Abstract
Three subtypes of attention-deficit/hyperactivity disorder (ADHD) based on numbers of symptoms of inattention (I) and hyperactivity-impulsivity (HI) were defined in DSM-IV to reduce heterogeneity of the disorder, but the subtypes proved to be highly unstable over time. A continuous alternative to nominal subtyping is evaluated in a longitudinal study of 129 4–6 year old children with ADHD and 130 comparison children. Children who met criteria for all subtypes in year 1 continued to exhibit greater functional impairment than comparison children during years 2–9. Among children with ADHD in year 1, I and HI symptoms differentially predicted teacher-rated need for treatment and reading and mathematics achievement scores over the next 8 years in controlled analyses. Consistent with other studies, these findings suggest that the use of diagnostic modifiers specifying the numbers of I and HI symptoms could reduce heterogeneity and facilitate clinical intervention, prognosis, and research.
Attention-deficit/hyperactivity disorder (ADHD) is widely viewed as a heterogeneous disorder (Nigg, 2005; Sonuga-Barke, Sergeant, Nigg, & Willcutt, 2008). For this reason, three subtypes of ADHD were defined in DSM-IV in an attempt to distinguish more homogenous subgroups of persons with ADHD. The goal of subtyping any mental disorder is to facilitate both clinical practice and research on the origins, nature, prognosis, and treatment of the heterogeneous disorder. The subtyping of ADHD in DSM-IV was based on evidence showing that there are two dimensions of ADHD symptoms that follow different developmental courses, are associated with different forms of functional impairment, and are associated with different concurrent and future mental disorders (Lahey & Willcutt, 2002).
Hyperactivity-impulsivity (HI) symptoms decline substantially from early childhood through at least adolescence and are associated with active peer rejection, unintentional injuries, disrupted relationships with parents and teachers, and conduct problems in the population. In contrast, inattention (I) symptoms decline less over increasing age and are associated with academic deficits, lack of peer popularity, and depression in the population (Lahey et al., 1994; Lahey et al., 2004; Lahey & Willcutt, 2002; Lee & Hinshaw, 2006; Wahlstedt, Thorell, & Bohlin, 2009). Therefore, three nominal subtypes of ADHD were defined based on exhibiting high levels of I symptoms only (predominantly inattentive type or ADHD-I), high levels of HI symptoms only (predominantly hyperactive-impulsive type or ADHD-HI), or high levels of both dimensions of symptoms (combined type or ADHD-C) (Lahey et al., 1994).
Given that the goal of subtyping diagnoses is to identify subgroups of persons with different characteristics, it is usually assumed that persons will not shift from one subtype to another over time. This is not a logical necessity for a subtyping scheme, but if persons change frequently from one mutually-exclusive subtype to another over relatively short periods of time, such instability would usually obviate the advantages of the subtypes. We previously reported that the DSM-IV subtypes of ADHD were far less stable than the overall diagnosis of ADHD over the first 8 years of the present longitudinal study of children who were first given the diagnosis of ADHD at 4–6 years of age, controlling for treatment, which was not associated with instability (Lahey, Pelham, Loney, Lee, & Willcutt, 2005). Some of this instability was predictable (i.e., shifting from ADHD-HI to ADHD-C from preschool to elementary school as attention deficits were revealed by the increasing demands of school, and shifting from ADHD-C to ADHD-I as hyperactive-impulsive symptoms decline in later childhood and adolescence. Much of the observed instability was unpredictable, however, likely reflecting measurement error, changes in teachers from year to year or other situational changes, and variable improvement or worsening in symptoms. More recently, two other longitudinal studies of children with ADHD found similar marked instability over 5 years in the DSM-IV subtypes of ADHD in a clinic sample of 11–18 year old girls (Hinshaw, 2006) and a representative sample of twin 7–19 year old girls and boys (Todd et al., 2008), indicating that the instability of subtypes is not limited to young children.
Therefore, although the degree of heterogeneity associated with differences in the two dimensions of symptoms of DSM-IV ADHD is important, nominal subtypes appear be too unstable to be an acceptable way of denoting this heterogeneity. This is because any comprehensive set of subtypes that classifies all persons with the disorder based on numbers of different types of symptoms will necessarily differ from one another by one symptom. Therefore a change of ± 1 symptom over time can change the subtype, which almost guarantees instability.
It is very important, therefore, to consider alternative ways to recognize the heterogeneity of ADHD in DSM-V. The goal of any alternative would be to distinguish relatively stable individual differences among persons given the diagnosis of ADHD. In this paper, we propose and test a continuous alternative to the subtypes of ADHD defined in DSM-IV using data from a 9-year longitudinal study of children who were first given the diagnosis of ADHD at 4–6 years of age and demographically matched non-ADHD comparison children (Lahey et al., 2005). This alternative is designed to retain the advantages of the nominal DSM-IV subtypes, but avoid the problems inherent in them. We propose that after determining if an individual meets overall diagnostic criteria for ADHD, the numbers of I and HI symptoms present at the time of diagnosis be used as continuous diagnostic modifiers. In the present analyses, two hypotheses upon which the continuous alternative to nominal subtyping is based are tested:
Although there is enough variation in the numbers of symptoms from year to year to cause considerable shifting among the nominal subtypes, counts of symptoms of I and HI are nonetheless relatively stable over multiple years (i.e., the rank position of individuals is relatively stable), in spite of variations in absolute numbers of symptoms. That is, counts of each dimension of ADHD symptoms are hypothesized to reflect both trait-like and state-like processes.
Among children who meet criteria for any subtype of ADHD, counts of I and HI each differentially predict future functional impairment. This is of fundamental importance as the pattern of impairment strongly influences the selection of therapeutic interventions. Note that this test sets an appropriately high bar for the continuous alternative to nominal subtypes of ADHD. Although it is clear that I and HI are differentially associated with several forms of domain-specific impairment in the general population (Willcutt et al., 2010), it is not clear that I and HI are differentially associated with functional impairment among children who meet overall criteria for ADHD. This is because the two dimensions of symptoms are highly correlated and potentially collinear (Lahey et al., 2008) and positively skewed (i.e., there are few children who meet criteria for ADHD who have very low numbers of either I or H). This could mean that I and HI symptoms would not, therefore, differentially predict impairment among children with ADHD. If not, a continuous alternative to DSM-IV subtypes of ADHD would not be viable.
To compare the nominal subtypes and continuous modifier approaches, we first determine if the nominal subtypes of ADHD in year 1 differ in predicting future functional impairment over the next 8 years. Second, the alternative approach of using counts of I and HI as continuous modifiers is tested by determining if the future functional impairment of children who meet the overall diagnostic criteria for ADHD in year 1 varies as a function of their varying counts of I and HI symptoms in year 1. Specifically, we predict that global measures of impairment that are sensitive to any form of dysfunction will be predicted by both I and HI symptoms, but more domain-specific forms of impairment will be differentially predicted by I and HI.
METHOD
Subjects
Two cohorts of 4–6 year old children were recruited in consecutive years in Chicago and Pittsburgh. Participants were required to live with their biological mothers and to be enrolled in a structured educational preschool or school. In Chicago, all ADHD probands were recruited from an urban or a suburban child psychiatry clinic. In Pittsburgh, 42% of probands were recruited from an urban child psychiatry clinic, with the rest recruited through advertisements. Probands recruited from clinics or advertisements did not differ significantly on demographic or impairment measures (Lahey et al., 1998). Five participants were excluded because they had received clinical diagnoses of pervasive developmental disorder, mental retardation, or seizure disorder. Parents of participants gave written informed consent and children gave oral assent.
Comparison children were recruited from the same schools or neighborhoods as the probands. None had been referred for services for mental health problems, but were not excluded if they met criteria for a mental disorder other than ADHD in the year 1 assessment. Comparison children were selected from among those who volunteered to match the probands on the basis of sex, ethnicity, and age. Two children who met criteria for ADHD in the wave 1 diagnostic assessment were recruited as controls and 12 children who were recruited as probands did not meet criteria for ADHD. These children were conservatively included in the ADHD and comparison groups, respectively. Of the 315 eligible participants recruited from clinics and advertisements, 259 (82%) agreed to participate. Retention of participants was excellent, with 93.0% of youth being reassessed in either year 8 or 9.
