerv Ment Dis. 1996;184:86–94. doi: 10.1097/00005053-199602000-00004. [DOI] [PubMed] [Google Scholar]
- Grob CS. Psilocybin research with advanced-stage cancer patients. Multidisciplinary Association for Psychedelic Studies (MAPS) Bulletin. 2005;15:8. [Google Scholar]
- Grof S. Perinatal roots of wars, totalitarianism, and revolutions: observations from LSD research. J Psychohist. 1977;4:269–308. [Google Scholar]
- Grof S. LSD Psychotherapy. Pomona, CA: Hunter House; 1980. [Google Scholar]
- Grof S, Goodman LE, Richards WA, Kurland AA. LSD-assisted psychotherapy in patients with terminal cancer. Int Pharmacopsychiatry. 1973;8:129–144. doi: 10.1159/000467984. [DOI] [PubMed] [Google Scholar]
- Grof S, Halifax J. The Human Encounter with Death. New York: EP Dutton; 1977. [Google Scholar]
- Gutstein HB, Akil H. Opioid analgesics. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed. New York: McGraw-Hill; 2006. pp. 547–590. [Google Scholar]
- Halpern JH. The use of hallucinogens in the treatment of addiction. Addiction Research. 1996;4:177–189. [Google Scholar]
- Halpern JH, Pope HG. Do hallucinogens cause residual neuropsychological toxicity? Drug Alcohol Depend. 1999;53:247–256. doi: 10.1016/s0376-8716(98)00129-x. [DOI] [PubMed] [Google Scholar]
- Halpern JH, Pope HG. Hallucinogen persisting perception disorder: what do we know after 50 years? Drug Alcohol Depend. 2003;69:109–119. doi: 10.1016/s0376-8716(02)00306-x. [DOI] [PubMed] [Google Scholar]
- Halpern JH, Sherwood AR, Hudson JI, Yurgelun-Todd D, Pope HG. Psychological and cognitive effects of long-term peyote use among Native Americans. Biol Psychiatry. 2005;58:624–631. doi: 10.1016/j.biopsych.2005.06.038. [DOI] [PubMed] [Google Scholar]
- Harner MJ. The sound of rushing water. Natural History Magazine. 1968;77:28–33. 60–61. [Google Scholar]
- Harner MJ. Jivaro Souls. American Anthropologist. 1962;64:258–272. [Google Scholar]
- Harvard Mental Health Letter. Reviving the study of hallucinogens. Harv Ment Health Lett. 2006;23:5. (editorial) [PubMed] [Google Scholar]
- Hasler F, Bourquin D, Brenneisen R, Bär T, Vollenweider FX. Determination of psilocin and 4-hydroxyindole-3-acetic acid in plasma by HPLC-ECD and pharmacokinetic profiles of oral and intravenous psilocybin in man. Pharm Acta Helv. 1997;72:175–184. doi: 10.1016/s0031-6865(97)00014-9. [DOI] [PubMed] [Google Scholar]
- Hasler F, Bourquin D, Brenneisen R, Vollenweider FX. Renal excretion profiles of psilocin following oral administration of psilocybin: a controlled study in man. J Pharm Biomed Anal. 2002;30:331–339. doi: 10.1016/s0731-7085(02)00278-9. [DOI] [PubMed] [Google Scholar]
- Hasler F, Grimberg U, Benz MA, Huber T, Vollenweider FX. Acute psychological and physiological effects of psilocybin in healthy humans: a double-blind, placebo-controlled dose-effect study. Psychopharmacology. 2004;172:145–156. doi: 10.1007/s00213-003-1640-6. [DOI] [PubMed] [Google Scholar]
- Hidalgo WT. Estudio comparativo psicofisiologico de la mescalina, dietilamida del acido D-lisérgico y psilocybina. Acta Med Venez. 1960;8:56–62. [Google Scholar]
- Hoch PH, Pennes HH, Cattell JP. Psychoses produced by administration of drugs. Res Publ Assoc Res Nerv Ment Dis. 1953;32:287–296. [PubMed] [Google Scholar]
- Hoffer A, Callbeck MJ. Drug-induced schizophrenia. J Ment Sci. 1960;106:138–159. doi: 10.1192/bjp.106.442.138. [DOI] [PubMed] [Google Scholar]
- Hollister LE. Clinical, biochemical and psychologic effects of psilocybin. Arch Int Pharmacodyn Ther. 1961;130:42–52. [PubMed] [Google Scholar]
- Hollister LE, Hartman AM. Mescaline, lysergic acid diethylamide and psilocybin: comparison of clinical syndromes, effects on color perception and biochemical measures. Comprehens Psychiat. 1962;3:235–241. doi: 10.1016/s0010-440x(62)80024-8. [DOI] [PubMed] [Google Scholar]