Parents were asked to discontinue medications on the day of the assessment if approved by the child’s physician. Parents and teachers were asked to rate children who took medication as they are when off medication. We tested whether medication or psychosocial treatments in wave (treated as a time-varying covariate) were associated with outcomes in the present sample (Lahey et al., 2005). When treatments were significantly related to outcomes, they were associated with greater persistence of ADHD. We interpret this as indicating that children with more persistent ADHD received more treatment and did not covary treatment in the present analyses.
Measures
ADHD was assessed each year using the same measures, except that the fifth annual assessment was omitted due to a gap in funding. The DSM-IV field trials (Lahey et al., 1994) version of the Diagnostic Interview Schedule for Children (DISC) (Shaffer, Fisher, Piacentini, Schwab-Stone, & Wicks, 1993) was administered to the mother in each assessment to query DSM-IV diagnostic criteria for ADHD and other mental disorders during the last 6 months. Information on symptoms of the disruptive behavior disorders also was obtained from teachers by mail using the DSM-IV version of the DBD Rating Scale (Pelham, Gnagy, Greenslade, & Milich, 1992).
Child intelligence was estimated using the Stanford-Binet Intelligence Scale Short Form (Thorndike, Hagen, & Sattler, 1986) by averaging scores from administrations in years 1 and 2. The range of mean intelligence scores was 64–143. The Letter-Word and Applied Problems scales from the Woodcock-Johnson Psychoeducational Battery (Woodcock, 1977) were administered each year to operationalize reading and mathematics achievement. Differences among the subtypes of these measures in the present sample across years 1–8 have previously been reported (Massetti et al., 2008). Each year, the parent was asked if the child had suffered an injury more serious than a scratch, bruise, or bump on the head that the parent attributed to the child’s carelessness, impulsiveness, or poor judgment. In addition, the child’s primary or English teacher estimated the proportion of the child’s classmates who like, dislike, and ignore the child on three separate 5-point scales each year (Dishion, 1990).
Diagnosis of ADHD
Based on evidence that both parents and teacher contribute to the validity of the diagnosis of ADHD (Bird, Gould, & Staghezza, 1992; Hart, Lahey, Loeber, & Hanson, 1994; Jensen et al., 1999), the diagnosis of ADHD in year 1 was based on a combination of parent reports of DSM-IV symptoms in DISC interviews and teacher reports on the DBD. We used the standard method (Pelham et al., 1992), of considering teacher ratings of the DBD of “pretty much” or “very much” as indicating that the symptom was present by teacher reports was used. As in the DSM-IV field trials (Lahey et al., 1994), each ADHD symptom was considered to be present if each symptom was reported by either teacher or parent using the simple ‘or’ rule (Piacentini, Cohen, & Cohen, 1992).
Due to their age in year 1, all children met the age of onset criterion for ADHD. Impairment was assessed in two ways for the diagnosis of ADHD. First, the parent was asked in the DISC if the child’s ADHD symptoms had caused problems (a) at home or with friends, or (b) at school. Second, parents and teachers completed the Impairment Rating Scale (IRS) (Fabiano et al., 2006), in which the child’s need for treatment in multiple areas was rated using 7-point scales ranging from “No problem; definitely does not need treatment” (=0) to “Extreme problem; definitely needs treatment” (=6). Parents rated the child on problems in relations with peers, siblings, and parents, academic progress at school, self-esteem, and impact on the family. Teachers rated problems in relations with classmates and teachers, academic progress, classroom disruption, and self-esteem using the IRS. Both respondents rated the child’s overall need for treatment. For the year 1 diagnosis of ADHD, based on previous studies, children were said to be impaired if they received a rating of ≥3 on at least one IRS scale (Fabiano et al., 2006).
Children were said to exhibit ADHD in year 1 if they met DSM-IV symptom criteria and exhibited impairment in at least one setting. We relaxed the DSM-IV requirement of impairment in two settings for 7 of 129 children because of previous findings from this sample that nearly all of these children met criteria for ADHD with impairment in two settings in later years (Lahey et al., 2005) and because of concerns that children with serious impairment in only setting should not be excluded from the diagnosis. Children were assigned to subtypes of ADHD using strict DSM-IV criteria. A total of 129 children who met symptom criteria for ADHD were reported to be impaired in ≥1 setting in year 1 at 4–6 years and 130 comparison children did not meet criteria for ADHD.
When testing the continuous alternative to the nominal DSM-IV subtypes, counts of I and HI symptoms were similarly based on the number of symptoms that were reported by either the parent in the DISC or the teacher in the DBD.
Data Analysis
Alpha was set at < .05 for all tests. All analyses were performed on unstandardized variables. When the response variables were normally distributed, linear regression was used in longitudinal general estimating equations (GEE). When the response variable was dichotomous, binomial regression was used and when skewed and discontinuous, Poisson regression was conducted in GEE with correction for overdispersion. These analyses used autoregressive correlation structures and robust variance estimates.
All predictive analyses controlled both methodologic covariates (site, cohort, and the blindness of the interviewer to information about the child from previous assessments, and the number of parent and teacher informants in each assessment). In addition, to address impairment specific to ADHD, mothers and teachers reported on concurrent symptoms of conduct disorder (CD) and oppositional defiant disorder (ODD), and mothers reported on internalizing symptoms (anxiety and depression combined) in year 1. Intelligence, and age, sex, race-ethnicity, and logged total family income in year 1 were included as fixed covariates in all tests of predictive validity. Blindness of the interviewer was not controlled when it was not relevant to the response variable (e.g., ratings from teachers with whom the interviewer did not interact). For all measures of impairment, tests were conducted of the subtypes-by-time interaction and reported when significant. The I x HI interaction was never significant at p < .05. Formal tests of differences in the regression coefficients for I and HI symptoms with each measure of impairment were conducted in generalized estimating equations to take the correlation between I and HI into account.
RESULTS
Characteristics of the Sample
As shown in Table 1, the case-control recruitment strategy selected children with ADHD and a non-ADHD comparison group that did not differ significantly in sex, race-ethnicity, or age in year 1. Counts of I and HI symptoms in year 1 were highly correlated in the full sample (Spearman’s ρ = .82, p < .0001). As shown, the three subtypes of ADHD differed in intelligence, family income, and the number of concurrent symptoms of other mental disorders in year 1 (Lahey et al., 1998). Among children with ADHD in year 1, the count of HI symptoms accounted for significant independent variance in ODD symptoms (β = 0.50, z = 18.92, p < .0001) and CD symptoms (β = 0.22, z = 6.00, p < .02) in year 1, but I symptoms did not. In contrast, the count of I symptoms accounted for significant independent variance in anxiety/depression symptoms in year 1 (β = 0.64, z = 11.61, p < .001), but HI symptoms did not.
Table 1.
Comparison of subtype and comparison groups on demographic characteristics and other concurrent symptoms in the initial assessment.
| Not ADHD | ADHD-C | ADHD-HI | ADHD-I | χ2 | d.f. | |
|---|---|---|---|---|---|---|
| N = | 130 | 88 | 27 | 14 | ||
| Age1 (mean, sd) | 5.2 (0.8) | 5.2 (0.7) | 5.1 (0.8) | 5.7 (0.5) | 7.72 | 3 |
| Family Income2 (mean, sd) | 47647 (35034)b | 37580 (34858)a | 46204 (33628)a,b32964 (36237) a,b | 10.07* | 3 | |
| Intelligence (mean, sd) | 103.7 (14.1)c | 90.1 (12.2)a | 96.9 (14.8)b | 92.8 (10.0)a,b | 57.54**** | 3 |
| Sex (% male) | 80.0 | 86.4 | 88. 9 | 64.3 | 5.38 | 3 |
| Race-Ethnic Group (%) | 4.96 | 6 | ||||
| African American | 30.8 | 35.2 | 22.2 | 21.4 | ||
| Non-Hispanic white | 63.8 | 56.8 | 74.1 | 78.6 | ||
| Other groups | 5.4 | 8.0 | 3.7 | 0.0 | ||
| Concurrent Symptoms (mean, sd) | ||||||
| Anxiety+Depression | 1.9 (2.5)a | 5.8 (4.6)c | 3.4 (2.7)b | 5.9 (5.0)c | 71.72**** | 3 |
| ODD | 0.7 (1.4)a | 4.6 (2.5)c | 3.8 (2.7)b,c | 2.7 (2.2)b | 173.77**** | 3 |
| CD | 0.1 (0.5)a | 1.8 (1.9)b | 1.7 (1.8)b | 0.4 (.4)a | 118.23**** | 3 |
In year 1.
The log of family income in year 1 was taken before statistical comparisons were made.
p < .05
p < .0001
Note: Means and Proportions and means with different superscripts differ at p < .05, not controlling concurrent psychopathology in year 1.
Stability of Symptom Dimensions
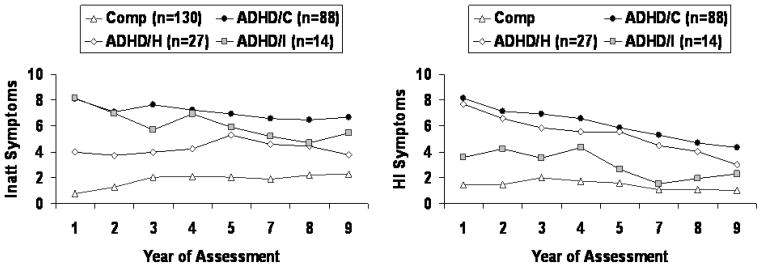
As shown in the left panel of Figure 1, longitudinal Poisson regression revealed that the three groups of children who met criteria for ADHD-C (β = 1.05, z = 11.05, p < .0001), ADHD-I (β = 1.14, z = 8.73, p < .0001), and ADHD-HI (β = 0.73, z = 5.91, p < .0001) each exhibited more I symptoms across years 2–9 than children in the comparison group. Consistent with the definitions of the nominal subtypes, the ADHD-HI group exhibited fewer I symptoms over years 2–9 than the ADHD-C group (β = −0.42, z = −4.74, p < .0001) and the ADHD-I group (β = −0.41, z = −3.26, p < .0001), but there was not a significant difference between ADHD-C and ADHD-I on the number of I symptoms (p = .98). Two subtype-by-time (i.e., repeated assessments over years 2–9) interactions were significant, indicating that the magnitude of the differences in numbers of I symptoms between the comparison group and both ADHD-C (β = −0.07, z = −3.36, p < .001) and ADHD-I (β = −0.09, z = −2.81, p < .005) became smaller over time, but the ADHD-HI-by-time interaction was not significant.
Figure 1.
Numbers of symptoms of inattention (left) and hyperactivity-impulsivity (right) reported by parents and teachers combined during the course of the study among children in the non-ADHD comparison group and children who met criteria for the combined (ADHD-C), predominantly hyperactive-impulsive (ADHD-HI), or predominantly inattentive (ADHD-I) subtype of attention-deficit/hyperactivity disorder in the year 1 assessment.
The groups of children who met criteria for ADHD-C (β = 1.40, z = 13.86, p < .0001), ADHD-I (β = 0.89, z = 5.20, p < .0001), and ADHD-HI (β = 1.30, z = 11.10, p < .0001) each exhibited more HI symptoms during the next 8 years than children in the comparison group. As expected, children in the ADHD-I group exhibited fewer HI symptoms than in the ADHD-C group (β = −0.50, z = −3.24, p < .005) and the ADHD-HI group (β = −0.40, z = −2.39, p < .02). When the subtypes-by-time interactions were tested, there were no significant changes in the magnitudes of differences between any subtype and the comparison group or among the three subtypes over 8 years.
Stability of the Diagnosis of ADHD among the Three Subtypes
The percentage of children who met criteria for any subtype of ADHD in either year 8 or year 9 was: comparison = 27.5%, ADHD-C = 81.7%, ADHD-HI = 53.8%, and ADHD-I = 53.8%. This degree of stability of the overall diagnosis of ADHD is consistent with the results of a meta-analysis of the stability of ADHD over increasing age (Faraone, Biederman, & Mick, 2006). Using logistic regression, the groups of children who met criteria for ADHD-C (β = 2.49, χ2 = 33.54, p < .0001; O.R. = 12.11, 95% C.I.: 5.20–28.17), ADHD-HI (β = 1.20, χ2 = 5.98, p < .02; O.R. = 3.30, 95% C.I.: 1.27–8.73), and ADHD-I (β = 1.40, χ2 = 4.21, p < .05; O.R. = 4.06, 95% C.I.: 1.06–15.44) were each far more likely to meet criteria for ADHD in either year 8 or 9 than was the comparison group.
Comparison children who met criteria for ADHD in later years did so less consistently (i.e., in both years 8 and 9) than children with ADHD in year 1 (39.4% versus 73.2%, respectively, χ2 = 11.58, d.f. = 1, p < .001). It is important to note, however, that 20 (15.4%) of the 130 comparison children who did not meet criteria for ADHD in year 1 later met criteria for ADHD during three of more of the next eight assessments. For the purposes of the present predictive validity analyses, it is appropriate to conservatively leave these 20 cases of relatively persistent ADHD in the comparison group. Because these 20 children were all impaired in at least one setting when other ADHD criteria were met, however, differences in future impairment between the children with ADHD in year 1 and the comparison group may have been even greater had they been deleted.
Instability of the Nominal Subtypes of ADHD
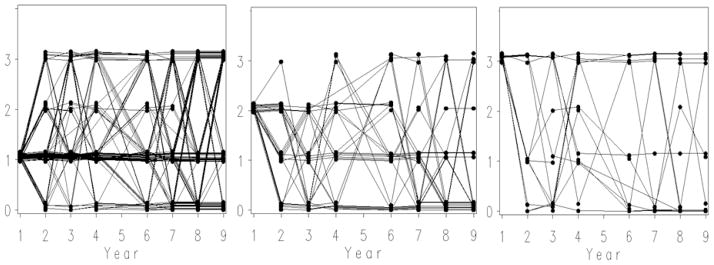
To provide a foundation for understanding the present analyses, Figure 2 reveals the marked instability of the nominal DSM-IV subtypes of ADHD over years 1–9, which was previously reported across years 1–8 (Lahey et al., 2005). Longitudinal binomial regression showed that year-to-year shifting among subtypes was not significantly attributable to just meeting the diagnostic threshold for a subtype by one symptom at p< .05. Over years 1–9, the percent of children who always met criteria for the same subtype in every year in which they were assessed (with assessments in which a child with ADHD in year 1 was not diagnosed as ADHD liberally not counted as a change in subtype) was very low; ADHD-C = 23.8%; ADHD-HI: 11.11%; ADHD-I: 38.5%. Furthermore, at least some children met criteria for both of the other two subtypes over years 1–9. Note in Figure 2 that the instability of the nominal subtypes did not decline with increasing age. For example, when year 3 (ages 6–8 years) was taken as the starting place, the percent of children who always met criteria for the same subtype of ADHD (prorated for the number of subsequent assessments) was essentially the same as when year 1 was the starting point: ADHD-C = 27.6%; ADHD-HI: 23.8%; ADHD-I: 35.7%.
Figure 2.
Plots of jittered data for individual children representing the subtype of ADHD that each child met criteria for in years 2–9 (no assessment in year 5). The three panels present data for children who initially met criteria in year 1 for the combined type (left), the predominantly hyperactive-impulsive type (middle), and the predominantly inattentive type (right). Note: 1 = combined type; 2 = predominantly hyperactive-impulsive type; 3 = predominantly inattentive type; 0 = does not meet criteria for ADHD in that assessment.