- Hollister LE. Clinical, biochemical and psychologic effects of psilocybin. Archives Internationales de Pharmacodynamie et de Therapie. 1961;130:42–52. [PubMed] [Google Scholar]
- Hollister LE, Shelton J, Krieger G. A controlled comparison of lysergic acid diethylamide (LSD) and dextroamphetamine in alcoholics. Am J Psychiatry. 1969;125:1352–1357. doi: 10.1176/ajp.125.10.1352. [DOI] [PubMed] [Google Scholar]
- Irwin S, Egozcue J. Chromosomal abnormalities in leukocytes from LSD-25 user. Science. 1967;157:313–314. doi: 10.1126/science.157.3786.313. [DOI] [PubMed] [Google Scholar]
- Isbell H. Comparison of the reactions induced by psilocybin and LSD-25 in man. Psychopharmacologia. 1959;1:29–38. doi: 10.1007/BF00408109. [DOI] [PubMed] [Google Scholar]
- Kast E. Attenuation of anticipation: a therapeutic use of lysergic acid diethylamide. Psychiatr Q. 1967;41:646–657. doi: 10.1007/BF01575629. [DOI] [PubMed] [Google Scholar]
- Kast EC, Collins VJ. Lysergic acid diethylamide as an analgesic agent. Anesth Analg. 1964;43:285–291. [PubMed] [Google Scholar]
- Kuramochi H, Takahashi R. Psychopathology of LSD intoxication; Study of experimental psychosis induced by LSD-25: description of LSD symptoms in normal oriental subjects. Arch Gen Psychiatry. 1964;11:151–161. doi: 10.1001/archpsyc.1964.01720260045006. [DOI] [PubMed] [Google Scholar]
- Keeler MH, Reifler CB. Suicide during an LSD reaction. Am J Psychiatry. 1967;123:884–885. doi: 10.1176/ajp.123.7.884. [DOI] [PubMed] [Google Scholar]
- Kurland AA. LSD in the supportive care of the terminally ill cancer patient. J Psychoactive Drugs. 1985;17:279–290. doi: 10.1080/02791072.1985.10524332. [DOI] [PubMed] [Google Scholar]
- Kurland AA, Pahnke WN, Unger S, Savage C, Goodman E. Psychedelic psychotherapy (LSD) in the treatment of the patient with a malignancy. In: Cerletti A, Bove FJ, editors. The Present Status of Psychotropic Drugs: Pharmacological and Clinical Aspects. Amsterdam, Holland: Excerpta Medica; 1969. pp. 432–434. [Google Scholar]
- Kurland AA, Grof S, Pahnke WN, Goodman LE. Psychedelic drug assisted psychotherapy. In: Goldberg IK, Malitz S, Kutscher AH, editors. Patients With Terminal Cancer Psychotheramacological Agents for the Terminally Ill and Bereaved. New York: Columbia University Press; 1973. pp. 86–133. [Google Scholar]
- Kurland A, Savage C, Pahnke WN, Grof S, Olsson JE. LSD in the treatment of alcoholics. Pharmakopsychiatr Neuropsychopharmakol. 1971;4:83–94. [Google Scholar]
- Lancet. Lancet. Vol. 367. 2006. Reviving research into psychedelic drugs; p. 1214. (editorial) [DOI] [PubMed] [Google Scholar]
- Leary T. The religious experience: Its production and interpretation. Psychedelic Rev. 1964;1:324–346. [Google Scholar]
- Leary T, Litwin GH, Metzner R. Reactions to psilocybin administered in a supportive environment. J Nerv Ment Dis. 1963;137:561–573. doi: 10.1097/00005053-196312000-00007. [DOI] [PubMed] [Google Scholar]
- Leary T, Metzner R, Alpert R. The Psychedelic Experience: A Manual Based on the Tibetan Book of the Dead. New York: Citadel Press; 1964. [Google Scholar]
- Lee MA, Shlain B. Acid dreams: The Complete Social History of LSD: The CIA, the Sixties, and Beyond, Revised Edition. New York: Grove Press; 1992. [Google Scholar]
- Leuner H. Die Experimentelle Psychose. Berlin: Springer; 1962. [Google Scholar]
- Lerner AG, Gelkopf M, Skladman I, Oyffe I, Finkel B, Sigal M, Weizman A. Flashback and hallucinogen persisting perception disorder: clinical aspects and pharmacological treatment approach. Isr J Psychiatry Relat Sci. 2002;39:92–99. [PubMed] [Google Scholar]