Predictive Validity: Associations with Future Functional Impairment
Prospective analyses were conducted to determine if functional impairment over the next 8 years were predicted by either (a) the DSM-IV subtypes of ADHD, or (b) counts of I and HI symptoms in year 1 among only children who met criteria for ADHD with impairment in at least one setting in year 1 (at 4–6 years of age). Four models were conducted for each measure of impairment:
Model 1 provided a test of the DSM-IV model by determining the extent to which the three subtypes of ADHD in 4–6 year old children are differentially associated with future functioning. Model 2 also controlled counts of symptoms of three types of concurrent mental disorders in year 1. Model 3 tested the extent to which variations in numbers of I and HI symptoms among children who met overall DSM-IV criteria for ADHD in year are differentially associated with functional impairment. Model 4 also controlled concurrent psychopathology in year 1.
Predictive Validity: Global Ratings of Impairment
Maternal IRS ratings of need for treatment
Regardless of whether year 1 concurrent symptoms of other forms of psychopathology were not controlled (Model 1) or controlled (Model 2), mothers gave higher ratings indicating greater overall need for treatment on the IRS during years 2–9 to children who met criteria for all three subtypes of ADHD than comparison children (Table 2 and Figure 3). Children with ADHD-C received higher ratings than those with ADHD-HI (β = 0.32, z = 2.52, p < .02), but the ADHD-I group did not differ significantly from either group when concurrent psychopathology in year 1 was not controlled. There were no significant differences among the three subtypes when concurrent psychopathology in year 1 was controlled.
Table 2.
Prediction of future global measures of impairment from DSM-IV subtypes versus the comparison group and (Models 1 and 2) and numbers of symptoms of inattention and hyperactivity-impulsivity (Models 3 and 4) among children with ADHD in year 1.
| Nominal Subtypes as Predictors vs. Comparison | Counts of ADHD Symptoms as Predictors | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||
| Predictors | β | z | β | z | Predictors | β | z | β | z |
| Outcome Variable: Maternal Ratings of the Child’s Overall Need for Treatment (IRS) Across Years 2–9 | |||||||||
| ODDa | 0.08 | 3.39**** | ODDa | 0.06 | 2.78** | ||||
| CDa | 0.01 | 0.49 | CDa | 0.02 | 0.55 | ||||
| Internalizinga | 0.02 | 1.36 | Internalizinga | 0.02 | 1.73 | ||||
| ADHD-I | 1.51 | 6.79**** | 1.29 | 5.92**** | Ia | 0.06 | 2.40* | 0.04 | 1.69 |
| ADHD-HI | 1.52 | 7.90**** | 1.22 | 6.26**** | HIa | 0.072 | 2.46* | 0.04 | 1.33 |
| ADHD-C | 1.81 | 10.88**** | 1.41 | 7.53**** | |||||
| Outcome Variable: Teacher Ratings of the Child’s Overall Need for Treatment (IRS) Across Years 2–9 | |||||||||
| ODDa | 0.06 | 3.28*** | ODDa | 0.03 | 1.53 | ||||
| CDa | 0.02 | 0.88 | CDa | 0.02 | 1.16 | ||||
| Internalizinga | −0.01 | −0.80 | Internalizinga | 0.00 | 0.50 | ||||
| ADHD-I | 0.91 | 6.40**** | 0.83 | 6.10**** | Ia | 0.07 | 3.16** | 0.06 | 2.73** |
| ADHD-HI | 0.66 | 4.52**** | 0.47 | 3.00** | HIa | 0.03 | 2.03* | 0.01 | 0.62 |
| ADHD-C | 0.98 | 9.13**** | 0.74 | 5.88**** | |||||
| Outcome Variable: Interviewer CGAS Ratings Across Years 2–9 | |||||||||
| ODDa | −0.02 | −4.25**** | ODDa | −0.02 | −3.03** | ||||
| CDa | −0.01 | −1.14 | CDa | −0.01 | −1.05 | ||||
| Internalizinga | 0.01 | −4.03**** | Internalizinga | −0.01 | −2.71** | ||||
| ADHD-I | −0.19 | −4.72**** | −0.10 | −3.44**** | Ia | −0.02 | −3.18** | −0.02 | −2.39* |
| ADHD-HI | −0.18 | −5.64**** | −0.09 | −3.03** | HIa | −0.02 | −2.90** | −0.01 | −1.22 |
| ADHD-C | −0.28 | −11.96**** | −0.14 | −5.96**** | |||||
< .05;
< .01;
< .001;
< .0001
Counts of symptoms; beta estimates reflect differences in effect at each greater number of symptoms.
Notes:
Model 1 = subtypes of ADHD and the comparison group are the predictors; methodologic (site and cohort) and demographic (age in year 1, sex, race-ethnic group, total family income, and intelligence) covariates included.
Model 2 = subtypes of ADHD and the comparison group are the predictors; methodologic and demographic covariates include with numbers of symptoms on concurrent mental disorders in year 1 (oppositional defiant disorder, conduct disorder, and internalizing disorders).
Model 3 = numbers of inattention and hyperactivity-impulsivity symptoms are the predictors among children who meet criteria for ADHD with impairment in at least one setting; methodologic and demographic covariates include with numbers of symptoms on concurrent mental disorders in year 1 (oppositional defiant disorder, conduct disorder, and internalizing disorders).
Model 4 = numbers of inattention and hyperactivity-impulsivity symptoms are the predictors among children who meet criteria for ADHD with impairment in at least one setting; methodologic and demographic covariates include with numbers of symptoms on concurrent mental disorders in year 1 (oppositional defiant disorder, conduct disorder, and internalizing disorders).
ODD = number of symptoms of oppositional defiant disorder in year 1; CD = number of symptoms of conduct disorder in year 1; internalizing = total number of symptoms of depression and anxiety disorders in year 1; ADHD-I = predominantly inattentive subtype; ADHD-HI = predominantly hyperactive-impulsive subtype; ADHD-C = combined subtype; HI = hyperactivity-impulsivity; I = inattention; O.R. = odds ratio; C. I. = confidence interval. All statistical tests compare the ADHD subtype groups to the non-ADHD comparison group.
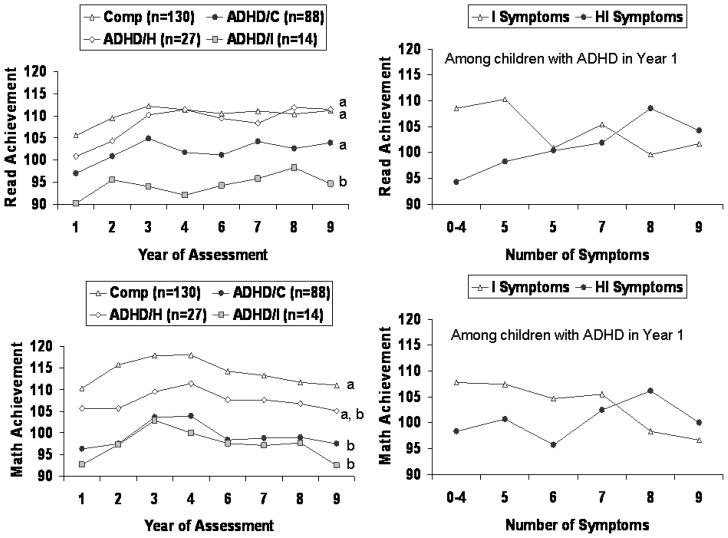
Figure 3.
Unadjusted continuous maternal ratings of need for treatment over years among children who met criteria in year 1 for the combined (ADHD-C), predominantly hyperactive-impulsive (ADHD-HI), or predominantly inattentive (ADHD-I) subtypes of attention-deficit/hyperactivity disorder in the year 1 assessment and for children in the comparison group (upper left). Unadjusted continuous maternal ratings of need for treatment averaged over year 2–9 as a function of the number of inattention and hyperactivity-impulsivity symptoms (upper right) among children who met criteria for any subtype of ADHD in year 1 (upper right). The corresponding data on unadjusted continuous interviewer-completed Children’s Global Assessment Scale (CGAS) scores averaged over year 2–9 in the lower left and right panels, respectively. Means with different superscripts differ at p < .05, not controlling concurrent psychopathology in year 1.
Among children who met criteria for any subtype of ADHD in year 1 (at 4–6 years) counts of both I symptoms and HI symptoms independently predicted maternal ratings of need for treatment across years 2–9 when concurrent psychopathology in year 1 was not controlled (Model 3). Neither I nor HI symptoms were significantly associated with maternal IRS ratings when concurrent psychopathology in year 1 was controlled (Model 3), however.
Teacher IRS ratings of need for treatment
As reported in Table 2, regardless of whether year 1 concurrent symptoms of other forms of psychopathology were or were not controlled, the children’s succession of different teachers over the next 8 years rated children who met criteria for all three subtypes of ADHD as exhibiting greater need for treatment than children in the comparison group. When terms for the interactions between time (assessment years) and each subtype were added to Model 1, there was a significant decline in the difference in rated need for treatment between both ADHD-C (β = −0.06, z = −2.09, p < .05) and ADHD-HI (β = −0.08, z = −2.27, p < .05) and the comparison group over years 2–9. Among children who met criteria for ADHD in year 1, the ADHD-C group was given higher teacher ratings of need for treatment across years 2–9 than the ADHD-HI group when concurrent psychopathology in year 1 was not controlled (β = 0.35, z = 3.01, p < .005) and controlled (β = 0.29, z = 2.61, p < .01), but ADHD-I differed significantly from neither subtype.
Among children with ADHD in year 1, counts of I and HI symptoms each independently predicted teacher ratings of overall need for treatment over years 2–9 when concurrent symptoms of other forms of psychopathology were not controlled. Only counts of I symptoms predicted teacher ratings of overall need for treatment when concurrent psychopathology in year 1 was controlled, however. GEE revealed that the magnitude of association of I symptoms with teacher ratings of need for treatment was significantly greater than for HI symptoms when concurrent psychopathology in year 1 was controlled (β = −0.08, z = −4.44, p < .0001).
Interviewer CGAS ratings
As reported in Table 2 and Figure 3, all three subtypes of ADHD exhibited lower continuous levels of interviewer-rated global functioning on the CGAS than comparison children across years 2–9, even when concurrent psychopathology in year 1 was controlled. Tests of the subtypes-by-time interactions showed that there were declines in the magnitudes of differences between the comparison group and ADHD-C (p < .01), ADHD-HI (p < .05), and ADHD-I (p < .01). The ADHD-C subtype received lower CGAS scores over years 2–9 than the ADHD-HI (β = −0.10, z = −2.54, p < .02) and ADHD-I subtypes (β = −0.10, z = −2.28, p < .05), but ADHD-I and ADHD-HI did not differ significantly when concurrent psychopathology in year 1 was not controlled; there were no significant differences among the three subtypes when concurrent psychopathology was controlled.
Among children with ADHD in year 1, both I symptoms and HI symptoms independently predicted interviewer CGAS ratings across years 2–9 when concurrent psychopathology was not controlled, but only counts of I symptoms significantly predicted interviewer CGAS scores when concurrent psychopathology was controlled. GEE revealed that the difference between the magnitudes of association of I and HI symptoms with interviewer CGAS ratings was not significant, however, when concurrent psychopathology in year 1 was controlled.
Predictive Validity: Domain-Specific Ratings of Impairment
Teacher ratings of peer disliking
As reported in Table 3, teachers rated children who met criteria for ADHD-C and ADHD-HI in year 1 as being disliked by significantly more classmates than comparison children across years 2–9, regardless of whether concurrent psychopathology in year 1 was controlled. The ADHD-C group was rated by teachers as being disliked by more classmates than the ADHD-I group, both when concurrent psychopathology in year 1 was not controlled (β = 0.26, z = 2.37, p < .02) and was controlled (β = 0.22, z = 2.04, p < .05), but ADHD-HI did not differ from either subtype. Among children with ADHD, counts of I symptoms were not significantly related to disliking, but HI symptoms predicted ratings of greater peer disliking by teachers across years 2–9 when concurrent psychopathology in year 1 was not controlled, but not when it was controlled.
Table 3.
Prediction of future domain-specific measures of impairment from DSM-IV subtypes versus the comparison group and (Models 1 and 2) and numbers of symptoms of inattention and hyperactivity-impulsivity (Models 3 and 4) among children with ADHD in year 1.
| Nominal Subtypes as Predictors vs. Comparison | Counts of Symptoms as Predictors | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||
| Predictors | β | z | β | z | Predictors | β | z | β | z |
| Outcome Variable: Teacher Ratings of Peer Disliking across Years 2-9 | |||||||||
| ODDa | 0.03 | 2.48* | ODDa | 0.01 | 0.73 | ||||
| CDa | 0.01 | 0.41 | CDa | 0.01 | 0.58 | ||||
| Internalizinga | −0.00 | −0.14 | Internalizinga | 0.01 | 1.09 | ||||
| ADHD-I | 0.19 | 1.75 | 0.13 | 1.26 | Ia | 0.01 | 0.59 | 0.00 | 0.27 |
| ADHD-HI | 0.35 | 4.50**** | 0.24 | 2.64** | HIa | 0.04 | 2.55* | 0.03 | 1.89 |
| ADHD-C | 0.43 | 8.45**** | 0.30 | 4.15**** | |||||
| Outcome Variable: Teacher Ratings of Peer Ignoring across Years 2–9 | |||||||||
| ODDa | 0.03 | 2.62** | ODDa | 0.02 | 1.46 | ||||
| CDa | −0.02 | −1.42 | CDa | −0.02 | −1.33 | ||||
| Internalizinga | −0.01 | −1.18 | Internalizinga | −0.01 | −1.41 | ||||
| ADHD-I | 0.26 | 3.26** | 0.23 | 2.85** | Ia | 0.03 | 2.45* | 0.03 | 2.41* |
| ADHD-HI | 0.13 | 1.82 | 0.09 | 1.08 | HIa | 0.02 | 1.06 | 0.01 | 0.58 |
| ADHD-C | 0.30 | 6.28*** | 0.24 | 4.22**** | |||||
| Outcome Variable: Reading Achievement Scores across Years 2–9 | |||||||||
| ODDa | 0.23 | 0.48 | ODDa | 0.45 | 0.79 | ||||
| CDa | −0.07 | −0.11 | CDa | 0.04 | 0.06 | ||||
| Internalizinga | −0.45 | −1.47 | Internalizinga | −0.81 | −2.08* | ||||
| ADHD-I | −7.94 | −2.10* | −6.78 | −1.75 | Ia | −0.50 | −0.75 | −0.18 | −0.26 |
| ADHD-HI | 2.71 | 0.92 | 2.61 | 0.78 | HIa | 2.05 | 3.22** | 1.79 | 2.60** |
| ADHD-C | 0.98 | 0.51 | 1.60 | 0.63 | |||||
| Outcome Variable: Mathematics Achievement Scores across Years 2-9 | |||||||||
| ODDa | 0.52 | 1.36 | ODDa | 0.92 | 1.81 | ||||
| CDa | −0.87 | −1.98* | CDa | −0.74 | −1.74 | ||||
| Internalizinga | −0.57 | −2.26* | Internalizinga | −0.89 | −2.73** | ||||
| ADHD-I | −7.00 | −3.02** | −5.66 | −2.44* | Ia | −1.16 | −2.40* | −0.92 | −2.04* |
| ADHD-HI | −1.59 | −0.68 | −1.21 | −0.50 | HIa | .45 | 0.98 | 0.07 | 0.21 |
| ADHD-C | −4.49 | −3.15** | −3.33 | −1.79 | |||||
< .05;
< .01;
< .001;
< .0001
Counts of symptoms; beta estimates and odds ratios reflect differences in effect at each greater number of symptoms.