- Long SY. Does LSD induce chromosomal damage and malformations? a review of the literature. Teratology. 1972;6:75–90. doi: 10.1002/tera.1420060110. [DOI] [PubMed] [Google Scholar]
- Lowy B. New records of mushroom stones from Guatemala. Mycologia. 1971;63:983–993. [PubMed] [Google Scholar]
- Ludwig A, Levine J, Stark L, Lazar R. A clinical study of LSD treatment in alcoholism. Am J Psychiatry. 1969;126:59–69. doi: 10.1176/ajp.126.1.59. [DOI] [PubMed] [Google Scholar]
- Malitz S, Esecover H, Wilkens B, Hoch H. Some observations on psilocybin: a new hallucinogen in volunteer subjects. Compr Psychiatry. 1960;1:8–17. doi: 10.1016/s0010-440x(60)80045-4. [DOI] [PubMed] [Google Scholar]
- Mangini M. Treatment of alcoholism using psychedelic drugs: a review of the program of research. J Psychoactive Drugs. 1998;30:381–418. doi: 10.1080/02791072.1998.10399714. [DOI] [PubMed] [Google Scholar]
- Masters REL, Houston J. The Varieties of Psychedelic Experience. New York: Holt, Rinehart, & Winston; 1966. [Google Scholar]
- McCabe OL. Psychedelic drug crises: toxicity and therapeutics. Journal of Psychedelic Drugs. 1977;9:107–121. [Google Scholar]
- McGlothlin WH, Arnold DO. LSD revisited A ten-year follow-up of medical LSD use. Arch Gen Psychiatry. 1971;24:35–49. doi: 10.1001/archpsyc.1971.01750070037005. [DOI] [PubMed] [Google Scholar]
- Metzner R. Forward. In: Adamson S, editor. Through the Gateway of the Heart: Accounts of Experiences with MDMA and other Empathogenic Substances. San Francisco: Four Trees Press; 1985. [Google Scholar]
- Metzner R. Introduction: visionary mushrooms of the Americas. In: Metzner R, Darling DC, editors. Teonanácatl: Sacred Mushroom of Visions. El Verano, CA: Four Trees Press; 2004. pp. 1–48. [Google Scholar]
- Metzner R, Litwin G, Weil G. The relation of expectation and mood to psilocybin reactions: a questionnaire study. Psychedelic Review. 1965;5:3–39. [Google Scholar]
- Middlefell R. The effects of LSD on body sway suggestibility in a group of hospital patients. Br J Psychiatry. 1967;113:277–280. doi: 10.1192/bjp.113.496.277. [DOI] [PubMed] [Google Scholar]
- Mogar RE, Aldrich RW. The use of psychedelic agents with autistic schizophrenic children. Psychedelic Review. 1969;10:5–13. [PubMed] [Google Scholar]
- Moreno FA, Wiegand CB, Taitano EK, Delgado PL. Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J Clin Psychiatry. 2006;67:1735–1740. doi: 10.4088/jcp.v67n1110. [DOI] [PubMed] [Google Scholar]
- Morris K. Hallucinogen research inspires “neurotheology”. Lancet Neurol. 2006;5:732. [Google Scholar]
- Moss EL, Dobson KS. Psychology, spirituality, and end-of-life care: an ethical integration? Canadian Psychology. 2006;47:284–299. [Google Scholar]
- National Institute on Drug Abuse. National Institute on Drug Abuse, Research Report Series. 2001. Hallucinogens and dissociative drugs. NIH Publication No 01-4209. [Google Scholar]
- National Institute on Drug Abuse. LSD, NIDA Infofacts. Rockville, MD: National Institute on Drug Abuse; 2006. [Google Scholar]
- Nichols DE. Hallucinogens. Pharmacol Ther. 2004;101:131–181. doi: 10.1016/j.pharmthera.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Nichols DE, Hoffman AJ, Oberlender RA, Jacob P, 3rd, Shulgin AT. Derivatives of 1-(1,3-benzodioxol-5-yl)-2-butanamine: representatives of a novel therapeutic class. J Med Chem. 1986;29:2009–2015. doi: 10.1021/jm00160a035. [DOI] [PubMed] [Google Scholar]
- Novak SJ. LSD before Leary: Sidney Cohen's critique of 1950s psychedelic drug research. Isis. 1997;88:87–110. doi: 10.1086/383628. [DOI] [PubMed] [Google Scholar]
- Ott J. Pharmacotheon: Entheogenic Drugs, their Plant Sources and History. Kennewick, WA: Natural Products Co; 1996. [Google Scholar]