Note: Reading and mathematics achievement scores tested with generalized linear regression. See notes at the bottom of Table 2.
Teacher ratings of peer ignoring
As reported in Table 3, teachers rated children who met criteria for ADHD-C and ADHD-I as being ignored by more classmates than comparison children across years 2–9, regardless of whether symptoms of other mental disorders in year 1 were controlled. Children in the ADHD-C group were rated by teachers as being more ignored by classmates than children in the ADHD-HI group when concurrent psychopathology in year 1 was not controlled (β = 0.18, z = 2.92, p < .005) and controlled (β = 0.18, z = 2.94, p < .005), but ADHD-I did not differ from either ADHD-C or ADHD-HI in either comparison. Among children with ADHD in year 1, counts of I symptoms predicted ratings of peer ignoring across years 2–9 whether concurrent psychopathology in year was controlled or not. HI symptoms did not significantly predict peer ignoring, but GEE revealed that the difference between regression coefficients for I and HI symptoms was not significant among children with ADHD when concurrent psychopathology in year 1 was controlled.
Reading achievement scores
As shown in Table 3 and Figure 4, controlling for intelligence and the other covariates, reading achievement scores across years 2–9 were lower in children in the ADHD-I group than the comparison group, but the other subtypes did not differ significantly from comparison children. When concurrent psychopathology in year 1 was controlled, none of the subtypes differed significantly from the comparison group on reading. When concurrent psychopathology in year 1 was not controlled, children in the ADHD-I group had lower reading scores over time than children in the ADHD-C (β = −9.14, z = −2.41, p < .02) and the ADHD-HI groups (β = −10.95, z = −2.35, p < .02). When concurrent psychopathology in year 1 was controlled, however, there were no significant differences among the subtypes on reading.
Figure 4.
Unadjusted continuous reading achievement scores over years among children who met criteria in year 1 for the combined (ADHD-C), predominantly hyperactive-impulsive (ADHD-HI), or predominantly inattentive (ADHD-I) subtypes of attention-deficit/hyperactivity disorder in the year 1 assessment and for children in the comparison group (upper left). Unadjusted continuous reading achievement scores averaged over year 2–9 as a function of the number of inattention and hyperactivity-impulsivity symptoms among children who met criteria for any subtype of ADHD in year 1 (upper right). The corresponding data on continuous mathematics achievement scores averaged over year 2–9 are presented in the lower left and right panels, respectively. Means with different superscripts differ at p < .05, not controlling concurrent psychopathology in year 1.
Among children with ADHD in year 1, Table 3 and Figure 4 show that trends for the associations of I and HI symptoms with reading achievement were in opposite directions. Although I symptoms were not significantly associated reading among children with ADHD in year 1, youth with ADHD who exhibited more HI symptoms in year 1 had higher reading scores when intelligence and concurrent psychopathology in year 1 were controlled (β = 1.82, z = 2.63, p < .01). GEE revealed that the positive association with reading scores was significantly stronger for HI than for I among children with ADHD when concurrent psychopathology in year 1 was controlled (β = 0.01, z = 3.39, p < .001).
Mathematics achievement scores
As reported in Table 3 and Figure 4, mathematics scores were significantly lower across years 2–9 in children with both ADHD-C and ADHD-I than in the comparison group (Model 1). When concurrent symptoms of other forms of psychopathology in year 1 were added as covariates, only ADHD-I differed significantly from the comparison group on mathematics (Model 2). There were no significant differences among the three ADHD subtypes, however, on mathematics scores when concurrent psychopathology in year 1 was or was not controlled.
Among children with ADHD in year 1, Table 3 and Figure 4 show that the trends for the associations of I and HI symptoms with mathematics achievement also were in opposite directions. HI symptoms did not significantly predict low mathematics achievement, but children with ADHD who exhibited more I symptoms had lower mathematics achievement scores, whether concurrent psychopathology in year 1 was controlled or not. GEE revealed that the inverse association with mathematics achievement was significantly greater for I than for HI among children with ADHD, with nearly identical differences found when concurrent psychopathology was controlled (β = 0.01, z = 5.12, p < .0001).
Unintentional injuries
Because of the low prevalence of unintentional injuries in each year, predictive logistic regression analyses for reporting at least one injury by year 9 were conducted. As reported in Table 4, parents reported that children who met criteria for ADHD-C (61.4%) and ADHD-HI (55.6%) in year 1 were significantly more likely to have experienced at least one nontrivial unintentional injury during years 2–9 than comparison children (29.2%), which ADHD-I (42.9%) not differing significantly from any other group. ADHD-C exhibited more injuries than the comparison group when concurrent psychopathology in year 1 was controlled (Model 2). There were no significant differences among the three subtypes of ADHD in the proportion who experienced at least one unintentional injury by year 9, however, regardless of whether concurrent psychopathology in year 1 was controlled. Similarly, among children with ADHD in year 1, neither I nor HI symptoms predicted the child experiencing an unintentional injury by year 9, regardless of whether concurrent psychopathology in year 1 was controlled.
Table 4.
Prediction of parent report of at least one nontrivial unintentional injury of the child during years 2–9 from DSM-IV subtypes versus the comparison group and (Models 1 and 2) and numbers of symptoms of inattention and hyperactivity-impulsivity (Models 3 and 4) in the full sample.
| Nominal Subtypes as Predictors vs. Comparison | Counts of ADHD Symptoms as Predictors | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||
| Predictors | O.R. | 95% C.I. | O.R. | 95% C.I. | Predictors | O.R. | 95% C.I. | O.R. | 95% C.I. |
| ODDa | 1.22 | (1.04 – 1.43) | ODDa | 1.18 | (1.00 – 1.40) | ||||
| CDa | 0.65 | (0.50 – 0.84) | CDa | 0.66 | (0.52 – 0.85) | ||||
| Internalizinga | 1.14 | (1.03 – 1.25) | Internalizinga | 1.13 | (1.03 – 1.24) | ||||
| ADHD-I | 2.38 | (0.70 – 8.08) | 1.28 | (0.34 – 4.76) | Ia | 1.01 | (0.83 – 1.25) | 0.92 | (0.73 – 1.15) |
| ADHD-HI | 2.86 | (1.18 – 6.97) | 2.66 | (0.96 – 7.39) | HIa | 1.01 | (0.81 – 1.27) | 1.03 | (0.79 – 1.33) |
| ADHD-C | 3.73 | (1.91 – 7.28) | 2.67 | (1.12 – 6.37) | |||||
Counts of symptoms; odds ratios reflect differences in odds at each greater number of symptoms.
Effect sizes
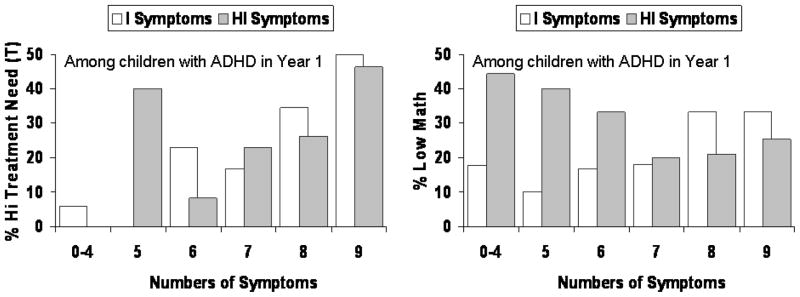
How much do variations in I and HI symptoms matter among children with ADHD? Although care must be taken in interpreting relative risks in case-control studies, relative risk was estimated for the measures of future impairment for which there was a significant difference in the magnitudes of association between I and HI symptoms to provide an easily interpreted index of effect sizes. For these analyses, dichotomized high impairment was defined as an average score on all completed assessments in years 2–9 ≥ 1 SD from the sample mean in the direction of impairment. As shown in Figure 5, among children with ADHD in year 1, the risk of exhibiting high teacher-rated need for treatment increased by an average of 46% with each additional I symptom. As a result, the risk that children with 8–9 I symptoms in year 1 would exhibit high teacher-rated need for treatment (44.6%) was 11.6 times greater than for children with 0–5 I symptoms (3.8%). Also shown in Figure 5, the risk of low mathematics achievement increased by an average of 24% with each additional I symptom. As a result, the risk of low mathematics achievement was 220% greater (relative risk = 2.2) among children with 8–9 I symptoms (33.3%) than children with 0–5 I symptoms in year 1 (14.8%). Thus, for these key indicators of functioning in school, the differences between children with varying levels of I symptoms are clinically significant.
Figure 5.
Percent of children who met criteria for ADHD in year 1 who exhibited dichotomized high impairment (i.e., an average score across all completed assessments in years 2–9 ≥ 1 SD from the sample mean in the direction of impairment) at each number of inattention (I) and hyperactivity-impulsivity symptoms for measures of impairment for which inattention symptoms were significantly more strongly related to impairment than hyperactivity-impulsivity symptoms (left panel) and vice-versa (right panel). Counts of 0-4 symptoms were collapsed because few children with ADHD had fewer than 4 symptoms of either dimension in year 1.
Summary of findings
Table 5 presents a summary of significant differences identified in the present analyses among children who met criteria for any subtype of ADHD in year 1. If the present alternative diagnostic modifiers are adopted in DSM-V, it will be necessary to determine if the overall diagnosis should still be based on ≥ 6 symptoms of either I or HI symptoms. Determining the optimal diagnostic threshold for the overall diagnosis is beyond the scope of this paper, but to consider the validity of the continuous modifiers should a change in the overall diagnosis be made, all analyses summarized in the last two columns of Table 5 were repeated for children who exhibited ≥ 6 of any ADHD symptoms. The results were qualitatively similar, but even when concurrent psychopathology in year 1 was controlled, both I and HI significantly predicted caregiver-reported need for treatment and HI significantly predicted peer disliking. In contrast, I symptoms no longer significantly predicted reading scores when concurrent psychopathology was controlled (but did so when it was not controlled).
Table 5.
Summary of significant differences among the three subtypes of ADHD and associations of inattention and hyperactivity-impulsivity symptoms with on continuous measures of impairment across years 2–9 among children who met criteria for any subtype of ADHD in year 1. Results are presented separately for analyses in which symptoms of other forms of concurrent psychopathology in year 1 were not and were controlled.
| Nominal Subtypes | Counts of Symptoms | |||
|---|---|---|---|---|
| Controlling Concurrent Psychopathology in Year 1: | No | Yes | No | Yes |
| Global Measures of Impairment (Informant) | ||||
| Need for treatment (parent) | ADHD-C > ADHD-HI | No differences | I, HI | Neither |
| Need for treatment (teacher) | ADHD-C > ADHD-HI | ADHD-C > ADHD-HI | I, HI | Ic |
| CGAS (interviewer)a | ADHD-C < ADHD-I = ADHD-HI | No differences | I, HI | I |
| Domain-Specific Measures of Impairment (Informant) | ||||
| Peer disliking (teacher) | ADHD-C > ADHD-I | ADHD-C > ADHD-I | HI | Neither |
| Peer ignoring (teacher) | ADHD-C > ADHD-HI | ADHD-C > ADHD-HI | I | I |
| Reading achievement (youth) | ADHD-I < ADHD-C = ADHD-HI | No differences | HI | HIc |
| Mathematics achievement (youth) | No differences | No differences | I (inverse) | I (inverse)c |
| Unintentional injury (parent) | No differences | No differences | No differences | No differences |
Lower scores reflect greater impairment.
Subtype that is not listed did not differ at p < .05 from either of the listed subtypes.
Difference between magnitudes of the associations of I and HI symptoms significant at p < .05 when concurrent psychopathology in year 1 was controlled.
Note: CGAS = Children’s Global Assessment Scale; ADHD-I = predominantly inattentive subtype; ADHD-HI = predominantly hyperactive-impulsive subtype; ADHD-C = combined subtype; no differences = no differences among the three subtypes of ADHD at p < .05; neither = no association between either the number of symptoms of inattention or the number of hyperactive-impulsive symptoms at p < .05.
DISCUSSION
Consistent with a recent meta-analytic review of the literature of mostly cross-sectional studies (Willcutt et al., 2010), the present findings strongly support the predictive validity of the DSM-IV diagnostic criteria for ADHD; at least one subtype of ADHD exhibited high levels of every measure of functional impairment over the next 8 years (except for reading scores), even when intelligence, demographics, and concurrent psychopathology in year 1 were controlled. In addition, each subtype of ADHD is valid in the sense of predicting the overall diagnosis of ADHD 8–9 years later. These results are impressive given that the measures of impairment were obtained from four sources: mothers, teachers, interviewers, and individual academic testing of the youth. Because each subtype of ADHD was found to exhibit long-term functional impairment relative to comparison children over and above impairment associated with concurrent forms of psychopathology, it is essential that the DSM-V definition of ADHD comprehensively capture all children who meet DSM-IV criteria for all three subtypes of ADHD.
Concurrent Symptoms of Other Mental Disorders in Year 1
All three subtypes of ADHD exhibited more concurrent symptoms in year 1 of mother-reported anxiety and depression and mother and teacher-reported ODD, and CD symptoms than the comparison group. However, there were significant differences among the subtypes: Children who met criteria for ADHD-C exhibited more ODD symptoms than the ADHD-I group; both the ADHD-C and ADHD-HI groups exhibited more CD symptoms than ADHD-I; and the ADHD-C group exhibited more anxiety and depression symptoms than ADHD-HI (Table 1). Among children who met criteria for any subtype of ADHD in year 1, only the number of HI symptoms was independently associated with the numbers of concurrent symptoms of ODD and CD and only the number of I symptoms was independently associated with the number of concurrent anxiety and depression symptoms. These findings are consistent with evidence that I and HI symptoms are associated with different forms of concurrent and future psychopathology (Lahey & Willcutt, 2002), but also mean that it is essential to control symptoms of concurrent psychopathology in assessing the predictive validity of alternative approaches to reducing the heterogeneity of ADHD.
Instability of the Nominal Subtypes of ADHD
As previously reported for the present sample through year 8 (Lahey et al., 2005), a marked degree of unsystematic shifting among the DSM-IV subtypes of ADHD over time was found in the present analyses through year 9 (Figure 2). When considered with the similar findings of studies of children and adolescents diagnosed at older ages (Hinshaw, 2006; Todd et al., 2008), the lack of stability of the DSM-IV subtypes indicates that nominal subtypes are untenable. One cannot meaningfully subtype affected persons if those persons frequently change from one subtype to another over time.
Therefore, it is essential to evaluate alternative ways of accounting for individual differences among children with ADHD to facilitate both clinical practice and research. Although nominal subtypes of ADHD are unstable over time, Figure 1 shows that the number of symptoms of HI (and, to a lesser degree, the number of I symptoms) continued to differentiate the three DSM-IV subtype groups defined in year 1 over many years. That is, although nominal subtypes are unstable, counts of I and HI symptoms among children with ADHD may be stable enough over time to be valid.
Predictive Validity of Counts of Symptoms as a Diagnostic Modifier
In the present study, an alternative approach to reducing the heterogeneity of ADHD was evaluated. This alternative posits that: (1) the heterogeneity among children with ADHD is related to their numbers of I and HI symptoms, and (2) although nominal subtypes are inherently unstable over time, the numbers of each dimension of symptoms are stable enough over long periods of time to be useful diagnostic modifiers. As summarized in Table 5, among children who met criteria for ADHD in year 1, their numbers of I and HI symptoms in year 1 were associated with the same global measures of impairment in two instances. In addition, I symptoms in year 1 significantly predicted several measures of impairment across years 2–9 in fully controlled analyses. As shown in Figure 5, the magnitudes of the associations of I symptoms with future impairment were robust. Children with ADHD with high levels of I symptoms were more than twice as likely as children with few I symptoms to have low mathematics scores and over 11 times more likely to receive high teacher ratings of need for treatment, even when intelligence, concurrent psychopathology, and other covariates were controlled.