- O’Brien CP. Drug addiction and drug abuse. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed. New York: McGraw-Hill; 2006. pp. 607–627. [Google Scholar]
- Pahnke W. Thesis presented to the President and Fellows of Harvard University for the PhD in Religion and Society. 1963. Drugs and mysticism: An analysis of the relationship between psychedelic drugs and the mystical consciousness. [Google Scholar]
- Pahnke WN. Psychedelic drugs and mystical experience. Int Psychiatry Clin. 1969;5:149–162. [PubMed] [Google Scholar]
- Pahnke WN, Kurland AA, Goodman LE, Richards WA. LSD-assisted psychotherapy with terminal cancer patients. In: Hicks RE, Fink PJ, editors. Psychedelic Drugs: Proceedings of a Hahnemann Medical College and Hospital Symposium. New York: Grune & Stratton; 1969. pp. 33–42. [Google Scholar]
- Passie T, Seifert J, Schneider U, Emrich HM. The pharmacology of psilocybin. Addict Biol. 2002;7:357–364. doi: 10.1080/1355621021000005937. [DOI] [PubMed] [Google Scholar]
- Patel JK, Pinals DA, Breier A. Schizophrenia and other psychoses. In: Tasman A, Kay J, Lieberman JA, editors. Psychiatry. Second Edition. Volume 2. New Jersey: John Wiley & Sons, Ltd; 2003. pp. 1131–1206. [Google Scholar]
- Poling A, Bryceland J. Voluntary drug self-administration by nonhumans: a review. J Psychedelic Drugs. 1979;11:185–190. doi: 10.1080/02791072.1979.10472103. [DOI] [PubMed] [Google Scholar]
- Reitman J, Vasilakis A. The lost freshman. Rolling Stone Magazine. 2004;944:62–66. [Google Scholar]
- Reynolds PC, Jindrich EJ. A mescaline associated fatality. J Anal Toxicol. 1985;9:183–184. doi: 10.1093/jat/9.4.183. [DOI] [PubMed] [Google Scholar]
- Rhead JC. The use of psychedelic drugs in the treatment of severely disturbed children: a review. J Psychedelic Drugs. 1977;9:93–101. [Google Scholar]
- Riba J, Rodriguez-Fornells A, Urbano G, Morte A, Antonijoan R, Montero M, Callaway JC, Barbanoj MJ. Subjective effects and tolerability of the South American psychoactive beverage Ayahuasca in healthy volunteers. Psychopharmacology. 2001;154:85–95. doi: 10.1007/s002130000606. [DOI] [PubMed] [Google Scholar]
- Richards WA. Psychedelic Drug-assisted psychotherapy with persons suffering from terminal cancer. Journal of Altered States of Consciousness. 1980;5:309–319. [Google Scholar]
- Richards WA. Entheogens in the study of mystical and archetypal experiences: Research in the Social Scientific Study of Religion. Brill. 2003;13:143–155. [Google Scholar]
- Richards WA. Entheogens in the study of religious experiences: current status. J Religion Health. 2005;44:377–389. [Google Scholar]
- Richards WA, Grof S, Goodman LE, Kurland AA. LSD-Assisted psychotherapy and the human encounter with death. Journal of Transpersonal Psychology. 1972;4:121–150. [Google Scholar]
- Richards WA, Rhead JC, DiLeo FB, Yensen R, Kurland AA. The peak experience variable in DPT-assisted psychotherapy with cancer patients. J Psychedelic Drugs. 1977;9:1–10. [Google Scholar]
- Richards WA, Rhead JC, Grof S, Goodman LE, Di Leo F, Rush L. DPT as an adjunct in brief psychotherapy with cancer patients. Omega. 1979;10:9–26. [Google Scholar]
- Rinkel M, Atwell CR, DiMascio A, Brown J. Experimental Psychiatry V Psilocybine: A New Psychotogenic Drug. N Engl J Med. 1960;262:295–299. doi: 10.1056/NEJM196002112620606. [DOI] [PubMed] [Google Scholar]
- Roberts TB, Jesse RN. Recollections of the Good Friday Experiment: an interview with Huston Smith. Journal of Transpersonal Psychology. 1997;29:99–104. [Google Scholar]
- Ruck CA, Bigwood J, Staples D, Ott J, Wasson RG. Entheogens. J Psychedelic Drugs. 1979;11:145–146. doi: 10.1080/02791072.1979.10472098. [DOI] [PubMed] [Google Scholar]