It is important to note that the present analyses provided a rigorous test of the predictive validity of I and HI symptoms in two ways. First, in order to be relevant to the proposal to use numbers of I and HI symptoms as diagnostic modifiers of the diagnosis of ADHD, the associations of I and HI symptoms with future impairment could only be assessed among children who met criteria for ADHD in year 1. Thus, the robust associations of I and HI symptoms with future impairment were found in spite of the highly skewed distributions of symptoms among children with ADHD. Second, it was necessary to control intelligence, demographic and methodologic covariates, and concurrent psychopathology in year 1 to be certain that the association of counts of I and HI symptoms with future impairment did not only reflect confounded factors. The results for I and HI symptoms are particularly impressive given that concurrent psychopathology often was a significant predictor of future impairment in these models. In particular, consistent with earlier analyses of the present sample, ODD symptoms were often a significant independent predictor of global impairment (Lahey et al., 2004) and internalizing symptoms were a robust independent predictor of academic achievement (Massetti et al., 2008)
Limitations and Future Directions
The present study is the only multi-year longitudinal study of the DSM-IV subtypes of ADHD and one of only three longitudinal studies of the stability of the DSM-IV subtypes of ADHD (Hinshaw, 2006; Todd et al., 2008). Nonetheless, it is important to acknowledge two key limitations of the present study. First, because the number of children who met criteria for each subtype of ADHD in year 1 was modest, particularly for the ADHD-HI and ADHD-I subtypes, it is very likely that the present analyses underestimate the number of differences among the subtypes due to limited statistical power. In the same way, differences among children with ADHD associated with their numbers of I and HI symptoms are likely to be underestimated as well, although perhaps to a lesser extent because of the greater power associated with counts of symptoms than nominal subtypes.
Second, because the participants were 4–6 years old in year 1, it is possible that the children who met criteria for ADHD-I may not be typical of children who first present with this subtype of ADHD at older ages. Nonetheless, it is important to note that all of the present findings regarding ADHD-I are consistent with the conclusions of a meta-analytic review of the large literature of cross-sectional and longitudinal studies relevant to the validity of ADHD and its subtypes based on children and adolescents across a broad age range (Willcutt et al., 2010).
Future studies should address the unexpected finding that 20 of 130 children in the comparison group met criteria for ADHD at least three times over the ensuing 8 years. Thirty-percent of these children exhibited 4 or more symptoms of either inattention or hyperactivity-impulsivity in year 1, and hence, might be viewed as incipient cases. The majority had few ADHD symptoms in year 1, however. All current estimates of the prevalence of ADHD are based on cross-sectional samples. In the absence of longitudinal data on the prevalence of ADHD in representative samples, one cannot conclude that the number of comparison children who met criteria for ADHD at least three times in 8 years in the present study was either high or low. To fully understand the burden of ADHD over childhood and adolescence longitudinal studies of representative samples are needed.
Conclusions
Although the nominal subtypes of ADHD are too unstable over time to be useful in clinical practice or research, the numbers of I and HI symptoms could be used effectively to reduce the heterogeneity of ADHD related to differences in school-based outcomes. Because prognosis is a key issue in treatment planning, it may be highly useful for clinicians to qualify the diagnosis of ADHD with counts of the numbers of each dimension of symptoms (e.g., “7 symptoms of I and 3 symptoms of HI were present at the time of assessment”). Such a shift away from nominal subtypes would focus attention on the dimensions of symptoms and their differential associations with other forms of psychopathology and future impairment. Similarly, researchers could study individual differences in prognosis, etiology, pathophysiology, and response to treatment among children with ADHD by studying differences associated with continuous counts of the two dimensions of ADHD symptoms.
Contributor Information
Benjamin B. Lahey, University of Chicago
Erik G. Willcutt, University of Colorado
References
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Dishion TJ. The peer context of troublesome child and adolescent behavior. In: Leone PE, editor. Understanding troubled and troubling youth. Newbury Park, CA: Sage; 1990. pp. 128–153. [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, et al. A practical measure of impairment: Psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Hanson KS. Criterion validity of informants in the diagnosis of disruptive behavior disorders in children: A preliminary study. Journal of Consulting and Clinical Psychology. 1994;62:410–414. doi: 10.1037/0022-006X.62.2.410. [DOI] [PubMed] [Google Scholar]
- Hinshaw S, Owens E, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. Journal of Consulting and Clinical Psychology. 2006;74:489–499. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, et al. Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd GW, et al. DSM-IV field trials for attention-deficit/hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, et al. Three-year predictive validity of DSM-IV attention–deficit/hyperactivity disorder in children diagnosed at 4–6 years of age. American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Stein MA, Loney J, Trapani C, Nugent K, et al. Validity of DSM-IV attention-deficit/hyperactivity disorder for younger children. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:695–702. doi: 10.1097/00004583-199807000-00008. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Hulle CV, Garriock HA, Urbano RC, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Willcutt E. The validity of attention-deficit/hyperactivity disorder among children and adolescents. In: Jensen PS, Cooper J, editors. Attention deficit hyperactivity disorder: State of the science, best practices. Kingston, NJ: Civic Research Institute; 2002. pp. 1–23. [Google Scholar]
- Lee SS, Hinshaw SP. Predictors of adolescent functioning in girls with attention deficit hyperactivity disorder (ADHD): The role of childhood ADHD, conduct problems, and peer status. Journal of Clinical Child and Adolescent Psychology. 2006;35:356–368. doi: 10.1207/s15374424jccp3503_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massetti GM, Lahey BB, Pelham WE, Loney J, Ehrhardt A, Lee SS, et al. Academic achievement over 8 years among children who met modified criteria for attention-deficit/hyperactivity disorder at 4–6 years of age. Journal of Abnormal Child Psychology. 2008;36:399–410. doi: 10.1007/s10802-007-9186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT. Neuropsychologic theory and findings in attention-deficit/hyperactivity disorder: The state of the field and salient challenges for the coming decade. Biological Psychiatry. 2005;57:1424–1435. doi: 10.1016/j.biopsych.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms of the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Piacentini JC, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? Journal of Abnormal Child Psychology. 1992;20:51–62. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Piacentini J, Schwab-Stone M, Wicks J. Diagnostic Interview Schedule for Children. New York: Columbia University; 1993. [Google Scholar]
- Sonuga-Barke EJS, Sergeant JA, Nigg J, Willcutt E. Executive dysfunction and delay aversion in attention deficit hyperactivity disorder: Nosologic and diagnostic implications. Child and Adolescent Psychiatric Clinics of North America. 2008;17:367. doi: 10.1016/j.chc.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Thorndike RL, Hagen EP, Sattler JM. Stanford-Binet Intelligence Scale. Chicago: Riverside Press; 1986. [Google Scholar]
- Todd RD, Huang H, Todorov AA, Neuman RJ, Reiersen AM, Henderson CA, et al. Predictors of stability of attention-deficit/hyperactivity disorder subtypes from childhood to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:76–85. doi: 10.1097/chi.0b013e31815a6aca. [DOI] [PubMed] [Google Scholar]
- Wahlstedt C, Thorell LB, Bohlin G. Heterogeneity in ADHD: Neuropsychological pathways, comorbidity and symptom domains. Journal of Abnormal Child Psychology. 2009;37:551–564. doi: 10.1007/s10802-008-9286-9. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, et al. Validity of DSM-IV attention deficit/hyperactivity disorder. Unpublished manuscript 2010 [Google Scholar]
- Woodcock RW. Woodcock–Johnson Psychoeducational Battery. Allen, TX: DLM Teaching Resources; 1977. [Google Scholar]