- Rümmele W, Gnirss F. Untersuchungen mit Psilocybin, ein psychotropen Substanz aus Psilocybe Mexicana, Schweizerische, Archive für Neurologie. Neurochirurgie und Psychiatrie. 1961;87:365–385. [PubMed] [Google Scholar]
- Savage C, McCabe OL. Residential psychedelic (LSD) therapy for the narcotic addict: a controlled study. Arch Gen Psychiatry. 1973;28:808–814. doi: 10.1001/archpsyc.1973.01750360040005. [DOI] [PubMed] [Google Scholar]
- Schultes RE. Hallucinogens of plant origin. Science. 1969;163:245–254. doi: 10.1126/science.163.3864.245. [DOI] [PubMed] [Google Scholar]
- Schultes RE, Hoffman A, Rätsch C. Plants of the Gods: Their Sacred, Healing, and Hallucinogenic Powers. Revised Edition. Rochester, VT: Healing Arts Press; 2001. [Google Scholar]
- Sessa B. Can psychedelics have a role in psychiatry once again? Br J Psychiatry. 2005;186:457–458. doi: 10.1192/bjp.186.6.457. [DOI] [PubMed] [Google Scholar]
- Shulgin AT, Shulgin A. Pihkal: A Chemical Love Story. Berkeley, CA: Transform Press; 1991. [Google Scholar]
- Shulgin AT, Shulgin A. Tihkal: The Continuation. Berkeley, CA: Transform Press; 1997. [Google Scholar]
- Sjoberg BM, Jr, Hollister LE. The effects of psychotomimetic drugs on primary suggestibility. Psychopharmacologia. 1965;8:251–262. doi: 10.1007/BF00407857. [DOI] [PubMed] [Google Scholar]
- Smart RG, Storm T, Baker EFW, Solursh L. A controlled study of lysergid in the treatment of alcoholism: The effects on drinking behavior. Quart J Stud Alcohol. 1966;27:469–485. [PubMed] [Google Scholar]
- Smith H. Cleansing the Doors of Perceptions: The Religious Significance of Entheogenic Plants and Chemicals. New York: Penguin Putnam Inc; 2000. [Google Scholar]
- Snyder SH. Psychotogenic drugs as models for schizophrenia. Neuropsychopharmcology. 1988;1:197–199. doi: 10.1016/0893-133x(88)90016-4. [DOI] [PubMed] [Google Scholar]
- Stockings GT. A clinical study of the mescaline psychosis, with special reference to the mechanism of the genesis of schizophrenia and other psychotic states. J Mental Sciences. 1940;86:29–47. [Google Scholar]
- Stolaroff MJ. The Secret Chief Revealed: Conversations with Leo Zeff, Pioneer in the Underground Psychedelic Therapy Movement. Sarasota, FL: Multidisciplinary Association for Psychedelic Studies (MAPS); 2004. [Google Scholar]
- Stolz J, Marsden C, Middlemiss D. Effect of chronic antidepressant treatment and subsequent withdrawal on [3H]-5-hydroxytryptamine and [3H]-spiperone binding in rat frontal cortex and serotonin receptor mediated behaviour. Psychopharmacology. 1983;80:150–155. doi: 10.1007/BF00427959. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. Adverse reactions to psychedelic drugs: a review of the literature. The Journal of Nervous and Mental Disease. 1984;172:577–595. doi: 10.1097/00005053-198410000-00001. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. Human hallucinogenic drug research in the United States: a present-day case history and review of the process. J Psychoactive Drugs. 1991;23:29–38. doi: 10.1080/02791072.1991.10472572. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. Human hallucinogen interactions with drugs affecting serotonergic neurotransmission. Neuropsychopharmacology. 1992;7:241–243. [PubMed] [Google Scholar]
- Strassman RJ. Human psychopharmacology of N,N-dimethyltryptamine. Behav Brain Res. 1996;73:121–124. doi: 10.1016/0166-4328(96)00081-2. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. DMT: The Spirit Molecule. Rochester, VT: Park Street Press; 2001. [Google Scholar]
- Strassman RJ, Qualls CR. Dose-response study of N,N-dimethyltryptamine in humans: neuroendocrine, autonomic, and cardiovascular effects. Arch Gen Psychiatry. 1994;51:85–97. doi: 10.1001/archpsyc.1994.03950020009001. [DOI] [PubMed] [Google Scholar]
- Strassman RJ, Qualls CR, Berg LM. Differential tolerance to biological and subjective effects of four closely spaced doses of N,N-dimethyltryptamine in humans. Biol Psychiatry. 1996;39:784–795. doi: 10.1016/0006-3223(95)00200-6. [DOI] [PubMed] [Google Scholar]
- Strassman RJ, Qualls CR, Uhlenhuth EH, Kellner R. Dose-response study of N,N-dimethyltryptamine in humans II: subjective effects and preliminary results of a new rating scale. Arch Gen Psychiatry. 1994;51:98–108. doi: 10.1001/archpsyc.1994.03950020022002. [DOI] [PubMed] [Google Scholar]
- Umbricht D, Vollenweider FX, Schmid L, Grubel C, Skrabo A, Huber T, Koller R. Effects of the 5-HT2A agonist psilocybin on mismatch negativity generation and AX-continuous performance task: implications for the neuropharmacology of cognitive deficits in schizophrenia. Neuropsychopharmacology. 2003;28:170–181. doi: 10.1038/sj.npp.1300005. [DOI] [PubMed] [Google Scholar]
- Ungerleider JT, Frank IM. Management of acute panic reactions and drug flashbacks resulting from LSD ingestion. In: Bourne P, editor. Acute Drug Emergencies. New York: Academic Press; 1976. pp. 133–138. [Google Scholar]
- Tjio JH, Pahnke WN, Kurland AA. LSD and chromosomes, A controlled experiment. JAMA. 1969;210:849–856. [PubMed] [Google Scholar]
- Vollenweider FX, Csomor PA, Knappe B, Geyer MA, Quednow BB. The effects of preferential 5-HT2A agonist psilocybin on prepulse inhibition of startle in healthy human volunteers depend on interstimulus interval. Neuropsychopharmacology. 2007 Feb 14; doi: 10.1038/sj.npp.1301324. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Geyer MA. A systems model of altered consciousness: integrating natural and drug-induced psychoses. Brain Res Bull. 2001;56:495–507. doi: 10.1016/s0361-9230(01)00646-3. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Leenders KL, Scharfetter C, Maguire P, Stadelmann O, Angst J. Positron emission tomography and fluorodeoxyglucose studies of metabolic hyperfrontality and psychopathology in the psilocybin model of psychosis. Neuropsychopharmacology. 1997;16:357–372. doi: 10.1016/S0893-133X(96)00246-1. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Vollenweider-Scherpenhuyzen MFI, Bäbler A, Vogel H, Hell D. Psilocybin induces schizophrenia-like psychosis in humans via serotonin-2 agonist action. Neuroreport. 1998;8:3897–3902. doi: 10.1097/00001756-199812010-00024. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Vontobel P, Hell D, Leenders KL. 5-HT modulation of dopamine release in basal ganglia in psilocybin-induced psychosis in man – a PET study with [11C]raclopride. Neuropsychopharmacology. 1999;20:424–433. doi: 10.1016/S0893-133X(98)00108-0. [DOI] [PubMed] [Google Scholar]
- Weil A. The Natural Mind: A Revolutionary Approach to the Drug Problem. Revised Edition. Boston, MA: Houghton Mifflin Co; 2004. [Google Scholar]
- Winkelman MJ, Roberts TB, editors. Psychedelic Medicine: New Evidence for Hallucinogenic Substances as Treatments. Westport, CT: Praeger; 2007. [Google Scholar]
- Wittmann M, Carter O, Hasler F, Cahn BR, Grimberg U, Spring P, Hell D, Flohr H, Vollenweider FX. Effects of psilocybin on time perception and temporal control of behaviour in humans. J Psychopharmacol. 2007;21:50–64. doi: 10.1177/0269881106065859. [DOI] [PubMed] [Google Scholar]
- Wolbach AB, Isbell H, Miner EJ. Cross tolerance between mescaline and LSD-25 with a comparison of the mescaline and LSD reactions. Psychopharmacologia. 1962;3:1–14. doi: 10.1007/BF00413101. [DOI] [PubMed] [Google Scholar]
- Wolbach AB, Miner EJ, Isbell H. Comparison of psilocin with psilocybin, mescaline and LSD-25. Psychopharmacologia. 1962;3:219–223. doi: 10.1007/BF00412109. [DOI] [PubMed] [Google Scholar]